Abstract
Russia has seen one of the world’s fastest-growing HIV epidemics. Transmission risk behavior, HAART-taking, and psychosocial distress of the growing population of Russian people living with HIV (PLH) in the HAART era are understudied. Participants of a systematically-recruited cross-sectional sample of 492 PLH in St. Petersburg completed measures of sexual and drug injection practices, adherence, perceived discrimination, and psychosocial distress. Since learning of their status, 58% of participants had partners of HIV-negative or unknown serostatus (mean = 5.8). About 52% reported unprotected intercourse with such partners, with 30% of acts unprotected. Greater perceived discrimination predicted lower condom use. A 47% of IDU PLH still shared needles, predicted by having no primary partner, lower education, and more frequently-encountered discrimination. Twenty-five percentage of PLH had been refused general health care, 11% refused employment, 7% fired, and 6% forced from family homes. Thirty-nine percentage of participants had probable clinical depression, 37% had anxiety levels comparable to psychiatric inpatients, and social support was low. Of the 54% of PLH who were offered HAART, 16% refused HAART regimens, and 5% of those on the therapy took less than 90% of their doses. Comprehensive community services for Russian PLH are needed to reduce AIDS-related psychosocial distress and continued HIV transmission risk behaviors. Social programs should reduce stigma and discrimination, and promote social integration of affected persons and their families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Russia has seen one of the most rapidly-escalating HIV epidemics in the world, and highly-active antiretroviral therapy (HAART) became widely available in the country only in the past few years [1]. Access to contemporary HIV treatment in Russia has introduced a major shift from what had been a deadly disease to a potentially more manageable one. Little is known about the psychosocial needs and mental health characteristics, HIV transmission risk behavior practices, and treatment adherence of people living with HIV (PLH) in HAART-era Russia, and this is the first study to examine these characteristics in a large, systematically-recruited sample.
Widescale social, psychological, discrimination, and health care access problems as well as AIDS stigma are commonly encountered by Russian PLH, experiences that negatively affect life quality [2]. Research undertaken before HAART became available also showed that many HIV-positive persons engaged in unprotected sex and shared needles. In a 2002 sample of PLH in St. Petersburg, Russia’s second largest city, most IDUs continued to share needles and about half of PLH reported unprotected intercourse with serodiscordant/status-unknown partners. Mental health problems were widespread [3].
Russia’s AIDS epidemic began in the late-1990s and first primarily affected Russia’s approximately 1.6 million injection drug users (IDUs) [4]. However, the proportion of incident HIV infections attributable to heterosexual transmission increased from 6% in 2001 to 35% in 2008 [5]. To date, 516,167 HIV infections have been officially recorded in Russia [6]. However, the true number of infections is believed to be 940,000, establishing the country’s prevalence at a level of 1.1%. Between 23,000 and 71,000 persons have died of AIDS as of 2007 [7]. In St. Petersburg alone, almost 40,000 HIV infections and 1,726 deaths were officially recorded by 2009 [5], but the true number of infections is probably much higher. A recent review found HIV prevalence of between 8 and 64% among IDUs depending upon region in the country, and up to 9% among MSM, up to 8% among commercial sex workers (CSWs), and 5% among prisoners [8].
Russia’s HIV epidemic has particularly affected young people, with HIV prevalence of 1.3% among 15- to 24-year-olds [7]. About 73% of infected individuals in Russia are under age 30 [5] compared with about 30% in the U.S. [9]. A recent study found an alarming 37% HIV prevalence rate in a large community sample of St. Petersburg street children [10]. There has been a steady annual increase in the proportion of infections among females who are neither IDUs nor sex workers. Currently, females account for 33.5% of all persons with HIV in Russia, and 42% of the incident cases in 2008 [5].
In western countries, extensive prior research has explored levels of transmission risk behavior and treatment adherence in community samples of PLH [11–15]. In addition, recent attention has been directed to the manner in which psychosocial distress, substance use, and sociodemographic characteristics may affect ongoing transmission risk behavior and treatment adherence [16–18]. In spite of Russia’s widescale HIV/AIDS epidemic, no systematic, empirical studies have examined the psychosocial and behavioral circumstances of persons living with HIV infection in Russia since a 2002 study [3] showing pervasive and severe mental health problems, discrimination, and high levels of continued risk behavior. Since that time, contemporary antiretroviral therapies have become more widely available in Russia. Adherence to HAART has been identified as a major national AIDS-related challenge in Russia [8]. However, little to date is also known about HAART adherence rates and barriers among Russian PLH. In addition, HIV epidemiology in the country is changing from a pattern of IDU-associated transmission to one increasingly characterized by sexual transmission. HIV has become an established epidemic in Russia, and the proportion of women among PLH has increased. For these reasons, there is a need to update public health knowledge about psychosocial needs and transmission risk behaviors among Russian PLH and to characterize their access and adherence to HAART regimens.
