Abstract
A growing body of research has identified food insecurity as a barrier to antiretroviral therapy (ART) adherence. We systematically reviewed and summarized the quantitative literature on food insecurity or food assistance and ART adherence. We identified nineteen analyses from eighteen distinct studies examining food insecurity and ART adherence. Of the thirteen studies that presented an adjusted effect estimate for the relationship between food insecurity and ART adherence, nine found a statistically significant association between food insecurity and sub-optimal ART adherence. Four studies examined the association between food assistance and ART adherence, and three found that ART adherence was significantly better among food assistance recipients than non-recipients. Across diverse populations, food insecurity is an important barrier to ART adherence, and food assistance appears to be a promising intervention strategy to improve ART adherence among persons living with HIV. Additional research is needed to determine the effectiveness and cost-effectiveness of food assistance in improving ART adherence and other clinical outcomes among people living with HIV in the era of widespread and long-term treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adherence to antiretroviral therapy (ART) is a primary determinant of HIV clinical outcomes [1–4]. Poor ART adherence is associated with virologic failure [2], CD4 decline [3], progression to AIDS [1], and increased mortality [4]. In addition to the clinical benefits of high levels of ART adherence for people living with HIV (PLHIV), ART dramatically reduces the likelihood of HIV transmission, underscoring the value of adherence for secondary prevention [5]. Despite the importance of high ART adherence, a meta-analysis found that the proportion of patients achieving adequate levels of ART adherence (as defined within each study) was 77 % in sub-Saharan Africa and 55 % in North America [6]. As the push for expanded access to HIV treatment intensifies under the new WHO treatment recommendations [7], it is essential to identify constraints to ART adherence and strategies to overcome them.
In qualitative data from resource-constrained settings, PLHIV have indicated lack of sufficient food or food insecurity as a reason for ART non-adherence due to the aggravation of side effects, increased hunger from treatment, and the inability to prioritize treatment among competing subsistence needs [8–10]. Food security “exists when all people, at all times, have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life” and is determined by adequate food availability, access, and utilization [11]. Food insecurity can manifest as inadequate intake of calories, poor diet quality and insufficient intake of diverse foods and nutrients required for a healthy life, and adverse psychosocial effects such as anxiety about the ability to find food [12]. Food insecurity is associated with adverse clinical outcomes among PLHIV, including incomplete HIV RNA suppression [13–16], CD4 decline over time [17], lower body mass index [18], opportunistic infections [19], increased hospitalizations [19], worse health-related quality of life [19], and HIV-related mortality [20]. Food insecurity likely produces these adverse clinical outcomes among PLHIV through various pathways, such as adversely affecting a patient’s nutritional status or mental health, and hindering adherence to ART and retention in care [21]. The extent to which food insecurity affects the health of PLHIV by impacting ART adherence has been increasingly explored in quantitative studies, but limited awareness of the breadth of this literature has precluded conclusions about the strength of this evidence or the consistency of the findings. In addition, food supplementation and livelihood support interventions are increasingly common among food-insecure HIV-infected populations [22–24]. Across 336 HIV care and treatment sites in nine sub-Saharan African countries, treatment for severe malnutrition and food rations were available at 36 and 31 % of sites, respectively [25]. Early data have suggested that food assistance may improve retention in care [23, 26], but the effect of such support on adherence to ART is poorly understood. As policymakers increasingly recommend food assistance as an important component of HIV care and as more resources are directed towards nutritional support for PLHIV [7], it is critical to understand the extent to which food insecurity is a barrier to ART adherence and if food assistance programs are effective in improving adherence. Thus, the purpose of this paper is to systematically review and summarize the evidence regarding the association between (1) food insecurity and ART adherence and (2) food assistance and ART adherence in order to better inform programmatic efforts.
