Abstract
Despite decline in needle sharing in some countries, many injectors continue to share injection paraphernalia such as cookers and cotton. While individual and structural factors are associated with injection risk behavior, little attention has been given to the influence of social network members, such as norms, on injection paraphernalia sharing. The present study is a longitudinal analysis of the association between perceived norms and sharing syringes and non-syringe injection paraphernalia. Participants were enrolled in the STEP into Action study and reported injection drug use at both baseline and follow-up assessments (n = 398). Results showed that descriptive norms, or believing that peers practiced risky injection behaviors, predicted sharing both syringes and nonsyringe paraphernalia. However, there was no association between injunctive norms (i.e., perceived peer approval) and either syringe or non-syringe paraphernalia sharing. Changing norms may lead to sustained behavior change. Accessible, norms-based interventions are needed to discourage drug injectors from sharing injection paraphernalia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Injection Drug Users (IDUs) are at risk for blood-borne infections such as HIV and Hepatitis C (HCV) through sharing needles and other injection paraphernalia including cotton filters, rinse water, and cookers (Des Jarlais et al. 1985). Despite decline in the frequency of needle sharing in some countries, many IDUs continue to share other injection paraphernalia (Des Jarlais et al. 2007; Page et al. 2006).
Individual-level factors such as being female (Montgomery et al. 2002), homeless (Evans et al. 2003), HIV positive status (Des et al. 2004; Gasiorowicz et al. 2005) and going to a shooting gallery (Dolan et al.1987), are related to sharing injection paraphernalia. Furthermore, structural elements such as drug paraphernalia laws have been linked to decreased risky injection practices (Rich et al. 2007). In addition, recent research has shown that individuals who utilize Needle Exchange Programs are less likely to share syringes and non-syringe injection equipment (Ouellet et al. 2004).
Drug use involves several social interactions, including purchasing drugs, selling drugs and paraphernalia, sharing injection paraphernalia, and injecting in shooting galleries (Friedman et al. 1998). Many of these interactions directly or indirectly increase an injector’s risk for disease transmission. These interactions suggest a need for further understanding of how an injector’s social environment affects their risk behaviors.
Norms are one component of the social environment. Perceived norms have been conceptualized as an individual’s perceptions of what other people are doing (called descriptive norms) and perceptions of what behaviors other people consider acceptable (referred to as injunctive or proscriptive norms) (Cialdini et al.1990). Social norms are a key construct in many theories of behavior change and HIV prevention interventions (Ajzen and Fishbein 1980; Green and Kreuter 1991; Kelly et al. 1991; Latkin et al. 2003).
Research has shown that norms are associated with risk behaviors. Friedman et al. (1987) found unadjusted associations between the behavior of IDUs and their perceived behavior of others (descriptive norms). Similarly, Magura et al. (1989) found that IDUs who reported that their peers used drugs were more likely to share needles.
Since these early studies, researchers have continued to examine the relationship between norms and drug behaviors. In a sample of HIV-positive injectors, Metsch et al. (2007) found that individuals who believed that their close friends supported safer injection behaviors were less likely to lend their used syringe to someone else. Our previous research showed that believing that drug partners practiced and approved of risky behaviors was cross-sectionally associated with needle sharing among male injectors (Davey-Rothwell and Latkin 2007). Among female injectors, on the other hand, only perceived peer behavior, not perceived approval, was associated with needle sharing.
Several studies from the Drug Users Intervention Trial (DUIT) cohort, which have been conducted with young injectors in 5 US cities, have shown that peer norms are associated with risky injection behaviors. These findings include: (1) believing that peers shared injection paraphernalia was associated with injector’s own sharing of injection paraphernalia, not including needles; (2) injectors who perceived that their peers were supportive of needle sharing were more likely to give a used needle to another injector; and (3) belief that peers did not oppose needle sharing was associated with receptive needle sharing at both baseline and follow-up assessments (Bailey et al. 2007; Golub et al. 2007; Thiede et al. 2007).
