Abstract
There is growing recognition of the influence of substance use, particularly alcohol use, on HIV disease progression. This study investigated how hazardous/harmful use of alcohol and drugs impacts the health status of 1503 patients attending HIV clinics. Of the sample, 37 % indicated hazardous/harmful drinking and 13 % indicated a drug problem. Hazardous/harmful use of alcohol and drugs was significantly related to health status, with participants using substances more likely to have TB-positive status (χ2 = 4.30, p < 0.05), less likely to be on ARVs (χ2 = 9.87, p < 0.05) and having lower CD4 counts (t = 4.01, p < 0.05). Structural equation modelling confirmed the centrality of hazardous/harmful use of alcohol as a direct and indirect determinant of disease progression. Based on these findings it is recommended that patients attending HIV clinics be routinely screened for problematic alcohol and/or drug use, with strong emphasis on ensuring ARV adherence in those with problematic alcohol use.
Resumen
Existe un creciente reconocimiento de la influencia del consumo de sustancias, en particular el uso de alcohol, en la progresión de la enfermedad del VIH. Este estudio investigó cómo el uso riesgoso/nocivo de alcohol y drogas afecta el estado de salud de 1.503 pacientes que acuden a las clínicas de VIH. De la muestra, el 37 % indicó consumo riesgoso/nocivo y 13 % indicó un problema de drogas. El uso riesgoso/nocivo del alcohol y las drogas estuvo significativamente asociado con el estado de salud, con los participantes que usaron sustancias mostrando mayor probabilidades de tener TB positiva (c2 = 4.30, p < 0.05), menor probabilidad de estar en ARV (c2 = 9.87, p < 0.05) y que tiene más bajos recuentos de CD4 (t = 4.01, p < 0.05). Modelos de ecuaciones estructurales confirmaron la centralidad del consumo riesgoso/nocivo del alcohol como un determinante directo e indirecto de la progresión de la enfermedad. Basándose en estos resultados, se recomienda que los pacientes que asisten a clínicas de VIH se examinan rutinariamente para detectar alcohol problemático y/o el consumo de drogas, con un fuerte énfasis en asegurar la adherencia al ARV en los pacientes con consumo problemático de alcohol.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There are 33.3 million people living with HIV in the world today. South Africa has an estimated 5.6 million HIV-positive people and continues to be the country with the largest epidemic in the world [1]. The overall prevalence rate for HIV in South Africa is estimated at 10.6 % [2]. According to the South African National HIV Prevalence, Incidence, Behaviour and Communication Survey conducted in 2008, the prevalence of HIV across all nine provinces ranged from 3.8 % in the Western Cape, to 5.9 % in the Northern Cape, to 15.4 % in Mpumalanga and 15.8 %, in Kwa Zulu-Natal [3].
Hazardous or harmful alcohol use and/or problematic drug use, like HIV, is another major health challenge facing the country [4]. Although alcohol continues to be the primary and most abused substance in South Africa, in recent years there has been an increase in the use of heroin, cocaine and amphetamine-type stimulants [5], and South Africa had the second highest prevalence of past year substance abuse (5.8 %) compared to the 14 other participant countries in the 2003–2004 World Mental Health Survey [6]. In the Western Cape particularly, there has been an increase in heroin and methamphetamine as primary drugs of abuse. For the reporting period of July –December 2011, 94 % of all admissions in Western Cape treatment centres were for methamphetamine, alcohol, cannabis or heroin [7].
Given the nexus between problematic alcohol and drug use and HIV infection, it is likely that many HIV infected persons are also users of alcohol and/or other drugs and develop abuse and dependence. HIV and substance abuse and dependence interact in complex ways, with each impacting on the other and hindering optimal health, well-being and quality of life [8]. Substance abuse among persons living with HIV can lead to non-adherence to treatment, especially to anti-retroviral therapy. As a consequence, poor adherence may lead to a reduction in the CD4 count (an indicator of the amount of white blood cells that fight infection), vulnerability to opportunistic infections, possible drug resistance, and an earlier onset of death [9].
Furthermore, alcohol abuse was found to impact on different aspects of the immune system and to weaken the natural course and outcome of bacterial and viral infections, thereby increasing the risk of infections. This review also found that alcohol abuse affects the gastrointestinal and respiratory tract immune barriers and compromises the main parts of the innate and adaptive immune systems [10].
