Abstract
Many women with HIV are primary caregivers for their children. Social factors, including family dynamics, play a major role in women’s depression. We hypothesized an impact of HIV seropositivity on greater depression mediated through poorer family functioning and social support. Participants include 332 Mothers Living with HIV (MLH) and 200 Neighborhood Control Mothers (NCM) recruited in Los Angeles County. The NCM were matched by neighborhood. All had children ages 6 through 20. Analyses using structural equation modeling (SEM) indicated HIV seropositivity was positively correlated with depression and negatively correlated with positive social support and effective family functioning. In a predictive path model, the relationship between having HIV and depressed mood was mediated by social support and family functioning. Findings offer explanation for increased depression resulting from HIV and social and family dynamics, and suggest innovative interventions to abate psychosocial health problems and lower risk for depression among women with HIV.
Resumen
Muchas mujeres con VIH son las cuidadoras primarias de sus hijos. Los factores sociales, incluyendo la dinámica familiar, juega un rol importante en la depresión de las mujeres. La hipótesis es que habrá un impacto de la seropositividad d al VIH a un mayor grado de depresión mediada por el mal funcionamiento familiar y el apoyo social. Las participantes incluyen 332 madres viviendo con el VIH (MLH por sus siglas en inglés) y 200 madres de Control de Vecindarios (NCM por sus siglas en inglés) reclutadas en Los Ángeles. Las NCM fueron emparejadas por vecindad. Todas tenían niños entre las edades de 6 a 20 años. Análisis con modelos de ecuaciones estructurales (SEM por sus siglas en inglés) indicaron que el seropositividad de VIH se correlacionó positivamente con la depresión y se correlación negativamente con el apoyo social positivo y funcionamiento efectivo de la familia. En un modelo de camino predictivo, la relación entre tener VIH y un estado de ánimo depresivo estaba mediada por el apoyo social y el funcionamiento familiar. Los hallazgos ofrecen una explicación para el aumento de la depresión como resultado de tener VIH y por las dinámicas sociales y familiares, y siguieren intervenciones innovadoras para mitigar los problemas psicosociales de la salud y disminuir el riesgo de depresión entre las mujeres con el VIH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HIV has taken a toll on the lives of millions of women worldwide, with the number of women infected increasing steadily [1]. Women make up an increasing proportion of persons living with HIV. Worldwide, women make up approximately 45% of persons living with HIV/AIDS [2] and in the United States, women currently account for more than one-quarter of all new HIV diagnoses [3]. Many women living with HIV/AIDS have children [4, 5] and are the primary caregivers of those children within the family [6]. It is estimated that 76% of women with HIV have children under the age of 18 in their homes [7], while 25% of women infected with HIV/AIDS desire to bear children some time during their lifetimes [8].
Further, women have higher rates of depression than men [9–12], and evidence suggests that social factors, including family dynamics, play a major role in women’s depression [13–16]. Women who are living with HIV/AIDS, many of whom are raising children, have an increased risk for depression [17], which may result from having other needs (e.g., family and finances) that compete with their own healthcare needs [18]. This suggests a need to explore the role of family dynamics (both social support and family functioning) and mental health among mothers with HIV and to contrast these relations with mothers in similar socioeconomic circumstances who are not HIV-positive. Functional impairment due to maternal HIV and maternal depression and their often mutual interactions can have numerous deleterious effects within the family. Family members typically function within a socially prescribed set of roles. Mothers’ impairment may disrupt their normative central caregiving roles or other family members’ roles may be compromised or strained when a mother becomes HIV infected or develops AIDS, impacting family functioning. For example, the emotional and physical toll HIV places on mothers with HIV/AIDS may mean that family members’ roles often shift from being cared for by the mother to providing care for her [19–23], including but not limited to ensuring adherence to antiretrovirals (ARVs).
This type of shift or disruption of family functioning has been found to lead to emotional distress [24–27] and increased symptomatology in women with other chronic diseases [28–31] including breast cancer [32–34]. For instance, Lewis et al. [35] found that more frequent illness symptoms were associated with higher levels of parental depressed mood, which negatively affected the family. When the family was less well adjusted, it negatively affected the family’s overall behavior. This type of disruption of family functioning may lead to increased symptoms of emotional distress for the mother because she cannot fully perform the primary role of caring for other members of the family. In addition, role strain due to HIV-based priorities may arise between a mother’s role as primary caregiver of others in the family and her own HIV care. Consequently, this tension between meeting her own healthcare needs and needs of the family can exacerbate emotional distress for the HIV infected mother, including but not limited to symptoms of depression. This is especially the case among HIV positive women because this is very much a disease of poor, mostly minority women with limited access to resources, which presents challenges with linkage to care, adherence to ARVs and overall quality of life for marginalized women, all of which may intensify emotional distress. Even with efficacious ARV therapy, HIV-positive women continue to struggle with appointments, adherence to regimens, and other health related issues that may impact their ability to perform their societally prescribed caretaker functions.
