Abstract
South Africa continues to be the global epicenter of HIV infection. Further, extensive gender disparities in HIV infection exist with females four times as likely to be infected with HIV/AIDS as males (UNAIDS, AIDS epidemic update, 2006; WHO, Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections, 2006). A cross-sectional collection of drug users recruited in the Pretoria region of South Africa (N = 385) was used to model HIV infection as a function of sexual risk behaviors and drug use as modified by gender. Receiving money from illicit sources and knowing someone with AIDS were loosely associated with HIV. Gender interactions were observed for age, cocaine use and condom use. Gender stratified analyses revealed that males who used condoms, were younger and tested negative for cocaine use were less likely to test positive for HIV. Findings suggest that males may have more control of risk behaviors and support the need for gender specific prevention strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many sub-Saharan African countries remain in the midst of a “global epidemic” of HIV infection with 32% of all people with HIV and 34% of deaths due to AIDS occurring in South Africa (UNAIDS 2006; WHO 2006). Perhaps what is so staggering about these estimates is that while such epidemics in the rest of the world are primarily concentrated among injection drug users, men who have sex with men, and sex workers and their partners (Doherty et al. 2000; Simbayi et al. 2005; Todd 2007), in South Africa the dominant mode of acquiring HIV is through heterosexual sex (Heymann and Edstrom 1991; Hunter 1993). In South Africa, females bear the brunt of the HIV epidemic and are four times as likely to be infected with HIV/AIDS as males (UNAIDS 2006; WHO 2006). Further, death from AIDS in young females aged 20–29 has tripled from 1997 to 2004 (UNAIDS 2006; WHO 2006).
Several studies have hypothesized reasons for gender disparities in HIV infection in this region. Sexual transmission of HIV has been determined to be a function of infectiousness, mode of contact and susceptibility of individual persons (Vernazza et al. 1999). That is, variability in sexual transmission may be due to both biological difference in infectiousness and transmission as well as differences in sexual risk behaviors (Vernazza et al. 1999).
Biological factors that may predispose women to a higher susceptibility of HIV infection include differences in genital contact surfaces with coital injury more common in women, and women are exposed to infectious fluids for a longer period of time than men (MacPhail et al. 2002; Nicolosi et al. 1994). Several partner studies have determined that male to female transmission is two to three times greater than female to male transmission. (de Vincenzi 1994; Nicolosi et al. 1994). Also, young women are particularly at risk of HIV infection due to the vulnerability of immature genital tract tearing during sexual activity (Turmen 2003). Although several biological explanations exist for the gender disparity of HIV in South Africa, we cannot forget that the HIV epidemic in South Africa occurs in the “framework of a complex social atmosphere” and therefore societal norms that may directly or indirectly affect risk behaviors may also influence HIV infectivity (Hunter 1993).
With this in mind, several studies of HIV risk behaviors have been conducted in South Africa. Simbayi et al. (2005) studied the risk factors and behaviors among young people in a South African township. They found that 68% of men and 56% of women reported high risk behaviors, with high risk behavior in men associated with fewer years of education, lower levels of AIDS knowledge, infrequent condom use and cannabis use. Whereas, risk behaviors in women were correlated with beliefs that condoms get in the way of sex and high rates of unprotected vaginal intercourse (Simbayi et al. 2005). Other studies have found that positive HIV seroprevalence was highest among young females aged 16–25, with seroprevalence higher in women divorcees and widows (Gregson et al. 2001). In a population of male factory workers in Harare, Zimbabwe, risk factors for HIV included marital status, history of STD, multiple partners, cash payment for sex and condom use (Bassett et al. 1996). Further, the incidence of HIV-1 infection was explored in the adult rural population of Uganda; findings indicated HIV-1 rates to be highest in young females aged 20–24 and males aged 20–44 (Kengeya-Kayondo et al. 1996).
