Abstract
This paper examines the relationship of frequency, type of alcohol use, sexual risk behaviors and sexually transmitted infections (STIs) among married men living in economically marginal communities in Mumbai, India. The findings indicate that men who consume alcohol daily were four times more likely to have had extramarital sex in the past 12 months. In terms of sexually transmitted infections, men who were daily drinkers were four times more likely than those not consuming alcohol in the last month to have gonorrhea (NG) and Chlamydia (CT) infection and three times more likely to have had a past history of exposure to herpes simplex virus-2 (HSV-2) and/or syphilis as determined by biological testing. These results demonstrate that men with daily alcohol use are at greatest risk for STIs and need to be targeted for community outreach, de-addiction services and sex risk reduction education program in India and elsewhere.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol use among married men in India is common and varies widely by region. States in the northern and northeast regions show the highest rates of consumption of alcohol by men [1]. With recent economic liberalization policies, alcohol has become more available, with more varieties and outlets [2]. This ease of access is reflected in the drinking behavior of men in India [1], and studies investigating dependency report that as high as 50% of those who drink alcohol are addicted to it [3, 4].
The consistent relationship between alcohol consumption and the prevalence of sexual risk behaviors has now been extensively examined globally [5–8]. In India too, the nation-wide behavior surveillance survey conducted by the National AIDS Control Organisation (NACO) among clients of female sex workers, found that nearly three-fourths of the respondents reported ever having alcohol [9]. Other studies in India document that men who frequent community-based alcohol outlets or wine shops are more likely to be engaged in high risk sexual behavior [10], and truck drivers who consumed alcohol were 2.71 times more likely to visit a commercial sex worker than those who did not [11]. A study in Chennai which examined the linkages between alcohol use and HIV prevention behavior showed that the “Ideal Man” avoids alcohol use and extramarital sexual behavior and a “Typical Man” drinks alcohol excessively, beats his wife and involves in sexual relationships with women outside marriage [12].
The behavioral effects of alcohol are multifactorial, including social disinhibition or interference with judgment and decision making, which may lead to a higher risk of STI exposure [13]. Sensation seeking is defined as the tendency to seek novel, exciting, and optimal levels of stimulation and arousal [14, 15]. A recent study in India found that among heavy alcohol users, sensation seeking was significantly associated with sexual risk taking behavior [16].
In Mumbai, the economic capital of India, alcohol use was reported by approximately 70% of the male clients of female sex workers (FSW) attending STI clinics [17]. Cross-sectional baseline data from a cohort of high-risk men attending an STI clinic in Mumbai indicated that men who drink alcohol when visiting FSWs engage in riskier behavior and are more likely to have STIs or HIV. In this study, 92% of men reported sex with an FSW, and of these, 66% reported having sex while under the direct influence of alcohol [18].
Most studies [10, 11, 18], of alcohol use and sexuality focus on individuals in high risk categories; that is men known to be involved in the transmission of HIV, including partners of commercial sex workers and other women in the sexual services industry, truck drivers and men who have sex with men. Little is known about alcohol consumption in the general population and its relationship to sexually risky behavior especially among married men. Further, studies on the relationship of alcohol to sexual risk have focused on reported behavior with little capacity to verify the relationship through biological testing for STIs. In this paper, we seek to address these deficiencies by drawing on data from a comprehensive study conducted in Mumbai to examine the factors involved in married men’s sexual risk and to implement a multilevel, culturally appropriate intervention. As a part of this study, data was collected on the frequency of alcohol use as reported by married men in the age-group of 21–40 years and of the presence of sexually transmitted infections as measured by biological testing.
Methods
Data Source
Data for this study were obtained from research conducted as part of a 6-year (2001–2007) Indo-US collaborative project funded by the U.S. National Institute of Mental Health. The project, known as “RISHTA” (meaning “relationship” in Hindi/Urdu and an acronym for “Research and Intervention in Sexual Health: Theory to Action”) aimed to reduce unsafe sexual risk among married men in three economically marginalized low income communities in Mumbai, India. The study communities are located in the northeastern part of Mumbai have a total population of approximately 700,000. The overall design of the RISHTA project has been described in detail elsewhere [19–21]. In order to obtain a representative sample of married men in the age-group of 21–40 years for baseline and endline measures of intervention outcomes, we used a two-stage systematic sampling procedure in which lanes/sub-areas were enumerated and randomized during the first stage, and the eligible households were systematically randomly selected from lanes/sub-areas during the second stage. A married man of the household in the age 21–40 years was randomly selected from eligible household roster using KISH grid tables for participation in the survey. The Kish table is a statistical tool to facilitate randomness when households have more than one individual that satisfies the eligibility criteria.