Family functioning is a concept that consists of a complex set of dimensions comprising affective, structural, control, cognitive, and external familial relationships. Research suggests that family functioning is dynamically changed when the matriarch (e.g., mother) becomes ill with a chronic disease (e.g., HIV) [36]. For the present study, the measurement of family functioning itself is the synthesis of many earlier attempts at studying family dynamics [37], including family theory [38, 39] and family systems theory [40]. The conceptual clustering of numerous concepts from family therapy and other social science fields reveals two significant dimensions of family behavior, cohesion and adaptability [40]. Cohesion refers to the level of bonding and the degree of autonomy family members experience. Adaptability refers to the degree to which family power structure, roles and rules of communication are rigid or changeable. In family systems research, these patterns of cohesion and adaptability, including feelings of power and control, become the norm for the family, are stabilized over time and have been found to be associated with health behaviors such as medication adherence [41]. Under-cohesive and non-expressive (disengagement) and over-cohesive (enmeshed) families are problematic and can lead to increased emotional distress. Olson [40, 42] points out that falling somewhere in between is optimal as a measure of “good family functioning.”
The effect of family dynamics on physical [43] and mental health has been studied for many years [44]. For instance, in 1951, Durkheim [45] concluded that suicide rates were higher among unmarried individuals compared to married individuals. This theory, while emphasizing the importance of marital status as one form of support, does not consider the quality of interactions among the family members (i.e., family functioning), which may also serve as a source of stress or as a source of support. The concept of family functioning, which has grown out of a clinical tradition, describes family interactions that have been shown to have numerous effects on health and mental health outcomes. These include outcomes for those suffering from both acute and chronic illnesses [46–49]. Better family functioning has been shown to be associated with increased perceptions of social support and better health behaviors [50], whereas family dysfunction has been associated with increased emotional distress [51] including depression, especially in women [52].
Social support has been defined as the functional content of interpersonal relationships [53] and the social resources one is able to call upon during a stressful life event [54]. For the purposes of this study, social support is defined as the perceived availability of functional support [55–57] in any combination of emotional, tangible, and affectionate support resources that can be called upon in the event of stressful life circumstances. Social support theory considers positive social support as a buffer between stress and mental and behavioral, and physical health outcomes; therefore, a lack of social support may also directly influence depressive symptoms. Extrapolation of these findings to mothers with HIV further suggests that social support may function as a mediator between their HIV status and depression. More positive sources of social support may help buffer the impact of their status on their depressive symptoms.
Although recent studies have examined the impact of correlates such as social support on depression [58, 59] very few, if any, take into account poor family functioning, which may affect depression further. Thus depression may be exacerbated by having HIV with the influence of family functioning and social support mediating this relationship. Mediation analysis is a useful method for testing these complex relationships and can assist in better understanding the mechanisms that impact depression [60–62].
Few studies have had the opportunity to examine relationships among family functioning, social support and depressive symptoms in mothers infected with HIV and to contrast them with normative control women from their same communities. Inclusion of comparable community women would be a positive step and help disentangle the effect of HIV- positive status on mental health outcomes in families that may already have significant problems due to poverty, racism, and other stressors. Research on the added effects of family functioning on depression for mothers with HIV is important because it provides depth regarding interpersonal family relationships that may further affect mental health above and beyond what is observed in women without HIV (controls). Thus, such findings offer the ability to challenge the notion that families are solely a source of support for mothers with HIV.
This present study builds on prior literature and examines the role of family functioning and social support in explaining the relationship between HIV and depression. We hypothesize that the deleterious direct impact of HIV on mothers’ depression is also mediated through family functioning and social support. Findings of this study will offer an explanation for increased depression that results from both HIV and family dynamics, and could guide the development of a set of innovative interventions to abate psychosocial health problems, and in the process, lower risk for depression among women with HIV. The study is strengthened with the inclusion of a set of matched neighborhood control women.
Methods
Participants
The data set consists of 532 women: 332 were Mothers Living with HIV (MLH); 200 women were Neighborhood Control Mothers (NCM). The MLH were recruited in Los Angeles County, California. As they were part of a larger study that also involved their children, inclusion criteria required that they were the mothers or primary female caregivers of at least one child between the ages of 6 and 20 who was living with them. MLH were recruited from HIV/AIDS clinics, general medical clinics, HIV/AIDS community based organizations, peer referrals, and from the rosters of previous studies. The women were recruited in waiting rooms of clinics, referred by providers, approached by members of the study staff after presentations to support groups, or were volunteers after reading promotional posters/flyers posted at participating agencies (refusal rate = 6.4%).