Methods
Study Inclusion Criteria
Studies were included in the review if they examined the association between food insecurity and ART adherence or food assistance and ART adherence and presented or permitted calculation of an overall measure of association (e.g. risk ratio). This included studies that examined any measure of restricted food access or use, with the exception of medication-related food restrictions or instructions, or that assessed the influence of food rations or other types of food aid, with the exception of studies of micronutrient supplements as these have been summarized in another review [27] and were not considered a form of food assistance. Clinic- and community-based studies examining the influence of food insecurity or food supplementation on ART adherence were eligible for inclusion regardless of whether other outcomes (e.g. CD4 count) were of primary interest. Adherence was conceptualized as daily compliance with prescribed medications, which we defined as distinct from missed clinic visits, treatment interruption greater than 3 months, or loss-to-follow-up and attrition. All adherence measurements, including self-report, unannounced or announced pill counts, pharmacy records and electronic medication monitoring, were acceptable for inclusion as were all adherence thresholds (i.e. >95, <90, <85, <80 % of prescribed doses or inadequate adherence according to missed doses). Qualitative studies, reviews or editorials, research published in abstract form only or that did not undergo peer review, studies examining adherence to pre- or post-exposure prophylaxis or prophylaxis for the prevention of mother-to-child transmission, and any studies that did not report a measure of association between food insecurity or food assistance and adherence were excluded. Methods for the review and inclusion criteria were specified in advance, with the following additional inclusion criteria specified after the full text review: (1) definition of treatment interruption as non-adherence for at least 3 months and exclusion of papers examining treatment interruption as the outcome, (2) exclusion of two papers identified in the search that compared adherence in two groups of wasted HIV patients receiving different types of food supplements [28, 29]; and (3) exclusion of studies identified in the search that evaluated combination support programs for PLHIV that included a nutritional component but did not present or permit estimation of the individual effect of food assistance distinct from the other services in the program [30–33]. Although we did not limit inclusion to adult populations, no studies examined the association between food insecurity and ART adherence in pediatric populations, and only one study examined the association between food assistance and adherence in a pediatric population [34], but was excluded because it did not specify the type of food assistance or the criteria for receiving such support.
Search Strategy
The review was conducted in accordance with PRISMA guidelines. We systematically searched PubMed/MEDLINE, Web of Science, PsychInfo, Sociological Abstracts, and EconLit from inception to August 15, 2013. We purposefully designed a broad search strategy to identify studies assessing the association between food insecurity and ART adherence or food assistance and ART adherence. There were no language or study design restrictions. Our search combined terms from broad categories of antiretroviral therapy, adherence, and food security and supplementation (see “Appendix” for full PubMed search strategy). When available, we utilized the databases’ controlled vocabulary or index (e.g., medical subject headings (MeSH)) as well as free text terms. In addition to food-related search terms (e.g. “food,” “hunger,” “nutrition”), we included search terms to identify papers examining a variety of adherence risk factors (e.g. “poverty,” “barrier,” “risk factors”) as we anticipated that, in some manuscripts, food insecurity may be assessed as a covariate but not as the main exposure of interest. In these cases, when included as a covariate, we hypothesized that food insecurity would be unlikely to appear as a key word or in the title or abstract. After excluding papers by title and abstract review, we conducted a manual, full-text search of each potentially relevant article by searching for key terms related to food insecurity and food assistance such as “food,” “hunger,” “nutrition,” “meal” or foreign language equivalents for articles written in French and Portuguese. In addition, we reviewed the reference list of all included studies for manuscripts that may have not been identified by our initial search strategy.
Data Abstraction and Analysis
From each study, we abstracted the following: date of publication, setting and timeframe of the study, sample size, measure of adherence, measure of food insecurity or food assistance, and the measure of effect for the association between food insecurity or food assistance and adherence. In order to better understand the intersection of food insecurity and poverty, we also abstracted any reported measure(s) of socioeconomic status (SES) (e.g. income, occupation, education) and whether SES was assessed as a confounder or effect modifier. Quality and risk of bias in individual studies was assessed by abstraction of the following indicators: clear description of the setting and study population, data measurement sources, study design, and other indicators of internal validity such as participation rate and sampling method. For intervention studies of food assistance, we paid particular attention to study design in order to assess internal validity. However, quality was not an inclusion criterion consistent with recommendations for systematic reviews and meta-analysis [35]. For the studies of food insecurity and ART adherence, we summarized measures of association with a forest plot and assessed the risk of bias by visual assessment of a funnel plot using STATA version 12 [36]. Due to the small number of intervention studies and the distinct measures of association, we were unable to create forest and funnel plots for the intervention studies on food assistance and ART adherence. Due to the variety of ART adherence thresholds and food insecurity or food assistance indicators, as well as significant variability in study populations and geographic locations, a meta-analysis to produce a pooled measure of effect was not conducted.
Results
Search Yield
The database search produced 1,883 papers, of which 960 were excluded based on title alone and 554 were excluded based on abstract review (Fig. 1). Of the 369 remaining papers, 17 full-length papers were unable to be retrieved electronically but did not indicate by title or abstract that they included food insecurity or food assistance in their analyses. Overall, 352 full-length articles were searched for key terms related to food insecurity and food assistance.
