Abstract
The current study was designed to develop a better understanding of the nature of the relationships between mental health burden, drug use, and unprotected sexual behavior within a sample of emerging adult gay and bisexual men, ages 18–19 (N = 598) and to test a theory of syndemics using structural equation modeling. Participants were actively recruited from community-based settings and the Internet for participation in a seven-wave cohort study. Data for participant characteristics and mental health were collected via computer-assisted survey, while drug use and unprotected sex behaviors for the month prior to assessment were collected via a calendar-based technique. Using the baseline data, we developed and tested structural equation models for mental health burden, drug use, and unprotected sex and also tested a second-order model for a single syndemic. First-order measurement models for each of the three epidemics were successfully identified using observed data. Tests of a second-order model seeking to explain the three epidemics as a single syndemic fit poorly. However, a second-order construct comprised of mental health burden and drug use fit the data well and was highly associated with the first-order construct of unprotected sex. The findings advance a theory of syndemics and suggest that in order to be maximally effective both HIV prevention and HIV care must be delivered holistically such that sexual risk behaviors are addressed in relation to, and in sync with, the drug use and mental health of the individual.
Resumen
El estudio actual fue diseñado para desarrollar un mejor entendimiento de la naturaleza de la relación entre la salud mental, el uso de drogas y el comportamiento sexual sin protección en una muestra de hombres gay y bisexuales al inicio de la adultez, en edades entre los 18–19 años (N = 598) y para probar una teoría sindémica utilizando modelos de ecuaciones estructurales. Los participantes fueron reclutados activamente en la comunidad y en el Internet para participar en un estudio de cohorte 7 veces. Los datos acerca de las características de los participantes y salud mental fueron colectados por medio de una encuesta asistida por computadora, mientras que el uso de drogas y el comportamiento sexual sin protección en el mes anterior a la valoración fueron colectados por medio de una técnica basada en calendario. Usando los datos de base, nosotros desarrollamos y probamos modelos de ecuaciones estructurales para la salud mental, el uso de drogas, y el comportamiento sexual sin protección; y también probamos un modelo de segundo-orden para una sola sindemia. Los modelos de medición de primer-orden para cada una de las tres epidemias fueron identificados con éxito utilizando los datos observados. Las pruebas de un modelo de segundo-orden buscando explicar las tres epidemias como una sola sindemia se ajustaron pobremente a los datos. Sin embargo, una construcción de segundo-orden de la salud mental y el uso de drogas se ajustó a los datos adecuadamente y fue altamente asociada con la construcción de primer-orden del comportamiento sexual sin protección. Los hallazgos avanzan una teoría sindémica y sugieren que para ser máximamente eficiente tanto la prevención del VIH como el cuidado del VIH deben de ser suministrados de manera integral de forma que los comportamientos sexuales de riesgo sean abordados en relación a, y en coordinación con, el uso de drogas y la salud mental de los individuos.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gay and bisexual men represent only 2 % of the population [1], yet these and other men who have sex with men (MSM) account for more than 50 % of all HIV infections and new infections in the United States [2]. Particularly vulnerable are young MSM (YMSM) of color. In 2008, among Black MSM, approximately 52 % of new HIV infections were detected in those ages 13–29. Similarly, in all Hispanic MSM, the largest number of new HIV infections was detected in the same age group (ages 13–29) [2]. In New York City, a major HIV epicenter since the onset of the epidemic, HIV infection rates have doubled among YMSM ages 13–29 in all races/ethnicities in the period of 2001–2006 but disproportionately among Black MSM (126 % increase) and Hispanic YMSM (81 % increase) [3]. Moreover, 2009 was the first year in which more than 50 % of new diagnoses were reported in YMSM, ages 30 and younger [4].
Since the onset of the HIV epidemic, behavioral health researchers have sought to identify risk factors which predispose MSM to unprotected anal intercourse and in turn increase the potential for HIV seroconversion. Most of these approaches have been directed by paradigms rooted in social cognitive understandings of human behavior [5]. While this body of work had been helpful in equipping both researchers and clinicians with a tangible means of understanding the relations between risk taking and the spread of HIV, it has been limited in its understanding of how gay and bisexual men undertake their decisions surrounding risk [6]. Halkitis [7] suggests, as we enter the fourth decade of AIDS, and in light of biomedical advances, HIV prevention requires a more holistic approach that integrates all aspects of health and well being and examines HIV within the context of gay men’s lives.
