Abstract
This study explores the sexual behavior of 27 men who have sex with men (MSM) who regularly engage in unprotected anal intercourse (UAI), in the context of HIV home test (HT) use with potential sex partners. Participants were given 16 HT kits to use over 3 months. Among 40 sexual occasions following HIV-negative HT results, there were 25 UAI occasions (16 based on not typically using condoms and nine on HT results), 15 occasions in which condoms were used, and three in which sex did not occur. In the seven occasions where a potential partner received HIV-positive HT results, the sexual encounter ended. Almost all participants encountered potential partners who refused HT. Over half of these participants ended sexual encounters when HT was refused, perceiving these partners as HIV-positive or too high risk. Some participants reported that HT use heightened their awareness of HIV risk and their commitment to reducing it.
Resumen
El artículo examina la conducta sexual de 27 hombres que tienen sexo con hombres (HSH) y que regularmente practican el coito anal desprotegido, en el contexto del uso del examen casero rápido (ECR) con parejas sexuales potenciales. Los participantes recibieron 16 unidades del ECR para usarlas con sus parejas sexuales durante tres meses. De los 40 encuentros sexuales que ocurrieron después de obtener resultados negativos para VIH con el ECR, 25 resultaron en coito anal desprotegido (16 basadas en la falta rutinaria del uso de condones y nueve basadas en el resultado del examen); y en 15 ocasiones se utilizaron condones. En tres ocasiones no hubo contacto sexual. Casi todos los participantes encontraron parejas potenciales que se negaron a usar el ECR. Más de la mitad de esos participantes pusieron fin al encuentro sexual cuando la pareja potencial se negó a usar el ECR, ya que percibieron a estas parejas como VIH-positivas o como demasiado riesgosas. Algunos participantes informaron que el ECR aumentó su conciencia del riesgo para VIH y sus intenciones de reducirlo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies have shown that sexual decision making regarding whether or not to engage in sex, sexual role (i.e., insertive or receptive), and condom use are influenced by the partners’ relative characteristics. These can include the partner’s age, masculinity/femininity, physical attractiveness, and other physical characteristics such as height, skin tone, and penis size [1–5]. Thus, for example, men who are shorter, slighter in build, and smaller in penis size compared to their partner may be expected to assume a receptive role during sex, while those who are older, darker skinned, taller, and with a larger penis may be expected to assume an insertive role [1–3]. Furthermore, these characteristics may also influence decisions about condom use [5–8].
HIV status is another important factor in sexual decision making. Serosorting, selecting sexual partners based on seroconcordance, is used to guide decisions as to whether or not to engage in sex with a potential partner, use condoms, or engage in sexual practices that put partners at lower risk of HIV infection [9]. However, studies have also shown that there is little discussion about HIV status with potential partners and serosorting is often based on assumptions [9–11]. In a study of HIV-negative MSM who regularly engage in bareback sex, Balán et al. [12] found that serosorting was the most frequently cited HIV risk-reduction approach used by the participants. However, most participants used indirect ways of assessing serostatus (e.g., appearance or online profile), and only one-third reported asking sexual partners directly about their HIV status. In the absence of clear knowledge of a partner’s serostatus the assumption is often made that the partners are seroconcordant [9–11], which could result in increased HIV risk behavior [10].
With the recent FDA approval of a rapid HIV home test (HT) for over-the-counter sale, an HT could be used by sexual partners to test each other prior to engaging in sex. This would provide users with a more accurate assessment of their partner’s HIV status upon which to base their sexual decision making. Using HT with sexual partners is acceptable among MSM who frequently engage in UAI with multiple partners [13, 14]. In a recently published study, [14] participants (n = 27) proposed using HT with approximately 124 sexual partners, of whom 101 accepted. Testing was often mutual, with the participant testing himself with each new partner to encourage HT use by the partner. Overall, participants experienced very few problems using HT and expressed a strong desire to continue using HT and for its over-the-counter availability. One drawback of HT, however, is that like most antibody tests the window period can range from 25 days to 8 weeks on average [15]. Thus, HT is unable to detect recent infections, which coincides with a period of high infectiousness for those who have been recently infected with HIV [16, 17]. As such, users may overestimate its effectiveness in identifying HIV positive partners and, as a result, place themselves at greater risk of HIV infection. Similar concerns have been expressed in relation to microbicides [18, 19], circumcision [20, 21], pre- and post-exposure prophylaxis [18, 19, 22–26], and a future HIV vaccine [27, 28]. Understanding how HT use can affect sexual decision making is essential now that this product is available for over-the-counter purchase.