NCM were recruited through street outreach. After 25% of the MLH sample was recruited, the addresses of all participants were mapped. Five modal neighborhoods were identified based on clustering of MLH addresses. Screening and recruitment were conducted at grocery stores in these modal neighborhoods. Women of childbearing age were approached as they entered or left the participating market. If they were the mother or primary female caregiver of at least one child between the ages of 6 and 20 living with them they were eligible to participate. All eligible women were invited to participate in the study (NCM refusal rate = 53.0%). For all of the women, a $30.00 incentive was provided to complete the interview assessment. University Institutional Review Board approval was obtained for all study procedures and informed written consent was obtained prior to enrollment. HIV-negative status among the NCM was only ascertained by self-report.
Hispanics were primarily Spanish speaking (88%). All participants had the option to complete assessments in English or Spanish. Language preference was assessed based on the language used to conduct the interview. Literacy was low for many mothers, as approximately half of Hispanic mothers had not completed the 8th grade. All assessments were conducted by trained interviewers using laptop computers.
There were no specific quotas for racial/ethnic groups and, as a result, there are more black women in the NCM group than there are in the MLH group and more Hispanic women in the MLH group. Within the entire sample, 62% are Hispanic, 29% are black, 3% are white, less than 1% are Asian, and the remaining 6% are mixed or others. Among the MLH, 65% are Hispanic, 27% are black, 3% are white, less than 1% are Asian, and 4% are mixed or others. In the NCM set, 57% were Hispanic, 34% were black, 3% are white, less than 1% are Asian, and 5% are mixed or others.
The average age of the mothers was 40 years and the range was between 21 and 69 years. There was no significant difference between the ages of the MLH and the NCM. Fifty-seven percent of the entire sample had less than a high school education and 16% had a high school or general equivalency diploma (GED). Among the MLH, 64% had less than a high school education and 12% had a high school diploma or GED. Among the NCM, 48% had less than a high school education and 20% had a high school diploma or GED. This difference was statistically significant (p < .01). MLH were significantly less likely to be married to their current partner (−.20; p < .001) and their current partner was significantly less likely to be the father of their children (−.16, p < .01). There was no significant difference between the MLH and the NCM in the number of adults living in their households and in the number of children the women had.
Measures
The analytic method used in this study was structural equation modeling (SEM) using latent variables [63]. Indicators of latent variables are described below. The background predictors are single-item demographics. The mediators and outcome variables are latent variables.
Demographic characteristics used as background predictors included HIV status (positive: yes, no), age in years, educational level, whether they had a regular romantic partner, and their general financial status. Education was scaled from 1 to 9 and ranged from 1 (8th grade or less) to 9 (graduate or professional school degree). Seventy-four percent of the sample had a high school diploma, GED, or less. Their financial situation was described on a 1–4 scale and ranged from 1 (struggling to survive, not enough money), 2 (barely paying the bills), 3 (have the necessities, have money to cover needs, and 4 (comfortable, have money to purchase extras). To help account for the pre-existing ethnic differences between the two samples of MLH and NCM, both Hispanic and black ethnicity were included in the analyses as dummy variables (each variable scored 0–1). Others (e.g., white, Asian, mixed) served as the reference groups.
Social Support was assessed with the Medical Outcomes Study Scale [64] which originally consisted of 19 items scaled from 1 to 5 (“none of the time” to “all of the time”). Six items were not relevant for those who are not chronically ill and were not asked of the community women (e.g., “How often have you had someone to help you if you were confined to bed?”). Thus, the 13 items with complete data were used in this study. Typical items were: “How often have you had someone to give you good advice about a crisis?’ and “How often have you had someone who shows you love and affection?” Coefficient alpha was quite high among the items (.95) so items were combined randomly into parcels and means of the parcels were used as three indicators of a latent variable representing social support. Parceling is acceptable when coefficient alpha is high among the items [65]. Parceling allows one to reduce an initially large and highly related variable set to a manageable size [66].
Family Functioning items were from the Family Functioning Scale, which has been tested for reliability and validity in adult populations [67]. The three subscales that were used included “cohesion” (coefficient alpha = .87); “expressiveness” (coefficient alpha = .76) and “external locus of control” (coefficient alpha = .71). Example items include “Family members really help and support one another” (cohesion), “Family members feel free to say what is on their minds” (expressiveness), and “My family felt that they had very little influence over the things that happen to them” (reversed, external locus of control). The mean of items from each subscale were used as indicators of a latent variable representing Family Functioning.
Depression was indicated by five individual depression items from the Brief Symptom Inventory (BSI) [68, 69]. Reliability and validity of the BSI has been well established in this frequently used measure (e.g., Derogatis and Savitz [70]) including among black and Hispanic individuals [71]. Ratings ranged from 1 to 5 (1 = not at all, 5 = extremely); coefficient alpha in this group for the five items was .82. Items on the scale assessed whether the problem had bothered them during the past week.