A systematic review of the research on the association between alcohol use, alcohol-use disorders and TB concluded that there is a causal link between heavy alcohol use and/or alcohol-use disorders and incidence of TB and likelihood of re-infection [11]. Alcohol use also worsens TB infection, leading to higher rates of defaulting on treatment and possible drug-resistant forms of TB [11].
Several studies conducted outside South Africa have documented high rates of alcohol and drug use and dependence among people who are HIV positive [12–14] but research on the African continent has been limited. A cross-sectional study among HIV patients) at a hospital in Jos, Nigeria, found the prevalence of alcohol- related problems among patients to be 39.4 %, with 28.8 and 10.6 % reporting harmful and hazardous drinking respectively [15]. Similarly, another study among HIV patients in Nigeria (n = 167) found 18.8 % of the patients reporting harmful alcohol use [16].
Only two studies, both conducted in the Western Cape, have investigated the relationship between substance abuse and HIV among PLWHA in South Africa. The first study of 149 HIV positive patients at an infectious disease clinic in Cape Town found 10.1 % of the patients to be alcohol dependent, with 22.7 % of males reporting alcohol dependence compared to 4.7 % of females [13]. The second, a more recent study, found that of the 465 HIV positive patients enrolled for HIV treatment and care at primary health care clinics, 7 % reported alcohol dependence/abuse [12].
The aim of this study was to establish the prevalence of hazardous use of alcohol and drug problems among patients attending a representative sample of HIV clinics in Cape Town and to investigate the role of such substance use in health status and disease progression. More specifically, we sought to:
-
(i)
determine the extent and severity of harmful and hazardous use of alcohol and drug problems,
-
(ii)
establish the relationship between harmful and hazardous use of alcohol and problematic drug use and being on ARVs or not being initiated on ARVs as yet,
-
(iii)
clarify the impact of identified substance use on physical health status and HIV disease progression.
Methods
Sample
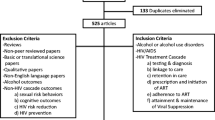
A cross-sectional study design was used. A total of 1503 patients attending HIV clinics in the Cape metropolitan area- greater Cape Town area, South Africa, participated in the study. Patients were initially informed about the study by their ARV counselor or the attending doctor and their participation requested at this information session. Once they agreed to participate they were interviewed by the research team and screened for eligibility (18 years and older and deemed cognitively competent on the basis of the International HIV Dementia Scale). Information on patients was only available to the research team once they had agreed to participate and not prior to this, hence it is unknown how many patients refused to participate at the initial briefing sessions.
All clinics serving HIV patients in the greater Cape Town area were identified and 23 clinics were randomly selected. Of these permission was granted for the study team to access patients from 8 clinics which the City of Cape Town and the Western Cape Province were able to accommodate in the research process. These 8 clinics came from suburbs such as Kraaifontien, Mitchell’s Plain, Heideveld, Mfuleni, Phillipi, and Crossroads and covered a broad spectrum of geographic areas in the Cape Flats, an area where persons from poorer socio-economic backgrounds reside in this city and the majority of whom are Coloured or African.
Instruments
Socio-demographic Variables and Health Characteristics
A brief demographic questionnaire was used to collect information about age, race, sex, occupation, marital status, highest level of education, employment status, family income, date of diagnosis, date of commencement of ARVs, date of diagnosis of tuberculosis (TB) and opportunistic infections. In terms of ARVs, it is important to note that information was only collected on whether or not patients were on ARVs and not on ARV adherence behaviours.
In this study, race included the categories of “white”, “black”, and “coloured”; these terms originate from the apartheid era. They refer to demographic markers and do not signify inherent characteristics. They refer to people of European, African and mixed (African, European and/or Asian) ancestry, respectively. These markers were chosen for their historical significance. Their continued use in South Africa is important for monitoring improvements in health and socio-economic disparities, identifying vulnerable sections of the population, and planning effective prevention and intervention programmes.