Between 2003 and 2006, two rounds of cross-sectional behavioral and epidemiological surveys were conducted using the same instruments. The baseline study took place during May–October, 2003 and the endline survey during February–April, 2006. The baseline survey interviewed a random sample of 2408 married men aged 21–40 years, and the endline survey interviewed an independent random sample of 2722 married men aged 21–40 years in the same three communities. The survey contained questions including socioeconomic and demographic characteristics, sexual behavior, drug and alcohol use, frequency of alcohol use, sexual and general health, STI knowledge, health care seeking behavior, marital relationships and attitudes concerning masculinity.
Random subsamples of men were selected from the baseline and endline cross-sectional samples (baseline n = 642; endline n = 891) and asked to give blood (baseline only) and urine samples (baseline and endline) for STI testing. At baseline, blood serum was tested for syphilis using rapid plasma reagin (RPR) and treponema pallidum haemagglutination (TPHA). Serum was also tested for the presence of IgM and IgG antibodies to herpes simplex virus-2 (HSV-2) (Vircell, Santase Granada, Spain). Urine samples were tested to detect chlamydia trachomatis (CT) and N. gonorrhea (NG) infection using Multiplex Amplicor PCR assay (Roche Diagnostic Systems, Branhburg, New Jersey, USA). Those who tested positive for syphilis, NG, and/or CT were counseled and provided with free treatment by a trained physician associated with the project, following the WHO standard syndromic treatment protocols [23]. Individual HIV testing was not conducted in the survey as a result of the lack of treatment capacity in the study communities at the time of the initiation of the study (in the year 2002) and was stated as such in the consent form. The endline sample of men was asked to provide urine samples only for NG and CT testing since acute rates for syphilis and HSV-2 were low; 1.3 and 0.9%, respectively of the total blood samples tested in baseline [21, 22]. The past history of STI (HSV-2 and syphilis) infection was available for a total of 642 men who were interviewed in the year 2003 and these data were used to examine the relationship between alcohol use and history of exposure to STIs.
The objective of this paper is to examine the association between alcohol use and sexually transmitted infections. To accomplish this objective, data from the baseline and endline surveys were combined to increase the statistical power while examining the relationship between alcohol use and sexual risk behaviors in low STI prevalence populations. This approach is justified by the fact that the period of time between 2003 and 2006 has not produced significant change in the social and environmental conditions of the study communities. While for some men, the RISHTA interventions that included community intervention (see article by Schensul et al. in this volume) may have affected the consumption of alcohol, for objectives of this paper use of cross-sectional data at both the intervals with independent individuals is relevant. Moreover, to ensure that there is no double counting of individuals in the analyses, 338 individuals from the endline sample who also participated in the survey and STI testing at the baseline have been removed from the analytical sample. This resulted into a combined 2003/2006 sample of 1195 independent individuals who participated in the survey and STI testing at either baseline or endline.
The RISHTA study was approved by the Ethics Committee of the Indian Council of Medical Research (HMSC-ICMR) and the institutional review boards (IRBs) of the collaborating partners: the International Institute for Population Sciences (IIPS) in Mumbai, India; the University of Connecticut Health Center in Farmington, Connecticut, USA; and the Institute for Community Research in Hartford, CT, USA. Written informed consent was obtained from each individual before the interview and STI testing.
Measures
A series of questions in the survey instruments concerning the type and frequency of alcohol consumption have been used in the data analyses reported in this paper. The survey instrument assessed the type of alcohol used including commercially available beer, “English liquor” (whisky, brandy, rum, gin brewed in the Western style) and desi daaru (country liquor) brewed locally. For each type of alcohol, the frequency of consumption was asked using a format in which respondents were asked how often they drank alcohol in the last 30 days (1 month). Responses included “Daily”, “Weekly”, “Rarely” and “Never”. The categories “Weekly” and “Rarely” were collapsed into a single category of “at least once in 30 days” resulting in three categories of alcohol consumption: “Daily”, “at least once in 30 days” or “Never”. We recognize that the measurement of alcohol consumption over the last three decades has become more sophisticated with a number of instruments geared to more accurate measurement. However, since the RISHTA project was not specifically focused on alcohol, the currently available RISHTA alcohol data nonetheless provides a unique opportunity to examine alcohol use and STI in a general community population.