This manuscript explores sexual behavior in the context of HT use among the 27 MSM previously mentioned [14]. Because these men regularly engage in UAI, this manuscript focuses on: (1) How does an HIV-negative HT result affect condom use decisions among these men? (2) How do HIV-positive HT results affect subsequent sexual behavior? and (3) How does the refusal of HT by a potential partner affect subsequent sexual behavior?
Methods
Recruitment
Prior to initiating participant recruitment, the study was reviewed and approved by the Institutional Review Board of the New York State Psychiatric Institute. Study candidates were recruited in the New York City metropolitan area either in person or via Web sites using an advertisement indicating that researchers were studying possible uses of a rapid HIV home test. Those interested in participating were asked to call the research office.
Pre-screening
A brief pre-screening questionnaire was administered to study candidates over the phone or at recruitment venues. The purpose of the pre-screening was to identify MSM at high risk of HIV infection who were willing to use an HT with sexual partners. Candidates were excluded if, by self-report, they were HIV-positive, did not have any male partners; were in a monogamous relationship; not interested in using an HT with sexual partners; engaged in receptive anal intercourse (RAI) less than three times per month; or used condoms on more than 20 % of their RAI occasions. RAI-related eligibility criteria were assessed by asking the participant for the total number of RAI partners and occasions during the past 3 months and the number of those occasions in which a condom was not used. Screening staff then calculated whether the sexual behavior criteria were met. Those who qualified were invited to a full screening interview at the study office.
Full Screening
The purpose of the full screening was to confirm that potential participants were HIV negative; understood the limitations of HT and could use it correctly; and felt they could handle potentially violent situations.
Men who attended the full screening (Visit 1) underwent a consent process and were given a detailed explanation about HT, how it worked, and its window-period-related limitations. They then completed a computer-assisted self-interview (CASI) which included sections on demographics, sexual behavior, knowledge of HT, substance use, and degree of comfort in handling potentially violent situations with partners. They were then given written instructions on how to use an OraQuick ADVANCE® Rapid HIV-1/2 Antibody Test kit and, to assess their ability to use the HT, were asked to test themselves while monitored by a researcher. Negative results were confirmed using Clearview® Complete HIV-1/2, a blood-based rapid test.
To enter into the study, candidates who attended Visit 1 needed to: be HIV-negative on both tests; confirm that they engaged in RAI at least three times per month and used condoms infrequently (no condom use in last 10 occasions for those with 4 or fewer partners or in less than 80 % of occasions for those with more than 4 partners in the past year) based on data they entered into CASI; be aware that unprotected RAI may lead to HIV transmission; report that they were likely to use HT to screen potential sexual partners; understand the window period of OraQuick®; and feel they could avoid or handle potential violence resulting from proposing the use of the test to a partner.
Study Participation
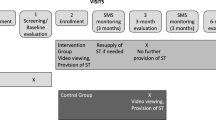
Study candidates who met the eligibility criteria returned to the research offices for Visit 2 on a subsequent day. After completing a new consent process, they entered the 3-month study. They received condoms, a bag containing 16 HT kits, written instructions on how to use the kit, a card with HIV- and violence-related community resources, the study Web site address, and a 24-h hotline number they could call for assistance. They were also asked to call into an interactive voice response system (IVRS) at least weekly to report their sexual behavior and HT use.
Follow-up Interview
Three months after Visit 2, participants attended Visit 3, during which they underwent an in-depth interview with a clinical psychologist that explored the participants’ experiences in using (or not using) HT with sexual partners. During the interviews, participants were asked to discuss three experiences using HT with sexual partners, which could include situations where a sexual partner refused to be tested. As part of relaying these experiences, participants were asked to sequentially describe bringing up HT, using HT, and what happened after HT results were obtained, including subsequent sexual behavior and whether condoms were used. At a later point in the interview, participants were asked how HT use affected their overall HIV risk behavior.
Incentives
Participants received incentives of $30 per visit for completing Visits 1 and 2, and $70 for completing Visit 3. They also received $1 per call to the IVRS up to a maximum of $10 per month for a subtotal of $30 for the 3 months, plus a bonus of $10 for every month in which a report was made at least weekly. The total compensation could reach $190.
