Abstract
Previous research reports that populations with HIV consume higher rates of alcohol than general population. This cross-sectional study (n = 391) was conducted to measure alcohol consumption, factors associated with consumption, and the relationship between alcohol and HIV viral loads among individuals receiving HIV care. Increased alcohol consumption was associated with being male, lower education attainment, and lacking a current HAART prescription. Additionally, among those currently on HAART, unsuppressed viremia was associated with higher levels of alcohol consumption. These findings suggest that there may be a relatively low level of alcohol consumption that is detrimental to virologic suppression among populations with HIV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The advent of Highly Active Antiretroviral Therapy (HAART) has transformed HIV into a chronic illness for those who have access to care. This change highlights the need to improve long-term health outcomes, quality of life, and secondary prevention efforts among individual with HIV. These aspects of care require an enhanced understanding of the complex factors that impact the clinical course of HIV infection. As a component of these factors, alcohol use is common among individuals with HIV and has been associated with adverse health effects that increase morbidity and mortality [1].
Alcohol use is estimated to be highly prevalent in populations with HIV, with the HIV Cost and Utilization Survey reporting rates of heavy drinking among individuals with HIV (8%) almost twice those found in the general population (4.5%). Additionally, individuals with lower levels of education attainment and those who have substance use disorders drink more heavily [1]. Consistently, men have reported drinking more often and heavily than women, without regard to HIV disease status [2, 3]. Physiologically, heavy alcohol consumption contributes to HIV-associated neuropathy, [4] hastens the progression of liver disease related to hepatitis C, and impairs neurocognitive function [5]. Additionally, poor self-care practices have been associated with alcohol consumption. Limited engagement in medical care and medication nonadherence, as it impacts viral load suppression, has been related to higher levels of alcohol consumption [6, 7]. Specifically, a dose–response relationship has been found between alcohol consumption and medication nonadherence [8]. Alcohol use has also been associated with use of illicit drugs, high-risk sexual and injection-related behaviors that challenge efforts of secondary HIV prevention [9].
Given the established relationship between HIV disease and alcohol use, screening for current alcohol frequency and quantity has been recommended as a component of routine HIV medical care [10, 11]. Unfortunately, consistent screening among patients who present for care has been difficult to establish in many care-providing environments. Limited time, competing secondary prevention efforts, and the social acceptability of alcohol use challenge routine screening. Particularly in the case of HIV, many patients have complex issues beyond medical management that include unstable housing and income, as well as the management of chronic and other psychiatric comorbidities. With these competing concerns and other prevention efforts, it may be difficult to prioritize a topic of brief intervention. The purpose of this study was to assess level of alcohol consumption, factors associated with those levels, and the relationship between alcohol consumption levels and HIV viral load among individuals receiving HIV care.
Methods
This was a cross-sectional examination of alcohol consumption, sociodemographic factors, and their association with HIV outcomes. As part of standard-of-care, all patients who attended the Washington University HIV Clinic (St. Louis, MO) completed a behavioral assessment during regular clinic visits. All patients with HIV who presented in the clinic were eligible to complete assessments between June and September 2007 (n = 421). As each patient entered their assigned clinic exam room, a trained rater conducted the paper-based interview prior to the physician visit. Less than 3% (n = 15) of the clinic population surveyed refused to complete the interview. The medical chart abstractions were conducted by medical assistants, they collected the medical measures (CD4 cell count and HIV viral load) from the same clinic visit date as when the interview was conducted. This study was approved by Washington University School of Medicine Human Research Protection Office.
The behavioral assessment was conducted by an interviewer to collect demographic characteristics (race, age, employment, education, and income), alcohol use, (frequency and quantity), self-reported medication adherence, and depressive symptomatology. Alcohol use was assessed for all participants who reported drinking within the past 4 months; a daily recall was conducted for those who endorsed drinking in the past 7 days. While National Institute for Alcohol Abuse and Alcoholism (NIAAA) suggests that 3 drinks daily for women (4 drinks for men) and that 7 drinks per week for women (14 drinks per week for men) is low-risk consumption, their recommendations vary by age and gender [12, 13]. In this study, we created a cut-off of “at-risk” drinking based on the median number of drinks our sample reported consuming in the previous week. Due to the increased harm alcohol has on women, we selected 4 drinks per week for women and 5 for men. Any additional consumption was determined to be “at-risk” weekly drinking. This selection was based on the median number of drinks per week in our sample, knowledge of the weekly recommendation of maximum consumption, and the lack of recommended amounts among individuals with HIV.
