Abstract
The relationship between coping with HIV/AIDS stigma and engaging in risky sexual behavior (i.e., inconsistent condom use) was examined in HIV-positive adults living in rural areas. Participants answered questions about their experiences with HIV/AIDS prejudice and discrimination (enacted stigma) and their perceptions of felt HIV/AIDS stigma (disclosure concerns, negative self-image, and concern with public attitudes). They were also asked about how they coped with HIV/AIDS stigma, and about their sexual activity during the past 90 days. We hypothesized that using disengagement coping to manage the stress of HIV/AIDS stigma would be related to risky sexual behavior. Multinomial logistic regression results showed that using disengagement coping (avoidance, denial, and wishful thinking) coupled with high levels of enacted stigma was associated with less risky rather than more risky sexual behavior. That is, disengagement coping coupled with high stigma increased the odds of not having vaginal or anal sex versus inconsistently using condoms. Implications for people with HIV/AIDS who use disengagement coping to manage stress to deal with HIV/AIDS stigma are discussed.
Resumen
La relación entre hacer frente al estigma de HIV/AIDS y el acoplamiento al comportamiento sexual aventurado (es decir, uso contrario del condón) fue examinada en los adultos seropositivos que vivían en zonas rurales. Los participantes contestaron a preguntas sobre sus experiencias con el prejudicar y la discriminación (estigma decretado) de HIV/AIDS y sus opiniones del estigma del fieltro HIV/AIDS (preocupaciones del acceso, uno mismo-imagen negativa, y preocupación con actitudes públicas). También les preguntaron acerca de cómo hicieron frente al estigma de HIV/AIDS, y acerca de su actividad sexual durante los últimos 90 días. Presumimos que usar la retirada que hace frente para manejar la tensión del estigma de HIV/AIDS sería relacionada con el comportamiento sexual aventurado. Los resultados logísticos polinomiales de la regresión demostraron que usando hacer frente de la retirada (evitación, negación, y optimismo a ultranza) juntado a niveles del estigma decretado fue asociado a menos aventurado algo que un comportamiento sexual más aventurado. Es decir, el hacer frente de la retirada juntado al alto estigma aumentó las probabilidades del no tener sexo vaginal o anal contra contrario usando los condones. Las implicaciones para la gente con HIV/AIDS que utilicen la retirada que hace frente para manejar la tensión para ocuparse del estigma de HIV/AIDS se discuten.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HIV/AIDS is particularly stigmatizing both because of its association with groups that are already marginalized in American society (e.g., homosexuals, intravenous drug users) and because of its association with contagion, sickness, and death [1, 2]. Surveys have shown that people say they would avoid individuals, such as co-workers and merchants, who are known to be HIV-positive [3]. Previous research has shown that the stigma of HIV/AIDS can have a variety of negative consequences for people with HIV/AIDS. People who are stigmatized by their HIV/AIDS have reported experiences of prejudice and discrimination, loss of jobs, and violence and threats to their personal well-being because of their serostatus [4, 5]. These perceptions and experiences of HIV/AIDS stigma may be shaped in part by the communities in which people with HIV/AIDS live and work. HIV/AIDS may be particularly stigmatizing in smaller or rural communities [6–9]. A person with HIV/AIDS living in a rural area may be isolated as the only or one of a very few individuals with the disease in their community, may have access to fewer resources for support (medical and/or social) than their urban counterparts, and may experience social rejection and differential treatment because of their status because of a lack of understanding about the disease and greater fears about transmission [8, 10, 11].
A consequence of HIV/AIDS stigmatization is its potential to impact decisions to practice safer sex. Stigma may prevent people with HIV/AIDS from discussing how to practice safer sex with health care professionals for fear of being judged [12, 13]. HIV/AIDS stigma may also make it difficult for people with HIV/AIDS to disclose their seropositive status with potential sexual partners, [14, 15] thereby making it difficult for individuals with HIV/AIDS to negotiate safer sex practices. These concerns may be magnified for people living with HIV/AIDS in rural areas [16]. Healthcare professionals working in rural areas may see fewer patients with HIV/AIDS [17] and thus may not be prepared to address questions about continued sexual intimacy after infection. Rural areas also present special challenges in finding sexual partners. Past research has shown that people in rural areas have fewer sexual partners than those in more urban areas [18]. Limited potential partners may increase fears of being rejected for being HIV-positive and increase concerns about disclosing one’s status to a potential partner [19]. Our own research has shown, for example, that rural HIV-positive women reported more concerns about disclosing their HIV status than HIV-positive men in rural areas, and rural women living with HIV/AIDS have more disclosure concerns than women living with HIV/AIDS in larger cities and towns [20]. Because HIV/AIDS is being found with increasing frequency in rural areas [21, 22], understanding the relationship between stigma and sexual risk behavior may play an important part in slowing the rate of new infections.