Data Analyses
Quantitative CASI data were analyzed using SPSS to calculate descriptive statistics. In-depth interviews were recorded, transcribed, and verified for accuracy. Repeated reading of transcripts by a team of four researchers led to the identification of the main themes that constituted the base for codebook development. Each code was then defined with inclusion and exclusion criteria, including examples. All transcripts were double-coded, and discrepancies discussed until consensus was reached. Through data coded under “Effects of HT on sexual behavior,” which included data specific to a sexual encounter as well as overall effects on sexual behavior, we identified a total of 40 specific sexual encounters following HIV-negative HT results. We then categorized these encounters as to whether condoms were not used, condoms were used, or no sex occurred. To explore sexual behavior following an HIV-positive HT result, data from this coding report were supplemented by a review of all the sexual encounters described by participants where a partner received HIV-positive results. To explore sexual behavior following HT refusal by a potential partner, data from this report was supplemented by data from a separate code (“HT Refusal”), which included references to sexual behavior following HT refusal. Text within each area of study was reviewed to identify modal responses and cases that contradicted the main trends as well as quotes to be included in the text. Quoted text has been edited for clarity and readability without compromising the integrity of the content. The quotes are followed by the participant’s identification number, age, and race/ethnicity.
Results
Participant Characteristics
As per Table 1, the mean age of the participants was 34 years, and the mean income was approximately $20,000. Approximately 60 % of participants were non-White and 75 % had not completed college; one-third had a high school education or less. Participants had a mean of 15 sexual partners during the previous 3 months, with approximately 14 occasions of RAI and 12 occasions of insertive anal intercourse (IAI). On average, 74 % of RAI and 78 % of IAI occasions were without condoms (see Table 2).
Sexual Behavior Following HIV-Negative HT Results
Participants reported sexual behaviors following HIV-negative HT results, categorized by instances where condoms were not used (n = 25), condoms were used (n = 15), and no sex occurred (n = 3). Approximately half the participants had experiences across categories. Below, we provide examples of the experiences reported by participants across these three sub-categories.
Decision to Not Use Condoms
Participants attributed 16 of the 25 occasions in which they did not use condoms following HIV-negative HT results to their typical practices and nine occasions to HT results.
Among participants who attributed not using a condom following HIV negative test results to their typical behavior, HT was not reported to have contributed to the decision forgo condom use, but participants felt that it provided added assurance that the partner was not HIV positive. This was often the case when HT was used with ongoing partners. However, some participants also reported that they typically do not use condoms even with casual partners. In these instances, HT appeared to diminish, but not eliminate concerns about a partner’s HIV status.
- Participant (P):
So he came back negative, and then yeah, we got together and went further.
- Interviewer (I):
And with that partner, was it with condoms or without condoms?
- P:
Without condoms.
- I:
And how did the test affect that decision?
- P:
To be honest, I don’t ever wear condoms. So it was just kind of—a situation that I should kind of really think about, but it’s always a lot better when you find out that they’re negative and things like that.
(#1013; 18, White).
- I:
And with this guy, the one you were telling me about, he turned out to be negative. So how did that affect the sex?
- P:
It was—I mean it was still great. I mean he’s an ongoing partner, so it was just like just the thought and knowing that you know, that he’s fine, he’s clean. You know, we could have sex with no condoms no more, so it was cool.
(#1030; 26, Hispanic).
- I:
[You had sex] without condoms with him. How was that experience for you compared to when you haven’t used a test?
- P:
I would have just had sex with him without thinking about it, even without asking. So whereas you know, with the test, if he would have said no, I probably wouldn’t have sex with him even though I probably would have (laughter) if we didn’t have the test, so. I guess it just made me think more than anything.
- I:
What do you mean?
- P:
It made me think about whether a person’s negative or positive or –.
- I:
Just the fact that you’re kind of engaging in this discussion.
- P:
Right, right. Because normally I just– I guess don’t worry about it or whatever.
(#1050; 28, African-American).
In nine of the occasions, the participant specifically attributed the decision to forgo condom use to HIV-negative HT results. When looking back over the 3-month study period, some of these participants also concluded that they had engaged in more UAI while using HT. These participants believed that less risk was involved because of the HIV-negative HT result.
- I:
So you have sex while you’re waiting, and you said that was with condoms. Then you get the results. And then what happens after?
- P:
So then, I was just like, look, you’re good, so let’s just keep going at it, then no condoms, and then I took the condoms off, and we did it for like another hour or 2 h.
(#1016; 43, White).
- P:
Oh, but [name], the guy who I let test himself, once he tested himself, we had sex again. Oh my God, no condom. Like you know, I fucking love the test.
(#1024; 24, Other).
- I:
Did in it any way make you be riskier?
