Abstract
This pilot study used a randomized controlled trial to test the efficacy of an HIV risk-reduction intervention for university students in Eastern Cape Province, South Africa. Randomly selected second-year students were randomized to one of two interventions based on social cognitive theory and qualitative research: HIV risk-reduction, targeting sexual-risk behaviors; health-promotion control, targeting health behaviors unrelated to sexual risks. Participants completed behavioral assessments via audio computer-assisted self-interviewing pre-intervention, 6, and 12 months post intervention, with 97.2% retained at 12-month follow-up. Averaged over the 2 follow-ups, HIV risk-reduction intervention participants reported less unprotected vaginal intercourse and more frequent condom use than control participants, with greater efficacy in non-South Africans than South Africans. Positive changes were also observed on theoretical mediators of condom use that the intervention targeted. Interventions based on social cognitive theory integrated with qualitative information from the population may reduce sexual risk behaviors among university students in sub-Saharan Africa.
Resumen
Este estudio piloto se utilizó una prueba controlada aleatoria para probar la eficacia de la intervención para reducir el riesgo de VIH entre estudiantes universitarios en la Provincia Oriental del Cabo, Sudáfrica. Estudiantes de segundo año seleccionados al azar fueron asignados a una de dos intervenciones basadas en teoría cognoscitiva social e investigación cualitativa: reducción de riesgo para VIH con atención a conductas de riesgo sexual; promoción de la salud con atención a conductas no relacionas a riesgos sexuales. Los participantes completaron encuestas por medio del uso de computadoras con audio, pre-intervención y 6 y 12 meses post-intervención, con un 97.2% de retención al darse seguimiento 12 meses después. Promediada sobre los 2 seguimientos, participantes de intervención de reducción del riesgo de VIH reportó menos relaciones sexuales sin protección y uso de preservativos más frecuentemente que los participantes de control, con una mayor efectos en aquellos que no eran sudafricano en comparación con los sudafricanos. Cambios positivos fueron también observados en mediadores teóricos del uso del condón. Las intervenciones basadas en la teoría cognitiva social integrada con información cualitativa de la población pueden reducir los comportamientos sexuales de riesgo entre los estudiantes universitarios en el África subsahariana.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The HIV/AIDS pandemic continues to have its greatest impact in sub-Saharan Africa [1], which accounted for 67% of HIV infections worldwide, 71% of all new HIV infections, and 72% of the world’s AIDS-related deaths in 2008 and where poverty, poor health systems, and limited resources for prevention and care fuel the spread of the HIV. In South Africa, an estimated 5.7 million were living with HIV at the end of 2008, [1] the largest number of people living with HIV in the world. South Africa, like many sub-Saharan countries, has a “generalized HIV epidemic,” which means that HIV has spread beyond high-risk groups to the general population [2]. Curbing the spread of HIV in a generalized epidemic requires interventions delivered in a variety of venues to reach all subpopulations that engage in HIV risk behaviors because intervening only with high-risk groups would not be sufficient to stem such an epidemic [3].
Evidence from several sources suggests that one of the subpopulations in sub-Saharan Africa that engages in HIV risk behaviors is university students. In one study, 26.0% of university students in South Africa reported ever being pregnant or fathering a pregnancy as compared with 8.3% of US students [4]. In addition, 15.0% of students in South Africa reported a history of STIs as compared to 1.9% of the US students [4]. STIs are commonly asymptomatic and, accordingly, are often not detected or treated promptly, fueling broader transmission especially in closed communities such as university campuses. Moreover, STIs increase susceptibility to HIV [5].
Sexual risk behavior data further underscore the high risk of HIV/STI among university students in South Africa, particularly in the context of a generalized epidemic. In one study, about three-quarters of university students in South Africa and the US reported ever having sexual intercourse, but the students in South Africa reported a younger age at first sex, were less likely to report condom use at first sex, were more likely to report ever being forced to have sex, reported having sex with a greater number of lifetime sexual partners, and were more likely to report having multiple sexual partners (i.e., two or more) in the previous 3 months compared with US students. Although the rate of condom use in the previous 3 months did not differ between university students in South Africa and those in the US [4], given the differences in the nature of the epidemic and HIV prevalence between the two countries, failure to use condoms creates far greater risk in South Africa than in the US.