The aims of this study were to (a) identify the prevalence of sexual and needle-sharing transmission risk behavior practices among PLH in St. Petersburg; (b) describe their psychosocial and mental health characteristics; (c) assess their HAART adherence levels, and (d) identify factors associated with continuing transmission risk behavior practices and HAART nonadherence.
Methods
Carried out during 2008–2009, this study was approved by the IRBs of the Medical College of Wisconsin and Botkin Clinical Infectious Disease Hospital in St. Petersburg. In a preparatory research phase, local experts and key informants were consulted to identify all agencies in St. Petersburg that were known to provide medical and social services to PLH. These agencies included the city’s specialized AIDS center, two infectious disease hospitals, four PLH self-support groups, and an AIDS nongovernmental organization. All eligible PLH clients present in each agency setting over a 4-month period were approached and asked to participate. Clients were eligible to participate in the study if they had not already completed the assessment, were age 15 or older, did not exhibit signs of substance use impairment, and agreed to participate. About 80% of those approached by professionally-trained study staff provided informed consent and completed the anonymous self-administered measure battery (n = 492). The main reason for declining to participate in the 40-min assessment was lack of time. Incentives of approximately $10 value compensated participants for their time.
Measure
Sociodemographic Indicators
Participants were asked their age, gender, education level, marital status, current sexual identity, and length of HIV-positive status knowledge. Respondents indicated if they were currently in school or employed.
HIV Disclosure and Perceived Discrimination
Participants indicated to whom they disclosed their positive HIV status and whether HIV testing was with their consent. The measure then listed 12 situations representing potential types of AIDS-related discrimination regarding employment, social relations, health care, and breach of confidentiality. Participants used four-point scales to report how often they encountered each situation.
Sexual Behavior Indicators
Respondents indicated their number of lifetime opposite- and same-gender partners, number of partners since learning about their HIV-positive status, and—of these—their number of HIV-negative or status-unknown partners. Participants were then asked whether and how often they had vaginal or anal intercourse with opposite- and with same-gender HIV-negative or unknown status partners since learning about their own HIV-positive status, and how often they used condoms from 0 (never) to 100% (always).
Substance Use and Needle Sharing Behavior
Participants specified how many alcohol drinks they consumed per week and whether they used any kind of illicit drugs in the past 3 months. Participants marked how often they used marijuana, hallucinogens, ecstasy, heroin, recreational psychotropic medications, and other drugs common in Russia. Finally, participants indicated whether they ever injected drugs, and—if so—frequency of injection and sharing needles in the past 3 months.
HAART Treatment and Adherence Measures
Participants were asked whether they were receiving HAART. Those on HAART completed an adherence measure [19], responding to questions about the number of medication pills prescribed and then the number of pills actually taken on each of the past 2 days before the assessment. Participants indicated whether they interrupted or discontinued therapy since beginning their regimen. Using multiple response options, participants then specified reasons for missing doses and for treatment discontinuation.
Depression
The Center for Epidemiological Studies of Depression Scale (CES-D [20, 21]) consists of 20 statements that tap cognitive, affective, and somatic aspects of depression that do not highly overlap with symptoms of HIV infection [22]. Respondents used four-point scales to indicate on how many days of the past week each depressive feeling occurred (sample item: ‘I had crying spells’) (Cronbach’s alpha, present sample = 0.89).
State Anxiety
State anxiety was assessed with the State-Trait Anxiety Inventory, Form Y-1 (STAI [23]), on which respondents used four-point scales to indicate how much 20 statements describe feelings indicative of current anxiety (sample item: ‘I am tense’). STAI scores range from 20 to 80 (Cronbach’s alpha = 0.89).
