Abstract
The present study investigated the relationships between positive religious coping (e.g., seeking spiritual support) and spiritual struggle (e.g., anger at God) versus viral load, CD4 count, quality of life, HIV symptoms, depression, self-esteem, social support, and spiritual well-being in 429 patients with HIV/AIDS. Data were collected through patient interview and chart review at baseline and 12–18 months later from four clinical sites. At baseline, positive religious coping was associated with positive outcomes while spiritual struggle was associated with negative outcomes. In addition, high levels of positive religious coping and low levels of spiritual struggle were associated with small but significant improvements over time. These results have implications for assessing religious coping and designing interventions targeting spiritual struggle in patients with HIV/AIDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals faced with difficult or stressful experiences often use religious coping methods (e.g., seeking spiritual support) to deal with these events (see Pargament 1997). A review of research on religious coping indicated that the prevalence of religious coping ranges from 30% to almost 80% across various samples (Harrison et al. 2001).
Researchers have identified two types of religious coping techniques: positive religious coping and spiritual struggle. Positive religious coping consists of methods that reflect a secure relationship with God, a belief in life’s larger meaning, and a sense of spiritual connectedness with others. Positive religious coping includes strategies such as seeking spiritual support, benevolent religious reappraisals (e.g., trying to find a lesson from God in the event), and purification rituals (Pargament et al. 1998). Spiritual struggle is defined as an expression of conflict, question, and doubt regarding matters of faith, God, and religious relationships that represents an effort to conserve or transform a spirituality that has been threatened or harmed (Pargament et al. 2005). Spiritual struggle tends to be less common than positive religious coping (Meisenhelder and Marcum 2004; Tarakeshwar and Pargament 2001) and differs from other forms of spiritual coping by the spiritual stress that emerges within the coping process. Positive religious coping and spiritual struggle are not mutually exclusive; use of positive religious coping strategies does not indicate an absence of spiritual struggle (Fitchett et al. 2004).
The purpose of this study is to explore positive religious coping and spiritual struggle in individuals with HIV/AIDS within a bio-psycho-social-spiritual model (Prest and Robinson 2006; Wright et al. 1996). Specifically, this study examines the cross-sectional and longitudinal relationships between positive religious coping and spiritual struggle versus biological, psychological, social, and spiritual well-being in individuals with HIV/AIDS.
Qualitative research indicates that individuals with HIV/AIDS reflect on their spirituality after receiving an HIV diagnosis (Tarakeshwar et al. 2006) and often view their lives and illness from a spiritual perspective (Guillory et al. 1997; Tarakeshwar et al. 2006). In addition, despite less involvement in organized religion, individuals diagnosed with HIV/AIDS incorporate God (Jenkins 1995; Woodward and Sowell 2001) and previous experiences with religiosity and spirituality (Jacobson et al. 2006) into the coping process. They also use religious coping strategies to find meaning in their lives and impending deaths (Corless 2002; Hall 1998).
Consistent with this body of qualitative research, quantitative research suggests that spirituality is important to people with HIV/AIDS and that these individuals incorporate their spirituality into the coping process (Cotton et al. 2006; Cotton et al. 2006). In fact, 45% of a sample of individuals with HIV reported an increase in their spirituality in response to their HIV diagnosis (Ironson et al. 2006). In addition, spirituality has been associated with beneficial outcomes in individuals with HIV/AIDS (Cotton et al. 2006). For example, higher levels of spirituality were associated with less psychological distress (Simoni et al. 2002), less pain and greater energy (Ramer et al. 2006), less depression (Coleman 2004; Simoni and Ortiz 2003; Yi et al. 2006), better mental well-being, better cognitive and social functioning, and fewer HIV symptoms (Coleman 2004). Higher levels of spirituality also predicted greater likelihood of feeling life has improved since being diagnosed with HIV (Szaflarski et al. 2006).
Spirituality has also been associated with physiological indicators of HIV progression. Participants who reported an increase in spirituality following an HIV diagnosis had lower rates of CD4 cell loss and lower rates of viral load increase over four years than participants whose spirituality decreased following their diagnosis (Ironson et al. 2006). In addition, viewing God as loving and merciful was associated with increases in CD4 and lower viral load over a four-year period (Ironson et al. 2006). These results suggest that spirituality may have beneficial health outcomes for individuals with HIV/AIDS.
Religious behaviors have also been associated with beneficial outcomes in HIV-positive individuals (Sowell et al. 2000). For example, prayer, church attendance, and association with a religious denomination have been associated with less emotional distress, better quality of life, better medical adherence, higher CD4 counts, and the feeling that life is better than before the HIV diagnosis (Flannelly and Inouye 2001; Parsons et al. 2006; Szaflarski et al. 2006; Woods et al. 1999). In addition, more frequent prayer and formal religious practice were associated with greater use of adaptive coping strategies and greater perceived support from family members in HIV-positive men and women (Somlai and Heckman 2000).
These results indicate that spirituality and religious behaviors are associated with positive outcomes in individuals with HIV/AIDS. Nevertheless, relatively few studies have explicitly investigated the relationship between religious coping strategies and well-being in people with HIV/AIDS. In addition, the results of available research do not create a coherent picture. For example, research indicates that greater use of positive religious coping strategies is associated with lower levels of depression and anxiety after controlling for HIV-related stressors (Woods et al. 1999), less psychological distress (Simoni et al. 2002), better quality of life (Flannelly and Inouye 2001), less alcohol use, greater life satisfaction, and greater optimism (Cotton et al. 2006). However, positive religious coping in people with HIV has also been associated with worse overall functioning and less HIV mastery after controlling for demographic and clinical (e.g., time since diagnosis and CD4 count) variables (Cotton et al. 2006). In addition, in a study of HIV positive men, spiritual coping was not associated with mental health related quality of life (Frame et al. 2005). These studies suggest that religious coping may be associated with beneficial outcomes in individuals with HIV/AIDS. However, further research is necessary to clarify this relationship.