The Theory of Syndemics
It was not until Singer [8, 9] studied the interplay between substance abuse, poverty, violence, and AIDS among urban women that such a holistic approach emerged. The underlying premise of this theory, rooted in anthropological understandings, suggests that numerous health conditions such as HIV and substance use are mutually reinforcing and are predisposed by social inequities, which lead to health disparities. Singer [8] indicates that HIV/AIDS disproportionately affects those who are most marginalized in our society, who experience psychosocial stressors due to these social structures, the contexts which place individuals at risk for HIV must be understood from a perspective that transcends risk groups or victim blaming. In this perspective, those at risk for HIV are predisposed to this condition by fundamental causes [9], which lead to fewer social resources and thus heightened vulnerabilities for health disparities. At the heart of the theory is the conceptualization of a syndemic [10] versus an epidemic, to explain the co-occurrence of mutually influencing and overlapping epidemics and endemics. Building upon these ideas, Halkitis [7] indicates that mental health burden, substance use, and unprotected sexual behaviors leading to HIV acquisition form a syndemic in MSM, and thus HIV prevention programs must holistically address the health of gay men by targeting all three epidemics, which are synergistic, and moreover to consider the psychosocial burdens that fuel this syndemic.
A series of studies, mostly informed by public health approaches, have tested syndemic theory in gay, bisexual, and other MSM. In 2003, Stall et al. [11] first applied the framework to include several other psychosocial health variables including polydrug use, depression, and sexual abuse in a large diverse cohort of urban MSM, and found that additively, these psychosocial burdens exacerbate rates of unprotected sex. Since then, numerous other studies have applied and upheld the tenets of syndemic theory in MSM [12, 13] and YMSM, specifically [14, 15]. Moreover, the theory of syndemics is a robust ecosocial paradigm that has applicability to numerous populations affected by health disparities and is applicable to studies beyond HIV, such as understandings cigarette smoking [15].
The Present Study
While each of the aforementioned studies has played an invaluable role in extending Singer’s [10] syndemic framework, they are not without their shortcomings. All of the current investigations have employed additive measurement models to create a measure of psychosocial burden and relied heavily on simple correlations in the assessment of the co-occurrence of psychosocial problems with unprotected sex. These models often weigh each psychosocial variable equally and employ measurement models that assume that all variables (e.g., arrest history, history of depression, use of cocaine) in the model equally contribute to sexual risk taking or HIV seroconversion among MSM, and moreover that these various psychosocial factors constitute a single construct. Such modeling is common in public health studies; however a psychological perspective posits that variables must be shown to constitute a single underlying construct. In this perspective, sophistical measurement models must be developed and tested.
The ensuing analyses are drawn from the baseline data of a prospective cohort study of YMSM in New York City. We employ structural equation modeling [16] to develop theoretically driven measurement models of the three overlapping epidemics and to test the potential for a single syndemic. Observable variables for mental health burden, drug use, and unprotected sexual behavior were examined to separately develop latent constructs for each of the three epidemics and in relation to each other to build a model for the syndemic. The research to date has demonstrated an association of mental health vulnerabilities and drug use with unprotected sex. Our goal was to advance our understanding of syndemics theory and to more elaborately examine the relations of the three health conditions, specifically the extent to which three health states indicate one all-encompassing health condition. In this regard, we hypothesized that individual indicators of each of the three constructs (mental health burden, drug use, unprotected sex) would collectively load on one latent construct for each of the behavioral domains and that these latent constructs would together form a second-order construction (i.e., the syndemic).
Methods
Study Design and Overview
Project 18 (P18) is a longitudinal study that recruited a baseline sample of 601 gay, bisexual and other YMSM in the New York City metropolitan region. Three duplicate cases were removed from the dataset, yielding a final baseline sample of 598. The study consists of seven waves of data collection at 6-month intervals; however, only the baseline data were used for this analysis. To be eligible for the study, participants must have been 18 or 19 years old at the baseline appointment. Additional inclusion criteria included sex with a male partner in the past 6 months, consenting to the study protocol and oral HIV antibody testing, and agreeing to come in for a baseline assessment and six follow-up assessments spaced 6 months apart.
Participants were actively recruited from multiple venues including social media sites on the Internet, city streets and parks, gay identified events, and community centers. Passive recruitment included snowball sampling, whereby participants were randomly selected to be eligible to receive a cash incentive for each eligible participant they referred to the study. The recruitment occurred for a period of 23 months, between June 2009 and May 2011, with a total of 2,068 individuals screened for eligibility. The majority of individuals who were ineligible did not meet the strict age criterion.
Each of the participants was screened for eligibility over the telephone and those individuals eligible to participate were provided with a scheduled appointment. At the baseline appointment written consent was obtained. The New York University Institutional Review Board approved the study protocol, and the study holds a federal certificate of confidentiality.