Our present study is a longitudinal analysis of the association between perceived norms about injection risk behaviors at baseline and the sharing of syringes and non-syringe paraphernalia at follow-up. This study has several strengths that will enhance the published research. First, this study utilizes a longitudinal design. Although several studies have shown that norms are associated with risky injection behaviors, almost all have been cross-sectional. Since many HIV prevention interventions are designed to alter norms to change behavior, longitudinal studies are needed to assess if norms predict behavior. Second, we focus on norms among “drug buddies”, a term commonly used among our sample to describe the people they do drugs with. This group has been shown to be most influential on drug-using practices (Latkin et al. 1995, 1996). Finally, we assessed the relationship between sharing syringes and non-syringe paraphernalia and both descriptive and injunctive norms. Since each type of norm has differential effects on behavior, as well as implications for prevention, it is important to examine each type as a separate construct.
Methods
Participants
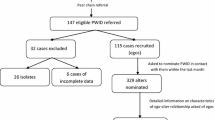
The sample was comprised of participants from the STEP Into Action study, an HIV prevention intervention designed for active drug users and their social network members. Participants were recruited through targeted street outreach, posted advertisements, and word-of-mouth. Potential participants were screened to determine eligibility. Inclusion criteria were: (1) aged 18 years and older; (2) a Baltimore city resident; (3) report of injection of cocaine or heroin in the past 3 months; and (4) willingness to refer social network members into the study. Participants who met these criteria were classified as “primary participants”. Each primary participant referred up to five social network members, who were their drug or sex partners, into the study. Eligibility criteria for network participants included: (1) 18 years or older; (2) Baltimore city resident; and (3) one of the following four behaviors: (a) self-reported use of heroin or cocaine in the past 6 months; (b) drug use with primary participant; (c) shared injection paraphernalia with primary participant; or (d) sex partner of primary participant. Network members were not required to be injection drug users. However, the present study was restricted to both index and network participants who injected drugs in the past 6 months.
Study Procedures
Both primary and network participants completed interviews during the baseline and follow-up visits. After providing written informed consent, participants completed a face-to-face interview with a trained interviewer at a community-based research clinic. Audio-Computer-Assisted- Self-Interview (ACASI) software was used to gather information on drug and sex risk behaviors. All participants were paid $35 for completion of each assessment.
Primary participants also participated in a small-group, 8-session behavioral intervention. The purpose of the intervention was to train participants to become peer educators by teaching HIV risk reduction skills and communication skills to conduct peer outreach.
Baseline interviews were completed from March 2004 to 2006. Baseline data were collected from 1,024 individuals. Approximately 82% (n = 842) of the sample (both index and network participants) reported injecting heroin, cocaine, or speedball in the previous 6 months. Follow-up data were collected from November 2004 to February 2007. By study design, the follow-up visits were scheduled to be completed 6 months after completion of the intervention sessions. The duration of the follow-up after the last intervention session plus the follow-up window period resulted in an average follow-up of 8.4 months.
Follow-up assessments were completed with 588 individuals who reported injecting at the baseline assessment (70% retention rate). Intensive tracking protocols were utilized to retain the sample including advertising at local homeless shelters and service providers and making home-based visits to deliver appointment reminder letters. Of those participants who did not complete follow-up assessments, reasons included: unable to locate (53.9%), incarceration (18.1%), death (7.1%), moved out of the area (2.8%), hospitalization or medical problem (2.0%) being in drug treatment (1.6%), no longer interested in participating (0.8%), and other reasons (13.7%) despite extensive tracking efforts.
Since the outcomes for the present study were injection behaviors, the sample was restricted to primary and social network participants (n = 398) who reported injecting drugs at both baseline and follow-up assessments.
Measures
Perceived Norms
Two types of norms were assessed in the present study- descriptive norms and injunctive norms. Perceived norms were measured by two scales that were developed specifically for the STEP study. Prior to data collection, the scales were pilot-tested to assess their usability as well as the psychometric qualities.