- P:
Yeah. I have unprotected sex, yeah. ‘Cause before this, I was having unprotected, but a lot of times using a condoms at the same time, too. But this time, it was making me have a lot more unprotected sex. Since I had the test, and the test was telling me you’re negative, I’m having unprotected sex with you, you know. But even though I know there’s a window period, and you could be infected at the time, right? Yeah, but the risk is I’m having a lot of unprotected sex, a lot more.
- I:
OK. You also mentioned at some point using condoms with some guys. Were those guys that you tested, or guys that you didn’t test?
- P:
No, guys I didn’t test.
(#1014; 25, African-American).
Decision to Use Condoms
There were 15 instances in which participants reported using condoms even after obtaining HIV-negative HT results. Three main themes emerged from these men: heightened awareness of HIV risk, concerns about the window period, and distrust of the sexual partner. Some of these participants recognized that in similar sexual encounters they might have engaged in UAI even without HT. One participant (32-years-old, Hispanic) also mentioned that his sexual partners wanted to use condoms after HIV-negative HT results.
- I:
And with him, were you using condoms or no condoms?
- P:
Condoms. Yeah, before I used to not use condoms. Now since this whole process, I’ve been using condoms now.
- I:
And so what do you think that’s about?
- P:
I just want to play it safe. I don’t want to catch nothing, ya know?
- I:
So how do you think that using this test affected your sexual behavior, the things you did with guys?
- P:
It affected it in a good way. Just start using it, being protected, more knowledgeable of what to do when I’m having sex with somebody.
(#1032; 25, African-American).
- P:
We talked some more about his feelings about unprotected sex and how you have to be very careful and the likelihood that you can get infected, especially him being so young and everything. The tests came back negative. We used condoms anyway. Couple days later, we went for the test together [at a testing site].
(#1017; 47, White).
Although concerns about the window period were mentioned by most of the participants in the study, this issue seemed particularly important to these participants, possibly due to the increase in HIV risk awareness they experienced by using HT.
- I:
Yeah, it’s interesting because even though you were getting negative results—
- P:
Yeah, I was still using condoms. Sometimes it might not show up, there’s the window period. You understand what I’m saying?
- I:
Yeah. But it’s great, you really kind of kept that in your head. Like some people were like, “Oh, screw the window period.” But you really –.
- P:
It’s real, it’s real.
(#1032; 25, African-American).
Other factors that contributed to using condoms after an HT negative result were concerns about the appearance of the sexual partner, circumstances around the sexual encounter, or the partner’s hesitation to be tested.
- I:
So there’s folks who you tested, and you still used condoms. Tell me about that.
- P:
There are some people that I don’t fully trust, frankly. The guy who was from the bar, I don’t know, I don’t trust what you told me. You could have slept with someone earlier that day. You know, you said, Oh, I’m not really screwing around right now. I don’t know that.
(#1015; 33, White).
- I:
People like this guy–that you might have met and you might not have known a long time. Are those people that you always use with condoms or sometimes use condoms with or —
- P:
No, I usually don’t use condoms.
- I:
So you usually don’t use condoms even with –.
- P:
Hook-ups.
- I:
With hook-ups, okay. So then…what do you think made you use a condom with this guy, given that you don’t usually do it, and he had a negative HIV test?
- P:
I don’t know. I just felt like he, maybe he had something or have something. (laughter) I mean, you know, other STDs or whatever. So I just—he just didn’t sit right with me, I guess, for whatever reason.
(#1050; 28, African-American).
Decision Not to Proceed With Sex
There were only three instances reported by participants in which there was no sex following HIV-negative HT results. In all of these instances, there appeared to be an ebbing of the sexual dynamic between the partners, in two of the occasions as a result of negotiating HT use.
- I:
So what happened afterwards?
- R:
I don’t know if it was the liquor and stuff that I was speaking with him about, but after that I was like, “Let’s order pizza” because I wanted him gone because it was a bit uncomfortable just to get a test from him so I said to myself he probably has an STD or something and he didn’t want me to know. I ordered the pizza, we had pizza, and I was like, “Oh, let me walk you out.” That was it. It was just kind of weird.
(#1038, 30, African-American).
Sexual Behavior Following HIV-Positive HT Results
None of the study participants received HIV-positive HT results during the course of the study, however, five participants had partners (n = 7) who received HIV-positive HT results. In all of these instances, the sexual component of the encounter ended. Furthermore, most participants reported that if a potential partner received HIV-positive HT results, they would not engage in sexual activity with the person although a few participants indicated they would do so and use condoms.