Study Population
More than 70 % of the participants reported a race/ethnicity other than White, with 28.3 % Hispanic, 14.9 % Black, 9.4 % mixed race and 4.8 % Asian. Participants also reported on their perceived socioeconomic status with 9.4 % reporting lower, 24.1 % lower middle, 37.1 % middle, 25.3 % upper middle and 4.2 % upper class. The majority of participants were born in the United States (89.0 vs. 11.0 %). At baseline, we confirmed via oral antibody testing that 99.0 % of the participants had a confirmed HIV negative serostatus. Participants currently enrolled in school (85.6 %) outnumbered those who are not enrolled in school (14.4 %). While most participants had never been arrested, 15.7 % reported a history of arrest. Finally, utilizing the Kinsey measure of sexual orientation, 83.9 % of participants reported being exclusively or predominantly homosexual, 11.7 % equally heterosexual and homosexual, and 4.3 % predominately heterosexual. Participant demographic information can be seen in Table 1.
Measures
Demographic Characteristics
Race/ethnicity, nation of birth (dichotomized into US-born versus foreign born), school enrollment status, arrest history, and sexual orientation [17] (ranging from 0 to 6 with 0 indicating exclusively heterosexual, 3 equally heterosexual and homosexual and 6 indicating exclusively homosexual) were gathered during the baseline assessment. In addition, the HIV status of participants was confirmed utilizing oral fluids and the OraQuick Advance® rapid HIV 1/2 antibody test.
Mental Health Burden
Experience of post-traumatic stress disorder (PTSD) was assessed using the Trauma Awareness and Treatment Center PTSD Scale [18]. This measure uses ten Likert-type items to assess level of PTSD. Typical items examine how often, in the last week, an individual has experienced upsetting memories, flashbacks, avoided places, things, or had upsetting thoughts associated with the trauma. Answer options range from 0 “Never” through 3 “Often.” Summed scores of the ten items were calculated and the measure demonstrated high internal consistency (α = 0.88). Participants were assessed using the abridged UCLA Loneliness Scale (version 3) [19]. This measure uses four Likert-type items to assess level of loneliness. The items examine how often participants feel shy, outgoing, or alone. Answer options range from 0 “Never” through 3 “Often.” This measure has been shown to have high internal consistency and test–retest reliability, as well as convergent and construct validity [19]. In our study, sum scores of the four items were calculated and the measure demonstrated moderate internal consistency (α = 0.66). Level of depression was assessed using the Beck Depression Inventory—version II [20], which consists of 21 Likert-type items. Items determine indicators of depression including experiencing loss of pleasure, feelings of worthlessness, and loss of energy. Answer options range from 0 “None” through 3 “Very much.” This measure has been shown to have high internal consistency and test–retest reliability, as well as convergent and construct validity [20]. In our study, sum scores of the 21 items were calculated and the measure demonstrated high internal consistency (α = 0.91). Finally, suicidal ideation and acts were examined through two items indicating on a binary (Yes, No), if the individual had suicidal thoughts and had attempted suicide in the previous 12 months (year).
Drug Use
Data were collected through self-report with the Timeline Followback (TLFB) [21] and drug testing of urine (iCup® DX 10 panel drug test). From the TLFB the number of days of use of alcohol, marijuana and inhalant nitrates (poppers) were recorded, with a possible range from 0 to 30 for each of these three drugs. A fourth category, other drug using days, was also calculated. These other substances included powder cocaine, crack cocaine, ecstasy, GHB, ketamine, heroin, methamphetamine, rohypnol and the following pharmaceuticals without a prescription: PDE-5 inhibitors (i.e., Cialis®, Levitra®, Viagra®), opioid pain relievers (e.g., Percocet®, Oxycontin®), ADHD drugs/stimulants (e.g., Adderall®, Ritalin®, Concerta®), and benzodiazepines (e.g., Valium®, Xanax®). Utilizing the urine drug test kits, a dichotomous score of 1 or 0 was calculated based on whether participants tested positive for any of the following drugs: barbiturates, benzodiazepines, cocaine, marijuana, ecstasy, methamphetamine/amphetamine, opiates, oxycodone, phencyclidine, propoxyphene, methadone or Tricyclic antidepressants. A positive test result for any of these drugs also resulted in a score of a 1 for that particular drug. The total number of drugs detected was summed to create a composite score ranging from 0 to 12.
Unprotected Sexual Behavior
The TLFB [21] also was utilized to capture sexual behaviors during the past 30 days. For this analysis the number of episodes of unprotected oral sex, unprotected insertive anal intercourse (UIAI), and unprotected receptive anal intercourse (URAI) were tallied. An episode was defined as one instance of any of these three behaviors with a partner. When participants engaged in one of the three behaviors with more than one partner on the same day, each partner specific instance was counted as an episode.