Descriptive Norms
Descriptive norms were assessed by a 5-item scale measuring perceived injection behaviors of drug partners (i.e. drug buddies). This scale covered 5 injection behaviors: (1) sharing needles with other people; (2) cleaning needles with bleach before injecting; (3) using a brand new needle when injecting drugs; (4) using a brand new needle when splitting drugs; and (5) using a brand new cooker for splitting drugs.
For each item, participants reported the number of drug partners who did each behavior, categorized as: none; a few (About 25%); about half (About 50%); most (About 75%); or all (100%). Each response was numerically coded as 0–4 and a composite score was calculated by adding responses to the five items (range 0–20). Prior to computing the score, items were recoded so that higher scores signified perceived norms promoting risky behavior. Psychometric analyzes demonstrated that the scale represented one factor, which explained 61.2% of the variance (eigenvalue = 3.06) and had strong internal consistency (Cronbach’s α = 0.83).
Injunctive Norms
Injunctive norms were measured by asking participants to rate their level of agreement with eight statements on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree). Each item focused on a specific injection behavior: (1) If we were pressed for time, my drug buddies would not care if we shared the same needle; (2) If we did not have enough tools, my drug buddies would not care if we shared the same needle; (3) My drug buddies would give me a hard time if I cleaned my needle with bleach before getting high; (4) My drug buddies would not say anything to me if they saw me use a dirty needle; (5) My drug buddies would get upset if I refused to lend them a needle after I used it; (6) My drug buddies would get upset if I insisted on cleaning my needle before I lent it to them; (7) My drug buddies would give me a hard time if I wanted to use a separate needle just to split drugs wet; (8) My drug buddies would give me a hard time if I wanted to split drugs dry with them.
Results of exploratory factor analysis revealed that the eight items loaded on a single factor (eigenvalue = 3.41) explained 42.6% of the total variance. An overall score was calculated by adding the responses to each item (range 8–40). Several items were recoded prior to summation so that higher scores indicated perceiving that peers approved of risky injection behaviors. Internal consistency evaluation indicated an acceptable level of reliability (α = 0.76).
Prior to analysis, the norms variables were standardized. This standardization, which provides a basis for interpretation, indicates that any change in the outcome is based on change in one standard deviation of the independent variable. This standardization also allows for comparison of the magnitude of the association between the two norms scales.
Drug-related Behaviors
The present study has two outcomes of interest: (1) syringe sharing at follow-up and (2) sharing of non-syringe injection paraphernalia at follow-up. At both baseline and follow-up, syringe sharing was measured by asking respondents about their frequency of sharing a needle after someone without cleaning it first. Responses ranged from “Never” to “More than once a day”. Individuals who reported using an unclean needle were coded as “Sharing syringes”.
At both baseline and follow-up assessment, sharing non-syringe paraphernalia was assessed through 3 items: (1) In the past 6 months, when you injected drugs, how often did you use a cooker that had been used by another person?; (2) In the past 6 months, when you injected drugs, how often did you use a cotton that had been used by another person?; (3) In the past 6 months, when you injected drugs, how often did you use rinse water after someone else used it? If respondents reported sharing any of these three pieces of paraphernalia in the past 6 months, they were coded as “Shared non-syringe paraphernalia”.
In addition, participants were asked about going to a shooting gallery and exchanging needles at the Baltimore City Needle Exchange program in the past 6 months. Finally, data were collected on the frequency of smoking and injecting heroin, cocaine/crack, and speedball in the past 6 months.
HIV Status
HIV status was ascertained through collection of an oral sample to test for HIV antibodies using the OraSure oral specimen collection device (OraSure Technologies, Inc.) The OraSure test has both high specificity and sensitivity (Gallo 1997).
Data Analysis
Frequency distributions were calculated to examine the distribution of the variables and to generate a profile of this sample of injectors. In addition, t-tests and Chi-squares were computed to compare injectors who completed the follow-up assessment and injectors who were lost to follow-up.