The International HIV Dementia Scale (IHDS)
The IHDS was used to screen patients for cognitive impairment. It was used to rule out any HIV-related dementia and to ensure that patients were cognitively competent to further participate in the study. The maximum score is 12 and a score of <10 is indicative of a need for further assessment for dementia [17]. Studies conducted in developed and developing countries report that the IHDS is a useful screening test and has been validated as a sensitive and useful tool in measuring HIV dementia [17, 18].
The Alcohol use Disorders Identification Test (AUDIT)
The AUDIT was developed by the World Health Organisation and is used to screen for hazardous and harmful patterns of alcohol use and alcohol dependence [19] and has been used extensively in South Africa [20–22]. The AUDIT is a 10 item self-rating questionnaire and has been validated for use in primary health care settings and community settings. It is scored as follows: 0–7 indicates abstinence or low-risk drinking; 8–15 is indicative of hazardous drinking patterns; 16–19 indicates harmful levels of drinking and 20–40 indicates possible dependence. Hazardous drinking, as assessed by the alcohol use disorders identification test (AUDIT) is defined as levels of drinking or a pattern of drinking that increases an individual’s risk of harmful consequences and leads to adverse health events. Harmful drinking is defined as higher levels of drinking than hazardous drinking that causes damage physically or psychologically to an individual [19]. A standard drink in South Africa is 12 g compared to 10 g in most European countries and 8 g in the UK. Communal drinking is less common in urban populations. The interviewers were trained to explain to study participants how commonly used drinks containers measured up to a standard drink in South Africa.
The Drug use Disorders Identification Test (DUDIT)
The DUDIT consists of 11 items and is a screening instrument used to identify a list of possible drugs that may be used by a person, the patterns of drug use and various drug -related problems (i.e., substance abuse/harmful use or dependence). To identify men with drug related problems, a cut- off score of 6 or more is needed on the DUDIT, while for women with drug related problems a cut off score of 2 points or more is required. For both genders, a score of 25 or more indicates a high probability of dependence on one or more drugs [23].
Procedures
Participants with no cognitive impairment as assessed by the IHDS were asked to complete the AUDIT and the DUDIT. The AUDIT and DUDIT were administered, on paper by the fieldworkers, in the participant’s language of choice (Afrikaans or Xhosa). All the study questionnaires were previously translated into Afrikaans and Xhosa using the double blind technique. Prior to beginning the study, ethical approval was obtained from the Human Research Ethics Committee of Health Sciences Faculty from the Stellenbosch University.
Data Analysis
All data was analysed using SPSS, version 18. A 95 % confidence interval and a 5 % level of significance were used to interpret statistical significance. All statistical tests were two-tailed. Descriptive analyses (means, standard deviations and frequencies) were used to describe demographic data and clinical characteristics. Bivariate tests of association for categorical variables (χ2 tests) were used to examine associations between substance abuse and gender, opportunistic infections, TB and being on ARVs. Student’s t tests for continuous variables were used to test for group differences in CD4 counts based on categories of substance abuse. Pearson correlations were employed to assess the relationship between CD4 counts and alcohol use. Linear regression analysis was used to test for predictors of CD4 counts and harmful and/or hazardous use of alcohol. Variables entered into the regression models were selected on the basis of evidence from prior research as well as from the bivariate analyses undertaken in this study. The predictor variables were clustered into two groups: socio-demographic variables and clinical characteristics.
To enable proper application of relevant statistical tests the continuous dependent variables were analysed to assess their univariate normality. The results of this analysis revealed some deviation from normality for CD4 count and alcohol use in terms of skewness and kurtosis. However, the actual skewness and kurtosis indices for both variables were less than the recommended threshold value of 2 [24], and hence the deviations were not considered to be significantly different from normal. Accordingly, the variables were applied in the relevant parametric tests.
Following the regression analysis, a structural equation model was developed to examine the direct and indirect determinants of CD4 count. Variables entered into the model were selected on the basis of the bivariate and regression analyses. The following variables were entered into the model as likely predictors: age, gender, education level, alcohol (AUDIT scores), ARVs, opportunistic infections, and TB.
Results
Demographic and Clinical Characteristics
The sample consisted almost entirely of Black (89 %) and Coloured (10 %) participants, reflecting the demographics of the population of PLWHA attending the public health clinics where data collection occurred (Table 1).The mean age of participants was 35.8 years. Most participants were female (70 %), single (63 %), unemployed (66 %), and had some high school education (60 %). Only 1 % had a tertiary education. The monthly income for the majority of the participants (61 %) was less than R1000 ($120) and 37 % earned between R1000 and R5000 ($120–$602) (Table 1).