A recent HIV surveillance survey [6] provides more direct evidence of the high risk of HIV among university students in sub-Saharan Africa. It revealed that the national prevalence rate of HIV among university students in South Africa was 3.4%. Although lower than the 8.7% estimated national prevalence [7] among youth aged 15–24 years, 3.4% is still an alarmingly high prevalence rate. However, despite the high risk of HIV among university students in sub-Saharan Africa, few studies have reported tests of the efficacy of HIV risk-reduction interventions specifically designed for university students in sub-Saharan Africa, and none employing a randomized controlled design with a follow-up of at least 12 months has reported intervention-induced reductions in sexual risk behaviors [8]. This dearth of intervention trials is especially troubling because university students are the most capable and promising members of all societies and constitute the next generation of a nation’s leadership in all sectors [9, 10].
In response to the high risk of HIV among university students, the Higher Education HIV and AIDS Programme of South Africa [6] has called for peer-education HIV risk-reduction programs targeting university students, particularly first-year, second-year, and women students. Consistent with this call, we report a pilot study utilizing a randomized controlled trial to test the efficacy of an intervention to reduce sexual risk behavior among university students in South Africa. We drew upon the social cognitive theory [11] integrated with formative research, including focus groups and surveys, with the target population to develop an intervention that was both theoretically grounded and developmentally and contextually appropriate. We hypothesized that the intervention would reduce unprotected sexual intercourse compared with a health-promotion control intervention during a 12-month follow-up period. Secondary outcomes included other sexual behaviors and measures of psychological variables from the theoretical framework.
Methods
The Institutional Review Board at the University of Pennsylvania and the Ethics Committee at the University of Fort Hare approved all procedures. We conducted the study at a university located in a rural area in Eastern Cape Province, South Africa. The prevalence of HIV among university students in the Eastern Cape region at 6.4% ranked the highest of the five regions into which institutions were clustered in a national surveillance survey, and among Black students in the Eastern Cape region, the prevalence was 8.4% [6]. We conducted all research activities in English, the language of instruction at the university.
In November 2008, near the end of the academic year, the university’s administration provided a list with names, gender, nationality, and contact details of all first-year students (1,209 South Africans and 260 non-South Africans, for a total of 1,469 students). We used a standard recruitment protocol to invite them to participate in the trial, oversampling non-South African students. Using computer-generated number sequences, we randomly selected 240 students such that the sample included equal numbers of male and female and South African and non-South African students.
Students aged 18 to 24 years who had been randomly selected and who planned to remain as students at the university for the next two academic years, which would allow for intervention implementation and 12-month follow-up data collection, were eligible. Recruiters contacted the randomly selected students to determine their eligibility, willingness, and availability to participate. They invited eligible students to participate in “Wake Up,” a health promotion project designed to understand students’ behaviors that may create health risks such as heart disease, cancer, and STIs, especially HIV, and to find ways to teach students how to reduce these risks. Recruiters scheduled those who agreed to participate for the baseline data collection when they returned for the beginning of their second year in January 2009. Students who completed the baseline data collection were scheduled for randomization and intervention session 1.
Randomization to Interventions
The study utilized a randomized controlled trial design. Using a computer-generated random number sequences, we randomly assigned the students to 1 of 2 interventions—HIV risk reduction or health-promotion control. One researcher conducted the computer-generated random assignments; another researcher implemented the assignments. South African and non-South African male and female students were randomly assigned separately to ensure that nationality and sex were balanced across the interventions.
Intervention Methods
Each intervention consisted of 8, 45-minute modules, with 2 modules delivered during each of 4 weekly sessions. Each intervention was highly structured and involved interactive exercises, games, brainstorming, role-playing, videos, and group discussions implemented in mixed-sex groups of 7 to 11 participants (mean = 8.8 participants) by co-facilitator pairs using standardized intervention manuals. Table 1 contains an outline of the modules in the HIV risk-reduction intervention.