Social Support
The Social Provisions Scale (SPS [24, 25]) consists of 24 items that measure perceived social support (sample item: ‘There are people I can depend onto help me if I really need it’). Respondents used four-point response options to indicate their level of agreement with each statement (score range, 24–96, Cronbach’s alpha = 0.90). In prior studies with HIV-infected persons, SPS scores predicted depression and continued high-risk behavior [26] and also improved following psychotherapy [27].
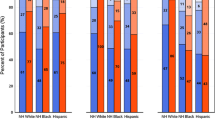
Statistical Methods
Univariate tests were conducted for demographic factors, psychosocial scales, STD history, sexual activities, and HAART treatment adherence variables broken down first by gender (males, n = 252 and females, n = 238; two participants did not indicate their gender) and then by probable mode of HIV exposure. Participants were defined as IDUs if they ever injected drugs and as MSM if they were males who reported lifetime sexual activity with men. Accordingly, four mutually exclusive subgroups were coded: non-MSM IDUs (both males and females, hereafter referred to as “IDUs,” n = 312), MSM IDUs (n = 34), non-IDU MSM (“MSM,” n = 24), and heterosexuals, males and females who were neither IDUs nor MSM (n = 118). Four participants who did not indicate if they injected drugs and two who did not report on same-sex activities were excluded. The statistical significance of gender differences was assessed by Pearson’s chi square for categorical data and the Mann–Whitney ranks test for all numerical measures. For HIV exposure mode subgroups, we first performed chi square tests or Kruskal–Wallace ranks tests to examine whether there was a significant overall difference among subgroups. If overall significance was found, multiple pairwise comparison tests (chi square or Dunn’s pairwise tests of mean ranks) determined the significance of intergroup differences at P < 0.05.
Based on prior research [16–18], we hypothesized that levels of transmission risk behavior and medication nonadherence would be associated with demographic characteristics, indicators of mental health distress, and substance use. Therefore, we used these variables in multivariate tests to predict condom use, needle-sharing, and HAART adherence by conducting least squares and logistic regression analyses. For each outcome, a series of univariate regressions evaluated sociodemographic characteristics, psychosocial scales, perceived AIDS-related discrimination experiences, and substance use variables. All predictors that attained a minimum P-value of 0.10 in the univariate analysis were then entered as covariates in a multiple regression model for that outcome.
Results
Participants
Table 1 shows participant demographic characteristics, overall and broken down by gender and by subsample. Participant mean age was 30.2 years and slightly varied across subgroups. Participants knew about their HIV-positive status for an average of 58.2 months. Both IDUs and IDU MSM knew of their HIV positive status for the longest periods and the heterosexual subgroup for the shortest period.
Patterns of Serostatus Disclosure and Perceived AIDS-Related Discrimination
Serostatus Disclosure
Respondents most often shared information about their HIV status with close family members (80%, n = 393), close friends (76%, n = 372), and other HIV-positive people (68%, n = 335). With respect to circumstances surrounding testing, 70% of participants (n = 342) said that their testing was voluntary, 21% (n = 105) were tested without their knowledge, and 8% (n = 38) said testing was forced.
Discrimination Situations
Table 2 shows the prevalence of perceived AIDS-related discrimination events encountered by persons in the sample. Nearly 25% of persons said they had been refused general health care, 16% refused dental care, and 21% isolated from other patients in a hospital or clinic because of their HIV status. A 9% of persons said they had been refused health care for their HIV disease. Sixteen percentage of participants were forced by physicians—and 6% by police—to provide information about their sexual or drug use partners, and 13% were forced by police to provide personal information about themselves. About 12% of participants said they were forced by physicians or police to sign a written statement declaring their HIV positive status, a procedure used to create evidence that may form the basis for criminal charges against those suspected of putting others at risk. About 11% were refused a job offer, 7% had been fired from their jobs, and 6% forced by family members to leave their homes because of their HIV status.
Psychosocial Adjustment of Persons Living with HIV/AIDS
Psychosocial scale results are presented in Table 3. The mean CES-D score was 20.6, with IDUs and IDU MSM both having significantly greater depression than the heterosexual subgroup. Using established CES-D cutoffs for interpreting levels of depression [20], 67.4% of persons (n = 230) scored at or above 16, the indicator of possible clinical depression, and 39.0% (n = 191) scored at or above 23, indicating probable clinical depression and major depressive symptomatology. The mean SPS total score for this sample was 74.0 (n = 361), similar to the levels of social support found in a sample from the USA of HIV positive persons seeking mental health services before HAART was available [27]. Females’ social support scores were significantly higher than those of males, and also higher among the heterosexual subgroup than among IDUs. Finally, the mean STAI anxiety score was 44.2 (n = 412). About 51.3% (n = 251) of participants scored at or above 43, comparable to medical patients with psychiatric components to their health problems [23]. A total of 37.0% (n = 181) of participants scored at or above 48 on the STAI, scores comparable to those found among psychiatric inpatients [23].