The dependent measure of sexual risk behavior used in this paper included: sex with a sex worker, sex with a non-spousal or casual partners, sex with either partner, sex with more than 2 partners excluding spouse in the last 12 months. Sex in the last 12 months prior to the survey by type of partner was assessed based on two separate single questions. A report of sex with sex worker in the last 12 months was coded as 1 and the remainder was coded as 0. Similarly, sex with a regular non-spousal or casual partner was coded as 1 or 0. Sex with either a sex worker (or) regular non-spousal or casual partner was calculated by combining the two previous variables. Respondents reporting neither sex with sex worker nor with non-spousal or casual partner are coded as 0 and rest were coded as 1. The number of sexual partners was calculated from the questions on the number of sex workers visited in the last 12 months and the number of regular non-spousal or casual partners (sex with <2 non-spousal partners is coded as 0 and sex with 2 or more non-spousal partners is coded as 1).
Neisseria gonorrheaoe (NG) and/or Chlamydia Trachomatis (CT) infection was calculated as a dichotomous variable based on testing of urine samples using a PCR assay. Samples testing positive for either GC or CT were coded as 1; and negative for both GC and CT were coded as 0. Similarly, past history of syphilis and HSV-2 (were coded as 1 and the remainder was coded as 0). The assessed demographics were age, level of education, and income of the respondent.
Statistical Analyses
Calculation of proportions, t-test and χ2 tests were used to assess the significance of bivariate relationships. The association between an outcome (sexual risk behavior and STIs) and an independent variable (frequency of alcohol use, type of alcohol use) was assessed using a multiple logistic regression model to obtain the adjusted (for age, education and religion of the respondent) odds ratio (OR) and its 95% confidence interval (CI). Analyses were conducted using SPSS 15.0.
Results
Of the total of 1195 respondents included in the analysis, the median age was 32 years. Seventeen percent were illiterates and the average education was 7 years. The mean income of the respondents was 4070 rupees (approximately USD 90) per month and half of the total men were earning 3500 rupees or less.
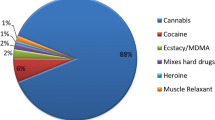
Four percent men in the survey reported consumption of alcohol daily and 30 percent reported consumption at least once in 30 days. Men report different rates of consumption for different types of alcohol. For example, approximately 11.6% (139/1195) of the males of the total sample have reported that they had beer (commercially bottled) in the last 1 month while approximately one-fourth of men (284/1195) reported that they had country liquor (desi daaru) brewed legally or illegally in the last 1 month. Twenty-two percent (266/1195) of the total number of men interviewed reported that they had Indian brewed and bottled whiskey, rum and other products (“English liquor”) in the last 30 days. Six percent of the men (69/1195) reported that they had all the three types of alcohol in the last 1 month and 10.5% of the men (125/1195) reported that they had both desi daaru and English liquor but no other types of alcohol.
Daily alcohol use was highest among men in the age-group of 36–40 years (5.3%, 17/318) and among literates with primary (4.1%, 6/147) or middle school education (5.1%, 17/331). The proportion of men having daily alcohol use showed no significant differences across income categories (see Table 1). Comparatively, beer drinkers are higher among men earning less than 3000 rupees (14.9%, 58/390) when compared to men earning more than 5000 rupees (7.7%, 24/310). English liquor and desi daaru drinking did not differ significantly by age, education and income of the respondents.
Table 2 indicates the bivariate association between frequency of use, types of alcohol use and sexual risk behaviors. The proportion of men having sex with a sex worker in the last year varies with both type and frequency of alcohol consumption. The data indicate that men who reported drinking alcohol daily had at least one extramarital sex partner significantly more often than the men who did not drink alcohol in the last 1 month (19 vs. 6.5%; χ2 = 39.8; p < 0.001). Men who drank beer in the previous month reported that they had sex with a sex worker in the last 1 year more often than the men who did not take beer in the last 1 month (8.0 vs. 2.7%; χ2 = 10.9; df = 1; p < 0.001).