We drew upon the social cognitive theory [11], which has been employed to develop many behavioral interventions in many settings, including South Africa [12–16], and extensive formative research, including a cross sectional survey [4], a prospective survey [17], and focus groups with the target population to develop an HIV risk-reduction intervention that was both grounded in theory and culturally and developmentally appropriate for sub-Saharan African university students. We asked students (N = 108) in nine focus groups questions designed to elicit beliefs relevant to social cognitive theory constructs of outcome expectancy and self-efficacy. The participants in the focus groups expressed several positive outcome expectancies regarding condom use. They said that condoms can reduce the risk of “falling pregnant,” “contracting HIV,” and “contracting STIs,” and that “they are also good with early ejaculation.” Negative outcome expectancies included “you can get infected since condoms are not 100% safe,” “you won’t enjoy it to the fullest, eating a sweet with its wrapper on,” “condom might burst,” “it is a fact that they do sometimes cause infection,” and “perhaps my partner wouldn’t want to, and may suspect I am being unfaithful or not in love with him and leave me.” The beliefs relevant to self-efficacy included things that would make it easier to use a condom: “always have a condom in my room, bag, or pocket,” “having goals in life,” “bigger/large size condoms,” and “agreement and willingness of my partner.” The things that would make it harder to use condoms included “when my partner always insists that we must not use condoms,” “prolonged foreplay,” “my partner would think I am doubting him,” “they sometimes kill the mood and get in the way,” “drinking and then completely losing our mind,” and “what friends would say if they see condoms in my handbag.”
We designed the HIV risk-reduction intervention activities (a) to address condom-use outcome expectancies identified in the focus groups, (b) to increase skills and self-efficacy to address the things that the focus group participants said made it easy or hard to use condoms, and (c) to increase HIV risk-reduction knowledge, including condom-use knowledge. To address some beliefs we wished to target, we adapted activities from other efficacious HIV risk-reduction interventions [18–21].
Forced-choice activities in which participants publicly embraced and defended a belief were used to address outcome expectancies and peer pressure. A “HIV Magazine” video addressed myths and facts about HIV [21]. An interactive exercise, “HIV Risk Continuum,” addressed the degree of risk posed by different sexual behaviors [18]. An interactive exercise, the “Transmission Game,” addressed how STIs are transmitted through a sexual network [18]. A brainstorming and sentence-completion activity, “Benefits of Abstinence,” addressed the benefits of abstinence versus sexual intercourse [19]. Penis models were used to teach condom use skills. Participants pulled condoms over their hand and up their arm as a demonstration of the large volume a condom can accommodate. A 3-minute video clip contained an animation of female condom use. Participants were given “condom goodie bags” containing water-based lubricant, female condoms, and an assortment of condoms [20]. A brainstorming and sentence-completion activity was employed to address how to make using condoms more pleasurable and spontaneous [18]. A video clip illustrated effective condom use negotiation [21]. Participants learned a negotiation strategy, practiced negotiating safer sex and condom use and resisting pressure to have unprotected sex in role-play scenarios, and critiqued one another’s role-play performances [18]. In a “Rugby Review Game,” teams competed for points for correctly answering questions about material covered in the intervention [21]. Participants wrote a “Letter to Self” promising to practice safer sex and placed it in a self-addressed envelope that was mailed to them 6 weeks later as a reminder of their commitment [19].
The comparison condition was a health-promotion intervention designed to control for nonspecific features, including group interaction and special attention [22]. It contained activities similar to the HIV risk-reduction intervention, but focused on physical activity, fruit and vegetable consumption, and alcohol use—behaviors linked to risk of non-communicable diseases, including heart disease, hypertension, stroke, diabetes, and certain cancers, that are leading causes of morbidity and mortality among South Africans [23–26]. We conducted a preliminary pilot test of the interventions with 24 students from the study population randomized to the 2 interventions to gain information to help make final revisions to the study protocols.
The co-facilitators were 16 postgraduate students at the university (6 women and 10 men) aged 24–49 years (mean = 27.6; SD = 5.6) who had previously worked as HIV education peer educators. The focus groups had suggested that we employ as facilitators postgraduate students rather than the third or fourth year undergraduates we originally planned. The process of selecting facilitators involved oral and performance-based interviewing. We randomly assigned facilitators to a 5-day training to implement 1 of the 2 interventions. In this way, we randomized facilitators’ characteristics across interventions [27]. During the training, the trainers modeled the intervention activities and the facilitators learned their assigned intervention, practiced implementing it, received feedback, and created common responses to potential issues that might arise during implementation. The importance of fidelity to the intervention was emphasized, as was the importance of confidentiality. All facilitators were certified upon successful completion of the training, and only certified facilitators worked in the trial.