Food Insecurity and ART Adherence
Seventeen papers, from sixteen distinct study populations, were identified as meeting the inclusion criteria for food insecurity and ART adherence through the electronic search. We were aware of two additional papers meeting inclusion criteria [37, 38] from a previous review on food insecurity and ART adherence [39] that were not identified through the database search. Two papers on food insecurity and ART adherence were from the same study [40, 41] presenting measures of association from overlapping samples of PLHIV, and both were included. Two additional papers were on sub-samples from a large survey population in Cameroon and both were included [42, 43]. In total, 19 papers from 18 distinct study populations met the inclusion criteria for food insecurity and ART adherence and are included in the review.
Food Assistance and ART Adherence
Of the 352 full-length articles searched for key terms, three papers met the inclusion criteria for food assistance and ART adherence. One additional paper not yet indexed in the included databases was identified through Google Scholar [44]. In total, four papers met the inclusion criteria for food assistance and ART adherence.
Characteristics of Food Insecurity Studies
The studies examining the association between food insecurity and ART adherence were carried out in diverse populations and geographic locations (Table 1). Twelve studies [13, 37, 38, 40–43, 45–49] were cross-sectional, five were prospective cohort studies [15, 16, 50–52], one was a retrospective cohort [53], and one was a case–control study [54]. One cross-sectional study [37] analyzed ART adherence as the exposure and food insecurity as the outcome (the inverse of the pathway of interest); this study is included but cannot be directly compared to the other studies that examined food insecurity as the exposure of interest. Most studies used convenience or purposive samples; only five [13, 16, 38, 42, 43] used probability sampling and one [47] used administrative data. Of the eight studies that specified or allowed calculation of response rates, six [13, 15, 16, 42, 45, 50] had over 90 % participation.
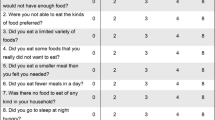
Only three studies [13, 15, 16] used complete, validated food security scales to measure food insecurity whereas six studies [37, 40, 41, 46, 47, 53] used modified versions of validated food insecurity scales (i.e. the US Food Security Scale and the Radimer/Cornell Questionnaire) and two studies [50, 54] assessed food access with multiple questions that were not from validated scales (Table 2). The remaining eight studies [38, 42, 43, 45, 48, 49, 51, 52] used single-question indicators of food access or number of meals consumed. Across the studies, food insecurity indicators had different recall periods (4 weeks/1 month, past year, or no time period specified) and used various terminology (e.g. “food insufficiency,” “hunger”) to refer to similar constructs. Measurement of ART adherence also varied; twelve studies used participant self-report, three [47, 50, 53] used pharmacy records, and four studies [13, 40, 41, 46] used unannounced pill counts to compute the ratio of pills counted relative to pills prescribed. The self-report assessments ranged from one to multiple questions or assessment by a visual analog scale and also had various recall periods.
Thirteen studies presenting the relationship between food insecurity and ART adherence adjusted for covariates, while six studies [13, 37, 43, 47, 49, 53] only presented an unadjusted measure of association. Studies adjusted for different sets of covariates, and most studies controlled for common confounders such as substance abuse, depression, and comorbidities. All thirteen studies that presented adjusted estimates considered confounding by SES in their analyses, with eight studies [15, 16, 38, 40, 41, 48, 50, 54] controlling for some measure of SES in their adjusted models (by inclusion of variables such as education, employment, income, household financial situation, and housing conditions). Five papers excluded a measure of SES from the final multivariable model either because it was determined not to be a confounder [42, 46, 51, 52] or because of collinearity with other variables in the model [45]. The funnel plot did not suggest that there was bias across studies of food insecurity and ART adherence, as most studies fell within or around the pseudo 95 % confidence intervals and were dispersed on both sides of the summary measure of association [55] (Fig. 2).
Forest plot of measures of association between food insecurity and ART non-adherence. *Anema et al. [47], Marcellin et al. [43], Parashar et al. [53], Peretti-Watel et al. [38], Van Dyk [49], and Weiser et al. [13] presented unadjusted odds ratios. All other studies present adjusted odds ratios. Forest plot excludes Anema et al. [37] and includes multiple measures of association presented in the same study for Berhe et al. [54] and Peretti-Watel et al. [38] (see Table 2). “Balanced meals” [54] was not defined. Poverty stressors [40] refers to a seven-item assessment adapted from the US Food Security Scale measuring food insecurity over the previous year, plus one question about housing access. Food privation [38] refers to whether or not a member of the household did not take any complete meal during a whole day due to lack of money during the prior 4 weeks
Association Between Food Insecurity and ART Adherence
Overall, of the thirteen studies that presented an adjusted effect estimate, ten found a statistically significant association between food insecurity and ART adherence (Table 2; Fig. 3). Nine of these studies found increased odds of ART non-adherence among food-insecure respondents. One study [52], conversely, found that food-insecure respondents were more likely to be adherent to ART in unadjusted and adjusted analyses. This association was based on reported food insufficiency in the 30 days prior to ART initiation. The investigators hypothesized that this positive association between food insufficiency at baseline and ART adherence at the end of the study period may be due to the possibility that participants reporting food insecurity at baseline were more likely to receive food assistance over the duration of the study from an external source, although the investigators were unable to validate this assumption. Finally, one study that did not find a statistically significant association between food insufficiency and ART adherence among the entire study population found that food insufficiency reduced the odds of perfect adherence (never missing a dose or having a late dose in the last week) compared to good adherence (having late doses but never missing a dose in the last week) when the analysis was restricted to adherent participants [48].