The Patient Health Questionnaire (PHQ-9) was used to measure depressive symptomatology and calculate symptom counts that signify major depressive disorder (MDD) and other depressive disorders (ODD). The reliability of the scale in this sample was assessed with Cronbach’s α = .851. The area under the curve of the receiving operating characteristic was excellent (AUC = 0.982) when testing the specificity and sensitivity of MDD/ODD identification. Additional analyses on depression and its associations in this sample using the PHQ-9 are included elsewhere [14].
Self-reported medication adherence was measured using the ACTG 4-day recall instrument [15]. Medication adherence was dichotomized to <95% and ≥95%, as commonly used [16]. Medical measures including current CD4 cell count, plasma HIV RNA level, and use and types of antiretroviral therapies prescribed were collected at time of the visit. HAART was defined as the use of at least three drugs from two different antiretroviral drug classes, or the use of ≥three NRTIs. Virologic suppression was defined as having an HIV RNA level of <400 copies/ml.
Statistical Analyses
Descriptive analyses were conducted to assess the levels of alcohol consumption among the sample. Analyses related to amount of alcohol consumed were conducted only with respondents who reported drinking within the past 7 days. HIV viral loads (<400 copies/ml and ≥400 copies/ml), education levels (≤high school degree/GED or >high school degree), race (Caucasian and African American/other minorities), employment status (unemployed and employed), annual income (≤ and >$10,000) and depression severity (MDD/ODD and no depressive disorders) were dichotomized.
Chi-square tests were used to determine the statistical significance of the associations between no and any alcohol consumption and each of the independent variables (gender, age, race, income, education, employment status, depressive symptomatology, HIV-related medical parameters [current HAART prescription, self-reported medication adherence, HAART type, CD4 cell count]); as well as between regular and “at-risk” drinking. Multivariate logistic regression models estimated the independent effects of each of the variables on the odds of regular alcohol consumption and at-risk drinking to test the hypothesized differences in factors related to levels of alcohol consumption by amount of alcohol consumed in previous week (≤4/5 drinks for women/men vs. >4/5 drinks). Mann–Whitney tests were conducted to compare CD4 counts by groups. As part of our analyses, we had hypothesized that individuals with current HAART prescriptions would be less likely to be at-risk drinkers and therefore have undetectable viral loads.
All tests were 2-tailed and P < 0.05 was considered significant. Data analyses were performed using SPSS software (version 16.0).
Results
A total of 391 individuals were screened for daily alcohol use. Of those, 39% (n = 154) of the sample reported drinking alcohol in the past week with the median number of 4.0 (IQR: 2, 10) drinks. Among individuals who reported drinking alcohol within the past 4 months, but not in the past week (n = 66, 17%), the median number of drinks consumed in a typical week was 2.0 (IQR: 2, 5). Among the planned comparisons (sociodemographic factors), the only differences by bivariate analyses among individuals who did or did not consume any alcoholic drinks within the previous 7 days was that men reporting drinking more often than women (33% vs. 24%; P < 0.05) and those who were unemployed drank more often than those employed (64% vs. 53%; P < 0.05) (Table 1).
Subsequent analyses were conducted among those who drank within the past 7 days (n = 154). Individuals who drank only beer (n = 61) the previous 7 days had a median 3.0 drinks (IQR = 1, 9), those who only drank wine (n = 16) had a median of 2.0 (IQR: 1, 4), and those who only drank liquor (n = 36) reported a median of 3.0 (IQR: 2, 6) drinks per week. Analyses were conducted to assess if drinking different types of alcohol differed in the HIV-related health outcomes (viral load, CD4 cell count) or the amount of alcohol consumed. If individuals reported drinking any combination of beer and wine, wine and liquor, liquor and beer, or all three, they were more likely to consume more alcohol in the previous 7 days (P < 0.001 for all) (Table 2).
While associated with viral load suppression, self-reported medication adherence had a moderate correlation (r = 0.52). When analyzing self-reported medication adherence, there were no associations found with amount of alcohol consumed. We analyzed virologic suppression only among individuals who were receiving HAART as to measure the success of their medication management; the relationship to at-risk drinking was hypothesized to be a factor that interfered with adherence (measured in this study by viral load).