Cognitive Functioning
All 1503 participants completed the IHDS and were found to be cognitively intact and eligible for the study.
Health Status
The average time between diagnosis of HIV and data collection was 3.7 years (SD = 3.1). The mean for current CD4 counts was 305.3 (SD = 193.7, N = 1478) and the CD4 nadir (lowest CD4 counts in the past 12 months) was 265.3 (SD = 178.1, N = 1467). The majority of participants (1336; 89 %) were on ARVs. 184 (12.2 %) were diagnosed with TB, and 175 (12 %) reported having an opportunistic infection at the time of data collection.
AUDIT and DUDIT
All participants completed the AUDIT and DUDIT. Of these 10 % scored between 0 and 7 indicating low risk drinking or abstinence; 33 % scored between 8 and 15 indicating hazardous drinking patterns, while 20 % scored between 16 and 19 indicating harmful levels of drinking. Over a third (37 %) scored between 20 and 40 indicating possible dependence (Table 2).
Thirteen percent of all respondents scored above the respective cut-off points on the DUDIT (≥2 for females and ≥6 for males) for a drug related problem (Table 2).There was a statistically significant relationship between gender and problematic drug use (χ2 = 43.185, p ≤ 0.05). More males (26 %) reported having a drug problem than females (7 %).
Hazardous and Harmful use of Alcohol and/or Problematic Drug use, Demographic Characteristics and Health Status
There was a significant relationship between hazardous and harmful use of alcohol and/or problematic drug use and gender (χ2 = 95.176, p < 0.05). More than half of males reported hazardous and harmful use of alcohol and/or problematic drug use compared to only a third of females. There was no significant relationship, however, between hazardous and harmful use of alcohol and/or problematic drug use and opportunistic infections (χ2 = 0.831, p > 0.05). There was a statistically significant relationship between hazardous and harmful use of alcohol and/or problematic drug use and TB status (χ2 = 4.308, p < 0.05). Of all participants who had TB, 87 (14 %) reported hazardous and harmful use of alcohol and/or problematic drug use, compared to 97 (11 %) participants that did not have an alcohol and/or drug problem (Table 3).
To examine the socio-demographic determinants of hazardous and harmful use of alcohol, a multiple linear regression analysis was conducted. The results revealed that the overall model was statistically significant (F = 19,723 p < 0.00). Age (β = −0.05, t = −2.06, p < 0.05), gender (β = −0.23, t = −8.99, p < 0.01) and education (β = −0.06, t = −2.26, p < 0.05) were found to be statistically significant determinants of hazardous and harmful use of alcohol. Multiple regression analysis was not conducted with the DUDIT as the number of patients reporting problematic drug use was too small to permit such multivariate analysis.
Hazardous and Harmful use of Alcohol and/or Problematic Drug use and CD4 Count
There was a significant relationship between CD4 count and hazardous and harmful use of alcohol and/or problematic drug use. Patients reporting hazardous and harmful alcohol use and/or problematic drug use had a lower CD4 count than patients reporting no alcohol or drug problems (t = 4.018, p < 0.05).There was also a significant relationship between CD4 count and gender. Females had a higher CD4 count than males (t = −5.324, p < 0.05). A significant negative correlation between AUDIT scores and CD4 counts was also noted with the AUDIT scores of patients increasing as their CD counts deceased (r = −0.114, p < 0.05).
To examine the socio-demographic and clinical determinants of CD4 count, a multiple linear regression analysis was conducted. The results revealed that the overall model was statistically significant (F = 5.772, p < 0.05). Age (ß = 0.10, t = 2.26, p < 0.05), gender (ß = 0.11, t = 2.60, p < 0.01), opportunistic infections (ß = 0.08, t = 1.97, p < 0.05) and duration of HIV (ß = 0.22, t = 5.47, p < 0.01) were found to be statistically significant determinants of CD4 count regardless of education level and hazardous and harmful use of alcohol (Table 4).