Data Collection and Measures
The participants completed confidential questionnaires before the intervention, immediately after it, and 6 and 12 months after the intervention via audio computer-assisted self-interviewing (ACASI). Sexual behavior data were collected at baseline and the 2 follow-up assessments, whereas psychological variables were measured at all 4 assessments. Facilitators were not involved in the data collection, and data collectors were blind to participants’ intervention. Data collectors received a 3-day training that included modeling of data-collection procedures and practice with performance feedback. All data collection was completed by March 2010.
The primary outcome measure was frequency of unprotected vaginal intercourse assessed using the question, “In the past three months, on how many days did you have vaginal intercourse without using a condom?” Vaginal intercourse was defined as “your penis in a female’s vagina” (male version) or “a male’s penis in your vagina” (female version). The secondary outcome measures included other sexual risk behaviors in the previous 3 months and psychological variables. Participants reported their frequency of condom use during vaginal intercourse on a scale from never (1) to always (5). Frequency of vaginal intercourse was the number of days on which they reported having vaginal intercourse. Multiple partners was the report of having two or more vaginal partners.
We took several steps to increase the validity of self-reported sexual behavior. To facilitate the students’ ability to recall, we asked them to report their behaviors during a brief period (i.e., past 3 months), wrote the dates comprising the period on a whiteboard, and gave them calendars clearly highlighting the period. We stressed the importance of responding honestly, informing them that their responses would be used to create programs for other students like themselves and that we could do so only if they answered the questions honestly. We assured the participants that their responses would be kept confidential and that code numbers rather than names would be used on the questionnaires. Participants signed an agreement pledging to answer the questions honestly, a procedure that has been shown to yield more valid self-reports regarding sensitive issues [28].
Variables from the social cognitive theory [11] that the intervention targeted were measured with 5-point Likert scales used in previous studies [4, 7]. Outcome expectancies were measured with 15 items concerning the beliefs that condoms do not interfere with sexual enjoyment, partners would react positively to condom use, and condoms can prevent STI, HIV, and pregnancy (α = 0.84). Self-efficacy to use condoms was measured with 16 items concerning participants’ confidence they could use condoms skillfully, negotiate condom use, have condoms available when needed, and control themselves enough to use condoms; α = 0.82). In addition, HIV risk-reduction knowledge was the number correct on 21 true–false items regarding the transmission and consequences of AIDS and STIs, and knowledge specific to condom use was the number correct on 4 true–false items. Participants also evaluated the interventions. A 5-item scale measured how much participants liked their intervention (α = 0.81). A 2-item scale measured how much they thought they learned (α = 0.67). One item measured the extent to which they would recommend it to others.
The CAGE [29] was used to assess lifetime alcohol dependence and alcohol problems were denoted by CAGE scores greater than or equal to 2.
As compensation for participating in the data collection we gave each student a R120 grocery shop voucher, a certificate of completion, and a t-shirt with study logo at the immediate post-intervention assessment; a R60 voucher and a portfolio with study logo at the 6-month follow-up; and a R100 voucher and a backpack with study logo at the 12-month follow-up. The value of the rand to the dollar fluctuates greatly. At the time of informed consent, R1 was worth about $0.10.
Sample Size and Statistical Analyses
This trial is a pilot study and therefore has statistical power to detect only relatively large effects, not the typical effect sizes obtained in HIV risk-reduction intervention studies. Accordingly, the a priori power analysis assumed a one-tailed test for the primary outcome intent-to-treat analysis because the sample size was small and we had a firm basis for a directional hypothesis. Alpha = 0.05, one-tailed, and a final sample of 170 based on 15% attrition was projected to yield 80% power to detect an effect of Cohen’s d = 0.38 standard deviations on the primary outcome, the frequency of unprotected vaginal intercourse.
We used Chi-square and t tests to identify variables that predicted attrition and descriptive statistics to summarize the participants at baseline on sociodemographic and outcome variables. We tested the efficacy of the HIV risk-reduction intervention averaged over the post-intervention assessments by using a linear, logistic, or Poisson generalized estimating equations regression model depending on the type of outcome variable (continuous, binary, or count, respectively), and properly adjusting for longitudinal repeated measurements on students clustered within intervention groups [30, 31]. The models included baseline measure of the criterion, intervention condition, time (two categories representing 6-, and 12-month follow-up), sex, age group (coded 18 to 20 years or 21 to 24 years), nationality (coded South African or non-South African), and the Intervention-Condition × Nationality interaction. We specified an unstructured working correlation matrix in both the estimation of the model parameters and the robust sandwich estimators of the standard errors of these estimates.