The above reasoning would suggest that both the experiences of prejudice and discrimination (enacted stigma) and the negative feelings, concerns about disclosure and public reactions that arise from awareness of one’s stigmatized status (felt stigma) [23] should result in increased risky sexual behavior among people with HIV/AIDS. However, studies that have examined this issue have not documented a consistent relationship between HIV/AIDS stigmatization and risky sexual behavior. Some research has found that increased HIV/AIDS stigma directly [24, 25] or indirectly [26] predicted increased unsafe sexual behavior. For example, in a large study of people with HIV/AIDS in France, Peretti-Watel and colleagues [24] found that intravenous drug users and heterosexuals reporting stigma by friends, family, or coworkers because of their HIV status were more likely to report unsafe sexual behavior than people who did not experience HIV/AIDS stigma. Yet others have found no connection between HIV/AIDS stigma and sexual risk. Courtney-Quirk and associates [27] found no relationship between the experience of HIV stigmatization and reports of sexual risk in a sample of homosexual men. Furthermore, surveys of both heterosexual and homosexual HIV-positive populations have shown that other experiences, such as loneliness, predict unprotected sex better than stigmatization among people living with HIV/AIDS [28, 29]. We propose that the reason for these inconsistent findings is that the relationship between the experience of HIV/AIDS stigma and engaging in risky sexual behavior depends on the way in which the individual copes with HIV/AIDS stigma.
People with HIV/AIDS experience stressors that result directly from HIV infection, such as physical symptoms resulting from the disease or medication, [30] emotional stressors from facing a life-threatening illness [31] similar to others who live with a chronic illness, but they also experience stress stemming from the rejection, prejudice, and discrimination that characterize HIV/AIDS stigma [32–35]. We propose that the stress of HIV/AIDS stigma is a powerful stressor [34] that subsequently shapes behavioral choices. Pakenham and his colleagues [31, 36] have found that when people with HIV/AIDS were asked about the stressful problems they experience, they reported that the most stressful experiences were related to navigating challenging social situations including discrimination, stigma, confidentiality and disclosure.
We predict that the stress of HIV/AIDS stigma will predict sexual behavior as a function of how people with HIV/AIDS cope with HIV/AIDS stigma. Coping refers to cognitive, emotional, and behavioral strategies used to ameliorate a stressful event and help people return to a favorable state of being [37]. Our conceptualization of coping is based on a model of coping proposed by Compas and his colleagues [38, 39]. This model proposes that there are two major types of voluntary coping responses: engagement and disengagement coping. Engagement coping is characterized by responses that seek to change the stressful situation (called primary control engagement coping) and by responses that help the individual to adapt to the stressful situation (called secondary control engagement coping). Disengagement coping involves responses that distance the individual from the stressor and includes avoidance, denial and/or wishful thinking.
Prior research suggests that using disengagement coping strategies to cope with stress is related to risky sexual behavior. People who use avoidance, denial, and/or wishful thinking coping strategies to cope with HIV/AIDS stigma may be more likely than people who use other coping strategies to engage in behaviors that risk the transmission of HIV. For example, a study of gay men found no significant relationship between experiencing general stressors and engaging in unprotected anal intercourse (UAI) [40]. However, the same study found a significant relationship between coping with stress and risky sexual behavior. Participants who engaged in UAI reported using disengagement coping strategies such as keeping feelings to themselves and keeping others from knowing how bad things are. Similarly, a separate study found that people who coped with health-related stressors of HIV infection by using distraction and escape-avoidance strategies (disengagement coping) were more likely to report UAI than those who used other forms of coping [41]. However, these studies did not specifically look at the stress of HIV/AIDS stigma.
Current Study
These studies suggest that people with HIV/AIDS who are sexually active and who use disengagement coping to cope with stressors may be less likely to use condoms or to use condoms consistently. We predicted that using disengagement coping to deal with the stress of HIV/AIDS stigma would be related to inconsistent condom use, and that this relationship would be particularly strong for people with HIV/AIDS who perceive relatively more HIV/AIDS stigmatization.
Method
Participants
We recruited 203 people with HIV/AIDS through medical centers providing services to people with HIV/AIDS (regional comprehensive care clinics in Vermont and an HIV program at a major university-affiliated medical center in New Hampshire), AIDS service organizations in Vermont and neighboring states, and local newspaper advertisements. Eligibility requirements were that the participant was 18 years of age or older, had been diagnosed with HIV or AIDS, and could read, write, and understand the English language without assistance.