Analytic Plan
The data were analyzed in three stages. In the first stage, means and standard deviations for all observed indicators were examined. In the second stage, measurement models for each “epidemic” were fitted using exploratory factor analysis in MPlus [16] to test whether the hypothesized indicators for mental health burden, drug use in the past month, and unprotected sex in the past month fit the data well. Our first set of models (Model 1 in Tables 3, 4, 5) included the maximum number of observed indicators we had for each construct. Factor loadings for suicidal thoughts in the past 12 months, number of days of alcohol use, and number of UIAI episodes were fixed to 1 to provide a metric for the three respective latent constructs). For each subsequent model (Models 2–4 in Tables 3, 4, 5), we removed one or more variables that did not contribute in a statistically meaningful way to the latent constructs (determined by non-significant factor loadings as well as model fit statistics). In the final stage, after the best fitting and theoretically meaningful models for each latent construct were identified, we investigated whether the observed variables (or latent constructs) reflected a single index of syndemic production using confirmatory factor analysis. More specifically, we tested three additional measurement models: one in which we estimated a single latent construct (i.e., the syndemic) comprised of 13 observed indicators, one in which our three first-order latent constructs were used as indicators of a second-order latent construct, and one informed by previous studies of syndemic theory (e.g. 10) in which two of our first-order latent constructs (mental health burden and drug use in the past month) were used as indicators of a second-order latent construct, while unprotected sexual behavior activity in the past month remained a first-order latent construct that was allowed to correlate with the second-order construct. All models were fitted in MPlus version 5.1. Missing data were handled using Full Information Maximum Likelihood estimation [16]. Observed indicators were allowed to correlate within construct, as well as across construct, in the models testing the syndemic production factor. Goodness of fit was evaluated using multiple fit indices including χ2 (where lower, non-significant values suggest a good model fit), comparative fit index (CFI; where values between 0.90 and 1.00 suggest a good model fit), root mean square error of approximation (RMSEA; where values between 0 and 0.1 suggest a good model fit), and effect sizes indexed by the R 2 statistic (where values between 0.13 and 0.25 were considered medium and values greater than 0.25 were considered large) [22].
Results
Preliminary Analyses
Means, standard deviations, and ranges for the observed indicators representing the hypothesized latent constructs mental health burden, drug use in the past month, and unprotected sex in the past month are presented in Table 2. Less that one in five of the participants (16.6 %) contemplated suicide over the past 12 months and an even smaller proportion reported ever attempting suicide (5 %) in that period of time. Participants also reported relatively low levels of depressive symptoms, loneliness, and PTSD, although there was considerable variability around the mean (especially for depressive symptoms and PTSD) as indexed by the standard deviations (see Table 2). On average, participants reported drinking alcohol or using marijuana between 4 and 5 days during the past month but the range for these variables was considerable (from 0 to 27 days for alcohol and 0–31 days for marijuana). Use of other drugs, including inhalant nitrates (poppers), was relatively minimal. Urine testing on a random sample of participants indicated that more than a third were using some sort of drug (see Table 2). Finally, participants reported very low levels of UIAI and URAI in the past month (less than one episode per month) and slightly higher levels of unprotected oral sex. Again, the ranges for these unprotected sexual acts were sizeable, suggesting this is a very diverse sample of young men. Confirmed HIV-positive status was identified in only 1 % of the sample. Indicators of mental health burden and drug use in the past month were normally distributed, with two exceptions: number of days in past month using inhalant nitrates (skew = 13.09) and other drugs (skew = 7.98). Each of the four indicators of unprotected sex in the past month was skewed, with UIAI and HIV status being the most highly skewed (9.79 and 9.83, respectively). Note that transforming the skewed variables did not produce significantly different results and thus the variables were left in their original form.
First-Order Measurement Models: Mental Health Burden, Drug Use, and Unprotected Sex
Exploratory factor analysis was used to examine our first-order measurement models. Factor loadings for each indicator of the hypothesized latent constructs of mental health burden, drug use in the past month, and unprotected sex in the past month are presented in Tables 3, 4, 5, respectively. Coefficients outside of the parentheses are unstandardized while coefficients inside the parentheses are standardized. Tables 3, 4, 5 also include effect size coefficients (indexed by R 2) and model fit statistics. We describe in more detail below the results for each first-order latent construct. After examining multiple measurement models for each construct (i.e., mental health burden, drug use in the past month, and unprotected sex in the past month), we selected the models for each construct that both fit the data well and was the most theoretically meaningful.