- P:
It was such an awkward moment because I was, like, this shit is positive. You know, you have, you have AIDS. And the ultimate thing was, he felt like, so what, we can use condoms. I said to him, “My dick can’t get hard on that, you know, death in my mind”…I was like, hell no. And it was just like a guilt trip, you know? A lot of these—especially when they’re attractive, they try to make you feel guilty…he was saying things like, we could use protection or just oral, you know, you want to just suck on my dick only. He just—I didn’t want any interaction like that.
(#1028; 31, African-American).
- I:
So how did doing this test affect what you did sexually?
- P:
The people that I tested that actually came out positive, I didn’t proceed to have sex with them. I’m not going to lie, like I became kind of more reserved. I still hung out or whatever like that, but I didn’t wind up having sex though. It definitely put it in my mind that I shouldn’t have sex with the person. But other than that, it was good.
(#1030; 26, Hispanic).
- P:
I mean, if it came back positive, I really wouldn’t—I wouldn’t, obviously, even have sex with him with a condom. I’m not trying to be mean, but I just—you never know, I’m not going to take that risk, once you already know that they’re—so, yeah.
(#1013; 18, White).
Sexual Behavior with Partners Who Refused HT
Twenty-one (78 %) of the participants reported experiences with potential sex partners who refused HT, whether in person or by discontinuing online communication once HT was brought up. Over half these participants reported that if a sex partner refused HT they would assume the partner to be HIV positive or too high-risk. Although eleven participants reported that they did not proceed to have sex with partners who refused HT, six did proceed with the sexual encounter. Although in some of these encounters condoms were used, this was not always the case, which is consistent with the baseline sexual behavior of these participants.
- P:
There was a guy that I hooked up with a while ago, and I met him a couple of times, but it was a long time ago, and I found him in the Internet, you know, we were getting very excited to get together, and we did the arrangements, and we will get to see each other that day, and I told him “Oh by the way, I have a home HIV test.” The way that he totally changed his mind, like all of a sudden, he cannot make it, and he start making excuses and stuff like that. That probably got me like a red flag. Like, I understand if he’s afraid of taking any test because I get scared, and I don’t like to test myself as well. But the way that he acts just give me like a heads-up, like erased him from my list.
- I:
What did it mean to you, that reaction?
- P:
That reaction? It can mean two things: one, it can be afraid of taking the test, but people who’s afraid of taking the test will tell you up front, I don’t feel comfortable taking the test because I’m afraid of the test or something of the result. But they tell you, I’m negative, but I just don’t feel comfortable with. And I also got another reaction, just like no, I don’t want to take it at all without excuse, explanation, stuff like that. So that, that really make me think about this person having something and no be honest about it.
- I:
And did you wind up having sex with him afterwards or no?
- P:
No, no, no, no, no, no.
(#1029; 32, Hispanic).
- P:
And you know, most of them was down with it. I mean, some of them wasn’t. You know it was like oh no, you know? And the ones that wasn’t with it, either I didn’t do nothing with them, or I used a—or I used a condom with them. Yeah, cause I just didn’t trust it, ‘cause I was thinking they was infected.
(#1014; 25, African-American).
- P:
Then I’ve had people that flat out said no, you know, I’m not doing it or whatever like that. Sometimes I would try to not, not have sex with them, but you know it would be enticing too much, and I still will have sex, condoms, no condoms. It really wouldn’t matter.
(#1030; 26, Hispanic).
However, a few participants understood that potential sex partners might not be willing to use HT and did not perceive the refusals negatively.
- I:
Can you take me through one of those that said no?
- P:
I can’t remember exactly what happened, but I didn’t push anything. I didn’t ask for a dissertation on why they didn’t want to. If you don’t want to, you don’t want to. I didn’t want anybody to feel uncomfortable. I didn’t want anybody to get upset.
- I:
Okay. So then when someone said no, what would happen afterwards?
- P:
Same thing that was going to happen before. Same thing as if they said yes. Saying no didn’t make me think that they were positive. I can completely understand why someone wouldn’t want to go to a stranger’s home and, you know, give a saliva sample or whatever they’re taking out of their mouth and give private information. It’s not what you bargained for when you met me or when you contacted me. So that was fine. It didn’t make me think that they were positive or that they weren’t honest or that they weren’t truthful or anything like that.
- I:
And did it alter what you did sexually with them in any way?
- P:
No.
(#1053; 38, White).