Transmission Risk Behavior Among Persons Living with HIV/AIDS
Numbers of Sexual Partners
As shown in Table 3, participants reported 48.4 (median = 15) lifetime opposite-sex partners. Non-IDU MSM reported a mean of 94.3 (median = 30) lifetime same-sex partners. The greatest number of opposite-gender partners was reported by IDU MSM (mean = 126.5, median = 15 partners), while the number of same-sex partners in this subgroup was lower (mean = 116.7, median = 1 partner). Since learning about their HIV positive status, participants in the sample as a whole reported a mean of 5.4 (median = 1) opposite-gender seronegative partners or partners of unknown serostatus, and a mean of 2.4 (median = 1) opposite-gender seropositive partners. As Table 3 shows, participants reported more HIV-negative sexual partners or partners whose serostatus was unknown than seroconcordant partners since learning of their HIV-positive status.
Sexual Practices with HIV Negative or Status-Unknown Partners Since HIV Diagnosis
As Table 3 shows, 58% of sample members engaged in sex with opposite-gender HIV-negative or status-unknown partners, and 71% of non-IDU MSM had same-sex partners not known to be seroconcordant. Of them, a majority (52%) had some unprotected acts of vaginal or anal intercourse, and approximately one-third of all intercourse acts were unprotected.
STD History Since HIV Diagnosis
Almost 14% (n = 67) of participants reported having an STD since HIV positive diagnosis, with the greatest proportion (17%, n = 4) among MSM.
Drug Injection and Needle-Sharing Practices
As shown in Table 3, of the 346 IDUs in the sample, 52% (n = 180) injected drugs during the past 3 months, and 36% (n = 125) did so at least weekly. About 47% (n = 85) shared needles in the past 3 months, and almost one-third of them (n = 25) shared needles at least weekly. Since IDUs in the sample knew of their HIV-positive status for an average of nearly 5 years, almost all of these needle-sharing events took place after learning of their positive serostatus.
HAART Adherence
As Table 4 shows, 267 of the 492 participants in the sample (54%) had been offered HAART. Of them, 66.3% (n = 177) were currently on a HAART regimen, 17.6% (n = 47) had not yet initiated the therapy, and 16.1% (n = 43) refused their recommended HAART treatment. Participants on HAART reported being on the regimen for a mean of 19.9 months. Only 4.8% (n = 8) of participants missed at least 10% of their medication doses in the past 2 days, the level of nonadherence shown to produce suboptimal clinical response to antiretroviral regimens [28, 29]. The most common reasons for missing medication—each reported by ≥10% of participants—were forgetting to take the medicine, being away from home, running out of pills, and experiencing unwanted side effects. With respect to interruption of a HAART regimen, the most common reasons were adverse effects, running out of medication, and alcohol or drug use.
Multivariate Predictors of Risk Behaviors and HAART Taking
Table 5 reports significant multivariate predictors of risk behavior and HAART taking outcomes. As the table shows, percentage of condom use with HIV seronegative or status-unknown partners in the past 3 months was predicted by a single variable, number of AIDS-related discrimination situations encountered. Among participants who injected drugs in the past 3 months, any needle sharing was predicted by not having a primary partner, having no university education, perceiving a greater number of discrimination experiences, and a trend for greater depression.
The analyses also examined multivariate predictors of three HAART-taking outcomes. First, 225 participants (46%) had not been offered HAART. Multivariate predictors of not being offered HAART were fewer months since HIV diagnosis, presence of fewer HIV disease symptoms, and greater depression. Second, because 43 participants (16%) who were offered HAART did not accept it, we next examined multivariate predictors of HAART refusal. Depression and number of discrimination situations encountered both independently predicted refusal to take HAART. Third, and with respect to adherence, missing any medication dose in the past 2 days was predicted by the use of heroin in the past 3 months.