Further, gender and age interactions have been observed, with rates of HIV infection for males greater than 20 years being four times that of younger males (Kengeya-Kayondo et al. 1996). It has been proposed that gender and age interactions in HIV prevalence may be due to the relative age and socio-economic status of sexual partners with social norms condoning older male/younger female partnering (Luke 2005; MacPhail et al. 2002). That is, age and economic asymmetries in partnerships exist which in turn create gender power imbalances and thus imbalances in sexual risk behaviors (Luke 2005). Therefore, prevention efforts in South Africa may need to focus upon individual, age related, and gender specific sexual risk behavior trends (UNAIDS 2006).
Although a variety of studies in South Africa have explored the relationship between risk behaviors and HIV infection, until recently few studies have looked at drug users (Kalichman et al. 2006; Leggett 1999; Parry et al. 2008a, b; Sawyer et al. 2006; Sher et al. 1986; Wechsberg et al. 2006). Common illicit drugs of abuse in South Africa include cannabis and methaqualone followed by crack cocaine, powder cocaine and heroin (Parry et al. 2002; Parry et al. 2008a, b) with the most common mode of ingestion being smoking while injection is uncommon in South Africa. Although prevalence of injection drug use is low, use of non-injection drugs in the past 30 days has been estimated to be as high as 20% in some communities (Parry et al. 2002).
Studies of HIV prevalence in drug users may be especially warranted given the vulnerability of this population to high risk sexual behaviors during and as a result of substance use (Parry et al. 2008a, b; Sawyer et al. 2006). In this paper, we explore behavioral factors including sexual risk behaviors and recent drug use, in a population of drug users recruited in the Pretoria region of South Africa. Further, in view of gender disparities in HIV prevalence, we attempt to elucidate the specific factors that increase women’s vulnerability to HIV/AIDS infection. Therefore, this manuscript explores and describes some of the HIV prevalence discrepancy in terms of gender differences in risk behaviors.
Methods
The neurobehavioral model of HIV study is an epidemiological examination of neuropsychological, social-behavioral risk factors of HIV, and hepatitis A, B, and C with sites in the US, South Africa, and Russia. The present study is based on the South Africa site, which enrolled black South Africans between 2002 and 2006 in the Pretoria and Johannesburg regions. The South Africa study was funded by NIDA’s Southern Africa Initiative as a supplement to a parent study conducted in the US (DA014498). Referrals to drug and HIV treatment facilities were provided to all study participants following established protocols. All research staff in South Africa underwent intensive HIV counseling, recruitment, and assessment training provided by local and US clinicians and researchers on issues related to ethics, recruitment and assessment protocols, HIV counseling, and crisis management. The study and consent forms were approved in the US by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (FWA00000287) and in South Africa by the South African Medical Research Ethics Committee (FWAIRB00001569).
Participants
Equal numbers of males and females were recruited via community based word of mouth in Pretoria and from informal settlements in the Pretoria and Johannesburg region. Study participants were recruited by trained project staff from a variety of community based sources. Recruitment involved street outreach in Pretoria and surrounding informal settlements, treatment programs, bars, local emergency rooms, and health clinics. To be eligible for the study, participants had to be aged 18–40 years, report using injection or non-injection drugs during the previous 6 months and live in or around Pretoria. Informed consent was obtained during the initial visit prior to baseline assessment and participants received financial remuneration (150 ZAR, approximately $19 for a completed visit and an additional 50 ZAR, approximately $6 for transportation costs). The present study is based on a sample of 385 black South African drug users. This study analysis excluded a small number of white drug users recruited into the South Africa study because the number of white subjects was too small to analyze the data by race/ethnicity and substantial socioeconomic differences between white and black participants in the study.