Hazardous and Harmful use of Alcohol and/or Problematic Drug use and ARVs
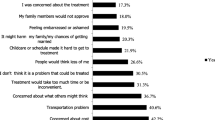
Hazardous and harmful use of alcohol and/or problematic drug users were more likely not to be on ARVs (14.2 %) compared to participants without an alcohol and/or drug problem (9.0 %) (χ2 = 9.877, p < 0.05). There was no significant relationship between gender and whether or not participants were on ARVs.
Factors Influencing CD4 Counts
Based on the bivariate and multiple regression analyses a structural equation model (SEM) was specified as illustrated in Fig. 1. The results of the SEM analysis revealed no residual errors and no data problems with the measurement model, thereby permitting use of the model indices and interpretation of the model results. The output indicated that the structural model provided a good fit to the data, as indicated by the following indices: Comparative fit index = 0.95, root mean square of error approximation (RMSEA) = 0.035 and χ2 df of 2.85 (χ2 = 31.3, df = 11). Furthermore, the Lagrange Multiplier Tests outputs confirmed the validity of the good fit indices and indicated that no further modifications were necessary for the model.
A number of significant direct predictive pathways were identified in the SEM. Firstly, gender was determined to be significant in predicting harmful and hazardous use of alcohol (ß = −0.22, p < 0.01). This reflects the fact that males are more likely to have higher scores on the AUDIT. Gender was also found to be a significant in direct predictor of CD4 counts (ß = 0.12, p < 0.01). Males had lower current CD4 counts than females, possibly indicating greater progression of HIV disease.
Secondly, whether or not participants were on ARVs was found to be significant in predicting current opportunistic infections (ß = −0.15, p < 0.00). Participants on ARVs were less likely to have opportunistic infections than those not on ARVs. Thirdly, harmful and hazardous use of alcohol significantly predicted whether or not participants were currently on ARVs (ß = 0.11, p < 0.01). Participants with higher scores on the AUDIT were less likely to be on ARVs. Fourthly, education had a direct role in predicting hazardous and harmful use of alcohol (ß = −0.06, p < 0.05). Participants with lower levels of education were more likely to score higher on the AUDIT. Hazardous and harmful use of alcohol had a direct role in predicting TB (ß = −0.04, p < 0.05). Participants with high scores on the AUDIT were more likely to have TB.
CD4 counts was found to have a number of significant direct predictors. Firstly, TB status was found to be an important determinant of CD4 counts (ß = 0.10, p < 0.01), with participants with TB registering significantly lower CD4 counts than those without TB. Similarly, age and gender were also direct determinants of CD4 counts, with males being more likely to have lower CD4 counts and older patients being more likely to have higher CD4 counts. Finally, harmful and hazardous use of alcohol was found to have a direct relationship to CD4 counts (ß = −0.07, p < 0.05), with participants scoring higher on the AUDIT being more likely to have lower CD4 counts. The last result is particularly noteworthy as problematic alcohol use was not found to be a significant direct predictor of CD4 counts in the regression analysis. The change in significance for this direct relationship from the regression model to the SEM is directly attributable to the fact that while the regression is only able to examine direct effects on the outcome variable, the SEM is able to examine both direct and indirect effects. Hence while accounting for the various indirect effects on CD4 counts by the other variables in the SEM (including that for problematic alcohol use), it was determined that problematic alcohol also has a significant direct impact on CD4 counts. No significant direct relationships were found between ARV and CD4 counts, opportunistic infections and CD4 counts.
Discussion
The results indicate that hazardous and harmful use of alcohol is a statistically significant and important determinant of lower CD4 counts, TB positive status and the likelihood of patients being on ARVs.
Hazardous and harmful use of alcohol also has an indirect influence on CD4 counts which was mediated by TB. It should be noted that the influence of alcohol on CD4 counts (both directly and mediated through TB) is in and of itself influenced by the level of education and gender of the patient. Hazardous and harmful use of alcohol also had an indirect effect on opportunistic infections but was mediated by whether or not the patient was on ARVs.
The prevalence of hazardous and harmful use of alcohol (37 %) and problematic drug use (13 %) are higher than that documented in other studies of patients attending HIV clinics in South Africa and sub-Saharan Africa [12, 13, 16]. A possible explanation for this high prevalence is that South Africa has one of the highest levels of per capita consumption per drinker globally. It was also identified as having one of the highest levels of heavy episodic drinking among men and women globally and one of the most negative ratings in Africa on an index measuring harmful patterns of drinking [25]. Furthermore, the difference in alcohol use could be partly due to differing measurement approaches used in the studies.