Three participants were removed from the analysis because of computer errors in the administration or recording of data. The majority of the participants (n = 147, 73.5 %) lived in Vermont, one of the most rural states in the union [42]. The remaining participants lived in New Hampshire (n = 39, 19.5 %), Massachusetts (n = 12, 6 %), and New York (n = 2, 1 %). The community sizes of the sample are described elsewhere [20], but briefly, 58 % of the sample resided towns with less than 50,000 people. The mean age of participants was 43.20 years old (SD = 8.70 years) with a range of 18–64 years. A comparison of participants’ current age with those who reported age at HIV diagnosis indicated that participants (n = 198) had lived with the virus for an average of 10.75 years (SD = 6.07 years). All participants were asked if they have ever had any HIV-related clinical conditions (e.g., Kaposi sarcoma) that the Centers for Disease Control and Prevention used to classify people into clinical categories [43]. Of the 200 participants, 137 (69 %) were categorized into the most severe clinical category, Category C, indicating that they had been diagnosed with an AIDS-defining condition. Five participants did not report their sexual activity, one participant did not report her/his age at diagnosis, and one participant did not report sexual activity or age at diagnosis, for a final sample size of 193 participants. Additional demographic information is reported in Table 1.
Measures
HIV/AIDS Stigma Scale
Perceptions of HIV/AIDS stigma were measured with a revised version [44] of the HIV/AIDS Stigma Scale [45]. The revised scale excludes 8 of the 40 items from the original scale that loaded on multiple factors. The measure consists of four subscales, each measuring different aspects of HIV/AIDS stigma. The enacted stigma subscale (11 items) includes statements about people’s actual experiences with stigma (e.g., “I have lost friends by telling them that I have HIV/AIDS.”). The disclosure concerns subscale (8 items) assesses people’s worry about who knows about their HIV-positive status (e.g., “I worry that people who know will tell others.”). The concern with public attitudes subscale includes six items assessing perceptions of how people with HIV/AIDS, in general, are viewed by others (e.g., “Most people think that a person with HIV/AIDS is really disgusting.”). Finally, the negative self-image subscale includes seven items that assess the impact of HIV/AIDS stigma on the self-worth of people living with HIV/AIDS (e.g., “I feel I am not as good as others because I have HIV/AIDS.”). Responses for all items could range from 1 (strongly disagree) to 4 (strongly agree), and mean scores for each subscale were calculated. All items are coded so that higher scores indicate more perceived stigma. In our sample, Cronbach’s alphas for the subscales ranged from 0.90 to 0.97.
Response to Stress Questionnaire-HIV/AIDS Stigma
Coping with the stigma of HIV/AIDS was assessed with the Response to Stress Questionnaire [39]. The scale can be tailored to direct participants’ focus towards a particular source of stress. In this study, participants were directed to think about how the stigma of HIV/AIDS caused them to experience stress. We used the disengagement coping subscale of this questionnaire for our analyses. The disengagement coping subscale (9 items) assesses avoidance (e.g., “I try not to think about it, to forget all about it.”), denial (e.g., “When I am around other people I act like the problems related to the stigma of HIV/AIDS never happened.”), and wishful thinking (e.g., “I deal with the problems related to the stigma of HIV/AIDS by wishing they would just go away, that everything would work itself out.”).
Participants were asked to indicate how much they used each strategy to cope with the stigma of HIV/AIDS on a scale from 1 (not at all) to 4 (a lot). Mean scores for each subscale were calculated and all items were coded so that higher scores indicate using a strategy more often. Cronbach’s alpha for the disengagement coping subscale was 0.78.
NIMH Risk Assessment Questionnaire
The measure of participants’ sexual risk behavior was adapted from the NIMH risk assessment questionnaire [46]. Participants were first asked whether they had vaginal, anal, or oral sex during the past 90 days. Those who indicated that they had been sexually active were asked how often they used condoms when they had vaginal or anal sex on a scale ranging from 1 (all of the time) to 5 (never). We classified participants as being an inconsistent condom user if they indicated that they had vaginal or anal sex and that they used condoms less than 100 % of the time (responses of 2–5). Participants were classified as consistent condom users if they indicated that they had anal or vaginal sex and they reported using condoms 100 % of the time (a response of 1). Participants who did not have anal or vaginal sex during the past 90 days, or who had indicated that they had only had oral sex in the past 90 days were classified as not having sex in the past 90 days.