Measures
The South African study assessment battery includes neuropsychological tools on executive functioning, attention and intellectual functioning and a detailed HIV risk behavior interview adapted from tools developed during landmark studies of HIV risk behavior (e.g., Vlahov et al. 1991) and used extensively at the US study site in Baltimore with adult drug users. The HIV risk behavior interview was subsequently pilot-tested with South African drug users prior to use in the study. Measures on drug-related HIV risk behaviors included drug use cessation and relapse, risky injection practices (i.e., direct and indirect syringe sharing), and injection in high risk contexts (e.g., shooting galleries). Detailed measures on a range of drugs used by type, route of administration, frequency and quantity, including tobacco, alcohol, cannabis, heroin, other opiates, cocaine, methaqualone (a sedative recreational drug commonly known as Mandrax), and other drugs were included. Measures on sexual practices include the number and types of partners (e.g., gender, regular partner, casual partner), type(s) of sexual acts (oral, vaginal and anal intercourse), condom use, survival sex (sex for money, drugs, shelter, food and protection), and incident sexually transmitted disease. Drug use and sexual risk behaviors were assessed for various time periods including: 24 h, last month, last 6 months and lifetime behaviors.
Diagnostic substance use and HIV testing was carried out at a pathology laboratory operated by a national pathology services. The assessment was administered on two separate occasions 6 months apart. At each assessment, blood and urine samples were collected. HIV testing included the standard ELISA screening and confirmatory Western Blots. Urinalysis (with gas chromatography-mass spectrometry methods) assessed the presence of psychoactive substances, including cannabinoids, cocaine, opiates and methaqualone to verify participant self-report of recent drug use. For this manuscript, we examine data from the first assessment of both recent (condom use for last sexual encounter) and lifetime (number of partners) self-reported sexual risk behaviors and recent substance use; i.e., urinalysis results of substance use.
Data Analysis
HIV prevalence was assessed for the sample overall as well as separately by gender. HIV correlates including demographics, drug use and sexual risk behaviors were assessed using logistic regression. First, simple logistic regression was used to compute unadjusted odds ratios (OR) and their 95% confidence intervals (CI). Multiple logistic regression was used to calculate adjusted odds ratios (AOR) and their 95% CI. Gender interactions with age were included in the model due to known age gender interactions in the literature. Additional gender interactions were assessed in terms of risk behaviors using a backward elimination process at an alpha = 0.1. The model was assessed for overall model fit and assumptions were tested. Since several gender interactions were determined to be both statistically and clinically significant, a gender stratified analysis was then conducted using two multiple logistic regression models.
All participants provided a HIV test result. For each covariate, missing data was less than 1%. Cumulative covariate missing data was approximately 5%. Since the percentage of missing data was small, a complete case analysis was utilized; in the presence of small amounts of missing data, estimates of complete case analysis will have little bias (Lipsitz et al. 1998).
Results
Sample Description
The sample consisted of 385 black South African males (49%) and females (51%) between the ages of 18 and 40 (Table 1). Most subjects reported having received some high school education. Only 33% of participants reported that their main income source was from legal activities; whereas, 30% reported illicit sources of income (excluding sex work) and 25% reported income from sex trade. Further, 86% of subjects tested positive for cannabis, 36% tested positive for cocaine and 56% tested positive for opiates and 2% tested positive for methaqualone. Although inclusion criteria included both injection and non-injection drug users, only 1 participant reported ever injecting in the sample of 385. Only 61% of participants reported using a condom the last time that they had sex and 59% of participants reported knowing someone with AIDS.
Overall prevalence of HIV for this sample was 36.4%. Unadjusted odds ratio (OR) results in Table 1 indicate that females (51%) have 3.79 the odds of males (21%) of testing HIV positive (95% CI = 2.42, 5.93, P < 0.01). Also, the older the participant the more likely they were to test positive for HIV. Specifically, participants aged 21–25 have 1.96 (95% CI = 1.13, 3.40, P < 0.05) the odds of participants less than 21 years of age to test positive for HIV. Those older than 26 years of age, have 2.70 (95% CI = 1.60, 4.56, P< 0.01) the odds of participants less than 21 years of age to test positive for HIV. No association was observed for education level and HIV seroprevalence. However, participants reporting sex trade as their main source of income had 2.76 (95% CI = 1.58, 4.80, P < 0.01) the odds of those reporting legal forms of income to test HIV positive. Recent drug use risk behaviors including cannabis, cocaine and opiates were not associated with HIV. Additionally, sexual risk behaviors of condom use, number of sex partners and type of relationship were not associated with a positive HIV test in the simple logistic regression results.