Analysis
The analyses were performed using the EQS structural equations program [63]. Latent variable analysis allows one to evaluate mediational hypotheses with correlated, non-experimental data. Goodness-of-fit of the models was assessed with the maximum-likelihood χ 2 statistic, the Comparative Fit Index (CFI), the Satorra-Bentler χ 2 (S–B χ 2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA) [63]. The Robust S–B χ 2 was used in addition to the maximum likelihood χ 2 because it is more appropriate when the data depart from multivariate normality. The normalized multivariate kurtosis estimate was high (z-statistic = 23.90) rejecting multivariate normality. The CFI and RCFI range from 0 to 1 and reflect the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. CFI and RCFI values at .95 or greater are desirable, indicating that the hypothesized model reproduces 95% or more of the covariation in the data. The RMSEA is a measure of lack of fit per degrees of freedom, controlling for sample size, and values less than .06 indicate a relatively good fit between the hypothesized model and the observed data.
An initial confirmatory factor analysis (CFA) assessed the adequacy of the hypothesized measurement model and the associations among the latent variables and the single item variables. Then a latent variable path model positioned the demographic background variables of HIV status, age, the ethnicity dummy variables, education, financial status, and whether they were partnered as predictors of the intermediate measures of social support and family functioning. Social support and family functioning in turn predicted depression. Initially the model was tested with no direct paths from the background variables to the outcome variable of depression to see the effect of full mediation. However, based on results of the LaGrange Multiplier Test (LM Test) [63], which suggests significant paths that can improve the fit of the model and that should be included in the model, additional associations were allowed between some of the background demographic variables and the outcome variable. For instance, we expected that HIV-positive status would directly predict more depression. Other effects of all of the background variables on depression were hypothesized to be mediated through the intervening family dynamics variables. To see their impact, indirect effects were examined for significance.
Results
Confirmatory Factor Analysis
Table 1 reports summary statistics of the measured variables and the factor loadings of the hypothesized factor structure among the latent variables. All factor loadings were significant (p ≤ .001). Fit indexes for the CFA model were excellent: ML χ 2 = 243.00, 97 df; CFI = .97, RMSEA = .053; S–B χ 2 = 213.40, 97 df; RCFI = .97; RMSEA = .048. No supplementary relationships were added.
Table 2 reports the bivariate correlations among the variables in the model before the directional hypothesized mediated path model was tested. As previously reported, the Hispanic women in the sample were somewhat more likely to be HIV-positive although the relationship was not significant (.08) and the black mothers were less likely to be HIV-positive (−.07 (also non-significant)). Ethnicity was not associated with depression. Women who were HIV-positive reported less education, less financial status, were less likely to be partnered, reported lower social support, and considerably worse family function. They were more likely to report depression (.35). Older women were more likely to report not having a partner, less social support, and modestly but significantly reported more depression (.10). Hispanic women reported less education, lower financial status and lower family function. Black women reported a better education, better financial status and better family function. They were modestly more likely not to have a partner. A better education was associated with better financial status, more social support, better family function, and less depression. Those with a partner reported better social support and family function, and less depression. Better social support and family function were associated with less depression.
Path Model
The final mediated structural equation model after model trimming is presented in Fig. 1. As expected, being HIV-positive was a direct predictor of more depression and had an independent effect on that construct not mediated through social support and family function. In addition, education did not significantly predict the intermediate variables but did predict the outcome of depression. No other non-hypothesized paths or correlations were added to this model. Fit indexes were very good: ML χ 2 = 269.49, 116 df; CFI = .97, RMSEA = .050; S–B χ 2 = 241.44, 116 df; RCFI = .97; RMSEA = .045. Although there were significant bivariate relations with depression in the CFA for all of the variables in the model (except for ethnicity), most of these effects were mediated through either or both of the family constructs in the path model. Additionally, an alternative model without the mediator variables was tested; there was a considerable decrement in fit and several of the variables did not independently predict depression even without the presence of the 2 mediating latent variables. The full mediated model explained 20% of the variance in depression; the model without the mediators explained only 11% of the variance in depression.
Significant regression paths among latent and measured variables in the structural equation model assessing demographic, social, and family function influences on depression (N = 532). Regression coefficients (represented as one-way arrows) and correlations (represented by two-way arrows) are standardized (a = p ≤ .05, b = p ≤ .01, c = p ≤ .001)
Indirect Effects
Depression was impacted indirectly by all of the background variables except for education which only was a direct predictor. In addition to its direct effect, HIV-positive status was a significant indirect predictor as mediated through its negative impact on both support and family function (p ≤ .001). Age had an indirect effect on more depression as it was mediated through less social support (p ≤ .05). Hispanic ethnicity exerted an indirect negative effect through its negative relationship with family function (p ≤ .05). Black ethnicity had an indirect impact on less depression due to its mediation through better social support (p ≤ .05). This was also the case for financial status and having a partner (p ≤ .05; p ≤ .001 respectively). Being partnered also mediated through better family function so its impact was intensified.