Mental Health Burden
A total of four measurement models for mental health burden were fitted (see Table 3). The first (Model 1) contained all five observed indicators of mental health (i.e., thought about suicide in the past 12 months, ever attempted suicide, depressive symptoms total, loneliness total, and PTSD total). The second and third models contained only four observed indicators, with either ever attempted suicide (Model 2) or thought about suicide in the past 12 months (Model 3) removed. Finally, both suicide variables were removed in Model 4. The best fitting and most substantively meaningful model was Model 2, in which the ever attempted suicide variable was removed. Compared to Model 1, Model 2 provides a significantly better fit to the data, Δχ2 = 118.89 [3], p < 0.001. Factor loadings suggest that the depressive symptoms total score was the strongest contributor to the construct, while thoughts of suicide in the past 12 months was the weakest contributor. Effect sizes for all four indicators were moderate to large.
Drug Use
We fit a total of three measurement models for drug use in the past month (see Table 4). As with mental health burden, the first (Model 1) contained all six observed indicators of drug use (i.e., number of days in the past month using alcohol, marijuana, inhalant nitrates (poppers), or other drugs, positive urine test for drugs, and number of drugs in urine). The second and third models contained only five observed indicators, with either number of drugs in urine (Model 2) or number of days using poppers (Model 3) removed. Although the best fitting model was Model 3 (indexed by a non-significant χ2, a CFI close to 1 and a RMSEA close to 0), it was not the most theoretically meaningful model. Therefore, we selected Model 2 as the best model. Model 2 provides a better fit to the data than does Model 1, Δχ2 = 87.69 [5], p < 0.001. The number of days using marijuana in the past month and a positive urine test each contributed approximately equally to the drug use latent construct. Number of days using inhalant nitrates (poppers) in the past month contributed very little to the model (see Table 4).
Unprotected Sexual Behavior
We fit two measurement models for sexual activity in the past month (see Table 5). The first model contained all four observed indicators of sexual activity (i.e., number of UIAI, URAI, and unprotected oral episodes, and confirmed HIV status). The second model contained only three observed indicators, with confirmed HIV status removed. Although confirmed HIV status appears to add very little to the measurement model (indexed by the non-significant factor loading and the effect size of 0), likely due to the low base rates of HIV, we chose to retain this variable in our measurement model for its substantive meaning. As such, we selected Model 1 as the best fitting. Note that Model 2 is a fully saturated model and thus a comparison of the χ2 statistics between Models 1 and 2 is not particularly meaningful. All three episode variables contribute highly to the sexual activity construct but the contribution of the number of episodes performing unprotected oral sex variable was somewhat larger than was the contribution for either UIAI or URAI. Effect size for number of episodes performing unprotected oral sex was nearly twice as large as the effect sizes for UIAI and URAI.
Second-Order Measurement Model for the Syndemic
To begin to investigate whether mental health burden, drug use in the past month, and unprotected sex in the past month represent a single latent construct (a syndemic), we fit three additional models using confirmatory factor analysis. In the first model, we used the 13 observed variables retained in the analyses described above as indicators of a single syndemic latent construct. Fit indices suggest that the model did not fit the data well at all (χ2 = 792.58 (65), p < 0.001; CFI = 0.495; RMSEA = 0.137) and an examination of the factor loadings revealed that not all observed variables loaded significantly onto the latent construct (i.e., number of days inhalant nitrates (poppers) used, number of episodes of UIAI, number of episodes of URAI, number of episodes performing unprotected oral sex, and confirmed HIV status). The poor fit was further evidenced by the fact that only six of the 13 variables had statistically significant R 2 statistics associated with them (number of days using other drugs, positive urine test, thoughts about suicide in the past 12 months, total depressive symptoms, total loneliness, and total PTSD). Given the poor model fit obtained with this specification, we fit a second model in which the three first-order latent constructs (i.e., mental health burden, drug use in the past month, and unprotected sex in the past month) were used as indicators of a single second-order latent construct (i.e., syndemic). Model fit for this specification was not achieved and thus results are not reported here.
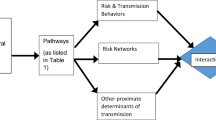
Given the above-mentioned findings, we then tested a second-order model in which mental health burden and drug use in the past month were indices of a single construct and unprotected sex was retained as a first-order construct. This approach was informed by previous examinations of syndemic theory using general linear modeling in which mental health and drug use are examined together as predictors of unprotected sexual behavior [10, 12, 13]. In this model, we allowed for correlations among variables within the first-order constructs as well as for correlations between the first (unprotected sex) and second-order (combined mental health burden and drugs use) constructs. Model fit statistics suggested that this model specification fit the data well (χ2 = 140.19 (62), p < 0.001; CFI = 0.946; RMSEA = 0.046), although neither the mental health burden nor drug use constructs explained statistically significant amounts of variance in the second-order factor. Importantly, the second-order construct of drug use and mental health was positively and significantly correlated with the first-order unprotected sex construct (r = 0.55, p < 0.001). This is shown in Fig. 1. Effect sizes for the observed variables ranged from as low as 0 (confirmed HIV) to as high as 0.83 (performing unprotected oral sex). Although number of poppers used in past month and confirmed HIV did not explain significant variation in the overall model (as evidenced by non-significant R 2 statistics), the factor loading for number of poppers used was statistically significant (unstandardized coefficient = 0.053, p < 0.01; standardized coefficient = 0.138, p < 0.01).