In order to take into account study design, we examined the results when stratified by type of study. Of the five prospective cohort studies, three found statistically significant increased odds of suboptimal ART adherence among persons reporting food insecurity [15, 16, 51], and one found a small and non-significant increased odds of suboptimal ART adherence among food-insecure persons [50]. One retrospective cohort study found reduced odds of ART adherence among food-insecure, unstably-housed PLHIV in an unadjusted analysis but did not assess this relationship in multivariate analyses [53]. The single case–control study [54] found increased odds of suboptimal ART adherence among participants reporting that they were unable to get adequate or quality food or that they ate less than three meals a day.
Among the seven cross-sectional studies presenting adjusted measures of association, five found an association between food insecurity and ART non-adherence. The four cross-sectional studies that only presented unadjusted estimates found reduced odds of ART adherence among food-insecure respondents [13, 43, 47, 49]. Finally, one additional cross-sectional study examining the inverse pathway of interest found that respondents with self-reported adherence greater than at least 95 % of prescribed medications were less likely to be food-insecure in unadjusted analyses [37].
Characteristics of Food Assistance Studies
Four studies were identified that examined the effect of food assistance (i.e. food rations) on ART adherence (Table 1). All four studies were conducted in sub-Saharan Africa, and examined food supplementation programs compared to clinics or regions not receiving the programs. Food assistance consisted of monthly food rations (e.g. cereal, legume, soy, fortified vegetable oil) designed to meet either the individuals’ or entire households’ nutritional needs. Two studies in Zambia compared ART adherence among recipients of food aid compared to PLHIV who attended clinics not selected for food aid or that would not receive food aid until a later time (four intervention and four “control” clinics) [22, 56]. One study in Mozambique compared patients from Sofala Province selected to receive food assistance with patients not receiving food aid in the Zambezia region, where there was not a food assistance program at the time [44]. The study in Niger compared food aid recipients with a historical control group from the same clinic [57].
In order to assess how well comparison groups approximated the counterfactual, we examined the methods used to compare food recipients and non-recipients. Of the two studies comparing intervention and control clinics, one study assessed comparability of the food and control groups according to baseline characteristics [22] while the other study matched intervention clinics to control clinics on several criteria (active patient population, duration of operation, and historical patient survival) [56]. Two studies used propensity score matching to match food assistance recipients and non-recipients based on observed characteristics (gender, education, household size, etc.) and used difference in differences estimation to compare the change in adherence over time for the food assistance recipients with the change in adherence over time for those who did not receive food aid by estimating the overall pre- and post- intervention difference between the two groups [44, 56].
Association Between Food Assistance and ART Adherence
In the Zambia study by Cantrell et al. which compared PLHIV in four clinics selected to receive food aid to PLHIV attending four clinics that did not receive food aid until a later time, patients in the food group were more likely to be adherent, defined as possessing their medication on at least 95 % of days during the first year of therapy, compared with those who did not receive food aid (RR = 1.5, 95 % CI (1.2–1.8) [22]. In another Zambia study, after propensity score matching of food recipients and non-recipients on socio-demographic characteristics, a greater proportion of food aid recipients had optimal adherence compared to those who did not receive food aid after 6 months (98 vs. 89 %, p < 0.01) [56]. Likewise, in Niger, a greater proportion of PLHIV receiving food assistance were found to be adherent compared to a historical control group from the same clinic prior to the implementation of the food assistance program (98.4 vs. 77.4 %, p < 0.005) [57]. Finally, a retrospective study in Mozambique found no significant difference in ART adherence, measured as the number of times patients failed to collect their medication, among food assistance recipients and non-recipients residing in two separate provinces after 6 and 12 months [44].