- P:
…except for one of them, that he reject the test right there, but he told me that like, he feels uncomfortable and scared to test himself in that environment… even when he goes to his physician, he’s scared. So he really told me like he tests himself every 6 months, but he’d rather to do it through his doctor. He was the only one, and I ended having sex with him, and pretty much I didn’t use condom either.
(#1029; 32, Hispanic).
Discussion
The results of this study show that among MSM who use condoms infrequently, prior patterns of condom use are seen as the most frequent reason for continuing to engage in UAI after obtaining HIV-negative HT results. Only in a minority of occasions did men attribute their lack of condom use to the HIV-negative test results. Although baseline condom use was extremely low, we observed the paradoxical effect that HIV-negative HT results were followed by actual condom use in 15 occasions. Ultimately, none of the occasions in which a partner tested HIV-positive was followed by sexual intercourse. Furthermore, when HT was refused, participants often ended the sexual encounter, perceiving these partners as HIV-positive or too high risk.
That some participants did not use condoms following HIV-negative HT results was not surprising given the target population. HT appears to provide an added level of HIV risk reduction beyond using direct inquiry or indirect assessment of the partner’s HIV status. Although some participants attributed their decision to forgo condoms to HT results, it is not clear whether these participants would have actually used condoms in those instances in the absence of HT. Similarly, reports of increases in frequency of UAI during the study period have to be seen within the context of already high baselines rates of UAI (approximately 75 % of anal intercourse occasions). Thus a question remains regarding the degree to which HT results are used as a rationalization for behavior that these men engage in nonetheless.
Other findings from the study, however, were surprising. First, that for a majority of participants, HIV-negative HT results did not always result in forgoing condoms was unexpected, especially since these men clearly state they prefer having sex without condoms, and HT can provide them with more information about the HIV status of their partners than by simply asking.
Second, we were surprised that participants remained cognizant of the window period, even during the heat of a sexual encounter. Due to concerns from public health officials and HIV prevention researchers and service providers regarding the window period, potential participants were quizzed about the window period and a demonstrated understanding of it was a requirement for study entry. However, participants could have minimized the importance of this information during their period of study participation. Interestingly, this issue was spontaneously mentioned by a majority of the participants, regardless of whether or not they used condoms following HT use, and limited the participant’s confidence in the ability of the HT to assess accurately the HIV status of their partner. Participants also remained aware that the HT did not detect other sexually transmitted infections.
Lastly, and most interestingly, is the increase in condom usage after HT use. HT demands a much lengthier conversation about HIV than is typical in sexual encounters where, even if a condom is used, there might be little or no discussion about it. Many of the participants who use the Internet to meet sexual partners reported that inquiries about HIV status are often limited to asking the potential sex partner whether he is “drug and disease free,” (DDF) usually with no further discussion of this issue once the partners meet. For our study participants, the lengthier discussion necessitated by HT use appeared to heighten their HIV risk awareness, which made it more uncomfortable to engage in UAI even after testing, especially with a new partner.
Another dynamic that emerged from the participant’s experiences is that condom usage following HT use varied depending on the relationship between the two partners. Even among those who used condoms after using HT, this was usually in the context of a new sexual partner, not a recurring sexual partner. The finding that most participants had experiences across the three categories explored in this study highlights the multi-dimensional factors at play in deciding whether to use condoms, with HT results being only one of those factors.
Clearly, HT was used by participants to screen out very high-risk sex partners for UAI. None of the participants whose partner received HIV-positive HT results had sex with that partner. Although only a few of the participants experienced this firsthand, most reported that if a partner had an HIV-positive HT result, they would end the sexual encounter. This raises concerns about HIV-related stigma. While none of the participants had sex with partners who tested HIV positive, participants were often supportive of these partners and, at times, expressed their willingness to engage in lower risk sexual behavior. Reactions to a partner testing HIV-positive were stronger among participants who did not encounter that situation. Paradoxically, these negative reactions might impede some HIV-positive MSM from disclosing their serostatus more regularly with their sexual partners, even if they use condoms during the encounter.
Many participants began to see a potential partner’s reactions to HT use as a barometer of the risk of having sex with that partner. Partners who were unwilling or even initially very hesitant to use HT during their encounter were perceived as too high-risk, resulting in an end to the sexual encounter or the use of other HIV risk reduction strategies (i.e., condom use, engaging in lower risk sexual behavior). This is consistent with previous studies [29] which have found that MSM who regularly engage in bareback sex approach sexual encounters with a default position of not using condoms unless something occurs in the interactions with a potential sex partner that triggers concern about HIV risk. For many participants, the refusal of HT appeared to act as that trigger, which resulted in them taking steps to reduce their risk of HIV infection.