In the case of the ordinal variable, frequency of condom use during vaginal intercourse in the past 3 months, we used a proportional odds GEE model with an independent working correlation matrix and did not control for baseline measure because the small number of participants reporting recent sexual intercourse at both baseline and follow-up would have severely limited the sample size. We report the estimated mean differences and corresponding 95% confidence intervals (CIs) for continuous measures, odds ratios (ORs) and corresponding 95% CIs for ordinal measures, rate ratios (RRs) and corresponding 95% CIs for binary measures, and event rate ratios and 95% CIs for counts to compare outcomes between intervention conditions.
Alpha was set at 0.05 one-tailed for the planned comparison of HIV intervention versus control on the primary outcome, unprotected sexual intercourse. All other analyses used two-tailed tests. Analyses were performed using an intent-to-treat mode with participants analyzed based on their intervention assignment regardless of the number of intervention or data-collection sessions attended. All analyses were completed using SAS V9.
Role of the Funding Source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or the writing of the report.
Results
Characteristics of the Sample
Table 2 summarizes selected participant characteristics at baseline by intervention condition. About 53.4% of participants were women; 46.6% were men. Age ranged from 18 to 25 years, with a mean of 20.8 (SD = 1.49). About 86.4% lived on campus. None of the participants were married. About 58.0% were Zimbabwean, 36.4% were South African, and 5.7% were from other countries. About 64.2% reported having experienced coitus at least once, and 47.2% reported having coitus in the previous 3 months. About 11.4% reported ever being pregnant or making someone pregnant and 8% reported having a child. About 35.8% reported having problems with alcohol on the CAGE, and 4.0% reported using dagga (marijuana) in the past 30 days.
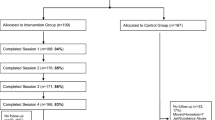
Intervention Attendance and Follow-up Retention
Figure 1 shows the flow of the participants through the trial. Of the 240 eligible students, 201 competed the baseline assessment, and 176 (73.3%) were randomized. Among the eligible students, only 64 (53.3%) South Africans compared with 112 (93.3%) of non-South Africans were randomized (χ2 = 49.09, P < 0.0001). The percentage of eligible women (78.3%) and men (68.3%) randomized was not significantly different (χ2 = 3.07, P = 0.08).
Attendance at intervention and data-collection sessions was excellent. A total of 173 (98.3%) attended Intervention Session 1, and 156 (88.6%), 161 (91.5%), and 170 (96.6%) attended sessions 2–4, respectively. The number of intervention sessions attended did not differ between the HIV (mean = 3.66) and health control (mean = 3.85) interventions, F (1, 171) = 3.69, P = 0.056. However, nationality affected the number of sessions attended. South Africans (mean = 3.41) attended fewer intervention sessions than did non-South Africans (mean = 3.95), F (1, 171) = 24.86, P < .0001. A significant Intervention × Nationality interaction, F (1, 171) = 6.81, P = .010, indicated that South Africans attended fewer HIV (mean = 3.18) sessions than health promotion (3.67) sessions whereas non-South Africans attended a similar number of HIV (mean = 3.95) and health promotion (3.95) sessions.
Of the trial participants, 173 (98.3%) attended at least 1 of the 2 follow-ups: 171 (97.2%) attended the 6-month and 171 (97.2%) attended the 12-month. The interventions did not differ significantly in retention at follow-up. Attending a follow-up session was unrelated to the age, sex, nationality, sexual behavior outcomes, or psychological variables.