Discussion
Within the last decade, HIV behavioral research has been increasingly informed by a theory of syndemics [7, 23]. A significant portion of this research has attended to gay and bisexual men, who are disproportionately affected by the HIV epidemic in the United States, but also has been applied to understandings of health disparities in women [8, 10] and is increasingly an ecosocial framework espoused by researchers and practitioners seeking to understand and ameliorate health disparities. Central to this theory of syndemics is the idea that mental health burden, drug use, and unprotected sex are synergistic, mutually reinforcing health epidemics that are exacerbated in gay and bisexual men due to socially produced stressors which increase the vulnerability of gay men to these health disparities [7, 23].
At the same time, the epidemiological profile of the HIV epidemic in the United States and in large urban centers such as New York City indicates that young gay, bisexual, and other MSM, especially Black and Hispanic men ages 13–29, are highly vulnerable to HIV infection [2]. Thus we sought to test a theory of syndemics in this affected population. Whereas previous research studies examining this theoretical paradigm have implemented simplistic additive models to associate the three overlapping health risks (i.e., mental health burden, drug use, and unprotected sex), we utilized structural equation modeling to test the associations of these health conditions through the determination of latent constructs and measurement modeling, thus further adding support to the theory.
We were able to effectively fit first-order models for mental health burden, drug use, and unprotected sex using multiple indicators in our sample of racially, ethnically, and socio-economically diverse gay and bisexual men. Please note that our sample is labeled as such given that none of the young men identified as exclusively heterosexual. For our modeling of mental health burden, a latent construct was fit and consisted of depression, loneliness, PTSD, and suicidal thoughts/ideation. While previous studies have found high levels of association with these mental health states [24–26], we demonstrated not only a high level of association but also the detection of an overriding mental health burden latent construct. Only suicide attempts failed to fit in this model, which may be due to both the measurement of the behavior and underreporting of the attempts in our investigation. Previous studies have indicated the difficulty and inconsistency of measuring suicidal attempts [27].
For drug use we effectively fit a first-order model consisting of both calendar-based reports and a biological assay. Specifically, number of days use of alcohol, inhalant nitrate, marijuana, and other drug (e.g., cocaine, methamphetamine, etc.), and a positive urine test loaded together on our first-order model. While the third model we tested excluding inhalant nitrates (i.e., poppers) demonstrated a better overall fit, we retained Model 2 given the extant literature which has implicated inhalant nitrate use in HIV risk taking behaviors [28–30]. Moreover, as our sample was relatively young, drug use was not as high as reported in other studies of MSM [31, 32]. This finding is consistent with a previous New York City based study of drug using behavior in adolescent and emerging adult YMSM [33, 34].
Two unprotected sexual behavior measurement models were created. We chose to utilize Model 1, even though the overall model fit was poorer than Model 2. This decision is based in part on our decision to include confirmed HIV status as a variable of interest in this model. The project sought HIV negative participants for the baseline. While six participants tested HIV positive at baseline, we have seen increased numbers of confirmed HIV positive serostatus in this cohort as the project has continued, and thus inclusion of serostatus in the model is critical. This is in part informed by the research which indicates high levels of mental health burden and drug use among seropositive MSM [35] but also the differential selection of sexual partners (i.e., serosorting [36] and sexual positioning [37]) in which HIV positive MSM engage.
Results suggest that a second-order factor model for drug use and mental health burden is highly associated with a first-order model for unprotected sex. Despite the fact that both the observable and latent constructs across all three health states failed to fit together as one model—a single syndemic—the results are in line with previous research in the field indicating the combined effects of drug use and mental health burdens as psychosocial stressors that predispose gay, bisexual, and other MSM to unprotected sexual behavior [11, 14]. In this view, mental health burden and drug use precede unprotected sexual behavior, and create a state of increased likelihood for unprotected sex which may lead to the transmission of HIV and other pathogens. Whereas previous studies have simply correlated a summation of psychosocial stressors with unprotected sex, we have effectively developed a second-order model (drug use and mental health burden) using multiple indicators and associated it with a first-order model for unprotected sex, also indicated by numerous variables. Thus we provide robust statistical support to a theory of syndemics insomuch as these more complex models overcome the potential spuriousness associated with findings of previous research. That is to say that in previous studies (e.g., 11, 12, 13), measures of association based on correlational and regression analyses and drawn from cross-sectional data may be incorrectly inferring causality from demonstrating mathematical associations of the variables.