More than half of the males in this study reported hazardous and harmful alcohol and problematic drug use, which is consistent with other similar studies [12, 13]. Gender was also found to be important in that women are more adept at taking care of their health than are men. Similarly, age has been found to be a significant factor in determining health status, with older people more likely than younger people to take better care of their health through better lifestyle, nutrition and behavioural choices.
Our finding that 13 % of patients had a drug related problem is comparable to a previous study which found that 9 % of HIV infected persons reported drug dependence in the past 12 months while 10 % reported drug abuse [26]. Drug use related factors have been found to be a barrier in using ARVs in this population.
In the present study, hazardous and harmful use of alcohol was also found to be a direct determinant of TB status. Studies in India found that almost a quarter of TB patients consumed alcohol and an equal number were hazardous drinkers. These patients were reported to be non-adherent to their TB medication [27, 28]. Alcohol use also worsens TB infection, leading to higher rates of defaulting on treatment and possible drug-resistant forms of TB. HIV-positive patients co-infected with TB and abusing substances can complicate their medical care and treatment [11].
The harmful and hazardous use of alcohol in predicting lower CD4 counts found in this study is consistent with a study that found frequent alcohol use is a predictor of a decline in CD4 counts in participants who were on ART and in those who were ART naive [29]. These findings that frequent alcohol use has a direct effect on low CD4 counts independent of ARV status is similar to the findings of our study.
The relationship between lower CD4 counts and hazardous and harmful alcohol and problematic drug use is clinically important because of the (already) compromised immune system of HIV positive individuals is significantly further compromised by the use of drugs and alcohol. These findings are consistent with documented poorer immunologic and virologic outcomes commonly associated with alcohol use disorders [30].This is further confirmed by the findings of the present study that harmful and hazardous use of alcohol has an indirect effect in predicting opportunistic infections, mediated by whether participants are on ARVs or not.
The study had a number of limitations that deserve mention. Firstly, the sample of was drawn from the Cape Metropolitan area and may not be representative of the HIV treatment seeking population across South Africa in terms of patterns of substance use and TB infection. Secondly, alcohol and drug use was measured by self-reports and not confirmed by laboratory testing for alcohol and drug abuse. However, it should be noted that a pilot study among PLWHA comparing self-report alcohol and drug use with urine and hair tests reinforced the value of self-report data on alcohol and drugs [31].Thirdly, only cross-sectional data was collected and this weakens any causal attributions being made regarding the effect of hazardous and harmful use of alcohol on health and other outcomes of PLWHA. Fourthly, a larger sample size of participants who have problematic drug use is needed to undertake multivariate analysis investigating drug use as predictor variable.
Based on the findings of this study, the screening patients attending HIV clinics to assess the level of problematic alcohol and/or drug use and to advise accordingly is strongly recommended. When using the AUDIT as a screening instrument, patients who score between 0 and 7 are low risk drinkers and require simple education on alcohol use. Patients who score between 8 and 15 need advice on the reduction of hazardous drinking, while patients who score between 16 and 19 require advice plus brief counselling and continued monitoring of their drinking. Patients who score between 20 and 40 are at risk of possible dependence and require referral to a specialist for diagnostic evaluation and treatment [19]. In addition, treatment providers should also inquire about drug use and polydrug use before prescribing ARVs [32]. Alcohol- related issues should form part of HIV treatment and prevention and the effects of alcohol on the immune system, on adherence to medication and sexual risk behaviour should be addressed [33].
It is recommended that there be an integration of alcohol, HIV and TB services at the primary care level in community-based settings so that patients can be treated at one facility. The need for screening of TB patients for alcohol use is highlighted by studies conducted in Chennai, India that found almost a quarter of TB patients could be diagnosed with an alcohol use disorder. This study emphasised the urgency of alcohol screening and the need for early intervention in such a population at all levels from the initiation of treatment through to management and follow-up [27, 28].