Procedure
Participants came to the project site or a research assistant met them at a convenient location, usually at a recruitment site. The measures were administered via a computer program (MediaLab, [47]) in order to reduce random errors and to promote honest responses [48]. After participants read (or had read to them) a description of the study and gave their written consent to participate, the experimenter assisted them in completing practice questions about innocuous topics (e.g., food preferences) to familiarize them with the computer and with different response formats. After participants indicated that they felt comfortable with the computer, the experimenter sat so that participants had privacy as they completed the measures, but also could easily request assistance from the experimenter. Participants were monetarily compensated for their time and travel expenses. All study procedures were approved by the Institutional Review Board at the University of Vermont.
Statistical Analyses
Two analytical approaches were used. First, mean scores and Pearson’s correlations were calculated to describe the levels of stigma experienced by our sample and the relationships between the four HIV/AIDS stigma subscales and disengagement coping. Second, we used four multinomial logistic regression models to test the hypothesis that the relationship between HIV/AIDS stigma with sexual risk behavior would depend on the use of disengagement coping strategies to cope with HIV/AIDS stigma. In these logistic regressions, sexual risk behavior was the outcome variable. Each model was tested in two steps. First, a main effects models was run that included disengagement coping and HIV/AIDS stigma along with three control variables: participant’s sex (females coded as 1), number of years that had passed between the participant’s HIV diagnosis and their participation in our study (in years, with mean replacement for year of diagnosis used for participants who reported diagnosis dates earlier than 1982, when HIV was first recognized as a diagnosis), and the ranked order of the number of symptoms participants reported as part of the Category C classification checklist. These control variables were included as previous research has shown that women and men may experience stigma differently [20], that length of time living with the disease may result in different sexual practice behaviors, [49, 50] and that illness related to symptoms may affect sexual choices [51, 52]. Second, an interaction model was run adding the interaction between disengagement coping and HIV/AIDS stigma to the main effects model. Continuous variables were centered prior to analysis. Alpha levels were set to .01 to account for inflation of Type I error rate by running four models.
Results
Mean scores for the stigma subscales and coping measures are shown in Table 2. The stigma subscales were positively correlated with each other (see Table 2). Participants who reported higher levels of HIV/AIDS stigma also reported using more disengagement coping to deal with the stress of HIV/AIDS stigma (see Table 2).
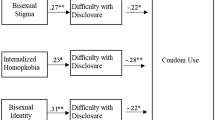
Tests of the multinomial logistic regression models revealed that only the model including the interaction between disengagement coping and enacted stigma was statistically significant (Table 3). This interaction model was a significant improvement over the main effects for disengagement coping and enacted stigma (Table 3). Table 4, which provides information about this interaction, shows the multinomial logistic regression coefficients, odds ratios, and confidence intervals for the three sexual behavior comparisons (inconsistent condom use versus no sexual activity, consistent condom use versus no sexual activity, and consistent condom use versus inconsistent condom use). Note that the odds ratios for the interactions in Table 4 represent a ratio of odds ratios [53–55]. As Table 4 shows, the interaction between disengagement coping and enacted stigma was significant at the P = 0.01 level (which was required due to multiple comparisons) for the comparison of inconsistent condom use versus no sexual behavior.
We used procedures recommended by Jaccard [56] to interpret this interaction. This involved rerunning the multinomial logistic regression using raw scores rather than centered variables. We then examined the significant interaction by using the multinomial logistic regression equation to calculate the log odds of inconsistent condom use versus no sexual activity at each of the four points of the enacted stigma subscale when disengagement coping was high (one standard deviation above the mean, 2.92) and low (one standard deviation below the mean, 1.60). The means of the three control variables (sex = 0.50, average time since diagnosis = 10.75 years, average ranked order of conditions = 3.00) were used when calculating the predicted log odds. We then transformed the predicted log odds to predicted odds. Using the predicted odds, we were able to calculate odds ratios. Each calculated odds ratio for inconsistently using condoms (compared to not engaging in sex) shows the odds comparing high disengagement coping versus low disengagement coping at each of the four levels of enacted stigma. These odds ratios are presented in Fig. 1. These odds ratios indicate that for a value of “1” on the enacted stigma subscale, which indicates strong disagreement with statements that the individual experiences enacted stigma, participants high in disengagement coping were 18.51 times more likely to inconsistently use condoms than were people low in disengagement coping. The odds ratios also show that for a value of “4” on the enacted stigma subscale, which indicates strong agreement that the individual experiences enacted stigma, the odds of participants high in disengagement coping inconsistently using condoms drops to 0.12 compared to participants low in disengagement coping, which indicates that they are less likely to inconsistently use condoms. Put another way, by calculating odds ratios predicting abstinence (versus inconsistent condom use), when a person strongly agrees that they experience enacted stigma, people high in disengagement coping are 8.06 times more likely to not have sex compared to people low in disengagement coping.