Overall Model: Multiple Logistic Regression
Multiple logistic regression was used to model HIV on demographics as well as drug risk and sexual risk behaviors. Known interactions in the literature including gender and age were included in the model. Further gender interactions were assessed in terms of risk behaviors using a backward elimination process. A final model with good fit using the Hosmer and Lemeshow Lack of Fit Test (Chi-Square (df) = 8.59(8), P = 0.38) and a global null hypothesis test (Chi-Square(df) = 88.44(23), P< 0.0001) had the following interaction terms included: gender and age (Wald Chi-Square(df) = 9.86(2), P < 0.01), gender and cocaine use (Wald Chi-Square(df) = 11.52(1), P < 0.01) and gender and condom use (Wald Chi-Square(df) = 4.29(1), P = 0.06). Regardless of gender, having an illegal source (excluding sex work) of income (AOR = 2.37, 95% CI = 1.00, 5.62, P = 0.07) and knowing someone with AIDS (AOR = 0.59, 95% CI = 0.35, 1.01, P = 0.06) was loosely associated with having a positive HIV test.
Stratified Model: Multiple Logistic Regression
Since several gender interactions were observed a gender stratified analysis was used to compare the adjusted odds of HIV for males versus females. That is, a multiple logistic regression model was estimated separately for males and females. Using the same covariates in each of the stratified models as that of the overall model, the global fit statistics test (Chi-Square(df) = 43.69(16), P < 0.001) for males was still good; however, for females the global fit statistics test (Chi-Square(df) = 17.46(16), P = 0.42) indicates that the covariates included in the model may not adequately explain HIV odds for females.
Adjusted odds ratio (AOR) results in Table 2 indicate that for males older age was associated with testing positive for HIV. Specifically, males aged 26 and older have 9.58 (95% CI = 2.59, 35.43, P < 0.01) the odds of males younger than 21 to test positive for HIV. This strong association with age was not demonstrated for females. For both genders, education level, cannabis use, opiate use, and type of first or last relationship were not associated with HIV. Furthermore, source of income differed for males and females, with males reporting no sex trade as a source of income. Sex trade was loosely associated with HIV; females who reported sex trade as a main source of income had 2.50 (95% CI = 0.94, 6.69, P = 0.07) the odds of females reporting licit sources of incomes to test positive for HIV.
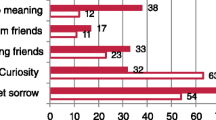
Recent cocaine use also differed by gender. Males testing positive for cocaine had 3.08 (95% CI = 1.00, 9.48, P = 0.05) the odds of testing positive for HIV. However, for females testing positive for cocaine was protective. That is, females who tested positive for cocaine had 0.36 (95% CI = 0.17, 0.78, P < 0.01) the odds of females who did not test positive for cocaine to have HIV. Gender stratified analyses further revealed that males who used condoms in their last sexual encounter were less likely to test positive for HIV infection (AOR = 0.37, 95% CI = 0.14, 0.98, P < 0.05). This association was not observed in females. Also, knowing someone with AIDS was protective for males (AOR = 0.35, 95% CI = 0.13, 0.92, P < 0.05) but not for females (AOR = 0.71, 95% CI = 0.36, 1.42, P = 0.33). Although not statistically significant, a linear trend was observed in the adjusted odds ratios of the number of sex partners; as the number of sex partners for males increased, the odds of testing positive for HIV increased. Males who had ten or more partners had 2.51 (95% CI = 0.65, 9.75, P = 0.18) the odds of males have three or less partners to test positive for HIV.