Discussion
We found that having HIV was positively correlated with depression and that having HIV was negatively correlated with positive social support and better family functioning. Moreover, we found that the relationship between having HIV and depressed mood was mediated by both social support and family functioning, which supports research showing that mental health is associated with family functioning [72, 73]. Additionally, women who had partners had better family functioning and therefore less depression, supporting research that indicates a significant association between mental health and having a partner [74, 75].
The findings from this study illuminate the emotional effects of having HIV and the importance of positive family dynamics and strong social support in lessening those effects. These findings have direct implications in tailoring of interventions aimed at improving the mental health of women who are the caregivers of children, which should consider the role of the family within this context.
There are several contributions to the field that this study can provide. The primary contribution is that it delineates family functioning and social support and their impact on emotional distress (e.g., depressive symptoms) and rigorously identifies which of these outcomes is impacted by having HIV. Findings show that the presence of HIV is particularly associated with impaired family functioning, which may further exacerbate depressive symptoms. Much of the existing literature on parental HIV has argued that HIV adds stress to the family, which negatively affects family dynamics, leading to poorer outcomes among adolescent children [19, 76–80]. This study examined these processes from a mother’s perspective with respect to how having HIV impacts her emotional health and future research should examine how these processes may affect her ability to care for herself (e.g., health care utilization and adherence to HIV treatment regimens).
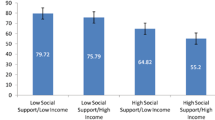
Findings from this study also provide insight into developing efficacious mental health interventions for HIV positive mothers who are already at higher risk for depression. Family function needs to be considered in any meaningful treatment plan for these women. Maternal depression is considered a significant risk factor for affecting the emotional and psychological well-being of children and other family members and impacts both parenting and child outcomes. This is especially true for low-income mothers, for which the cumulative effect of poverty, HIV and depression on the family is even greater [81]. This study helps to identify those at highest risk as suitable targets for mental health interventions because it highlights an unmet need for mothers with HIV who also have substantial family functioning difficulties, both of which have an aggregate effect on depression. Additionally, this study helps to identify the psychosocial processes, which should be the areas targeted in these interventions, including social support as lessening depression for mothers with HIV.
The findings from this study have several important implications for public health research and practice, specifically for mothers infected with HIV. The results confirm the findings of many prior studies on stress and depression and the influence of social support in abating those effects [53, 54, 56, 57, 82–87]. However, the results from this study suggest that family functioning should also be taken into account in order to assess its role in further explaining the relationship between HIV and depression, especially for black and Hispanic mothers. Therefore, funding research on the social, economic, demographic, and family factors that disproportionately place poor women of color at greatest risk for developing depression is essential. Additionally, interventions that promote access to mental health services can enhance the overall health profile of women at highest risk and should include the family.
Family functioning should be addressed if interventions are to be fully successful either through interventions that target the family specifically or interventions that incorporate the family’s role in lessening the mother’s depressive symptoms. Incorporating the family also illustrates an understanding of the importance of the family’s role because it conforms to the dual role of mothers who are infected with HIV.
There are some limitations to the present study. First, both subsamples were convenience samples. The MLH were recruited from clinical care settings, community centers, and peer referrals and the NCM were recruited at public venues in the modal neighborhoods. The generalizability of any findings is dependent upon how the sample is selected. Therefore, there may be unforeseen biases introduced by the recruitment process. For example both subsamples of mothers could have a greater need for financial resources for the assessment incentive compared to those who refused participation in the study. Similarly, the women who did participate in the study could have been more willing to participate (prosocial) or could have had more time to participate compared to the mothers who refused. The refusal rate among the MLH was very small. However, the high refusal rate among the NCM mothers lessens the representativeness of the control sample to some extent and impacts generalizing research findings since an unknown portion of the population is excluded. We cannot ascertain whether there were substantive differences between the enrolled community women and those that refused to participate as we were not able to obtain any information from those that refused. There may be an over-representation of those in financial need. Further, the use of different recruitment techniques for the subsamples introduces unknown selection bias into the sample. However, since the HIV negative mothers were recruited from the same zip codes as the HIV positive mothers, some of this bias was reduced and in many cases there were no significant differences between the two groups.
Second, this is a cross-sectional analysis, which means that attributions of causal influence among focal independent variables and the hypothesized mediators/moderators and outcomes cannot be made definitively [88]. Some establishment of directionality in the model is reasonable, such as the positioning of HIV status and the demographic variables as exogenous variables. Other causal directions, however, are more open to interpretation; for example, the conceptual model has a directional path that indicates that family functioning influences mothers’ emotional distress, yet logically it is plausible that the emotional distress of a mother can enhance conflicts within a family. However, this study was principally concerned with the impact of family functioning and social support on mothers’ depressive symptoms and the formulation of the model adequately tested these theories. Also, the cross-sectional nature of the data does not allow the examination of time trends with respect to depression. One consideration is that there may be differences in mother’s depressive symptoms over time that vary as a result of changes in the psychosocial factors that impact depression. Having data collected from multiple time points would be valuable in estimating these trends over time which suggests several avenues for future research.