Although the findings from this study offer important insights into how the use of HT with a potential sexual partner can contribute to subsequent condom use, a number of limitations need to be considered. First, because this study was not designed to formally test whether HT use resulted in changes in condom use, we did not repeat the sexual behavior assessment at the end of the study period and thus do not have data to compare sexual behavior prior to and during study participation. Second, both the quantitative and qualitative data are based on self-report, which can be inconsistent in its accuracy. Third, given the strict eligibility criteria for the study, especially the frequency with which participants had to engage in UAI, these MSM cannot be viewed as representative of MSM in general. Thus it is unclear how these findings would apply to MSM who use condoms more regularly. Fourth, these participants were provided with 16 HT kits free of charge, which would facilitate a frequency of use that might not be feasible if they had to pay for the kits every time they had sex. As such, the dynamics of HT use might be different if the test kits had to be purchased, which might alter decisions about condom usage with partners who did or did not test. Lastly, this study focused on MSM with multiple sexual partners, so the findings offer little insight into how HT might be used within longer-term relationships, especially in relation to the possibility of repeated testing. While these findings offer initial insights into how HT use may affect subsequent sexual behavior, further research with a larger number of participants is needed to study this issue more systematically. Future research should also focus on a broader group of MSM, not only those who frequently engage in UAI with multiple partners, to assess how they might utilize HT with sexual partners, and how HT use among those MSM might affect subsequent condom usage.
Nonetheless, these findings challenge the assumption that HT automatically will result in forgoing condom use, and highlight the nuance of sexual decision-making following HT use. Furthermore, the findings suggest that while HT might not be the preferred choice for some MSM, it can be a valuable tool in reducing HIV infection among MSM who regularly engage in UAI and are not committed to consistent condom use, a high-risk group for which non-condom-based HIV prevention approaches are critically needed.
References
Johns MM, Pingel E, Eisenberg A, Santana ML, Bauermeister J. Butch tops and femme bottoms? Sexual positioning, sexual decision making, and gender roles among young gay men. Am J Mens Health. 2012;6(6):505–18. doi:10.1177/1557988312455214.
Carballo-Diéguez A, Dolezal C, Nieves Rosa L, Diaz F, Decena C, Balán I. Looking for a tall, dark, macho man…Sexual-role behavior variations in Latino gay and bisexual men. Cult Health Sex. 2004;6:159–71.
Moskowitz DA, Hart TA. The influence of physical body traits and masculinity on anal sex roles in gay and bisexual men. Arch Sex Behav. 2011;40:835–41.
Moskowitz DA, Rieger G, Seal DW. Narcissism, self-evaluations, and partner preferences among men who have sex with men. Pers Individ Differ. 2009;46:725–8.
Shuper PA, Fisher WA. The role of sexual arousal and sexual partner characteristics in HIV + MSM’s intentions to engage in unprotected sexual intercourse. Health Psychol. 2008;27(4):445–54.
Kraft C, Robinson BE, Nordstrom DL, Bockting WO, Simon Rosser BR. Obesity, body image, and unsafe sex in men who have sex with men. Arch Sex Behav. 2006;35:587–95.
Lewis LA, Ross MW. A select body: The gay dance party subculture and the HIV/AIDS pandemic. New York: Cassell; 1995.
VanDevanter N, Duncan A, Burrell-Piggott T, et al. The influence of substance use, social sexual environment, psychosocial factors, and partner characteristics on high-risk sexual behavior among young Black and Latino men who have sex with men living with HIV: a qualitative study. AIDS Patient Care STDS. 2011;25(2):113–21.
Suarez T, Miller J. Negotiating risks in context: a perspective on unprotected anal intercourse and barebacking among men who have sex with men—where do we go from here? Arch Sex Behav. 2001;30:287–300.
Parsons JT, Severino J, Nanin J, et al. Positive, negative, unknown: assumptions of HIV status among HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18(2):139–49.
Gold RS, Skinner MJ, Hinchy J. Gay men’s stereotypes about who is HIV infected: a further study. Int J STD AIDS. 1999;10:600–5.
Balán IC, Carballo-Diéguez A, Ventuneac A, Remien RH, Dolezal C, Ford J. Are HIV- negative men who have sex with men and who bareback concerned about HIV infection? Implications for HIV risk reduction interventions. Arch Sex Behav. 2013;42(2):279–89.