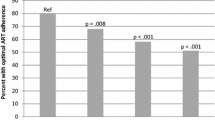
Bivariate analyses revealed that individuals who were at-risk drinkers were more often male (46% vs. 25%; P < 0.05), had ≤high school diploma (51% vs. 31%; P < 0.05), and less often had current HAART prescriptions (56% vs. 35%; P < 0.05). Of individuals receiving HAART, analyses revealed that at-risk drinkers more often had unsuppressed viremia (64% vs. 31%; P < 0.05). Logistic regression analyses revealed that when controlling for CD4 cell counts, at-risk drinkers were 4.2 times (95% CI = 1.071, 18.497) more likely to have viral loads >400 copies/ml than those who drank ≤4/5 drinks per week; individuals who completed lower levels of education were 2.8 times more likely to report at-risk drinking (AOR 2.8, 95% CI = 1.16, 6.84) as was gender, with more men drinking heavily than women (AOR 5.30, 95% CI = 1.51, 18.59).
Discussion
This study highlights the need for routine alcohol screening as an integral component of primary HIV care. These findings suggest that amount of alcohol consumed is associated with virologic suppression. Assessments between individuals who reported regular and at-risk drinking found that men, individuals with lower levels of education attainment, and those currently not prescribed HAART were more likely to be at-risk drinkers. Similar to previous research, for those on HAART, at-risk drinkers were more likely to have unsuppressed viremia, be male, and have attained lower levels of education [1–3]. Median CD4 cell counts were lowest among the at-risk drinking groups. Overall, this study highlights higher weekly amount of alcohol consumption is negatively associated with HIV RNA levels.
We found that 12% of our sample was categorized as at-risk drinkers. This proportion is higher than the HIV Costs and Services Utilization Survey yet, this seems to be similar as our definition is not one of “heavy” drinking, rather “at-risk” [1]. Our study did corroborate findings related to viral load suppression and increased alcohol consumption [6–8]. While we found that 43% of the sample had drank in the previous week, this was lower than other national survey findings where both the general and populations with HIV estimate 53% of individuals are regular drinkers [1].
This study raises the specter of safe alcohol consumption among individuals with HIV. While there is little understood of how much alcohol consumption alone affects HIV outcomes, we examined the differences among a regular drinking group of individuals and those who drink more heavily. While this consumption may be lower than high-risk levels by NIAAA guidelines, the association with worse outcomes suggests that perhaps NIAAA’s threshold is too high for populations with HIV. There is a need for clinically relevant and manageable brief interventions that are able to be delivered in HIV primary care to reduce alcohol consumption. In this study, we identified significant independent associations with unsuppressed viremia. While clinicians are often unaware of the amount of alcohol their patients typically consume, these findings suggest that more than 4 drinks for women and 5 drinks for men per week is negatively associated with viral load suppression, possibly mediated by poor medication adherence.
Routine alcohol screening has consistently been recommended by the NIAAA among all primary care providers, as well as by the Centers for Disease Control and Prevention for comprehensive HIV-related medical care [10, 12]. Providers do not routinely ask about alcohol consumption. Hence, patients may perceive a tacit approval for alcohol consumption, particularly given its social acceptability. Previous research has found that providers reported missing opportunities to screen patients when they do not have detectable viral loads or hepatitis [17]. Therefore, limited consistent screening and intervention likely results in suboptimal HIV care, possibly mediated through poor adherence to medications and clinic visits. The consequences of suboptimal care include progression of HIV disease, lack of medication adherence and/or suppressed viral loads, unfortunate synergy in neurocognitive decline, and increased hepatoxicity particularly for those co-infected with hepatitis [7, 8, 17, 18].
There are several limitations in this study. These data do not take alcohol dependence into account, specifically, these analyses only focused on the alcohol reportedly consumed during the previous 7 days in order to assess a more valid and reliable measure of frequency and quantity. Furthermore, with a cross-sectional design, we are unable to determine the longitudinal effect of alcohol on HIV outcomes. As with all self-reported data, there exists a reporting bias in these findings. The reliability of reporting risk behaviors in care settings is at times questionable, yet the format and recall period were selected to reflect a more reliable set of data.
This study offers important insight into the routine screening of alcohol frequency and quantity among individuals with HIV. Social acceptability of alcohol use serves as a significant barrier limiting the discussion of alcohol consumption in the provision of HIV care. Understanding the negative consequences of increased alcohol use will facilitate a more open discussion among patients and their care providers.