Discussion
HIV incidence in Russia and other post-Soviet countries has been among the world’s highest. The growth in number of people living with HIV in Russia is due to both negative and positive factors. On one hand, HIV incidence remains high in the region and contributes to the growth in cases. On the other hand, improved HAART access lowers disease mortality, resulting in longer life among persons with HIV in Russia. This study describes needs and behavioral characteristics of PLH in St. Petersburg, a major AIDS epicenter in Eastern Europe. Although not necessarily representative of the country, this study’s findings highlight important issues likely to characterize PLH elsewhere in the region.
High-risk sexual and needle sharing practices were common. Many participants had multiple partners since learning about their HIV positive status, and the number of participants reporting sex with HIV-negative or unknown status partners was high, particularly among IDUs, MSM, and IDUs who were also MSM. Over half of participants had unprotected intercourse with HIV-negative or status-unknown partners, and about one-third of intercourse acts with these partners were unprotected. Women and non-MSM IDUs reported the greatest levels of unprotected behavior. Further, over half of IDUs reported recent drug injection and almost a quarter of drug users shared needles in the past 3 months. These findings demonstrate the need to implement programs designed to encourage sexual risk reduction for infected persons seen in HIV clinical, social support, or other care service programs. The findings also highlight the need for improved harm reduction interventions directed toward PLH drug users who continue to share needles. Contemporary drug treatment is often unavailable in Russia, and Russian federal laws prohibit the use of opiate replacement therapies such as methadone. Such drug use policies may contribute to high levels of continuing drug use and needle sharing among IDU PLH in the country.
Nearly half of PLH in this sample reported that they had not been offered HAART. Clinicians in Russia usually follow traditional western guidelines for the initiation of antiretrovirals based on declining CD4 counts and disease progression, and this was borne out by the present study’s finding that shorter duration of positive serostatus and fewer HIV illness symptoms predicted not being offered HAART. Russian HIV care authorities acknowledge that the number of PLH in Russia in need of antiretroviral therapy greatly exceeds the number receiving it [30]. For example, as of 2008, 25% of all PLH were estimated to be in need of HAART, while only about half of this number were receiving it [30]. Steps to expand HAART access to cover persons requiring it based on current standards are urgently needed. Beyond this, “test and treat” strategies have recently been advocated and propose initiating antiretroviral therapy much earlier following HIV-positive diagnosis with the aim of decreasing infectivity to others [31]. If such early-treatment initiation is found to carry health and public health benefits, expanded use of HAART for PLH in Russia may need to take place.
A relatively high proportion of PLH reported that they declined a recommendation to begin HAART. Among those on the regimen, most participants reported that they took over 90% of their HAART medication doses in the last 2 days. This may be because contemporary HAART regimens are less complicated than in the past. However, we relied on self-reports of adherence for only a 2-day period, and self-report data can reflect an underreporting of socially undesirable responses. Access to HAART in Russia has been challenged by an insufficient HAART treatment service infrastructure with limited capacity to manage adverse treatment effects [32] and co-infections [33], and less opportunity for IDUs to receive HAART [1]. Additional studies need to employ more comprehensive methods to evaluate HAART treatment adherence and to identify reasons for treatment refusal.
Levels of depression, anxiety and poor social supports in this sample of Russian PLH were high and prevalent. Reports of discrimination were also common and show that AIDS-related stigma remains high in Russia. High prevalence and severity of emotional distress underscores the need to integrate improved mental health services into care programs for PLH in Russia. Attention to mental health indicators and AIDS-related stigma are important for the psychological well-being of PLH and also from a public health perspective, because both perceived discrimination and depression predicted engaging in high transmission risk sexual and needle-sharing practices as well as HAART therapy refusal.
Finally, some important differences emerge when comparing key findings of the current study with those from a 2002 pre-HAART report [3]. Although the samples were recruited in similar settings and ways, the mean age of PLH in the present sample was 5 years older and the mean duration of knowledge of one’s HIV positive serostatus was 5 years rather than the 2 years found in the 2002 sample. Consistent with national Russian HIV statistics, the representation of females was higher and the proportion of those reporting heterosexual exposure almost doubled between the 2002 and 2008 samples.