The two outcomes of interest: (1) Sharing syringes at follow-up and (2) Sharing non-syringe equipment at follow-up were dichotomous variables. Thus, logistic regression was done to assess the relationship between perceived norms and each of the injection risk behaviors. Two models were computed: Model A: Syringe sharing at follow-up as outcome; and Model B: Non-syringe sharing at follow-up as outcome.
In the multivariate model, both types of norms were entered simultaneously to examine the independent effect of each norm variable in the presence of the other variable. Since baseline sharing behaviors (syringe and non-syringe paraphernalia), injecting at a shooting gallery, gender, race, age, homelessness, and HIV status have all been associated with injection risk behavior, they were adjusted for in the multivariate models. We also controlled for intervention effect since attending intervention sessions may have led to changes in risk behaviors.
Since the sample included both primary and network participants, there was a need to account for possible clustering of responses. To account for this correlation, General Estimating Equation (GEE) was employed (Zeger and Liang 1986). GEE adjusts for variance within and between clusters of network members. Data were analyzed using SPSS 15.0 and Stata 8.0.
Results
Exploratory analyzes was done to compare individuals who reported injecting at baseline and completed the follow-up assessment (n = 588) and injectors who only completed the baseline assessment (n = 254). The two groups were compared across demographics (i.e. age, gender, race, education, and employment), drug use (smoking crack, and heroin, cocaine, and speedball injection), baseline sharing paraphernalia behaviors (syringes and non-syringe paraphernalia), and perceived norms (descriptive and injunctive norms). Individuals who completed the follow-up were more likely to be female [28.8 vs. 20.7%, χ 2 (1, N = 842) = 4.98, P < 0.05], African American [84.4 vs. 69.2%, χ 2 (1, N = 842) = 24.97, P < 0.01], and older [43.1 years (SD = 7.67) vs. 40.9 years (SD = 8.90), P < 0.01]. While there were no differences in sharing syringes at baseline, injectors who were lost to follow-up were more likely to share non-syringe paraphernalia at baseline [75.9 vs. 68.0%, χ 2 (1, N = 842) = 5.39, P < 0.05]. There were no differences in either type of perceived norms, education, employment, type of injection or smoking crack.
The majority of the study’s sample was African American (82.2%) and male (63.1%). The sample reported monthly income <$500 (48.9%), low rates of full-time employment (15.6%), and less than a high school education (55.1%). The most common types of drug use were injecting heroin (91.9%) and injecting speedball (80.9%). Approximately one-third (31.2%) of the sample injected drugs at a shooting gallery in the past 6 months. In addition, 147 participants reported utilizing the local Needle Exchange program to exchange needles at least once in the past 6 months. While 40.7% reported sharing syringes at baseline and 29.4% shared syringes by follow-up, many more participants reported sharing at least one piece of non-syringe paraphernalia at baseline and follow-up (70.6 and 63.1%., respectively).
Mean scores and standard deviations were computed for each of the norms variables. These data are shown in Table 1. As shown, individuals who shared syringes or non-syringe paraphernalia at follow-up had significantly higher descriptive norms scores. These scores indicate that individuals who shared injection paraphernalia, compared to non-sharers, were more likely to believe that their drug buddies practiced risky injection behaviors. While syringe and non-syringe paraphernalia sharers had higher injunctive norms scores than non-sharers, there was no significant difference between the two groups. These scores indicate that individuals who shared injection paraphernalia were no more likely to believe that their drug buddies approved of risky injection behavior compared to non-sharers.
Results of the multivariate analysis are shown in Table 2. Model A refers to the logistic model with syringe sharing as the outcome. As shown in the table, descriptive norms were significantly associated with syringe sharing at follow-up [AOR: 1.66, 95% CI: 1.17, 2.35]. There was not a significant relationship between injunctive norms and syringe sharing. Syringe sharing at follow-up was associated with baseline syringe sharing (P < 0.001), age (P < 0.05), and homelessness (P < 0.01).