Discussion
Over the past decade, the body of literature examining the relationship between food insecurity and ART adherence has expanded rapidly. Our review of this diverse literature found that food insecurity is an important barrier to ART adherence. Overall, the studies identified were conducted in very different geographic locations in both resource-rich and resource-poor countries, and both food insecurity and ART adherence were measured inconsistently across studies. However, there is a consistent negative association between food insecurity and ART adherence in all but three of the nineteen studies. In addition, three of four studies on food assistance found that food recipients were more adherent than non-recipients. These two lines of evidence buttress the growing body of qualitative evidence about the association between food insecurity, food assistance and adherence.
Nevertheless, weak study designs and inconsistent measurement limit our understanding of the causal relationship between food insecurity and ART adherence. Most of the studies to date are cross-sectional, precluding temporal or causal interpretation. However, four out of five longitudinal studies included in this review corroborated cross-sectional findings, suggesting that food insecurity may indeed lead to poor ART adherence. Furthermore, accurate measurement of both food insecurity and adherence is often inconsistent. All but seven of the food insecurity studies used self-reported ART adherence which may reflect only short-term or average adherence, or may overestimate adherence in comparison to more objective measurements such as pill counts, pharmacy data, or electronic medication monitoring [58–60]. Nine studies employed complete or modified validated food insecurity scales, while others used only single-question food insecurity indicators. Modified scales or single-question indicators may not adequately capture all aspects of food insecurity. Future research would benefit from more consistent indicators of food insecurity and distinct terms that indicate which measure has been employed: for example, “food insecurity” may refer exclusively to the construct captured by validated scales (e.g. U.S. Household Food Security Survey or Household Food Insecurity Access Scale) measured minimally at baseline and endline, whereas “food access,” “food utilization,” and “food availability” could refer to specific dimensions of food insecurity captured by shorter scales or single questions. Future research should also use longitudinal study designs and objective measures of adherence such as electronic medication monitoring to better understand impacts of food insecurity on adherence. In addition, not all studies measured or adjusted for covariates that may be associated with both food insecurity and ART adherence, such as depression and substance abuse, which could lead to residual confounding. Although these study limitations preclude definitive causal conclusions, the consistency of the findings across studies employing diverse food insecurity and adherence measurements and adjusting for different sets of confounders bolsters confidence in the association between food insecurity and poor adherence.
The relationship between food insecurity and ART adherence is likely bidirectional [21, 39], complicating interpretation of the cross-sectional studies. Food insecurity may undermine adherence, and ART non-adherence may exacerbate food insecurity through worse health outcomes and limited ability to work. Indeed, antiretroviral therapy is a significant predictor of improved food security over time [61, 62]. In order to better elucidate the pathways through which food insecurity and ART adherence influence each other, future research would be strengthened by clearly documenting the time-ordering of food insecurity and adherence measures, explicitly assessing the relationships between food insecurity and SES measures to determine the overlap of these constructs [63], and considering alternative analytic methods such as the use of marginal structural models or targeted variable importance methods which can be used to rank factors according to their impact on health [64]. Additionally, adherence to ART is only one aspect of an HIV care continuum that includes HIV testing, successful linkage to care, ART initiation, and adherence to medications and maintenance of care [65, 66]. Although this review focused on ART adherence, other studies have found a relationship between food insecurity and retention in care [19, 23, 26]. Thus, future reviews should consider the possible effects of food insecurity across the entire spectrum of the HIV care continuum.
Studies examining the effect of food assistance on adherence to ART provide important additional evidence regarding the relationship between food security and ART adherence. Although our review only identified four studies quantitatively examining whether food assistance can mitigate food insecurity and improve adherence, three of those studies found a positive association between food assistance and ART adherence. However, none of these intervention studies were randomized, which limits causal attribution. Randomized trials of food supplementation or other strategies to reduce food insecurity will provide valuable evidence for the benefits of improved food security on ART adherence and identify which types of support are best. Because ART must be continued for life, program evaluations that assess the long-term effectiveness of food assistance both for medication adherence as well as retention in care are critical to understanding strategies to mitigate the deleterious effects of food insecurity [67]. Although not included in our review, evidence indicating that food assistance increases adherence to clinic visits [23] suggests that food assistance may be used as an incentive to encourage patients to collect their medication [12, 68], and some argue that receipt of food support should be conditional upon both adherence to clinic visits and ART prescription refill compliance in order to optimize outcomes and increase sustainability. Though research on the role of conditional economic incentives in promoting ART adherence has been limited [68], additional studies are ongoing [69]. Food rations and livelihood support may be combined with other support services shown to improve adherence, such as treatment supporters, directly observed therapy, mobile-phone text messages, and diary cards [70], and such comprehensive treatment-support programs have been shown to increase ART adherence and retention [30, 31].