Third, the sample of mothers in the study had children between the ages of 6 and 20, which is a wide range and could be representative of families with a wide variety of parental and family stressors, thereby decreasing internal validity of the study. Despite this limitation, having a comparison group of HIV negative mothers with same-aged children increases ecological validity of the study.
Finally, our analysis did not control for pre-existing mental health problems, experiences with stigma or social isolation, all of which may influence both mothers’ family functioning as well as impact perceptions of available social support. Another factor that may have a large influence on depression is that women living with HIV are more likely to have histories that include substance use, trauma exposure, child abuse and partner violence, which all may influence current social role strain, influencing depression among the HIV positive mothers in the study. Future studies should take pre-existing mental health problems, stigma and social isolation into consideration when determining factors that may influence depression.
Despite several study limitations, the proposed study has several strengths. The unique contribution of maternal HIV was assessed by including a comparable sample of mothers who were not infected with HIV, enabling the assessment of the influence of HIV on study outcomes and mediators. The sample also was predominantly low-income, minority women, precisely the group for which little information is available. Additionally, the presence of measures of key constructs permitted the testing of the theoretical model.
References
U. S. Department of Health and Human Services, CDC. The Henry J. Kaiser Family Foundation, panel on clinical practices for treatment of HIV I. Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. Center for Disease Control and Prevention, MMWR. 1998;47(RR-5):43–82.
UNAIDS. 2006 Report on the global AIDS epidemic: executive summary. 2006.
Centers for Disease Control and Prevention. Epidemiology of HIV/AIDS—United States, 1981–2005. MMWR. 2006;55(21):589–92.
Schable B, Diaz T, Chu SY, et al. Who are the primary caretakers of children born to HIV-infected mothers? Results from a multistate surveillance project. J Pediatr. 1995;95(4):511–5.
Schuster MA, Collins R, Cunningham WE, et al. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. 2005;20(9):807–13.
Parrish M, Burry C, Pabst MS. Providing comprehensive case management services to urban women with HIV/AIDS and their families. Affilia. 2003;18(3):302.
Henry J. Kaiser Family Foundation. Women and HIV/AIDS in the United States. Menlo Park: Henry J. Kaiser Family Foundation; 2007.
Serovich JM, Craft SM, Yoon HJ. Women’s HIV disclosure to immediate family. AIDS Patient Care ST. 2007;21(12):970–80.
Nolen-Hoeksema S. Gender differences in depression. Curr Dir Psychol. 2001;10(5):173–6.
Blehar M, Oren DA. Gender differences in depression. Medscape Women’s Health. 1997;2(2):3–12.
Angst J, Gamma A, Gastpar M, Lépine J-P, Mendlewicz J, Tylee A. Gender differences in depression. Eur Arch Psychiatry Clin Neurosci. 2002;252(5):201–9.
Nolen-Hoeksema S, Hilt LM. Gender differences in depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2nd ed. New York: Guilford Press; 2009.
Keitner GI, Miller IW. Family functioning and major depression: an overview. Am J Psychiatry. 1990;147(9):1128–37.
Billings AG, Moos RH. Coping, stress, and social resources among adults with unipolar depression. J Pers Soc Psychol. 1984;46(4):877–91.
Keith PM, Schafer RB. Role strain and depression in two-job families. Fam Relat. 1980;29(4):483–8.
Walters V. Stress, anxiety and depression: women’s accounts of their health problems. Soc Sci Med. 1993;36(4):393–402.
Morrison MF, Petitto JM, Have TT, et al. Depressive and anxiety disorders in women with HIV infection. Am J Psychiatry. 2002;159(5):789–96.
Penniman TV, Taylor SL, Bird CE, Beckman R, Collins RL, Cunningham W. The associations of gender, sexual identity and competing needs with healthcare utilization among people with HIV/AIDS. J Natl Med Assoc. 2007;99(4):419–27.
Tompkins TL. Parentification and maternal HIV infection: beneficial role or pathological burden? J Child Fam Stud. 2007;16(1):113–23.
Stein JA, Riedel M, Rotheram-Borus MJ. Parentification and its impact on adolescent children of parents with AIDS. Fam Process. 1999;38(2):193–208.
Rotheram-Borus MJ, Lightfoot M, Shen H. Levels of emotional distress among parents living with AIDS and their adolescent children. AIDS Behav. 1999;3(4):367–72.
Rotheram-Borus M, Flannery D, Rice E, Lester P. Families living with HIV. AIDS Care. 2005;17(8):978–87.
Stein JA, Rotheram-Borus MJ, Lester P. Impact of parentification on long term outcomes among children of parents with HIV/AIDS. Fam Process. 2007;46(3):317–33.
Thompson MG, Heller K. Facets of support related to well-being: quantitative social isolation and perceived family support in a sample of elderly women. Psychol Aging. 1990;5(4):535–44.