Effects on Outcome Variables
Table 3 presents outcome variables by intervention condition and time. Table 4 presents event rate ratios, odds ratios, rate ratios, and mean differences and corresponding 95% confidence intervals for intervention efficacy on sexual behavior outcomes and psychological variables. As hypothesized, averaged over the 2 follow-up assessments, the HIV risk-reduction intervention had a significant effect on the primary outcome variable. Participants in the HIV risk-reduction intervention reported fewer days on which they had unprotected sexual intercourse than did those in the health promotion intervention (Z = −2.01, P = .022, one-tailed). The model-estimated number of unprotected acts was 0.553 (SE = 0.016) in the HIV risk-reduction intervention and 1.173 (SE = 0.090) in the health promotion intervention. In addition, a significant Intervention × Nationality interaction (Z = 3.02, P = 0.0025) indicated that the intervention caused a greater reduction in unprotected intercourse among the non-South African students compared with South African students. Among non-South Africans, the model-estimated number of unprotected acts was 1.677 (SE = 0.114) in the health promotion intervention and 0.427 (SE = 0.012) in the risk-reduction intervention. Among South Africans, in contrast, the model-estimated number of unprotected acts was 0.250 (SE = 0.009) in the health promotion intervention and 0.764 (SE = 0.020) in risk reduction.
As shown in Table 4, the HIV intervention had a significant effect on the rated frequency of condom use in the previous 3 months. Participants in the HIV intervention were more likely to report more frequent condom use during sex than were those in the health promotion intervention. The model-estimated probability of higher ratings of condom use was 0.766 (SE = 0.007) in risk reduction and 0.696 (SE = 0.008) in health promotion. A significant Intervention × Nationality interaction (Z = −2.40, P = 0.016) indicated that the HIV risk-reduction intervention compared with health control caused a greater increase in the odds of reporting more frequent condom use among non-South Africans than among South Africans. Among non-South Africans, the model-estimated probability of higher ratings of condom use was 0.812 (SE = 0.007) in risk reduction and 0.648 (SE = 0.011) in health promotion. Among South Africans, the model-estimated probability of higher ratings of condom use was 0.784 (SE = 0.011) in health promotion and 0.689 (SE = 0.013) in risk reduction.
Neither the main effects of the intervention nor the interactions with nationality were significant on frequency of sex or incidence of multiple partnerships.
The HIV risk-reduction intervention had significant effects on the psychological variables averaged over the 3 post-intervention assessments. As shown in Table 4, students who received the HIV risk-reduction intervention scored higher in condom-use outcome expectancies, self-efficacy to use condoms, HIV risk-reduction knowledge, and condom use knowledge. No Intervention × Nationality interactions were statistically significant on the psychological variables.
Evaluations of the Interventions
Participants’ evaluative ratings of the interventions were high (means for both intervention groups were greater than 4.6 on 5-point scales) and did not differ by intervention arm. Non-South African students compared with South African students said they liked the interventions more (means = 4.71 and 4.60, respectively; F[1, 166] = 4.68, P = 0.032) and learned more (means = 4.94 and 4.83, respectively; F[1, 166] = 7.36, P = 0.007) from the interventions. Nationality did not influence significantly the difference between evaluations of the HIV intervention compared to the health control intervention.
No adverse events occurred during the study.
Discussion
The present results revealed that the university students in the HIV risk-reduction intervention reported less unprotected sexual intercourse and more frequent use of condoms than did those in the health promotion control intervention. Paralleling this, in the HIV risk-reduction intervention, compared with the health promotion control intervention, participants expressed greater endorsement of psychological variables supportive of condom use, including condom-use outcome expectancies and self-efficacy to use condoms, and scored higher in HIV risk-reduction knowledge, including condom-use knowledge. Moreover, both interventions were acceptable. Large percentages of randomly selected students participated, attended the overwhelming majority of intervention sessions, and gave high evaluations of the interventions. However, the intervention did not decrease the self-reported frequency of sexual intercourse or incidence of multiple partners.
The HIV risk-reduction intervention’s effects on self-reported unprotected sex and condom use may have been occasioned by several factors. We drew upon social cognitive theory integrated with information from formative research with the population. The intervention included activities designed to address the specific outcome expectancies and self-efficacy beliefs of the population, which helped to make the intervention contextually appropriate. Thus, the approach of strengthening favorable outcome expectancies, reducing unfavorable outcome expectancies and buttressing skills and self-efficacy to engage in the specific behaviors may account for the effects of the intervention.
The findings are in accord with other studies of interventions to reduce sexual risk behaviors among young people, but few studies have tested interventions with university students in sub-Saharan Africa [8], where HIV is having its most devastating impact. In addition, none of the studies with university students in sub-Saharan Africa employed randomized controlled designs [32, 33].