In conclusion, food security appears to influence ART adherence across different environments. In many of the studies reviewed here, food insecurity was associated with sub-optimal ART adherence even after controlling for SES and other factors known to influence adherence. Furthermore, food assistance was associated with improved adherence in three of the four intervention studies. The importance of food security for ART adherence is increasingly recognized by policymakers: for example, new WHO guidelines on the use of antiretroviral drugs identify nutritional support as a critical component of HIV care in food-insecure settings [7]. However, operations and feasibility assessments are required to determine the optimal policies about eligibility and targeting of food assistance or livelihood support and its duration: for example, food assistance may be targeted at alleviating malnutrition and severe illness among wasted PLHIV only, encouraging treatment adherence among patients initiating long-term antiretroviral therapy, or mitigating the more complex effects of food insecurity on HIV health outcomes among affected households and society as a whole [12]. These various scenarios have different implications for the resources required, types of food products needed, and dissemination strategies, and must be weighed against alternate programs targeted to persons suffering from other illnesses with nutritional consequences and to healthy people struggling with food insecurity. Policy changes may also affect the implementation of food assistance or livelihood support programs: for example, as treatment eligibility criteria have been modified to encourage PLHIV to initiate ART at a CD4 count of 500 cells/mm3 or less [7], PLHIV starting treatment may be healthier and experience less severe food insecurity than in the past. Consequently, food and livelihood support programs may be more sustainable and less burdensome for the healthcare system in a setting of lower need. Furthermore, while several studies have examined the effect of food and nutrient supplementation on clinical outcomes such as viral load and CD4 count [71–73], much of this research was carried out before widespread and long-term use of ART. There is less understanding of the effects of food assistance on HIV virologic and immunologic outcomes and mortality among individuals on ART. Prospective studies examining the impact of food assistance that consider disease stage, duration of treatment, and adherence are needed to determine the extent to which food assistance improves clinical outcomes beyond ART alone. As the push for greater HIV treatment coverage intensifies, and with PLHIV remaining on ART for longer and longer durations of time, further examination of the impact of food insecurity on ART adherence is essential to understand ways to intervene to support PLHIV in maximizing treatment benefits and living longer and healthier lives.
References
Bangsberg DR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–3.
Maggiolo F, et al. Similar adherence rates favor different virologic outcomes for patients treated with nonnucleoside analogues or protease inhibitors. Clin Infect Dis. 2005;40(1):158–63.
Sungkanuparph S, et al. Rapid CD4 decline after interruption of non-nucleoside reverse transcriptase inhibitor-based antiretroviral therapy in a resource-limited setting. AIDS Res Ther. 2007;4:26.
Kiwuwa-Muyingo S, et al. The impact of first year adherence to antiretroviral therapy on long-term clinical and immunological outcomes in the DART trial in Uganda and Zimbabwe. Trop Med Int Health. 2012;17(5):584–94.
Cohen MS, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Mills EJ, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–90.
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. Geneva: WHO; 2013.
Nagata JM, et al. Social determinants, lived experiences, and consequences of household food insecurity among persons living with HIV/AIDS on the shore of Lake Victoria, Kenya. AIDS Care. 2012;24(6):728–36.
Goudge J, Ngoma B. Exploring antiretroviral treatment adherence in an urban setting in South Africa. J Public Health Policy. 2011;32(Suppl 1):S52–64.
Weiser SD, et al. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE. 2010;5(4):e10340.
AO F. Rome declaration on world food security. Rome: Food and Agriculture Organization; 1996.
Frega R, et al. Food insecurity in the context of HIV/AIDS: a framework for a new era of programming. Food Nutr Bull. 2010;31(4):S292–312.
Weiser SD, et al. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24(1):14–20.
Wang EA, et al. Food insecurity is associated with poor virologic response among HIV-infected patients receiving antiretroviral medications. J Gen Intern Med. 2011;26(9):1012–8.
Weiser SD, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–20.
Weiser SD, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of homeless and marginally housed HIV-infected individuals in San Francisco. AIDS. 2013;27(18):2953–8.
McMahon JH, et al. Repeated assessments of food security predict CD4 change in the setting of antiretroviral therapy. J Acquir Immune Defic Syndr. 2011;58(1):60–3.
Normen L, et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J Nutr. 2005;135(4):820–5.
Weiser SD, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS. 2012;26(1):67–75.
Weiser SD, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–9.
Weiser SD, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S–39S.
Cantrell RA, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–5.
Ivers LC, et al. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. 2010;7:33.
Sztam KA, Fawzi WW, Duggan C. Macronutrient supplementation and food prices in HIV treatment. J Nutr. 2010;140(1):213S–23S.