Discussion and Conclusion
Chronic disease such as HIV must be addressed in its specific environment and social context. In South Africa unlike other countries, infection of HIV is due to heterosexual transmission and females experience a greater burden of the epidemic. It has been hypothesized that gender disparities in HIV in South Africa may be due both to biological and socio-demographic and cultural reasons. HIV infection occurs, in a context, were societal norms that directly or indirectly affect risk behaviors may also influence HIV infectivity (Hunter 1993). That is, gender power imbalances may affect women’s ability to negotiate safe sex practices (Langen 2005) and social norms often permit younger female/older male partnerships (Luke 2005). In our study, observed gender differences in sexual risk behaviors were observed in a sample of drug users including condom use, partner selection (with younger females partnering with older males) and sex trade (with females more likely be involved in sex trade compared to men). Therefore, prevention methods of HIV in South Africa should focus on gender issues specific to South Africa. Specifically, prevention strategies may need to focus on risk factors that may differ by gender including sexual risk behaviors. Further, high risk groups such as drug users who may be at greater risk of infection need to be identified in order to better develop prevention and treatment strategies for individuals.
For this sample of 385 drug users, the prevalence of HIV was found to be 36.4%; a slightly higher prevalence than that of 32% in the general South African population (UNAIDS 2006; WHO 2006). In our sample, recent cannabis and heroin use verified via urinalysis was not associated with testing positive for HIV either overall or within gender. However there was an association between HIV and cocaine use which differed by gender. Specifically, males who tested positive for cocaine were more likely to test positive for HIV. However among females, testing positive for cocaine was protective. This result was unexpected considering that among males and females cocaine use is associated with sexual risk behaviors, e.g., not using protection (Parry et al. 2008a, b) as well as increased sexual desire (Volkow et al. 2007). Further, cocaine use in males has been associated with sexual dysfunction (Cocores et al. 1988). Therefore, the association between HIV and cocaine use by gender needs to be replicated and further explored to determine the direction of the association or rather whether results were spurious.
Similar to existing literature an age/gender interaction was observed in our study (Kengeya-Kayondo et al. 1996; Luke 2005). Younger females (<26) had a higher odds of testing positive for HIV compared to older females; whereas, older males (>26 years of age) had a higher odds of testing positive for HIV when compared to younger males. The presence of an age/gender interaction is consistent with extant literature, suggesting that older men/younger women partnering outside of marriage is socially acceptable (Luke 2005). Furthermore, gender and age based socioeconomic status disparities that give males more power than females and older males more power than younger males have produced both age and economic inequality in non-marital partnerships (Luke 2005). Existing literature and results from our study confirm the need to develop gender specific prevention strategies that focus on the power asymmetries that exist in male/female partnerships.
This analysis demonstrated further gender differences in sexual risk behaviors. Principally, gender stratified analyses revealed that males who used condoms in their last sexual encounter were less likely to test positive for HIV infection; however, this association was not observed in females. These results may demonstrate that males may have more control of their risk behaviors than females and therefore have less of a risk for HIV infectivity. Further findings demonstrated that male drug users in this sample did not report a main source of income as sex trade (either buying or selling). However, 49% of female drug users in this sample reported their main source of income as sex trade and of those females 53% tested positive for HIV. Knowing these gender differences in sexual risk behavior is invaluable for developing prevention strategies that incorporate gender activity and equality.
Results of this study did not demonstrate a statistically significant association between HIV and number of self-reported partners. Although not statistically significant, as the number of partners increased among males so did the odds of testing positive for HIV. This relationship was not observed in females, i.e., the odds of HIV was less for females who have greater than ten partners versus females with less than three partners while controlling for sex trade. This may be due to safer sex practices or high awareness of HIV/AIDS in the sex trade industry which may not have been captured in this study (AIDS 1996).
Several limitations of this study should be noted including the limited sample size for tests of interaction. Although a sample size of 385 is moderate to large and with this sample size several statistically significant interactions were kept in the overall model; analysis with interaction requires large sample sizes. In order to obtain a parsimonious model, we used a backward elimination method to choose statistically significant interactions at an alpha level of 0.10. Given, a larger sample size we may have been able to delineate further gender differences. Future epidemiologic studies may want to include a design with adequate sample size in order to further observe effect modification.