Model B is the multivariate model with the outcome of non-syringe equipment sharing. As shown in Model B, descriptive norms predicted non-syringe paraphernalia sharing at follow-up [AOR: 1.42, 95% CI: 1.07–1.89] even after controlling for baseline behavior. There was no significant relationship between injunctive norms and non-syringe paraphernalia sharing. Sharing non-syringe paraphernalia at follow-up was associated with baseline non-syringe paraphernalia sharing [AOR: 5.51, 95% CI: 3.09–9.79] and injecting at a shooting gallery [AOR: 2.07, 95% CI: 1.15, 3.71].
Discussion
In this sample of active heroin and cocaine injectors, we found that perceived norms about drug partners’ injection practices predicted engagement in these practices at follow-up. Specifically, individuals who believed that drug partners engaged in risky injection behaviors were significantly more likely to share syringes and non-syringe paraphernalia at the follow-up assessment. This association persisted even after adjusting for baseline risk behaviors. In addition, we found that peer approval for practicing risk behaviors did not predict sharing syringes or non-syringe paraphernalia at follow-up.
The results of this study indicate that perceived norms about what drug partners do are sufficiently stable to predict risk behaviors over 8 months later. As norms tend to be self-sustaining, changing norms may lead to sustained behavior change. Interventions are needed that are designed to promote risk reduction norms. However, since norms pertaining to peer approval did not influence risk behavior at follow-up, after adjusting for descriptive norms, it may be important for intervention messages to distinguish between norms. Based on our study’s findings, intervention messages such as “Your drug buddies don’t share their works” may be more powerful than “Your drug buddies don’t think sharing works is cool.”
It is important to note that contrary to our study, several cross-sectional studies have found an association between injunctive norms and risk behavior (Golub et al. 2007; Metsch et al. 2007). A main difference between our study and previous studies is that we focused on norms among drug buddies rather than a more general reference group such as peers or friends. We are unable to assess if the approval of another group, such as friends, would influence behavior. More research is needed to examine the longitudinal influence of different relationships such as friends, family, or sex partners on injection behaviors.
The high scores for both the descriptive and injunctive norms scales indicate that the prevailing norms are that drug users are engaging in risky injection practices and approve of these behaviors. These norms need to be altered so that risk reduction is seen as a normative behavior. Norms may be developed and transferred through observing others’ behaviors, receiving positive and negative reinforcement for behaviors, and verbal communication (Oostveen et al. 1996). Since our study focused on drug buddies, it is likely that individuals based their norms on what their drug partners did when they were using drugs together. One intervention approach is to train IDUs in risk reduction practices so they can model safer behaviors, which will promote risk reduction norms. Through modeling their behaviors, other injectors may begin to perceive that safer injection is widely practiced. These perceptions may influence their own behaviors.
This study has some limitations that should be noted. First, all data were self-reported. We used this method to minimize the potential for social desirability bias by utilizing ACASI which has been shown to decrease this bias and increase validity of self-reported data on risk behaviors (Mascalino et al. 2002). In addition, the participants were self-selected volunteers who may not be representative of the IDU population at-large. A final limitation is bias in our sample since those who completed the follow-up survey compared to those lost to follow-up were more likely to be African American or female.
As shown in this study, sharing injection paraphernalia, especially non-syringe equipment, continues to be prevalent. The majority of respondents reported sharing cookers, cotton, or rinse water at baseline and follow-up. Given the infectivity of HIV and especially HCV, these data are alarming. Interventions that are easy to access and reach a wide audience are needed to decrease sharing of any type of injection equipment. Changing norms is a valuable approach to HIV prevention that must occur at both interpersonal and structural levels. Both interpersonal and structural interventions have the power of altering norms and ultimately changing risky behaviors. In addition to peer education, an interpersonal approach, structural interventions, such expansion of needle exchange program services in municipalities including Baltimore are needed to increase access to new, sterile, clean injection paraphernalia and provide a setting that promotes norms against sharing injection equipment.
References
Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice Hall.
Bailey, S. L., Ouellet, L. J., Mackesy-Amiti, M. E., Golub, E. T., Hagan, H., Hudson, S. M., et al. (2007). Perceived risk, peer influences, and injection partner type predict receptive syringe sharing among young adult injection drug users in five US cities. Drug and Alcohol Dependence, 91(Suppl. 1), S18–S29. doi:10.1016/j.drugalcdep.2007.02.014.