Anema A, et al. Availability of nutritional support services in HIV care and treatment sites in sub-Saharan African countries. Public Health Nutr. 2012;15(5):938–47.
Lamb MR, et al. Association of adherence support and outreach services with total attrition, loss to follow-up, and death among ART patients in sub-Saharan Africa. PLoS ONE. 2012;7(6):e38443.
Forrester JE, Sztam KA. Micronutrients in HIV/AIDS: is there evidence to change the WHO 2003 recommendations? Am J Clin Nutr. 2011;94(6):1683S–9S.
Ndekha M, et al. Nutritional status of Malawian adults on antiretroviral therapy 1 year after supplementary feeding in the first 3 months of therapy. Trop Med Int Health. 2009;14(9):1059–63.
Ndekha MJ, et al. Supplementary feeding with either ready-to-use fortified spread or corn-soy blend in wasted adults starting antiretroviral therapy in Malawi: randomised, investigator blinded, controlled trial. BMJ. 2009;338:b1867.
Kabore I, et al. The effect of community-based support services on clinical efficacy and health-related quality of life in HIV/AIDS patients in resource-limited settings in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24(9):581–94.
Franke MF, et al. Improved Retention Associated With Community-Based Accompaniment for Antiretroviral Therapy Delivery in Rural Rwanda. Clin Infect Dis. 2013;56(9):1319–26.
Nyamathi A, et al. Impact of a rural village women (Asha) intervention on adherence to antiretroviral therapy in southern India. Nurs Res. 2012;61(5):353–62.
Talisuna-Alamo S, et al. Socioeconomic support reduces nonretention in a comprehensive, community-based antiretroviral therapy program in Uganda. J Acquir Immune Defic Syndr. 2012;59(4):e52–9.
Biadgilign S, et al. Adherence to highly active antiretroviral therapy and its correlates among HIV infected pediatric patients in Ethiopia. BMC Pediatr. 2008;8:53.
Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
StataCorp. Stata statistical software: Release 12, 2011, StataCorp LP: College Station, TX.
Anema A, et al. High prevalence of food insecurity among HIV-infected individuals receiving HAART in a resource-rich setting. AIDS Care. 2011;23(2):221–30.
Peretti-Watel P, et al. Vulnerability, unsafe sex and non-adherence to HAART: evidence from a large sample of French HIV/AIDS outpatients. Soc Sci Med. 2006;62(10):2420–33.
Young S, et al. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2013. doi:10.1007/s10461-013-0547-4.
Kalichman SC, et al. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–41.
Kalichman SC, et al. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prev Sci. 2011;12(3):324–32.
Boyer S, et al. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Soc Sci Med. 2011;72(8):1383–92.
Marcellin F, et al. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaounde, Cameroon (EVAL survey, ANRS 12-116). Trop Med Int Health. 2008;13(12):1470–8.
Posse M, et al. The effect of food assistance on adherence to antiretroviral therapy among HIV/AIDS patients in Sofala Province, in Mozambique: a retrospective study. J AIDS Clin Res. 2013;4(3):1000198. doi:10.4172/2155-6113.1000198.
Gebo KA, Keruly J, Moore RD. Association of social stress, illicit drug use, and health beliefs with nonadherence to antiretroviral therapy. J Gen Intern Med. 2003;18(2):104–11.
Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med. 2010;72(8):810–6.
Anema A, et al. Relationship between food insecurity and mortality among HIV-positive injection drug users receiving antiretroviral therapy in British Columbia, Canada. PLoS ONE. 2013;8(5):e61277.
Kelly A, et al. Moresby food isn’t good: food security, nutritional information and adherence to antiretroviral therapy in Papua New Guinea. P N G Med J. 2011;54(1–2):23–34.
Van Dyk AC. Treatment adherence following national antiretroviral rollout in South Africa. Ajar-Afr J Aids Res. 2010;9(3):235–47.
Birbeck GL, et al. Neuropsychiatric and socioeconomic status impact antiretroviral adherence and mortality in rural Zambia. Am J Trop Med Hyg. 2011;85(4):782–9.
Franke MF, et al. Food insufficiency is a risk factor for suboptimal antiretroviral therapy adherence among HIV-infected adults in urban Peru. AIDS Behav. 2011;15(7):1483–9.
Sasaki Y, et al. Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob. 2012;11:34.
Parashar S, et al. Sticking to it: the effect of maximally assisted therapy on antiretroviral treatment adherence among individuals living with HIV who are unstably housed. AIDS Behav. 2011;15(8):1612–22.