There were also differences by nationality. South Africans compared with non-South Africans were less likely to enroll in the study, attended slightly fewer intervention sessions, and rated the interventions somewhat less favorably. Most important, the HIV risk-reduction intervention caused a greater decrease in unprotected sex and a greater increase in condom use among non-South Africans than among South Africans. We would speculate that differences between the South African and non-South African students may at least in part account for the differences in results. Because the university was located in rural Eastern Cape Province South Africa, the South African students could go home easily and accordingly were less of a captive audience than were the non-South African students who may have been motivated to take part in on-campus extracurricular activities since their off-campus opportunities would have been more limited. Another difference is that the non-South African students tended to be of higher socioeconomic background than the South African students, which might reflect different motivational tendency for involvement in health promotion opportunities. Future research will have to explore empirically the reasons for the differential results.
This study had several limitations. This was a pilot study and thus the sample size was relatively small. The outcomes were measured with self-reports, which can be influenced by socially desirable responding. However, the use of ACASI may have mitigated potential problems with self-report validity [34, 35]. Nevertheless, the study might have been improved if it had included objective measures of STI incidence. The study also had important strengths. It employed a randomized controlled design, a theory-based contextually appropriate intervention, and a dose and modality equivalent comparison intervention, controlling for group interaction and special attention. The retention rate was high and did not differ by intervention arm. Randomly sampling participants increased generalizability.
Conclusions
In conclusion, the high rates of reported pregnancy and STI and the estimated 3.4% prevalence rate of HIV among university students in South Africa suggest that university students in sub-Saharan Africa are at high risk for morbidity and mortality from HIV. Accordingly, this study, which demonstrated that a theory-based contextually appropriate intervention that teaches skills caused positive changes on unprotected sex and condom use in sub-Saharan African university students, is important. Future studies must explore the generalizability of the findings to objective outcome measures of STI with a larger sample. In addition, there is a need for research into HIV prevention programming that will engage South African students, who attended fewer intervention sessions and benefitted less from the present intervention than did non-South African students. We are optimistic that the present study offers an approach that may help reduce sexual risk behaviors among university students in sub-Saharan Africa.
References
UNAIDS. AIDS epidemic update: December 2009. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO); 2010.
UNAIDS 2006 report on the global AIDS epidemic Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO) Geneva 2006.
Merson MH, Dayton JM, O’Reilly K. Effectiveness of HIV prevention interventions in developing countries. Aids. 2000;14(Suppl 2):S68–84.
Heeren GA, Jemmott JB III, Mandeya A, Tyler JC. Theory-based predictors of condom use among university students in the United States and South Africa. AIDS Educ Prev. 2007;19(1):1–12.
Eng TR, Butler WT. The hidden epidemic: confronting sexually transmitted diseases. Washington, DC.: National Academy Press; 1997.
Higher Education HIV and AIDS Programme (HEAIDS). HIV prevalence and related factors–higher education sector, South Africa, 2008–2009. Pretoria: Higher Education South Africa; 2010.
Shisana O, Rehle T, Simbayi LC, et al. South African national HIV prevalence, incidence, behaviour and communication survey, 2008. Cape Town: HSRC Press; 2009.
Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: their impact on sexual behaviors of young people throughout the world. J Adolesc Health. 2007;40(3):206–17.
Chetty D. Institutionalising the response to HIV/AIDS in the South African university sector: a SAUVCA analysis. Pretoria: SAUVCA Occasional Publications and Reports; 2000.
Mogobe KD, Seboni N, Brown MS, Ntsayagae E, Sebego M, Sabone M. HIV/AIDS education, prevention and control course (BNS101): the way forward. J Assoc Nurses AIDS Care. 2007;18(6):22–31.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986.
Jemmott JB III, Jemmott LS, O’Leary A, et al. Cognitive-behavioural health-promotion intervention increases fruit and vegetable consumption and physical activity among South African adolescents: a cluster-randomised controlled trial. Psychol Health. 2011;26(2):167–85.
Jemmott JB III, Jemmott LS, O’Leary A, et al. School-based randomized controlled trial of an HIV/STD risk-reduction intervention for South African adolescents. Arch Pediatr Adolesc Med. 2010;164(10):923–9.
Kalichman SC, Simbayi LC, Cloete A, et al. Integrated gender-based violence and HIV risk reduction intervention for South African men: results of a quasi-experimental field trial. Prev Sci. 2009;10(3):260–9.