Discussion
We had predicted that using more disengagement coping to deal with HIV/AIDS stigma, coupled with increased perceptions and experiences of stigma, would make negotiations around condom use more difficult and thereby make engaging in safer sex less likely. Like previous research [27], our main effects models did not reveal a main effect of perceived stigma on sexual behavior. However, unlike previous work [40, 41], we also did not find a main effect for coping with stigma on sexual behavior. Surprisingly, and in contrast with previous research on coping and sexual risk [40, 57], people with HIV/AIDS who used more disengagement coping were less likely to engage in risky sex as reports of enacted stigma increased. One explanation of this finding is that people who use more disengagement coping strategies avoid sex when they have experienced prejudice and discrimination because of their HIV status. Indeed, the predicted odds ratios suggest that for people who agree or strongly agree that they have experienced enacted stigma are less likely to engage in inconsistent condom use than to not have sex. Our finding that people who use more disengagement coping and who experience increasing amounts of discrimination and prejudice (enacted stigma) appear to refrain from sex completely may differ from previous findings that show disengagement coping was related to unprotected sex because of the unique nature of stigma as the source of stress. It may be that enacted stigma, in particular, drives this finding because the experiences of prejudice and discrimination may be more common in the context of interpersonal relationships and, by extension, romantic or sexual interpersonal relationships.
This poses an interesting public health dilemma regarding stigma, sexual behavior and the transmission of HIV. People who disengage to cope with HIV/AIDS stigma may not have sex and thereby reduce HIV transmission risk, but only when they also endure relatively high levels of prejudice and discrimination. These individuals may not feel threatened enough to abstain from sex if they also experience relatively low enacted stigma, and thus risk transmitting the virus through inconsistent condom use. In other words, a paradoxical implication of our findings is that for some individuals with HIV a reduction in enacted stigma may increase sexually risky behavior if they cope with HIV/AIDS stigma by disengaging from it.
This finding is consistent with research indicating that increased stigma may be useful in reducing some types of risk, for example by promoting smoking cessation [58, 59] and weight loss [60]. Such findings raise questions about the frequently made assumption among social scientists [61, 62] and public health professionals [63, 64] that a reduction in HIV/AIDS stigma will promote safer sexual practices. However, even if stigma is useful in reducing unwanted behaviors such as smoking and overeating, it is important to keep in mind a critical difference between these behaviors and HIV/AIDS. In the case of many stigmatized conditions related to health (e.g., smoking, obesity), it is possible (if not always feasible) to exit from the stigmatized group. That is, one can quit smoking or lose weight, and stigma may help motivate efforts to do so. In contrast, in the case of HIV infection it is not possible to change one’s status. Once infected an individual will continue to be infected. HIV/AIDS stigma is therefore likely to do more harm than good [63, 64].
Another implication of our findings is that is important to target interventions to people with HIV/AIDS who may not be sexually active at the time of the intervention. Our model suggests that people who use more disengagement coping and who perceive more enacted HIV/AIDS stigma are less likely to engage in sex than to inconsistently use condoms. From an intervention standpoint, these people may already be perceived as preventing transmission risks and conversations may not lean toward what would happen should they become sexually active. Although abstinence may be encouraged as a way to prevent the transmission of HIV, it may be difficult to maintain [65]. And, as our findings show, a change in perception (i.e., perceiving less enacted HIV/AIDS stigma) would place these same individuals at an increased risk for inconsistent condom use, which would be an acknowledged transmission risk. An intervention that includes people who are not currently sexually active should take into account the possibility of changes in perceived stigma over time and consider how coping with experiences of prejudice and discrimination may shift someone’s sexual behavior from being relatively safe (abstaining from sex) to being relatively risky (using condoms inconsistently).
Limitations and Future Directions
These data are correlational, so it is not possible to determine whether changes in HIV/AIDS stigma and/or changes in coping with HIV/AIDS stigma would actually produce changes in sexually risky and abstinent behavior. It may be that sexual experiences influence one’s perceptions of stigma and subsequently the resources and strategies used to cope with that stigma. We are currently conducting a longitudinal study to examine how experiences of HIV/AIDS stigma, coping with HIV/AIDS stigma, and sexual behavior change over time. In light of the current findings, we plan to examine how changes over time in disengagement coping and experiences with stigma are associated with shifts in sexual behavior. We are particularly interested in whether people who use disengagement coping are especially likely to shift between abstinence and risky sex as their experiences with stigma change over time.