Berhe N, Tegabu D, Alemayehu M. Effect of nutritional factors on adherence to antiretroviral therapy among HIV-infected adults: a case control study in Northern Ethiopia. BMC Infect Dis. 2013;13:233.
Sterne JAC, Harbord RM. Funnel plots in meta-analysis. Stata J. 2004;4(2):127–41.
Tirivayi N, Koethe JR, Groot W. Clinic-based food assistance is associated with increased medication adherence among HIV-infected adults on long-term antiretroviral therapy in Zambia. J AIDS Clin Res. 2012;3(7):171.
Serrano C, et al. Family nutritional support improves survival, immune restoration and adherence in HIV patients receiving ART in developing country. Asia Pac J Clin Nutr. 2010;19(1):68–75.
Chesney MA. Factors affecting adherence to antiretroviral therapy. Clin Infect Dis. 2000;30(Suppl 2):S171–6.
Spire B, et al. Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: from a predictive to a dynamic approach. Soc Sci Med. 2002;54(10):1481–96.
Gutierrez EB, et al. Measuring adherence to antiretroviral treatment: the role of pharmacy records of drug withdrawals. AIDS Behav. 2012;16(6):1482–90.
Palar K, et al. Role of antiretroviral therapy in improving food security among patients initiating HIV treatment and care. AIDS. 2012;26(18):2375–81.
Weiser SD, et al. Changes in food insecurity, nutritional status, and physical health status after antiretroviral therapy initiation in rural Uganda. J Acquir Immune Defic Syndr. 2012;61(2):179–86.
McCoy SI, et al. Food insecurity, socioeconomic status, and HIV-related risk behavior among women in farming households in Tanzania. AIDS Behav. 2014;18(7):1224–36.
Riley ED, et al. Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. Am J Epidemiol. 2011;174(5):515–22.
Mugavero MJ, Norton WE, Saag MS. Health care system and policy factors influencing engagement in HIV medical care: piecing together the fragments of a fractured health care delivery system. Clin Infect Dis. 2011;52(Suppl 2):S238–46.
McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26(14):1735–8.
de Pee S, et al. Antiretroviral therapy requires life-long adherence. Lancet Infect Dis. 2012; 12(9):661–662; author reply 662.
Galarraga O, et al. Conditional economic incentives to improve HIV treatment adherence: literature review and theoretical considerations. AIDS Behav. 2013;17(7):2283–92.
McCoy SI. Comparing food and cash assistance for HIV-positive men and women on antiretroviral therapy in Tanzania. 2013 [cited 2014 06/07/2014].
Barnighausen T, et al. Interventions to increase antiretroviral adherence in sub-Saharan Africa: a systematic review of evaluation studies. Lancet Infect Dis. 2011;11(12):942–51.
Grobler L, et al. Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database Syst Rev. 2013;2:CD004536.
Tirivayi N, Groot W. Health and welfare effects of integrating AIDS treatment with food assistance in resource constrained settings: a systematic review of theory and evidence. Soc Sci Med. 2011;73(5):685–92.
Koethe JR, et al. Macronutrient supplementation for malnourished HIV-infected adults: a review of the evidence in resource-adequate and resource-constrained settings. Clin Infect Dis. 2009;49(5):787–98.
Acknowledgments
Ms. Singer acknowledges support from NIEHS R01 ES09137. Dr. McCoy is supported by Award Number K01MH094246 from the National Institute of Mental Health. Dr. Weiser acknowledges support from the Burke Global Health Family Foundation, and NIMH K23 MH079713. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institute of Environmental Health Sciences, or the National Institutes of Health. The funding bodies had no role in the study. We thank Dr. Nancy Padian for helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Full PubMed Search strategy: (“Antiretroviral Therapy, Highly Active”[Mesh] OR “HIV Infections/drug therapy”[Mesh] OR “Anti-HIV Agents/therapeutic use”[Mesh] OR “Acquired Immunodeficiency Syndrome/drug therapy”[Mesh] OR antiretroviral OR HAART OR ART) AND (“Patient Compliance”[Mesh] OR “Medication adherence”[Mesh] OR adherence OR nonadherence OR non-adherence) AND (“Food Supply”[Mesh] OR food OR hunger OR “Socioeconomic factors”[Mesh] OR “risk factors” OR poverty OR barrier OR nutrition OR malnutrition).
Rights and permissions
About this article
Cite this article
Singer, A.W., Weiser, S.D. & McCoy, S.I. Does Food Insecurity Undermine Adherence to Antiretroviral Therapy? A Systematic Review. AIDS Behav 19, 1510–1526 (2015). https://doi.org/10.1007/s10461-014-0873-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0873-1