Kalichman SC, Simbayi LC, Vermaak R, et al. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Ann Behav Med. 2008;36(3):270–9.
Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2007;44(5):594–600.
Heeren GA, Jemmott JB III, Mandeya A, Tyler JC. Sub-Saharan African university students’ beliefs about condoms, condom-use intention, and subsequent condom use: a prospective study. AIDS Behav. 2009;13(2):268–76.
Jemmott JB III, Jemmott LS, Fong GT, Morales KH. Effectiveness of an HIV/STD risk-reduction intervention for adolescents when implemented by community-based organizations: a cluster-randomized controlled trial. Am J Public Health. 2010;100(4):720–6.
Jemmott JB III, Jemmott LS, Fong GT. Efficacy of a theory-based abstinence-only intervention over 24 months: a randomized controlled trial with young adolescents. Arch Pediatr Adolesc Med. 2010;164(2):152–9.
El-Bassel N, Jemmott JB, Landis JR, et al. National Institute of Mental Health Multisite Eban HIV/STD Prevention Intervention for African American HIV Serodiscordant Couples: a cluster randomized trial. Arch Intern Med. 2010;170(17):1594–601.
Jemmott JB, III, Jemmott LS, O’Leary A, et al. Neighborhood-based randomized controlled trial of an HIV/STD risk-reduction intervention for South African men. Philadelphia: Department of Psychiatry, Perlman School of Medicine, University of Pennsylvania; 2011.
Cook T, Campbell D. Quasi-experimentation: design and analysis for field settings. Chicago: Houghton Mifflin; 1979.
Alberts M, Urdal P, Steyn K, et al. Prevalence of cardiovascular diseases and associated risk factors in a rural black population of South Africa. Eur J Cardiovasc Prev Rehabil. 2005;12(4):347–54.
Asfaw A. The effects of obesity on doctor-diagnosed chronic diseases in Africa: empirical results from Senegal and South Africa. J Public Health Policy. 2006;27(3):250–64.
Joubert J, Norman R, Lambert EV, et al. Estimating the burden of disease attributable to physical inactivity in South Africa in 2000. S Afr Med J. 2007;97(8 Pt 2):725–31.
Schneider M, Norman R, Steyn N, Bradshaw D. Estimating the burden of disease attributable to low fruit and vegetable intake in South Africa in 2000. S Afr Med J. 2007;97(8 Pt 2):717–23.
Jemmott JB III, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized controlled trial. J Am Med Assoc. 1998;279(19):1529–36.
Sudman S, Bradburn NM. Response effects in surveys. Chicago: Aldine; 1974.
Ewing J. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905–7.
Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22.
Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New York: John Wiley & Sons; 2004.
Miller AN, Mutungi M, Facchini E, Barasa B, Ondieki W, Warria C. An outcome assessment of an ABC-based HIV peer education intervention among Kenyan university students. J Health Commun. 2008;13(4):345–56.
Terry PE, Mhloyi M, Masvaure T, Adlis S. An examination of knowledge, attitudes and practices related to HIV/AIDS prevention in Zimbabwean university students: comparing intervention program participants and non-participants. Int J Infect Dis. 2006;10(1):38–46.
Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–73.
Metzger DS, Koblin B, Turner C, et al. Randomized controlled trial of audio computer-assisted self-interviewing: utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. Am J Epidemiol. 2000;152(2):99–106.
Acknowledgments
The research reported in this article was supported, in part, by grant R34 MH078803 from the National Institute of Mental Health. The authors gratefully acknowledge the assistance of Lynette Gueits, MS, and Jillian Baker, PhD, in developing the interventions, Mandisa Magwa, MS, Phyllis Moore, MSW, Xoliswa Mtose, PhD, and Marcia Penn, MS, in training of facilitators, Janet Hsu, BS, in management of data and data collector training, and Raymond Chiruka, MSc, Jessica Batidzirai, MSc, Arnold Gwaze, MSc, and Show Marange, MSc, in data collection, recruitment, and retention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heeren, G.A., Jemmott III, J.B., Ngwane, Z. et al. A Randomized Controlled Pilot Study of an HIV Risk-Reduction Intervention for Sub-Saharan African University Students. AIDS Behav 17, 1105–1115 (2013). https://doi.org/10.1007/s10461-011-0129-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-0129-2