A targeted sampling method using community based word of mouth and street outreach was used for this study. While, nonrandom sampling methods may have inherent sample selection biases, the sampling frame could not be easily defined for this hidden population and therefore a random sampling plan for informal settlements was not feasible. Future studies of hidden populations may want to use other sampling techniques including respondent driven sampling.
For this analysis, we were interested in sexual risk behaviors in drug users and recent drug use was obtained using a urinalysis test result. Future studies will not only include urinalysis but also self-reported drug use in order to better gauge lifetime or past year drug use as correlates of HIV. Other studies have determined that cannabis use is associated with sexual risk behaviors and HIV infection (Simbayi et al. 2005; Wechsberg et al. 2008). The amount or frequency of substance use captured via self-report may be a better predictor of HIV status. Furthermore, our study sample was limited to black Africans in the Pretoria region who use drugs. Therefore, our findings may only generalize to similar populations.
Finally, it should be noted that the overall model in which this analysis was based had great fit. However, once the analysis was stratified by gender, the model with the same covariates still fit males well but not females. Therefore, future analysis may want to focus on predictors of HIV in females, particularly those with high risk behaviors. Other sexual risk behaviors should be explored in a model of HIV for females. We chose covariates including sex trade, condom use and number of partners because of the pervasiveness of such behaviors among at risk populations (Chen et al. 2007; Gregson et al. 2001; Hunter 1993; Leggett 1999; Simbayi et al. 2005). However, additional female specific risk behaviors may need to be delineated.
Although there are several limitations of this study, this study is novel due to focus upon a vulnerable population in South Africa, drug users. In addition, this manuscript suggests the need for further investigation of HIV by gender; in particular, female specific models of HIV need to be delineated with good predictive power. Female specific studies need to be developed in this population to test whether socioeconomic status, employment, marital status, partner drug use and sexual risk behavior, intimate partner violence, individual beliefs and acceptance of societal norms and gender and power theories (Wechsberg et al. 2006; Wingood and DiClemente 2000) are associated with HIV status.
Finally, this study’s findings contribute to the comprehension of HIV infectivity in South Africa and support the need for gender specific prevention intervention strategies. Given the results from this study, short term prevention efforts should focus on the promotion of safe sex among women who indicate a main source of income as sex trade. Furthermore, prevention studies are needed that focus on gender equality through socio-economic independence and empowerment for women (Wechsberg et al. 2006). Also, gender differences in the odds of HIV by age found in this study and in existing literature suggest that prevention efforts may be needed that challenge traditional norms of older male/younger female partnerships. Results from this study in men, suggest that prevention interventions may need to include drug use treatment, particularly cocaine use problems and the promotion of safe sex through condom use. Furthermore, these interventions are likely to be most beneficial if implemented early and continuously across development to promote behavioral changes in sexual risk such as safe sex negotiation for both men and women.
References
AIDS. (1996). Ground-breaking research into Ghanaian sex-workers suggests high awareness. Country surveys. AIDS Analysis Africa, 6, 14.
Bassett, M. T., McFarland, W. C., Ray, S., Mbizvo, M. T., Machekano, R., van de Wijgert, J. H., et al. (1996). Risk factors for HIV infection at enrollment in an urban male factory cohort in Harare, Zimbabwe. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology, 13, 287–293.
Chen, L., Jha, P., Stirling, B., Sgaier, S. K., Daid, T., Kaul, R., et al. (2007). Sexual risk factors for HIV infection in early and advanced HIV epidemics in sub-Saharan Africa: Systematic overview of 68 epidemiological studies. PLoS ONE, 2, e1001. doi:10.1371/journal.pone.0001001.