The proportion of men across the baseline/endline samples was 2.8%. The frequency varied according to the level of alcohol use and the type of alcohol (see Table 3). The association between men’s frequency of drinking alcohol and a positive NG/CT test is statistically significant (χ2 = 8.5; df = 2; p = 0.014), with a higher proportion of men who drank alcohol daily (9.3%) having NG/CT than those who drank at least once in 30 days (3.4%) or never (2.1%). There was a significant association between men who reported any use of beer in the 30 day period prior to the survey with or without a combination of other types of drinks and positive test for NG and/or CT (5.8 vs. 2.4%; χ2 = 5.3; df = 1; p = 0.03). Similarly, the proportion of men infected with NG and/or CT is higher among men who reported taking desi liquor, english liquor with or without a combination of other types of drinks.
The results in Table 3 also show that over 13% of men tested had a past history of HSV-2 (IgG+) and/or syphilis (RPR−/TPPA+). A past history of HSV-2 and/or syphilis varied significantly with the frequency and type of alcohol use. A little more than one-fourth of the total men who reported daily alcohol use had a history of HSV-2 and/or syphilis; the corresponding percentages among those men who took alcohol at least once in 30 days and those who did not drink at all during that time are 16 and 11% (χ2 = 7.3; df = 2; p = 0.02).
Table 4 shows the adjusted impact of frequency of alcohol use on extramarital sex behavior in the past 12 months, current infection to NG and/or CT, and past history of HSV-2 and/or syphilis, after adjusting for age, education and religion of the respondent. Men with alcohol use in the last 30 days were more likely to have engaged in extramarital sex (adjusted odds ratio [AOR]––3.5, 95% CI 1.5–7.9) than those who did not drink alcohol in the last 1 month. Men who reported daily alcohol use were four times more likely to be infected with NG and/or CT (AOR––4.0, 95% CI: 1.3–12.8) and were close to three times more likely to have a past history of infection to HSV-2 and/or syphilis (AOR: 2.7, 95% CI 1.1–7.1). In Table 5, men with consumption of all the three types of alcohol use were six times (95% CI: 3.5–11.5) more likely to engage in extramarital sex than those who did not consume alcohol.
Discussion
Previous research from developing nations shows that alcohol use is associated with extramarital sex behaviors [5–8]. Findings from this study are further confirmation of the association between reported alcohol use and sexual risk behaviors. This paper goes beyond this association by demonstrating that the practice of daily alcohol use is significantly associated with an increased risk of having extramarital sex in the past 12 months, current NG and/or CT infection and past history of exposure to HSV-2 and/or syphilis. Consistent with findings from the previous published studies [24], the results in the present study indicates that the men with daily alcohol use are at greater risk for STIs with implications for targeting interventions for the reduction of HIV/STI risk.
Among the reported three common types of alcohol used by men in this study, bivariate analyses showed that consumption of beer with or without other type of drinks is significantly associated with extramarital sex behavior, current infection to NG and/or CT, and past history of infection to HSV-2 and/or syphilis. These results are consistent with our ethnographic data concerning the venues for the consumption of the different types of alcohol. Beer is generally consumed in “beer bars” where groups of male friends go for socialization and where beer is served by “beer bar girls” who flirt with men and in many cases are available for sex. There are many such “beer bars” within three miles distance from the study communities and many men visit these bars in groups to have beer and interact (and sometimes have sex) with the women. Older men who drink beer and frequent beer bars are those who have strong peer networks and use that medium for pleasure associated with intoxication and sex.
Desi daaru in urban slums is purchased either at the few authorized shops, in unauthorized homes where it is brewed or it may be sold in small bottles by traveling vendors. The shops where desi daaru is sold are known as Desi bars. Frequently home brewers or their helpers are widows who receive a small amount for assistance in serving liquor and are available for sex for money. Additionally, women who sell eatables such as boiled eggs and nuts just outside the desi daaru shops are also available for sex. Usually sexual activities with these women take place in nearby isolated places or rooms within alcohol venues or restaurants where condom availability is rare. The study findings further indicate that men who consume desi daaru are significantly less likely to use a condom.