The implementation of such an intervention is likely to be challenging given the poor resources available in the country and the demands on health personnel. Additional interventionist would need to be employed and staff should be cross-trained in conducting routine screening of alcohol and drug use and TB in PLWHA and to refer appropriately in all these areas [33].
In addition further research to inform guidelines to such an intervention needs to be conducted. At a technical meeting on alcohol and infectious diseases in Cape Town in 2012, addressing research in this area was identified. Firstly, baseline information on patterns of drinking, risky HIV-sexual behaviours and information on treatment and adherence to ARVs and TB medication is required among HIV and TB patients. Secondly, randomised control trials (RCTs) are needed to evaluate alcohol focused-interventions that are evidence-based on reducing the risk of uninfected people acquiring HIV. Thirdly, RCTs evaluating evidence-based alcohol-focused interventions among persons initiating treatment for HIV and/or TB and their adherence to treatment is required [34].
Finally, more intervention studies are needed in South Africa, specifically a comparison of brief interventions vs. more long-term intensive interventions that address problems related to alcohol use and non-adherence as well as exploration of cost and feasibility issues in the treatment of PLWHA [33].
Conclusion
Problematic alcohol and other drug use among PLWHA is associated with poorer health outcomes such as non-adherence to treatment, reduction in CD4 count, opportunistic infections, possible drug resistance, toxic effects of alcohol/drug interactions with medications to treat HIV and opportunistic infections and an earlier onset of death [9]. Our findings highlight the importance of an integrated treatment model for PLWHAs co-infected with TB and abusing substances in South Africa. Untreated substance abuse in this population may result in HIV treatment being less effective owing to compromised adherence and ongoing risk behaviour. With almost two million South Africans now receiving ARVs this is an issue that requires urgent attention.
References
UNAIDS: Report on the global AIDS epidemic 2010 Available at: http://www.unaids.org/globalreport/Global_report.htm (2010). Accessed 18 April 2013.
Department of Health. National Antenatal Sentinel HIV and Syphilis Prevalence in South Africa, 2009. Pretoria: Department of Health; 2010.
Shisana O, Rehle T, Simbayi LC, et al. South African National HIV prevalence, incidence, behaviour and communication survey 2008: A turning tide among teenagers? Cape Town: HSRC Press; 2009.
Townsend L, Rosenthal SR, Parry CDH, Zembe Y, Mathews C, Flisher AJ. Associations between alcohol misuse and risks for HIV infection among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Care. 2010;22(12):1544–54.
Parry CDH, Pithey AL. Risk behaviour and HIV among drug using populations in South Africa. Afr J Drug Alcohol Stud. 2006;5(2):140–57.
Herman AL, Stein DJ, Seedat S, Heeringa SG, Moomal H, Williams DR. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. S Afr Med J. 2009;99(5):339–44.
Dada S, Plüddemann A, Parry C et al. Monitoring alcohol and drug abuse trends in South Africa (July 1996–December 2011). SACENDU Research Brief, 2012; 15(1): 1–15. Medical Research Council of South Africa.
Barroso J, Sandelowski M. Substance abuse in HIV positive women. J Assoc Nurses AIDS Care. 2004;15(5):48–59.
Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52:180–202.
Molina PE, Happel KI, Zang P, Kolls JK, Nelson S. Focus on: alcohol and the immune system. Alcohol Res Health. 2010;33(1):97–108.
Rehm J, Samokhvalov AV, Neuman MG, et al. The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health. 2009;9:450. doi:1186/1471-2458-9-450.
Myer L, Smit J, Le Roux L, Parker S, Stein D, Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care and STDs. 2008;22(2):147–58.
Olley BO, Gxamza F, Seedat S, et al. Psychopathology and coping in recently diagnosed HIV/AIDS patients-the role of gender. S Afr Med J. 2003;93(12):928–31.
Freeman M, Nkomo N, Kafaar Z, Kelly K. Mental disorders in people living HIV/Aids in South Africa. S Afr J Psychiatry. 2008;38(3):489–500.
Goar SG, Audu MD, Agbir MT, Dochalson. Prevalence and socio-demographic correlates of alcohol use disorders among HIV patients. Afr J Drug Alcohol Stud. 2011;10(11):11–6.