Cocores, J. A., Miller, N. S., Pottash, A. C., & Gold, M. S. (1988). Sexual dysfunction in abusers of cocaine and alcohol. The American Journal of Drug and Alcohol Abuse, 14, 169–173. doi:10.3109/00952999809001544.
de Vincenzi, I. (1994). A longitudinal study of human immunodeficiency virus transmission by heterosexual partners. European study group on heterosexual transmission of HIV. The New England Journal of Medicine, 331, 341–346. doi:10.1056/NEJM199408113310601.
Doherty, M. C., Garfein, R. S., Monterroso, E., Brown, D., & Vlahov, D. (2000). Correlates of HIV infection among young adult short-term injection drug users. AIDS, 14, 717–726. doi:10.1097/00002030-200004140-00011.
Gregson, S., Mason, P. R., Garnett, G. P., Zhuwau, T., Nyamukapa, C. A., Anderson, R. M., et al. (2001). A rural HIV epidemic in Zimbabwe? Findings from a population-based survey. International Journal of STD and AIDS, 12, 189–196. doi:10.1258/0956462011917009.
Heymann, D. L., & Edstrom, K. (1991). Strategies for AIDS prevention and control in sub-Saharan Africa. AIDS, 5, S197–S208.
Hunter, D. J. (1993). AIDS in sub-Saharan Africa: The epidemiology of heterosexual transmission and the prospects for prevention. Epidemiology, 4, 63–72. doi:10.1097/00001648-199301000-00012.
Kalichman, S. C., Simbayi, L. C., Kagee, A., Toefy, Y., Jooste, S., Cain, D., et al. (2006). Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Social Science and Medicine, 62, 1641–1649. doi:10.1016/j.socscimed.2005.08.021.
Kengeya-Kayondo, J. F., Kamali, A., Nunn, A. J., Ruberantwari, A., Wagner, H. U., & Mulder, D. W. (1996). Incidence of HIV-1 infection in adults and socio-demographic characteristics of seroconverters in a rural population in Uganda: 1990–1994. International Journal of Epidemiology, 25, 1077–1082. doi:10.1093/ije/25.5.1077.
Langen, T. T. (2005). Gender power imbalance on women’s capacity to negotiate self-protection against HIV/AIDS in Botswana and South Africa. African Health Sciences, 5, 188–197.
Leggett, T. (1999). Crack, sex work, and HIV. AIDS Analysis Africa, 9, 3.
Lipsitz, S. R., Parzen, M., & Ewell, M. (1998). Inference using conditional logistic regression with missing covariates. Biometrics, 54, 295–303. doi:10.2307/2534015.
Luke, N. (2005). Confronting the ‘sugar daddy’ stereotype: Age and economic asymmetries and risky sexual behavior in urban Kenya. International Family Planning Perspectives, 31, 6–14. doi:10.1363/3100605.
MacPhail, C., Williams, B. G., & Campbell, C. (2002). Relative risk of HIV infection among young men and women in a South African township. International Journal of STD and AIDS, 13, 331–342. doi:10.1258/0956462021925162.
Nicolosi, A., Correa Leite, M. L., Musicco, M., Arici, C., Gavazzeni, G., & Lazzarin, A. (1994). The efficiency of male-to-female and female-to-male sexual transmission of the human immunodeficiency virus: A study of 730 stable couples. Italian study group on HIV heterosexual transmission. Epidemiology, 5, 570–575. doi:10.1097/00001648-199411000-00003.
Parry, C. D., Bhana, A., Pluddemann, A., Myers, B., Siegfried, N., Morojele, N. K., et al. (2002). The South African community epidemiology network on drug use (SACENDU): Description, findings (1997–99) and policy implications. Addiction, 97, 969–976.
Parry, C. D., Dewing, S., Petersen, P., Carney, T., Needle, R., Kroeger, K., & Treger, L. (2008b). Rapid assessment of HIV risk behavior in drug using sex workers in three cities in South Africa. AIDS and Behavior, in press. Epub ahead of print retrieved March 7, 2008, from http://www.springerlink.com/content/hm67411g7x57g2j8.