Limitations
As with most behavioral studies of HIV and other high-risk states, our study must be considered with regard to its limitations. First and foremost, other than the urine assays and oral HIV antibody tests, all other measures, were self-reported. Still, we believe that our use of computer delivery for the study measures and use of calendar-based techniques for assessing the drug use and unprotected sexual behavioral increase our confidence in the quality of our data. Second, we base our analyses on cross-sectional data. While our overall cohort study empowers us with increased ability to comment on causation, a truly causal relation cannot be established in the absence of an experimental study. Given that caveat and based on three decades of behavioral research, we do, however have confidence in the fact that drug use and mental health burden likely predispose gay and bisexual men to sexual risk taking. As is noted by Vanzille-Tamsen et al. [38] in their measurement of behavioral risk taking in women, relations tested with structural equation modeling using cross-sectional data may actually be reciprocal. In our study, we believe that drug use and mental health burden predispose unprotected sex, but it is possible that the reciprocal is true in that unprotected sex predisposes these stressors. In fact, what likely exists is a bidirectional association. A major tenet of syndemics theory is that these health conditions are overlapping [7].
Conclusions
The findings of our investigation of syndemic theory in young gay and bisexual men strongly supports the idea that mental health burden, drug use, and unprotected sex are highly associated in this segment of the population, thus upholding the basic tenets of the theory. This finding must be translated to our work in prevention and practice insomuch as approaches to care for these young men must fully address the synergy that exists between the health states. In effect, if we are to fully address the HIV epidemic we must also address the drug use and mental health burdens that young gay men are experiencing. Furthermore, affecting a change in psychosocial stressors that young gay and bisexual men experience will likely result in lower levels of unprotected sex on the individual and population levels. Thus, if we effectively develop supportive policies and holistic programs that attend to the societal and structural conditions that create vulnerabilities in young gay and bisexual men, we will likely see reduction in the transmission of HIV. The support and enactment of marriage equality is one such structural change [39]. Finally, we believe that our study findings and the implications of our work may also be applied to other populations in the United States and internationally to gay and bisexual men who are disproportionately burdened with HIV/AIDS.
In terms of programming, a theory of syndemics suggests that healthcare and HIV prevention must be holistically enacted [7]. That is to say that programs seeking to reduce HIV disparities must attend to the drug use and mental health burdens of those most at risk. For example, effective HIV testing programs should include assessments of psychological co-morbidities and provide counseling with regard to these health conditions in tandem with safer sex counseling. So too, for the seropositive population, healthcare providers must also attend to the psychological comorbidities which may interfere with the full uptake of medical treatments. This latter issue is particularly brought to light in terms of the HIV cascade which shows that only 28 % of those infected with HIV in the USA reach full viral suppression [40]. In the absence of such holistic approaches, HIV will continue to be handled in a decontextualized and isolated manner in both prevention and care, and the outcomes of our efforts will never truly reach full fruition.
References
Chandra A, Mosher WD, Copen C, Sionean C. Sexual behavior, sexual attraction, and sexual identity in the United States: data from the 2006–2008 National Survey of Family Growth. Natl Health Stat Rep. 2011;36:1–36.
Centers for Disease Control and Prevention. Fact Sheet: HIV and young men who have sex with men. CDC; 2011. http://www.cdc.gov/HealthyYouth/sexualbehaviors/pdf/hiv_factsheet_ymsm.pdf. Accessed 15 Dec 2011.
New York City Department of Health and Mental Hygiene. New HIV diagnoses rising in New York City among men who have sex with men. Press Release No. 079-07. New York City: New York City Department of Health; 2007.
HIV Epidemiology and Field Services Program. HIV/AIDS among men who have sex with men in New York City 2009. New York City: New York City Department of Health and Mental Hygiene; 2011. http://www.nyc.gov/html/doh/html/dires/hivepi.shtml. Accessed 15 Dec 2011.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986.
Martin JI. Transcendence among gay men: implications for HIV prevention. Sexualities. 2006;9(2):214–35.
Halkitis PN. Reframing HIV prevention for gay men in the United States. Am Psychol. 2010;65(8):752–63.
Singer M. AIDS and the health crisis of the U.S. urban poor: the perspective of critical medical anthropology. Soc Sci Med. 1994;39(7):931–48.
Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Extra Issue:80–94.
Singer M. A dose of drugs, a touch of violence, and case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Sociol. 1996;24(2):99–110.
Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42.
Egan JE, Frye V, Kurtz SP, et al. Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual, on other men who have sex with men. AIDS Behav. 2011;15(1):35–50.