Additionally, future research should focus on the nature of enacted stigma experiences. People who report more enacted stigma experiences in the context of their interpersonal relationships, particularly within sexual relationships, may be more sensitive to the effects of enacted stigma on sexual behavior. Future research should also consider the importance of coping with stigma in contrast to other HIV-related stressors (e.g., medication adherence, financial concerns) and the strategies used to cope with those stressors.
Our participants live in mostly rural areas of New England, primarily in Vermont, and thus the findings of this study may not generalize to more urban populations. However, given the increasing prevalence of HIV/AIDS in rural settings, it is important to focus on how this population deals with stigmatization, and how stigmatization may translate into sexual risk. Previous research has shown that people with HIV/AIDS in rural areas may distance themselves more from their disease (a type of disengagement coping) than their urban counterparts [16]. It may be that people with HIV/AIDS in rural areas do not have enough opportunities to engage with their HIV status in a positive way (for example, through support groups). This adds support to recent research on HIV in rural America, which highlights that more services and outreach are needed in these smaller communities [17, 22, 66]. We would add that these services need to include time to acknowledge experiences of enacted stigma and how people deal with these experiences to help them to navigate social and sexual relationships.
Like most studies on sexual behavior, our study relied on a self-report measure of sexual activity and condom use. Because self-reports are virtually the only feasible way to obtain information about sexual behavior, the procedures of this study (e.g., use of computer administered measures) were designed to encourage honest responses. Finally, because we did not ask about participants’ sexual partners’ serostatus, it is possible that at least some of our “risky” participants believed that they were practicing safer sex because their partner already has HIV, and they are unaware of or ignore the risks of sexually transmitted diseases or being infected with a different strain of HIV [67].
In conclusion, this study extends prior research by showing how coping with HIV/AIDS stigma is related to sexually risky behavior. These results identify the important role that coping with HIV/AIDS stigma plays in understanding the effects of HIV/AIDS stigma on people’s sexual relationships and behaviors.
References
Capitanio JP, Herek GM. AIDS-related stigma and attitudes toward injecting drug users among black and white Americans. Am Behav Sci. 1999;42(7):1148–61.
Herek GM. Thinking about AIDS and stigma: a psychologist’s perspective. J Law Med Ethics. 2002;30(4):594–607.
Herek GM, Capitanio JP, Widaman KF. Stigma, social risk, and health policy: public attitudes toward HIV surveillance policies and the social construction of illness. Health Psychol. 2003;22(5):533–40.
Zierler S, Cunningham WE, Andersen R, Shapiro MF, Nakazono T, Morton S, et al. Violence victimization afer HIV infection in a US probability sample of adult patients in primary care. Am J Public Health. 2000;90(2):208–15.
Gostin LO, Feldblum C, Webber DW. Disability discrimination in America: HIV/AIDS and other health concerns. J Am Med Assoc. 1999;281(8):745–52.
Aruffo JF, Thompson RG, Gottlieb AA, Dobbins WN. An AIDS training program for rural mental health providers. Psychiatr Serv. 1995;46(1):79–81.
Goicoechea-Balbona A. Culturally specific health care model for ensuring health care use by rural, ethnically diverse families affected by HIV/AIDS. Health Soc Work. 1997;22(3):172–80.
Heckman TG, Anderson ES, Sikkema KJ, Kochman A, Kalichman SC, Anderson T. Emotional distress in nonmetropolitan persons living with HIV disease enrolled in a telephone-delivered. Coping Improvement Group Intervention. Health Psychol. 2004;23(1):94–100.
Reif S, Geonnotti KL, Whetten K. HIV infection and AIDS in the deep south. Am J Public Health. 2006;96(6):970–3.
Zukoski AP, Thorburn S. Experiences of stigma and discrimination among adults living with HIV in a low HIV-prevalence context: a qualitative analysis. AIDS Patient Care STDs. 2009;23(4):267–76.
Reif S, Golin CE, Smith SR. Barriers to accessing HIV/AIDS care in North Carolina: rural and urban differences. AIDS Care. 2005;17(5):558–65.
Makadon HJ, Safren SA. Prevention of HIV infection. In: Libman H, Makadon HJ, editors. HIV. 3rd ed. East Peoria: American College of Physicians and Versa Press; 2007.
Makadon HJ, Silin JG. Prevention of HIV infection in primary care: current practices, future possibilities. Ann Intern Med. 1995;123(9):715–9.