Parry, C., Petersen, P., Dewing, S., Carney, T., Needle, R., Kroeger, K., et al. (2008a). Rapid assessment of drug-related HIV risk among men who have sex with men in three South African cities. Drug and Alcohol Dependence, 95, 45–53. doi:10.1016/j.drugalcdep.2007.12.005.
Sawyer, K. M., Wechsberg, W. M., & Myers, B. J. (2006). Cultural similarities and differences between a sample of black/African and colored women in South Africa: Convergence of risk related to substance use, sexual behavior, and violence. Women and Health, 43, 73–92. doi:10.1300/J013v43n02_05.
Sher, R., de Miranda, D. S., Metz, J., Sifris, D., Lyons, S. F., & Schoub, B. D. (1986). Lack of evidence of HIV infection in drug abusers at present. South African Medical Journal, 70, 776–777.
Simbayi, L. C., Kalichman, S. C., Jooste, S., Cherry, C., Mfecane, S., & Cain, D. (2005). Risk factors for HIV-AIDS among youth in Cape Town, South Africa. AIDS and Behavior, 9, 53–61. doi:10.1007/s10461-005-1681-4.
Todd, C. S., Earhart, K. C., Botros, B. A., Khakimov, M. M., Giyasova, G. M., Bautista, C. T., et al. (2007). Prevalence and correlates of risky sexual behaviors among injection drug users in Tashkent, Uzbekistan. AIDS Care, 19, 122–129. doi:10.1080/09540120600852150.
Turmen, T. (2003). Gender and HIV/AIDS. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics, 82, 411–418. doi:10.1016/S0020-7292(03)00202-9.
UNAIDS. (2006). AIDS epidemic update. Geneva: UNAIDS/WHO.
Vernazza, P. L., Eron, J. J., Fiscus, S. A., & Cohen, M. S. (1999). Sexual transmission of HIV: Infectiousness and prevention. AIDS, 13, 155–166. doi:10.1097/00002030-199902040-00003.
Vlahov, D., Anthony, J. C., Celentano, D., Solomon, L., & Chowdhury, N. (1991). Trends of HIV-1 risk reduction among initiates into intravenous drug use 1982–1987. The American Journal of Drug and Alcohol Abuse, 17, 39–48. doi:10.3109/00952999108992808.
Volkow, N. D., Wang, G. J., Fowler, J. S., Telang, F., Jayne, M., & Wong, C. (2007). Stimulant-induced enhanced sexual desire as a potential contributing factor in HIV transmission. The American Journal of Psychiatry, 164, 157–160. doi:10.1176/appi.ajp.164.1.157.
Wechsberg, W. M., Luseno, W. K., Karg, R. S., Young, S., Rodman, N., Myers, B., & Parry, C. D. (2008). Alcohol, cannabis, and methamphetamine use and other risk behaviours among black and coloured South African women: A small randomized trial in the Western Cape. International Journal of Drug Policy, in press. Epub ahead of print retrieved April 19, 2008, from http://www.ncbi.nlm.nih.gov/pubmed/18207723.
Wechsberg, W. M., Luseno, W. K., Lam, W. K., Parry, C. D., & Morojele, N. K. (2006). Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS and Behavior, 10, 131–137. doi:10.1007/s10461-005-9036-8.
WHO. (2006). Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections. Geneva: World Health Organization.
Wingood, G. M., & DiClemente, R. J. (2000). Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education and Behavior, 27, 539–565. doi:10.1177/109019810002700502.
Acknowledgments
Funding for this study was made possible by NIDA supplement to R01DA014498 and T32DA007292 funding through the National Institute of Drug Abuse. The authors would like to acknowledge the Drug Dependence Epidemiology Training grant publication work group for assistance in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hedden, S.L., Whitaker, D., Floyd, L. et al. Gender Differences in the Prevalence and Behavioral Risk Factors of HIV in South African Drug Users. AIDS Behav 13, 288–296 (2009). https://doi.org/10.1007/s10461-008-9467-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-008-9467-0