Moeller RW, Halkitis PN, Surrence K. The interplay of syndemic production and serosorting in drug-using gay and bisexual men. J Gay Lesbian Soc Serv. 2011;23(1):89–106.
Mustanski BS, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45.
Storholm ED, Halkitis PN, Siconolfi DE, Moeller RW. Cigarette smoking as part of a syndemic among young men who have sex with men ages 13–29 in New York City. J Urban Health. 2011;88(4):663–76.
Muthen LK, Muthen BO. Mplus: statistical analysis with latent variables—user’s guide. Los Angeles: Muthen and Muthen; 2007.
Kinsey AC, Pomeroy WB, Martin CE. Sexual behaviors in the human male. Bloomington: Indiana University Press; 1998.
Trauma Awareness and Treatment Center. Posttraumatic Stress Disorder Scale. http://www.traumaawareness.org. Accessed 10 Feb 2009.
Russell DW. UCLA Loneliness Scale (version 3): reliability, validity, and factor structure. J Personal Assess. 1996;66(1):20–40.
Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77–100.
Sobell LC, Sobell MB. Timeline Followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto: Addiction Research Foundation; 1996.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus raw alternatives. Struct Equ Model. 1999;6(1):1–55.
Stall R, Friedman M, Catania JA. Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: health disparities affecting gay and bisexual men in the United States. Oxford: Oxford University Press; 2008.
Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Sexual orientation and mental health in a birth cohort of young adults. Psychol Med. 2005;35:971–81.
Hatzenbuehler ML. How does sexual minority stigma “Get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–30.
Mustanski BS, Garofalo R, Emerson EM. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual and transgender youth. Am J Public Health. 2010;100(12):2426–32.
Savin-Williams RC. Suicide attempts among sexual-minority youths: population and measurement issues. J Consult Clin Psychol. 2001;69(6):983–91.
Plankey MW, Ostrow DG, Stall R, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2007;45(1):85–92.
Carey JW, Mejia R, Bingham T, et al. Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS Behav. 2009;13(6):1084–96.
Ostrow DG, Plankey MW, Cox C, Li X, Shoptaw S, Jacobson LP, Stall RC. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immune Defic Syndr. 2009;51(3):349–55.
Pappas MK, Halkitis PN. Sexual risk taking and club drug use across three age cohorts of HIV-positive gay and bisexual men in New York City. AIDS Care. 2011;23(11):1410–6.
Grov C, Kelly BC, Parsons JT. Polydrug use among club-going young adults recruited through time–space sampling. Subst Use Misuse. 2009;44(6):848–64.
Halkitis PN, Moeller RW, Siconolfi DE. Young men who have sex with men (YMSM) HIV prevention project: findings from the quantitative survey of 18–29 year-old YMSM. Center for Health, Identity, Behavior and Prevention Studies, Steinhardt School of Culture, Education and Human Development, New York University; 2009 (Unpublished Report for the New York City Department of Health and Mental Hygiene).
Solomon TM, Halkitis PN, Moeller RW, Siconolfi D, Kiang MV, Barton S. Sex parties among young gay, bisexual, and other men who have sex with men in New York City: attendance and behavior. J Urban Health. 2011;88(6):1063–75.
Parsons JT, Halkitis PN, Wolitski RJ, Gómez CA, Study Team, T. S. U. M. Correlates of sexual risk behaviors among HIV positive men who have sex with men. AIDS Educ Prev. 2003;15(5):383–400.
Golden MR, Stekler J, Hughes J, Wood RW. HIV serosorting in men who have sex with men: Is it safe? J Acquir Immune Defic Syndr. 2008;49(2):212–8.
Parsons JT, Schrimshaw EW, Wolitski RJ, et al. Sexual harm reduction practices of HIV-seropositive gay and bisexual men: serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005;19(S1):S13–25.
Vanzille-Tamsen C, Testa M, Harlow LL, Livingston JA. A measurement model of women’s behavioral risk taking. Health Psychol. 2006;25(2):249–54.
Halkitis PN. Obama, marriage equality, and the health of gay men. Am J Public Health. 2012. doi:10.2105/AJPH.2012.300940.
Centers for Disease Control and Prevention. Vital signs: new hope for stopping HIV. CDC; 2011. http://www.cdc.gov/vitalsigns/HIVtesting/index.html. Accessed 15 Dec 2011.
Acknowledgments
This study was funded by the National Institute on Drug Abuse, Contract #R01DA025537 awarded to Perry N. Halkitis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Halkitis, P.N., Moeller, R.W., Siconolfi, D.E. et al. Measurement Model Exploring a Syndemic in Emerging Adult Gay and Bisexual Men. AIDS Behav 17, 662–673 (2013). https://doi.org/10.1007/s10461-012-0273-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0273-3