Thompson A, Bolger N. Emotional transmission in couples under stress. J Marriage Fam. 1999;61(1):38–48.
Larson RW, Almeida DM. Emotional transmission in the daily lives of families: a new paradigm for studying family process. J Marriage Fam. 1999;61(1):5–20.
Larson RW, Gillman S. Transmission of emotions in the daily interactions of single-mother families. J Marriage Fam. 1999;61(1):21–37.
Armistead L, Klein K, Forehand R. Parental physical illness and child functioning. Clin Psychol Rev. 1995;15(5):409–22.
Compas BE, Worsham NL, Epping-Jordan JE, et al. When mom or dad has cancer: markers of psychological distress in cancer patients, spouses, and children. Health Psychol. 1994;13(6):507–15.
Compas BE, Worsham NL, Ey S, Howell DC. When mom or dad has cancer: II. Coping, cognitive appraisals, and psychological distress in children of cancer patients. Health Psychol. 1996;15(3):167–75.
Forehand R, Steele R, Armistead L, Morse E, Simon P, Clark L. The Family Health Project: psychosocial adjustment of children whose mothers are HIV infected. J Consult Clin Psychol. 1998;66(3):513–20.
Lewis FM. Strengthening family supports. Cancer and the family. Cancer. 1990;65(3 Suppl):752–9.
Vess JD Jr, Moreland JR, Schwebel AI. A follow-up study of role functioning and the psychological environment of families of cancer patients. J Psychosoc Oncol. 1985;3(2):1–14.
Vess JD Jr, Moreland JR, Schwebel AI. An empirical assessment of the effects of cancer on family role functioning. J Psychosoc Oncol. 1985;3(1):1–16.
Lewis FM, Hammond MA, Woods NF. The family’s functioning with newly diagnosed breast cancer in the mother: the development of an explanatory model. J Behav Med. 1993;16(4):351–70.
Lee E-O, Park YS, Song M, Lee IS, Park Y, Kim HS. Family functioning in the context of chronic illness in women: a Korean study. Int J Nurs Stud. 2002;39(7):705–11.
Bloom BL. A factor analysis of self-report measures of family functioning. Fam Process. 1985;24(2):225–39.
Beavers WR, Hampson RB, Hulgus YF. Commentary: the Beavers systems approach to family assessment. Fam Process. 1985;24(3):398–405.
Anderson AR, Henry CS. Family system characteristics and parental behaviors as predictors of adolescent substance use. Adolescence. 1994;29(114):405–20.
Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family systems: I. Cohesion and adaptability dimensions, family types, and clinical applications. Fam Process. 1979;18(1):3–28.
Weiss SJ, Chen JL. Factors influencing maternal mental health and family functioning during the low birth weight infant’s first year of life. J Pediatr Nurs. 2002;17(2):114–25.
Olson DH. Circumplex model of marital and family systems: assessing family functioning. In: Walsh F, editor. Normal family processes. 2nd ed. Guilford family therapy series (pp. 104–137). New York: Guilford Press; 1993.
Umberson D. Gender, marital status and the social control of health behavior. Soc Sci Med. 1992;34(8):907–17.
Umberson D, Williams K. Family status and mental health. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. New York: Springer; 1999.
Durkheim E. Suicide (Spaulding JA & Simpson G, Trans.). Glencoe: Free Press (Original work published 1897); 1951.
Gazendam-Donofrio SM, Hoekstra HJ, van der Graaf WTA, et al. Family functioning and adolescents’ emotional and behavioral problems: when a parent has cancer. Ann Oncol. 2007;18(12):1951–6.
Ohannessian CMC, Lerner RM, Lerner JV, von Eye L. Discrepancies in adolescents’ and parents’ perceptions of family functioning and adolescent emotional adjustment. J Early Adolesc. 1995;15(4):490–516.
Shek DTL. Linkage between marital quality and parent-child relationship: a longitudinal study in the Chinese culture. J Fam Issues. 1998;19(6):687–704.
Trask PC, Paterson AG, Trask CL, Bares CB, Birt JA, Maan C. Parent and adolescent adjustment to pediatric cancer: associations with coping, social support, and family function. J Pediatr Oncol Nurs. 2003;20(1):36–47.
Franks P, Campbell TL, Shields CG. Social relationships and health: the relative roles of family functioning and social support. Soc Sci Med. 1992;34(7):779–88.
Denenberg R. HIV does not erase desire: addressing the sexual and reproductive concerns of women with HIV/AIDS. In: Goldstein N, Manlowe JL, editors. The gender politics of HIV/AIDS in women: perspectives on the pandemic in the United States. New York: New York University Press; 1997.
Leung KK, Lue BH, Lee MB, Tang LY. Screening of depression in patients with chronic medical diseases in a primary care setting. Fam Pract. 1998;15(1):67–75.
House JS. Social support and social structure. Sociol Forum. 1987;2(1):135–46.