Ciccarone DH, Kanouse DE, Collins RL, Miu A, Chen JL, Morton SC, et al. Sex without disclosure of positive HIV serostatis in a US probability sample of persons receiving medical care for HIV infection. Am J Public Health. 2003;93(6):949–54.
Derlega VJ, Winstead KG, Serovich J, Elwood WN. Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. J Health Psychol. 2002;7:415–32.
Heckman TG, Somlai AM, Kalichman SC, Franzoi SL, Kelly JA. Psychosocial differences between urban and rural people living with HIV/AIDS. J Rural Health. 1998;14(2):138–45.
Cohn SE, Berk ML, Berry SH, Duan N, Frankel MR, Klein JD, et al. The care of HIV-infected adults in rural areas of the United States. J Acquir Immune Defic Syndr. 2001;28(4):385–92.
Smith TW. Adult sexual behavior in 1989: number of partners, frequency of intercourse and risk of AIDS. Fam Plann Perspect. 1991;23(3):102–7.
Heckman TG, Silverthorn M, Waltje A, Meyers M, Yarber W. HIV transmission risk practices in rural persons living with HIV disease. Sex Transm Dis. 2003;30(2):134–6.
Gonzalez A, Miller CT, Solomon SE, Bunn JY, Cassidy DG. Size matters: community size, HIV stigma and gender differences. AIDS Behav. 2009;13(6):1205–12.
Hall HI, Jianmin L, McKenna MT. HIV in predominantly rural areas of the United States. J Rural Health. 2005;21(3):245–52.
Steinberg S, Fleming P. The geographic distribution of AIDS in the United States: is there a rural epidemic? J Rural Health. 2000;16(1):11–9.
Scambler G. Stigma and disease. Lancet. 1998;352:1054–5.
Peretti-Watel P, Spire B, Obadia Y, Moatti J-P. Discrimination against HIV-infected people and the spread of HIV: some evidence from France. PLoS One. 2007;2(5):e411.
Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, Holtgrave DR. The effects f HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons. AIDS Behav. 2009;13(6):1222–32.
Preston DB, D’Augelli AR, Kassab CD, Cain RE, Schulze FW, Starks MT. The influence of stigma on the sexual risk behavior of rural men who have sex with men. AIDS Educ Prev. 2004;16(4):291–303.
Courtenay-Quirk C, Wolitski RJ, Parsons JT, Gomez CA. Team TSUMsS. Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18(1):56–67.
Golub SA, Tomassilli JC, Pantalone DW, Brennan M, Karpiak SE, Parsons JT. Prevalence and correlates of sexual behavior and risk management among HIV-positive adults over 50. Sex Transm Dis. 2010;37(10):615–20.
Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on heath behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;10(5):473–82.
Bottonari KA, Roberts JE, Ceiesla JA, Hewitt RG. Life stress and adherence to antiretroviral therapy among HIV-positive individuals: a preliminary investigation. AIDS Patient Care STDS. 2005;19(11):719–27.
Pakenham KI, Rinaldis M. Development of the HIV/AIDS stress scale. Psychol Health. 2002;17(2):203–19.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company, Inc.; 1984.
Miller CT. Social psychological perspectives on coping with stressors related to stigma. In: Levin S, van Laar C, editors. Stigma and group inequality: social psychological perspectives. Mahwah: Lawrence Erlbaum Associates Publishers; 2006. p. 21–44.
Miller CT, Kaiser CR. A theoretical perspective on coping with stigma. J Soc Issues. 2001;57(1):73–92.
Miller CT, Major B. Coping with stigma and prejudice. In: Heatherton TF, Kleck R, Hebl MR, Hull JG, editors. The social psychology of stigma. New York: The Guilford Press; 2000. p. 243–72.
Pakenham KI, Dadds RM, Terry DJ. Relationship between adjustment to HIV and both social support and coping strategies. J Consult Clin Psychol. 1994;62(6):1194–203.
Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Annu Rev Psychol. 1993;44:1–21.
Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. 2001;127(1):87–127.
Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: measurement of coping and involuntary stress responses. J Consult Clin Psychol. 2000;66(6):976–92.
Folkman S, Chesney MA, Pollack L, Phillips C. Stress, coping, and high-risk sexual behavior. Health Psychol. 1992;11(4):218–22.
Barrett DC, Bolan G, Joy D, Counts K, Doll L, Harrison J. Coping strategies, substance use, sexual activity, and HIV sexual risks in a sample of gay male STD patients. J Appl Soc Psychol. 1995;25(15):1058–72.