Yunusa MA, Obembe A, Ibrahim T, Njoku CH. Prevalence and specific psychosocial factors associated with substance use and psychiatric morbidity among patients with HIV infection at Usmanu Danfodiyo University Teaching Hospital, Sokoto State, Nigeria. Afr J Drug Alcohol Stud. 2011;10(1):11–6.
Sacktor NC, Wong M, Nakasujja N, et al. The International HIV Dementia Scale: a new rapid screening test for HIV dementia. AIDS. 2005;19:1367–74.
Berghuis JP, Uldall KK, Lalonde B. Validity of two scales in identifying HIV associated dementia. J Acquir Immune Defic Syndr. 1999;21(2):134–40.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. 2nd ed. Geneva: World Health Organization Department of Mental Health and Substance Dependence; 2001.
Peltzer K, Davids SA, Njuho P. Alcohol use and problem drinking in South Africa: findings from a national population-based survey. Afr J Psychiatry. 2011;14:30–7.
Peltzer K, Naidoo P, Matseke G, Zuma K. Screening and brief interventions for hazardous and harmful alcohol use among patients with active tuberculosis attending primary care clinics in South Africa: a cluster randomized controlled trial protocol. BMC Public Health. 2011;4(11):394–402.
Julia L, Peltzer K, Matseke G. Prevalence of alcohol use and associated factors in pregnant antenatal care attendees in Mpumalanga, South Africa. J Psychol Afr. 2011;21(4):567–72.
Berman AH, Bergman H, Palmstierna T, Schlyter F. DUDIT manual the drug use disorders identification test. London: Karolinska Institutet Department of Clinical Neuroscience; 2005.
Field A. Discovering statistics using SPSS. 3rd ed. London: SAGE Publications Ltd; 2009.
Global Status report on alcohol and health 2011. Geneva: World Health Organization. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/en/ Accessed 18 April 2013.
Turner BJ, Fleishman JA, Wenger N, et al. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. J Gen Intern Med. 2001;16(9):625–33.
Thomas B, Suhadev M, Mani J, et al. Feasibility of an alcohol intervention programme for TB patients with alcohol use disorder (AUD)—a qualitative study from Chennai, South India. PLoS One. 2011;6(11):e27752.
Suhadev M, Thomas BE, Sakthivel R, et al. Alcohol use disorders (AUD) among tuberculosis patients: a study from Chennai, South India. PLoS One. 2011;6(5):e19485.
Azar MW, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112:178–93.
Malta M, Magnanini MMF, Strathdee SA, Bastos FI. Adherence to antiretroviral therapy among HIV-infected drug users: a meta-analysis. AIDS Behav. 2008. doi: 10.1007/s10461-008-9489-7.
Kader R, Seedat S, Koch JR, Parry CDH. A preliminary investigation of the AUDIT and DUDIT in comparison to biomarkers for alcohol and drug use among HIV-infected clinic attendees in Cape Town, South Africa. Afr J Psychiatry. 2012;15:346–51.
Peretti-Watel P, Spire B, Lert F, Obadai Y. The Vespa Group. Drug use patterns and adherence to treatment among HIV-positive patients: evidence from a large sample of French outpatients (ANRS-EN 12-VESPA 2003). Drug Alcohol Depend. 2006;82(1):71–9.
Parry CDH, Rehm J, Morojele NK. Is there a causal relationship between alcohol and HIV? Implications for policy, practice and future research. Afr J Drug Alcohol Stud. 2010;9(2):81–91.
Parry CDH, Ferreira-Borges C, Poznyak V, Lonnroth K, Rehm J. The international study on alcohol and infectious diseases: three priorities for research. Addiction. 2012;108:1–2.
Acknowledgments
This research has been supported by the US President’s Emergency Fund for AIDS Relief (PEPFAR) through the US Centers for Disease Control and Prevention (CDC), under the terms of Co-operative agreement grant number 5U2GPS001137. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or PEPFAR. The authors would also like to acknowledge Carlos Toledo at the CDC in Pretoria for his technical support and encouragement throughout the project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kader, R., Seedat, S., Govender, R. et al. Hazardous and Harmful use of Alcohol and/or Other Drugs and Health Status Among South African Patients Attending HIV Clinics. AIDS Behav 18, 525–534 (2014). https://doi.org/10.1007/s10461-013-0587-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0587-9