Pearlin LI, Aneshensel CS. Coping and social supports. In: Aiken LH, Mechanic D, editors. Applications of social science to clinical medicine and health policy. New Jersey: Rutgers University Press; 1986.
Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social support: theory, research and application. The Hague: Martinus Nijhoff; 1985.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57.
House JS, Kahn RL, McLeod JD. Social support and health. In: Cohen S, Syme SL, editors. Measures and concepts of social support. New York: Academic Press; 1985.
Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21(8):1007–13.
Mosack KE, Weinhardt LS, Kelly JA, et al. Influence of coping, social support, and depression on subjective health status among HIV-positive adults with different sexual identities. Behav Med. 2009;34(4):133–44.
Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82.
MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Curr Dir Psychol Sci. 2009;18(1):16–20.
MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593.
Bentler PM. EQS structural equations program manual. Encino: Multivariate Software, Inc.; 2006.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14.
Yuan KH, Bentler PM, Kano Y. On averaging variables in a confirmatory factor analysis model. Behaviormetrika. 1997;24(1):71–83.
Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: exploring the question, weighing the merits. Struct Equ Model. 2002;9(2):151–73.
Bloom BL. A factor analysis of self report measures of family functioning. Fam Process. 1985;24(2):225–39.
Derogatis L. The Brief Symptom Inventory (BSI): administration, scoring and procedures. Manual II. Baltimore: Clinical Psychometric Research, Inc.; 1992.
Derogatis LR. Brief symptom inventory. Baltimore: Clinical Psychiatric Research Inc.; 1975.
Derogatis LR, Savitz KL. The SCL-90 and the Brief Symptom Inventory (BSI) in primary care. In: Maruish ME, editor. Handbook of psychological assessment in primary care. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. p. 297–334.
Hoe M, Brekke J. Testing the cross-ethnic construct validity of the Brief Symptom Inventory. Res Soc Work Pract. 2009;19(1):93–103.
Sarmiento IA, Cardemil EV. Family functioning and depression in low income latino couples. J Marital Fam Ther. 2009;35(4):432–45.
Epstein-Lubow GP, Beevers CG, Bishop DS, Miller IW. Family functioning is associated with depressive symptoms in caregivers of acute stroke survivors. Arch Phys Med Rehabil. 2009;90(6):947–55.
Wood RG, Goesling B, Avellar S. The effects of marriage on health: a synthesis of recent research evidence. Washington: Department of Health and Human Services; 2007.
Shapiro A, Keyes CLM. Marital status and social well-being: are the married always better off? Soc Indic Res. 2008;88(2):329–46.
Bauman K, Faris R, Ennett S, Hussong A, Foshee V. Adding valued data to social network measures: does it add to associations with adolescent substance use? Soc Netw. 2007;29(1):1–10.
Tompkins C. Who will care for the grandparents? Exploring relationships between grandparents and grandchildren. J Psychiatr Nurs Ment Health Serv. 2007;45(5):19–22.
Heneghan AM, Silver EJ, Bauman LJ, Westbrook LE, Stein REK. Depressive symptoms in inner-city mothers of young children: who is at risk? Pediatrics. 1998;102(6):1394–400.
Witte SS, de Ridder NF. “Positive Feelings”: group support for children of HIV-infected mothers. Child Adolesc Soc Work J. 1999;16(1):5–21.
Rotheram-Borus MJ, Lee M, Leonard N, et al. Four-year behavioral outcomes of an intervention for parents living with HIV and their adolescent children. AIDS. 2003;17(8):1217–25.
Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113(6):e523–9.
Cassel J. The contribution of the social environment to host resistance: the fourth Wade Hampton Frost Lecture. Am J Epidemiol. 1976;104(2):107–23.
Cobb S. Social support as a moderator of life stress. Psychosom Med. 1976;38(5):300–14.
Cohen S, McKay G. Social support, stress, and the buffering hypothesis: a theoretical analysis. In: Baum A, Singer JE, Taylor SE, editors. Handbook of psychology and health, vol 4. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 1984. p. 253–267.
House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–5.
Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78(3):458–67.
Kessler RC, McLeod JD. Social support and mental health in community samples. In: Cohen S, Syme SL, editors. Social support and health. San Diego: Academic Press; 1985.
Wegener DT, Fabrigar LR. Analysis and design for nonexperimental data: addressing causal and noncausal hypotheses. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. New York: Cambridge University Press; 2000.
Acknowledgments
This research was supported by Grant MH-068194 from the National Institute of Mental Health, Grants DA 01070-38 and DA 007292-17 from the National Institute on Drug Abuse. The authors would also like to thank Dr. Brandon Brown and Alejandra Cabral for their assistance in translating the abstract into Spanish.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dyer, T.P., Stein, J.A., Rice, E. et al. Predicting Depression in Mothers With and Without HIV: The Role of Social Support and Family Dynamics. AIDS Behav 16, 2198–2208 (2012). https://doi.org/10.1007/s10461-012-0149-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0149-6