Differences were observed in sexual behavior between the 2002 and the current studies. Participants in the present sample reported greater numbers of sexual partners since learning about their HIV-positive status, perhaps because of their longer mean term of living with HIV. Of particular concern is that these differences were primarily due to a greater number of sexual partners not known to be seroconcordant. Further, over half of participants had unprotected intercourse with such partners. Modestly higher levels of condom use were found in 2008 relative to 2002. The approximately one-quarter of HIV-infected IDUs who reported needle-sharing in the past 3 months was slightly lower than the one-third who reported doing so in the 2002 study, but the current level of injection-related transmission behavior remains a cause of great public health concern.
The study has several limitations. Questionnaire-based assessments are subject to recall bias. The use of self-administered questionnaires rather than interview administration by ACASI may have resulted in the underreporting of stigmatized behavior. Because they were approached in medical, public health, and social service settings, participants’ responses may have been biased due to social desirability. Finally, this cross-sectional survey study—although representing PLH recruited from multiple access points—does not include individuals outside of care systems and those who declined to participate.
Policies and public health programs for PLH need to focus on comprehensive strategies to address continuing transmission risk behaviors as well as improve the psychosocial well-being, social circumstances, and other contexts in which these risks occur. It is imperative that PLH in Russia should receive improved and tailored services to reduce HIV transmission risk behaviors and improve life quality.
References
UNAIDS. Fact Sheet: Eastern Europe and Central Asia. December, 2009. Geneva: UNAIDS. http://data.unaids.org/pub/FactSheet/2009/20091124_FS_eeca_en.pdf. Accessed 27 Feb 2010.
Human Rights Watch. Lessons not learned: Human rights abuses and HIV/AIDS in the Russian Federation. 28 April 2004, D1605. http://www.hrw.org/sites/default/files/reports/russia0404.pdf. Accessed 27 Feb 2010.
Amirkhanian YA, Kelly JA, McAuliffe TL. Psychosocial needs, mental health, and HIV transmission risk behavior among people living with HIV/AIDS in St Petersburg, Russia. AIDS. 2003;17:2367–74.
United Nations Office on Drugs and Crime, Vienna. World drug report 2009. New York: United Nations. 2009. http://www.unodc.org/documents/wdr/WDR_2009/WDR2009_eng_web.pdf. Accessed 27 Feb 2010.
Federal Scientific Methodic Center for HIV Fight and Prevention. VICh-infektsiya: Informatsionnyy Byulleten’ [HIV infection: informational bulletin] (in Russian) No. 33. Moscow: Federal Scientific Methodic Center for HIV Fight and Prevention. 2009. http://www.hivrussia.org/files/bul_33.pdf. Accessed 27 Feb 2010.
Federal Scientific Methodic Center for HIV Fight and Prevention. The amount of HIV-infected persons in Russia by October 31, 2009. http://www.hivrussia.org/stat/2009/10.shtml. Accessed 27 Feb 2010.
UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance. Epidemiological fact sheet on HIV and AIDS, Russian Federation: 2008 update. Geneva. December, 2008. http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_RU.pdf. Accessed 27 Feb 2010.
Federal Service for Surveillance of Consumer Rights Protection and Human Well-Being of the Russian Federation. Country progress report of the Russian Federation on the implementation of the declaration of commitment on HIV/AIDS, Moscow. 2008. http://www.unaids.ru/files/publications/UNGASS%20report%20Russia%202008_EN.pdf. Accessed 27 Feb 2010.
Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2007. Vol. 19. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention. 2009. http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2007report/default.htm. Accessed 27 Feb 2010.
Kissin DM, Zapata L, Yorick R, et al. HIV seroprevalence in street youth, St. Petersburg, Russia. AIDS. 2007;21(17):2333–40.
Kalichman SC, Rompa D, Cage M. Sexually transmitted infections among HIV seropositive men and women. Sex Transm Infect. 2000;76:350–4.
Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: a review of social, psychological, and medical findings. AIDS. 2002;16:135–49.
Rotheram-Borus MJ, Lee M, Zhou S, et al. Variation in health and risk behavior among youth living with HIV. AIDS Educ Prev. 2001;13:42–54.
Fogarty L, Roter D, Larson S, Burke J, Gillespie J, Levy R. Patient adherence to HIV medication regimens: a review of published and abstract reports. Patient Educ Couns. 2002;46:93–108.
Weinhardt LS, Kelly JA, Brondino MJ, et al. HIV transmission risk behavior among men and women living with HIV in four US cities. J Acquir Immune Defic Syndr Hum Retrovirol. 2004;36:1057–66.