English liquor is consumed in the liquor in restaurants (“hotels”) in or near the study communities and is associated with two or three men getting together for smoking, drinking and socializing, but women are less likely to be present as service staff. As a result, these men are likely to visit red light districts or have sex with women who they knew are available in their communities. Men who consume “English liquor” are more likely to also report sex with both sex workers and casual, unpaid female partners.
Although there is no “red light” district within the study communities, the area is known to have many “home-based” sex workers who, with husband’s approval, contribute to household income through sex with men in the study community. Some women from the community work in local restaurants near the alcohol selling venues. Men usually buy their liquor from the shops and drink at the restaurants with spicy food and soft drinks. Some of these restaurants have rented rooms which are generally used with sex workers by intoxicated male restaurant customers. The study findings suggest that the great majority of men who have extramarital sex do so with non-formal sex workers in their own or nearby communities.
In order to understand the type of liquor and its association with sexual risk behaviors and STIs, a multivariate logistic regression analysis was conducted. The results show that exclusive use of any one drink is not linked with sexual risk behaviors; however, men who drink all three types of alcohol are six times more likely to engage in extramarital sex behaviors than those men who do not drink any alcohol.
In the RISHTA sample of married men in the age-group of 21–40 years, 3.6% of men reported daily alcohol use, with older and less educated men more involved in daily use. For the month prior to the survey, 29.7% had alcohol at least one time. The alcohol use reported in this study is consistent with previously conducted nation-wide research in India [1, 25].
Although results from this study offer important understanding into frequency and type of alcohol use, sexual risk behavior and STIs in low STI prevalence populations, these must be interpreted in the light of certain study limitations. As in any study, the associations that have been identified are based on general patterns of sexual risk behavior and alcohol consumption reported by the individual rather than at the specific event level. There is no information in our data to indicate how long men have been drinking alcohol daily or how often men are involved in sex, prior to or after drinking or level of drinking during sexual encounters with non-spousal partners. This gap in our knowledge of the association makes it difficult to precisely indicate how alcohol use may influence sexual risk behavior. Another limitation of this study is that we did not collect information on the quantity of alcohol use. Quantity of consumption is linked to sexual risk in some studies. Internationally validated alcohol measurement instruments that would include information on binge drinking and timing of alcohol use, would have added an important dimension to the results.
Despite its limitations, this study adds important evidence to the proposition that there is an association between alcohol use and sexually risky behavior as measured by biologically determines STIs. These results suggest that there should be a greater emphasis on the integration between prevention and treatment of alcohol use and abuse and STIs among married men in a low income, general community population. The results also indicate that men who drink alcohol daily are at highest risk for extramarital sex as well as sexually transmitted infections. Thus, daily or regular use of alcohol can serve as a way of identifying men who can be targeted for HIV/STI prevention. Such targeting would need to involve outreach to men in urban poor communities, involvement in de-addiction services and a curriculum focused on sexual risk reduction. HIV/STI prevention efforts could then focus both on reducing alcohol consumption and reducing instances of unprotected extramarital sex among the daily alcohol users.
References
Patel SK, Niranjan S. Linkages between substance use, couple characteristics and reproductive behavior in India. In: Tripathy SN, Bishoyi D, Patel SK, editors. Dynamics of population issues. New Delhi: Sonali Publications; 2007.
Basu K. Globalization and culture. India Today; 20 April 1998.
Benegal V. India: alcohol and public health. Addiction. 2005;100(8):1051–6.
Ustun TB. The world health surveys. In: Murray CJL, Evans DB, editors. Health systems performance assessment: debates, methods and empiricism. Geneva: World Health Organization; 2003.
MacDonald TK, Zanna MP, Fong GT. Why common sense goes out the window: effects of alcohol on intentions to use condoms. Pers Soc Psychol Bull. 1996;22:763–75.
Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behaviour? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57.
Kalichman SC, Weinhardt L, DiFonzo K, Austin J, Luke W. Sensation seeking and alcohol use as markers of sexual transmission risk behaviours in HIV-positive men. Ann Behav Med. 2002;24:229–35.
Testa M. The impact of men’s alcohol consumption on perpetration of sexual aggression. Clin Psychol Rev. 2002;22:1239–63.
NACO. National baseline high risk and bridge population behavioural surveillance survey 2002. New Delhi: National AIDS Control Organization; 2002.