References
Galvan FH, Bing EG, Fleishman JA, London AS, Caetano R, Burnam MA, et al. The prevalence of alcohol consumption and heavy drinking among people with HIV in the United States: results from the HIV cost and services utilization study. J Stud Alcohol Drugs. 2002;63(2):179–86.
Brady KT, Randall CL. Gender differences in substance use disorders. Psychiatr Clin North Am. 1999;22(2):241–52.
Wilsnack RW, Vogeltanz ND, Wilsnack SC, Harris TR. Gender differences in alcohol consumption and adverse drinking consequences: cross-cultural patterns. Addiction. 2000;95(2):251–65.
Lopez OL, Becker JT, Dew MA, Caldararo R. Risk modifiers for peripheral sensory neuropathy in HIV infection/AIDS. Eur J Neurol: Blackwell Publishing Limited; 2004. p. 97–102.
Cooper CL, Cameron DW. Effect of alcohol use and highly active antiretroviral therapy on plasma levels of Hepatitis C virus (HCV) in patients coinfected with HIV and HCV. Clin Infect Dis: Infect Dis Soc Am. 2005;41:S105–9.
Samet JH, Horton NJ, Traphagen ET, Lyon SM, Freedberg KA. Alcohol consumption and HIV disease progression: are they related? Alcohol Clin Exp Res. 2003;27(5):862–7.
Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. JAIDS J Acquir Immune Defic Syndr. 2006;43(4):411–7.
Braithwaite RS, McGinnis KA, Conigliaro J, Maisto SA, Crystal S, Day N, et al. A temporal and dose-response association between alcohol consumption and medication adherence among veterans in care. Alcohol Clin Exp Res. 2005;29(7):1190–7.
Stein M, Herman DS, Trisvan E, Pirraglia P, Engler P, Anderson BJ. Alcohol use and sexual risk behavior among human immunodeficiency virus-positive persons. Alcohol Clin Exp Res. 2005;29(5):837–45.
CDC. Incorporating HIV prevention into the medical care of persons living with HIV: recommendations of CDC, the health resources and services administration, the national institutes of health, and the HIV medicine association of the infectious diseases society of America. Morbidity and mortality weekly report. 2003;52(RR-12).
Temoshok LR, Wald RL. Integrating multidimensional HIV prevention programs into healthcare settings. Psychosom Med. 2008;70(5):612–9.
NIAAA. Helping patients who drink too much; 2007.
Kroenke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Shacham E, Nurutdinova D, Satyanarayana V, Stamm K, Overton ET. Routine screening for depression: identifying a challenge for successful HIV care. AIDS Patient Care STDs. 2009;23(11):949–55.
Reynolds N, Sun J, Nagaraja HN, Gifford AL, Wu AW, Chesney MA. Optimizing measurement of self-reported adherence with the ACTG adherence questionnaire: a cross-protocol analysis. JAIDS J Acquir Immune Defic Syndr. 2007;46(4):402–9.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000 July 4, 2000;133(1):21–30.
Conigliaro J, Gordon AJ, McGinnis KA, Rabeneck L, Justice AC, Study VAC-S. How harmful is hazardous alcohol use and abuse in HIV infection: do health care providers know who is at risk? JAIDS J Acquir Immune Defic Syndr. 2003;33(4):521–5.
Samet JH, Horton NJ, Meli S, Freedberg KA, Palepu A. Alcohol consumption and antiretroviral adherence among HIV-infected persons with alcohol problems. Alcohol Clin Exp Res. 2004;28(4):572–7.
Acknowledgments
This publication was partially supported by Grant Number UL1 RR024992 from the National Center for Research Resources (NCRR), specifically KL2RR024994. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Dr. Overton has served as a consultant or on an advisory board for the following companies: Gilead, Bristol Myers Squibb, Glaxo-Smith-Kline, Tibotec, Merck, Monogram Sciences and Boehringer Ingelheim. He also has received research support from the following companies: Abbott, Gilead, Bavarian Nordic, Glaxo-Smith-Kline, Boehringer Ingelheim, and Tibotec.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shacham, E., Agbebi, A., Stamm, K. et al. Alcohol Consumption is Associated with Poor Health in HIV Clinic Patient Population: A Behavioral Surveillance Study. AIDS Behav 15, 209–213 (2011). https://doi.org/10.1007/s10461-009-9652-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-009-9652-9