Cialdini, R. B., Reno, R. R., & Kallgreen, C. A. (1990). A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology, 58(6), 1015–1026. doi:10.1037/0022-3514.58.6.1015.
Davey-Rothwell, M. A., & Latkin, C. A. (2007). Gender differences in social network influence among injection drug users: Perceived norms and needle sharing. Journal of Urban Health, 84(6), 691–703. doi:10.1007/s11524-007-9215-1.
Des Jarlais, D. C., Braine, N., Yi, H., & Turner, C. (2007). Residual injection risk behavior, HIV infection, and the evaluation of syringe exchange programs. AIDS Education and Prevention, 19(2), 111–123. doi:10.1521/aeap.2007.19.2.111.
Des Jarlais, D. C., Friedman, S. R., & Hopkins, W. (1985). Risk reduction for the acquired immunodeficiency syndrome among intravenous drug users. Annals of Internal Medicine, 103, 755–759.
Des, J., Perlis, T., Arasteh, K., Hagan, H., Milliken, J., Braine, N., et al. (2004). “Informed altruism” and “partner restriction” in the reduction of HIV infection in injecting drug users entering detoxification treatment in New York City, 1990–2001. Journal of Acquired Immune Deficiency Syndromes, 35(2), 158–166. doi:10.1097/00126334-200402010-00010.
Dolan, M. P., Black, J. L., Deford, H. A., Skinner, J. R., & Robinowitz, R. (1987). Characteristics of drug abusers that discriminate needle-sharers. Public Health Reports, 102(4), 395–398.
Evans, J. L., Hahn, J. A., Page-Shafer, K., Lum, P. J., Stein, E. S., Davidson, P. J., et al. (2003). Gender differences in sexual and injection risk behavior among active young injection drug users in San Francisco (the UFO Study). Journal of Urban Health, 80(1), 137–146. doi:10.1093/jurban/jtg137.
Friedman, S. R., Des Jarlais, D., Sotheran, J. L., Garber, J., Cohen, H., & Smith, I. (1987). AIDS and self-organization among intravenous drug users. The International Journal of the Addictions, 22(3), 201–219.
Friedman, S. R., Furst, T., Jose, B., Curtis, R., Neaigus, A., Des Jarlais, D. C., et al. (1998). Drug scene roles and HIV risk. Addiction (Abingdon, England), 93(9), 1403–1416. doi:10.1046/j.1360-0443.1998.939140311.x.
Gallo, D. (1997). Evaluation of a system using oral mucosal transidate for HIV-1 antibody screening and confirmatory testing. OraSure HIV clinical trials group. Journal of the American Medical Association, 277(3), 254–258. doi:10.1001/jama.277.3.254.
Gasiorowicz, M., Llanas, M. R., DiFranceisco, W., Benotsch, E. G., Brondino, M. J., Catz, S. L., et al. (2005). Reductions in transmission risk behaviors in HIV-positive clients receiving prevention case management services: Findings from a community demonstration project. AIDS Education and Prevention, 17(Suppl. A), 40–52. doi:10.1521/aeap.17.2.40.58694.
Golub, E. T., Strathdee, S. A., Bailey, S. L., Hagan, H., Latka, M. H., Hudson, S. M., et al. (2007). Distributive syringe sharing among young adult injection drug users in five US cities. Drug and Alcohol Dependence, 91(Suppl. 1), S30–S38. doi:10.1016/j.drugalcdep.2007.02.013.
Green, L. W., & Kreuter, M. W. (1991). Health promotion planning: An educational and environmental approach (2nd ed.). Mountain View, CA: Mayfield Publishing Company.
Kelly, J. A., St Lawrence, J. S., Diaz, Y. E., Stevenson, L. Y., Hauth, A. C., Brasfield, T. L., et al. (1991). HIV risk behavior reduction following intervention with key opinion leaders of population: An experimental analysis. American Journal of Public Health, 81(2), 168–171. doi:10.2105/AJPH.81.2.168.