Duffy JJ, Hand SB, Orth RH. The Vermont encyclopedia. Lebanon: University Press of New England; 2003.
Castro KG, Ward JW, Slutsker L, Buehler JW, Jaffe HW, Berkelman RL. 1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. In: Prevention CDC, editor. Morbidity and Mortality Weekly Report;s 1992.
Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV/AIDS: a reexamination of the HIV stigma scale. AIDS Educ Prev. 2007;19(3):198–208.
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV Stigma Scale. Res Nurs Health. 2001;24(6):518–29.
Fishbein M, Coutinho R. NIMH multisite HIV prevention trial (Special Issue). AIDS. 1997;11(Suppl. 2):1–59.
Jarvis BG. MediaLab [Computer software]. v2004 ed. New York: Empirisoft Corporation; 2004.
Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108(3):339–62.
Emlet CA. Experiences of stigma in older adults living with HIV/AIDS: a mixed-methods analysis. AIDS Patient Care STDs. 2007;21:740–52.
Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53.
Dolezal C, Meyer-Bahlberg HFL, Liu X, Ehrhardt AA, Exner TM, Rabkin JG, et al. Longitudinal changes in sexual risk behavior among HIV+ and HIV− male injection drug users. Am J Drug Alcohol Abus. 1999;25(2):281–303.
Bogart LM, Collins RL, Kanouse DE, Cunningham WE, Beckman R, Golinelii D, et al. Patterns and correlates of deliberate abstinence among men and women with HIV/AIDS. Am J Public Health. 2006;96(6):1078–84.
Ai C, Norton EC. Interaction terms in logit and probit models. Econ Lett. 2003;80:123–9.
Norton EC, Wang H, Ai C. Computing interaction effects and standard errors in logit and probit models. Stata J. 2004;4(2):154–67.
Afifi A, Clark VA, May S. Computer-aided multivariate analysis. 4th ed. Boca Raton: Chapman &Hall/CRC; 2004.
Jaccard J. Interaction Effects in Logistic Regression. In: Lewis-Beck MS, editor. Thousand Oaks: Sage Publications; 2001.
Martin JI, Pryce JG, Leeper JD. Avoidance coping and HIV Risk behavior among Gay Men. Health Soc Work. 2005;30(3):193–201.
Bayer R. Stigma and the ethics of public health: not can we but should we. Soc Sci Med. 2008;67(3):463–72.
Bayer R, Stuber J. Tobacco control, stigma, and public health: rethinking the relations. Am J Public Health. 2006;96(1):47–50.
Latner JD, Wilson T, Jackson ML, Stunkard AJ. Greater history of weight-related stigmatization experience is associated with greater weight loss in obesity treatment. J Health Psychol. 2009;14(2):190–9.
Herek GM. AIDS and stigma. Am Behav Sci. 1999;42(7):1106–16.
Gilmore N, Sommerville MA. Stigmatization, scapegoating and discrimination in sexually transmitted diseases: overcoming ‘them’ and ‘us’. Soc Sci Med. 1994;39(9):1339–58.
Bell K, Salmon A, Bowers M, Bell J, McCullough L. Smoking, stigma and tobacco ‘denormalization’: further reflections on the use of stigma as a public health tool. A commentary on Social Science & Medicine’s Stigma, Prejudice, Discrimination and Health Special Issue (67: 3). Soc Sci Med. 2010;70(6):795–9.
Burris S. Stigma, ethics and policy: a commentary on Bayer’s ‘‘Stigma and the ethics of public health: not can we but should we’’. Soc Sci Med. 2008;67(3):473–5.
Barnet T, Parkhurst J. HIV/AIDS: sex, abstinence, and behaviour change. Lancet. 2005;5(9):590–3.
McKinney MM. Variations in rural AIDS epidemiology and service delivery in the United States. J Rural Health. 2002;18(3):455–66.
Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: a review of social, psychological, and medical findings. AIDS. 2002;16(2):135–49.
Acknowledgments
This study was supported by Grant R01 MH 066848 from the National Institute of Mental Health awarded to the second and third authors. The authors would like to acknowledge the Person Environment Zone Projects team, and particularly the data collection efforts of Tracy Nyerges, Lindsay Bisiker, and Daniel Cassidy. The authors also thank Janice Y. Bunn and an anonymous reviewer for statistical guidance and comments on earlier drafts of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Varni, S.E., Miller, C.T. & Solomon, S.E. Sexual Behavior as a Function of Stigma and Coping with Stigma Among People with HIV/AIDS in Rural New England. AIDS Behav 16, 2330–2339 (2012). https://doi.org/10.1007/s10461-012-0239-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0239-5