Kalichman SC. Co-occurrence and treatment nonadherence and continued HIV transmission risk behaviors: implications for positive prevention interventions. Psychosom Med. 2008;70:593–7.
Sikkema KJ, Watt MH, Drabkin AS, Meade CS, Hansen NB, Pence BW. Mental health treatment to reduce HIV transmission risk behavior: a positive prevention model. AIDS Behav. 2010;14:252–62.
Glass TR, Battegay M, Cavassini M, et al. Longitudinal analysis of patterns and predictors of changes in self-reported adherence to antiretroviral therapy: Swiss HIV cohort study. J Acquir Immune Defic Syndr. 2010;54:197–203.
Johnson MO, Charlebois E, Morin SF, Remien RH, Chesney MA. Effects of a behavioral intervention on antiretroviral medication adherence among people living with HIV: the healthy living project randomized controlled study. J Acquir Immune Defic Syndr Hum Retrovirol. 2007;46:574–80.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401.
Radloff LS, Locke BZ. The community mental health assessment survey and CES-D scale. In: Weissman MM, Myers JK, Ross CE, editors. Community surveys of psychiatric disorders. New Brunswick, NJ: Rutgers University Press; 1986. p. 177–87.
Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV/AIDS. J Nervous Mental Dis. 2000;188:662–70.
Spielberger CD. State-trait anxiety inventory (form Y). Palo Alto, CA: Consulting Psychologists Press; 1983.
Cutrona CE. Ratings of social support by adolescents and adult informants: degree of correspondence and prediction of depression symptoms. J Personality Soc Psychol. 1989;57:723–30.
Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. Adv Personal Relationships. 1987;1:37–67.
Kelly JA, Murphy DA, Bahr GR, et al. Factors associated with severity of depression and high-risk sexual behavior among persons diagnosed with human immunodeficiency virus (HIV) infection. Health Psychol. 1993;12:215–9.
Kelly JA, Murphy DA, Bahr GR, et al. Outcome of cognitive-behavioral and support group brief therapies for depressed HIV-infected persons. Am J Psychiatry. 1993;150:1679–86.
Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30.
García de Olalla P, Knobel H, Carmona A, Guelar A, Lopez-Colomes JL, Cayla JA. Impact of adherence and highly active antiretroviral therapy on survival in HIV-infected patients. J Acquir Immune Defic Syndr Hum Retrovirol. 2002;30:105–10.
Ladnaya NN. Key epidemiological indicators and trends of HIV infections in the Russian Federation. Report of the Federal Scientific-Methodological Center for Prevention and Fight With AIDS, 30 Sep 2010.
Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA. 2009;301:2380–2.
FrontAIDS. ARV therapy in Russia: barriers to treatment delivery. Alternative report to UN General Assembly Special Session on HIV/AIDS. 2008. http://www.icaso.org/resources/Shadow_russia1107ru.full%20report.pdf. Accessed 27 Feb 2010.
The HIV/TB Study Writing Group. Mortality from HIV and TB coinfections is higher in Eastern Europe than in Western Europe and Argentina. AIDS. 2009;23:2485–95.
Acknowledgment
Conduct of this research and preparation of the paper were supported by grants P30-MH52776 and R24-MH082471 from the U.S. National Institute of Mental Health. The authors thank the study participants and also Anastasia G. Kuyanova, Rudolph A. Amirkhanian, Maria Donskaya, and Roman A. Khoursine at ICART; Aza G. Rakhmanova, Svetlana V. Zhukova, Irina D. Yevseyeva, and Vladislav N. Koryagin at the Botkin Hospital for Infectious Diseases; Natalya V. Bodosova, Elena V. Stepanova, Olga V. Koltsova, and Olga N. Leonova at the AIDS Center, Infectious Disease Hospital #10 and PLH self-support groups in St. Petersburg; and Ruzanna Aleksanyan, Timothy L. McAuliffe, Tom Lytle, Anton M. Somlai, David W. Seal, Steven D. Pinkerton, Michelle Anderson-Lamb, and Allan C. Hauth at the Medical College of Wisconsin for their assistance in the research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amirkhanian, Y.A., Kelly, J.A., Kuznetsova, A.V. et al. People with HIV in HAART-Era Russia: Transmission Risk Behavior Prevalence, Antiretroviral Medication-Taking, and Psychosocial Distress. AIDS Behav 15, 767–777 (2011). https://doi.org/10.1007/s10461-010-9793-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-010-9793-x