Carballo-Diéguez A, Frasca T, Dolezal C, Balán I. Will gay and bisexually active men at high risk of infection use over-the-counter rapid HIV tests to screen sexual partners? J Sex Res. 2012;49(4):379–87.
Carballo-Diéguez A, Frasca T, Balán I, Ibitoye M, Dolezal C. Use of a rapid HIV home test prevents HIV exposure in a high risk sample of men who have sex with men. AIDS Behav. 2012;16(7):1753–60.
HIV testing basics for consumers. Centers for Disease Control and Prevention Web site (2010) http://www.cdc.gov/hiv/topics/testing/resources/qa/index.htm. Accessed 12 Feb 2013.
Brenner BG, Roger M, Routy JP, et al. High rates of forward transmission events after acute/early HIV-1 infection. J Infect Dis. 2007;195(7):951–9.
Pilcher CD, Tien HC, Eron JJ, et al. Brief but efficient: acute HIV infection and the sexual transmission of HIV. J Infect Dis. 2004;189(10):1785–92.
Eaton LA, Kalichman S. Risk compensation in HIV prevention: implications for vaccines, microbicides, and other biomedical HIV prevention technologies. Curr HIV/AIDS Rep. 2007;4(4):165–72.
Rudy BJ, Kapogiannis BG, Lally MA, et al. Youth-specific considerations in the development of preexposure prophylaxis, microbicide, and vaccine research trials. J Acquir Immune Defic Syndr. 2010;54(Suppl 1):S31–42.
Peltzer K, Banyini M, Simbayi L, Kalichman S. Knowledge, attitudes and beliefs about male circumcision and HIV by traditional and medical providers of male circumcision and traditionally and medically circumcised men in Mpumalanga, South Africa. Gend Behav. 2009;7(2):2394–429.
Peltzer K, Simbayi L, Banyini M, Kekana Q. HIV risk reduction intervention among traditionally circumcised young men in South Africa: a cluster randomized control trial. J Assoc Nurses AIDS Care. 2011;22(5):397–406.
Templeton DJ. Male circumcision to reduce sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):344–9.
Martin JN, Roland ME, Neilands TB, et al. Use of postexposure prophylaxis against HIV infection following sexual exposure does not lead to increases in high-risk behavior. AIDS. 2004;18(5):787–92.
Abbas UL, Anderson RM, Mellors JW. Potential impact of antiretroviral chemoprophylaxis on HIV-1 transmission in resource-limited settings. PLoS ONE. 2007;2(9):e875.
Golub SA, Kowalczyk W, Weinberger CL, Parsons JT. Preexposure prophylaxis and predicted condom use among high-risk men who have sex with men. J Acquir Immune Defic Syndr. 2010;54(5):548–55.
Galea JT, Kinsler JJ, Salazar X, et al. Acceptability of pre-exposure prophylaxis as an HIV prevention strategy: barriers and facilitators to pre-exposure prophylaxis uptake among at-risk Peruvian populations. Int J STD AIDS. 2011;22:256–62.
Chesney MA, Chambers DB, Kahn JO. Risk behavior for HIV infection in participants in preventative HIV vaccine trials: a cautionary note. J Acquir Immune Defic Syndr. 1997;16:266–71.
Newman PA, Roungprakhon S, Tepjan S, et al. Preventive HIV vaccine acceptability and behavioral risk compensation among high-risk men who have sex with men and transgenders in Thailand. Vaccine. 2010;28(4):958–64.
Balán I, Carballo-Dieguez A, Ventuneac A, Remien RH. Intentional condomless anal intercourse among latino MSM who meet sexual partners on the internet. AIDS Educ Prev. 2009;21(1):14–24.
Acknowledgments
This research was supported by a grant from NIMH (R01 MH79692; Principal Investigator: Alex Carballo-Diéguez, Ph.D.), Additional support was provided by the National Institute of Mental Health to the HIV Center for Clinical and Behavioral Studies at NY State Psychiatric Institute and Columbia University (P30-MH43520; Principal Investigator: Anke A. Ehrhardt, Ph.D.). The authors acknowledge the support received from Dr. Ana Ventuneac in early stages of this project. They are also extremely thankful to participants who volunteered their time and candidly expressed their opinions on very intimate topics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balán, I.C., Carballo-Diéguez, A., Frasca, T. et al. The Impact of Rapid HIV Home Test Use with Sexual Partners on Subsequent Sexual Behavior Among Men Who have Sex with Men. AIDS Behav 18, 254–262 (2014). https://doi.org/10.1007/s10461-013-0497-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0497-x