Sivaram S, Latkin CA, Solomon S, Celentano DD. HIV prevention in India: focus on men, alcohol use and social networks. Harv Health Policy Rev. 2006;7(2):125–34.
Chaturvedi S, Singh Z, Banerjee A, Khera A, Joshi RK, Dhrubajyoti D. Sexual behaviour among long distance truck drivers. Indian J Commun Med. 2006;31(3):153–6.
Go V, Sethulakshmi C, et al. When HIV-prevention messages and gender norms clash: the impact of domestic violence on women’s HIV risk in slums of Chennai, India. AIDS Behav. 2003;7(3):263–72.
Halphen-Felsher BL, Millstein SG, Ellen JM. Relationship of alcohol use and risky sexual behavior: a review and analysis of findings. J Adolesc Health. 1996;19:331–6.
Zuckerman M, Eysenck S, Eysenck HJ. Sensation seeking in England and America: cross-cultural, age and sex comparisons. J Consult Clin Psychol. 1978;46:139–49.
Zuckerman M. Behavioural expressions and biosocial bases of sensation seeking. New York: Cambridge University Press; 1994.
Chandra PS, Krishna VAS, Benegal V, Ramakrishna J. High-risk sexual behaviour and sensation seeking among heavy alcohol users. Indian J Med Res. 2003.
Das S, Yemul V, Deshmukh R. Incidence and association of HIV and other STDs in 200 persons belonging to a high risk group in central Mumbai. Venereology. 1998;11(1):19–23.
Madhivanan P, Hernandez A, et al. Alcohol use by men is a risk factor for the acquisition of sexually transmitted infections and human immunodeficiency virus from female sex workers in Mumbai, India. Sex Transm Dis. 2005;32(11):685–90.
Schensul SL, Verma RK, Nastasi BK. Responding to men’s sexual concerns: research and intervention in slum communities in Mumbai, India. Int J Men’s Health. 2004;3:197–220.
Schensul SL, Mekki-Berrada A, Nastasi BK, Saggurti N, Verma RK. Healing traditions and men’s sexual health in Mumbai, India: the realities of practiced medicine in urban poor communities. Soc Sci Med. 2006;62:2774–85.
Saggurti N, Schensul SL, Verma RK. Migration, mobility and sexual risk behaviour in Mumbai, India: mobile men with non-residential wife show increased risk. AIDS Behav. 2009;13(5):921–7.
Schensul SL, Hawkes S, Saggurti N, Verma RK, Narvekar SS, Nastasi BK, Burleson JA, Risbud A. STIs in men in Mumbai slum communities: the relationship of prevalence to risk behavior. Sex Transm Dis. 2007;34(7):444–50.
WHO. Guidelines for the management of sexually transmitted infections. Geneva, Switzerland: World Health Organization; 2003.
Go VF, Solomon S, Srikrishnan AK, Sivaram S, Johnson SC, Sripaipan T, Murugavel KG, Latkin C, Mayer K, Celentano DD. HIV rates and risk behaviors are low in the general population of men in Southern India but high in alcohol venues: results from 2 probability samples. J Acq Immune Def Syndr. 2007;46(4):491–7.
International Institute for Population Sciences (IIPS) and Macro International. National family health survey (NFHS-3), 2005–2006. Vol I. Mumbai, India: IIPS; 2007. http://www.measuredhs.com/pubs/pdf/FRIND3. Accessed 3 July 2009.
Acknowledgements
This study was supported by the National Institute of Mental Health grant R01-MH064875. The authors would like to thank the organizers of the Alcohol and Sexual Risk Conference, Dr. Jean J. Schensul, Senior Researcher and Founding Director of the Institute for Community Research in Hartford, CT, USA and Dr. S.K. Singh, Associate Professor, International Institute for Population Sciences, Mumbai, India, where this paper was first presented. Source of Support: Analyses for this study were conducted via funding from the National Institute of Mental Health (Grant #: R01-MH064875).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saggurti, N., Schensul, S.L. & Singh, R. Alcohol Use, Sexual Risk Behavior and STIs Among Married Men in Mumbai, India. AIDS Behav 14 (Suppl 1), 40–47 (2010). https://doi.org/10.1007/s10461-010-9728-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-010-9728-6