Latkin, C. A., Mandell, W., Oziemkowska, M., Celentano, D., Vlahov, D., Ensminger, M., et al. (1995). Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug and Alcohol Dependence, 38, 1–9. doi:10.1016/0376-8716(94)01082-V.
Latkin, C. A., Mandell, W., Vlahov, D., Oziemkowska, M., & Celentano, D. (1996). People and places: Behavioral settings and personal network characteristics as correlates of needle sharing. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology, 13(3), 273–280.
Latkin, C. A., Sherman, S., & Knowlton, A. (2003). HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology, 22(4), 332–339. doi:10.1037/0278-6133.22.4.332.
Magura, S., Grossman, J. I., Lipton, D. S., Siddiqi, Q., Shapiro, J., Marion, I., et al. (1989). Determinants of needle sharing among intravenous drug users. American Journal of Public Health, 79(4), 459–462. doi:10.2105/AJPH.79.4.459.
Mascalino, G. E., Celentano, D. D., Latkin, C. A., Strathdee, S. A., & Vlahov, D. (2002). Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-negative injection drug users. AIDS Education and Prevention, 14(5), 367–378. doi:10.1521/aeap.14.6.367.24075.
Metsch, L. R., Pereyra, M., Purcell, D. W., Latkin, C. A., Malow, R., Gomez, C. A., et al. (2007). Correlates of lending needles/syringes among HIV-seropositive injection drug users. Journal of Acquired Immune Deficiency Syndromes, 46(Suppl. 2), S72–S79.
Montgomery, S. B., Hyde, J., De Rosa, C. J., Rohrbach, L. A., Ennett, S., Harvey, S. M., et al. (2002). Gender differences in HIV risk behaviors among young injectors and their social network members. The American Journal of Drug and Alcohol Abuse, 28(3), 453–475. doi:10.1081/ADA-120006736.
Oostveen, T., Knibbe, R., & De Vries, H. (1996). Social influences on young adults’ alcohol consumption: Norms, modeling, pressure, socializing, and conformity. Addictive Behaviors, 21(2), 187–197. doi:10.1016/0306-4603(95)00052-6.
Ouellet, L., Huo, D., & Bailey, S. L. (2004). HIV risk practices among needle exchange users and nonusers in Chicago. Journal of Acquired Immune Deficiency Syndromes, 37(1), 1187–1196. doi:10.1097/01.qai.0000120802.43677.ea.
Page, J. B., Shapshak, P., Duran, E. M., Even, G., Moleon-Borodowski, I., & Llanusa-Cestero, R. (2006). Detection of HIV-1 in injection paraphernalia: Risk in an era of heightened awareness. AIDS Patient Care and STDs, 20(8), 576–585.
Rich, J. D., Hogan, J. W., Wolf, F., De Long, A., Zaller, N. D., Mehrotra, M., et al. (2007). Lower syringe sharing and re-use after syringe legalization in Rhode Island. Drug and Alcohol Dependence, 89(2–3), 292–297. doi:10.1016/j.drugalcdep.2007.02.016.
Thiede, H., Hagan, H., Campbell, J. V., Strathdee, S. A., Bailey, S. L., Hudson, S. M., et al. (2007). Prevalence and correlates of indirect sharing practices among young adult injection drug users in five US cities. Drug and Alcohol Dependence, 91(Suppl. 1), S39–S47. doi:10.1016/j.drugalcdep.2007.03.001.
Zeger, S. L., & Liang, K. Y. (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 42(1), 121–130. doi:10.2307/2531248.
Acknowledgment
This study was funded by the National Institute on Drug Abuse (grant# 1RO1 DA016555).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Davey-Rothwell, M.A., Latkin, C.A. & Tobin, K.E. Longitudinal Analysis of the Relationship Between Perceived Norms and Sharing Injection Paraphernalia. AIDS Behav 14, 878–884 (2010). https://doi.org/10.1007/s10461-008-9520-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-008-9520-z