Spirituality and religious behaviors typically represent positive aspects of religiosity. However, it is important to consider potential negative aspects of spirituality, such as spiritual struggle. Research on spiritual struggle in people with HIV/AIDS is limited. However, qualitative research indicates that individuals with HIV experience spiritual struggle, particularly in the months following their diagnosis (Tarakeshwar et al. 2006). In addition, a quantitative study suggested that a marker of spiritual struggle, discontent spiritual coping (e.g., anger at God and alienation from God), was associated with higher levels of depression and loneliness in individuals with HIV/AIDS (Jenkins 1995). Similarly, negative religious beliefs, such as a belief that HIV is a sin, have been associated with poor medical adherence (Parsons et al. 2006). A view of God as judgmental and punishing was associated with faster CD4 decline and greater increases in viral load in a sample of HIV positive men and women (Ironson et al. 2006). Finally, spiritual struggle in individuals with HIV was associated with less HIV mastery, lower self-esteem, and less optimism (Cotton et al. 2006). These studies suggest that negative aspects of spirituality can be detrimental to individuals with HIV/AIDS.
Individuals with HIV/AIDS may be particularly vulnerable to the detrimental outcomes associated with spiritual struggle for various reasons. First, HIV/AIDS is a high-magnitude stressor that places considerable strain on the orienting system, a generalized system of beliefs, practices, relationships, and values that shape how individuals view and approach the world (Pargament 1997). Orienting systems include coping resources, including spirituality, for dealing with stressful events and burdens that inhibit the individual’s ability to cope successfully. Individuals’ orienting systems may not contain adequate coping resources to deal with an event as stressful as HIV/AIDS, increasing the risk for negative outcomes following spiritual struggle.
Second, individuals with HIV/AIDS may lose coping resources, such as social support, due to the stigmatization that often accompanies an HIV/AIDS diagnosis (Corless 2002; Holt et al. 1999). Patients with HIV/AIDS may experience other stigma-related losses as well, such as being fired from their jobs or evicted from their apartments (Menz 1987). Finally, people diagnosed with HIV/AIDS may lose support and feel ostracized from their religious communities because HIV/AIDS is associated with behaviors, such as homosexuality, sexual promiscuity, and drug use, that run counter to the beliefs of many religious traditions (Cotton et al. 2006; Holt et al. 1999; Woodward and Sowell 2001; Yarhouse and Anderson 2002). As a result, persons with HIV/AIDS may not have adequate spiritual resources to address questions regarding their relationships with God and life after death.
Positive religious coping and spiritual struggle have been largely unexplored in individuals living with HIV/AIDS. In addition, research on religiousness in patients with HIV/AIDS has focused on a narrow range of outcome variables and has not examined the longitudinal relationship between religious coping and well-being. The current study applies a bio-psycho-social-spiritual conceptual model (Prest and Robinson 2006; Wright et al. 1996) to positive religious coping and spiritual struggle in individuals with HIV/AIDS. Specifically, this study explores the cross-sectional and longitudinal relationships between positive religious coping and spiritual struggle versus biological (viral load, CD4 count, HIV symptoms), psychological (quality of life, depression, self-esteem), social (social support), and spiritual (harmony, strength of faith, compassion) well-being. We hypothesized that positive religious coping would be associated cross-sectionally with positive psychological, physiological, social, and spiritual outcomes at baseline and that spiritual struggle would be associated with negative outcomes (Aim 1). We also hypothesized that individuals who utilized positive religious coping strategies at baseline would experience improvements in well-being over time. Conversely, we hypothesized that individuals who reported spiritual struggle at baseline would experience declines in well-being over time (Aim 2).
Methods
Participants and Procedure
The sample was recruited between February 2002 and February 2003 from four sites: the George Washington University Medical Center, Washington, DC; the Veterans Affairs (VA) Pittsburgh Healthcare System, Pittsburgh, PA; the Cincinnati VA Medical Center, Cincinnati, OH; and the University of Cincinnati Medical Center, Cincinnati, OH. The initial sample consisted of 450 outpatients with various stages of HIV/AIDS. For these analyses, we excluded 21 participants who were neither Caucasian nor African-American in order to increase the racial homogeneity of the sample, leaving an analytic sample of 429 participants. Physiologic indicators, including viral load levels and CD4 count, were collected via chart review and patient interview. Questionnaires were administered by trained interviewers at baseline and again 12–18 months later (Time 2). All participants received $30 for completing each questionnaire battery.
Measures
Biological Outcomes
Physiologic Indicators. Viral load and CD4 levels were ascertained through chart review. For purposes of categorization and interpretation, viral load levels were dichotomized as detectable (>400 copies/ml) or undetectable (≤400 copies/ml).
HIV Symptoms. The HIV Symptom Index (HSI; Justice et al. 2001) was used to assess the presence of and degree the person feels bothered by 20 symptoms (e.g., fever, headache, fatigue) by using a five-point scale ranging from “I do not have this symptom” (0) to “I have this symptom and it bothers me a lot” (4) (Cronbach’s alpha = 0.91). Responses were dichotomized so that the response options “I have this symptom and it doesn’t bother me” and “I have this symptom and it bothers me a little” were coded zero and response options “I have this symptom and it bothers me” and “I have this symptoms and it bothers me a lot” were coded one. Five items from the HSI were excluded for the current analyses, due to overlap with similar items on the Center for Epidemiological Studies-Depression (CESD-10) scale used to measure depression (discussed below).
Psychological Outcomes
Quality of Life. Quality of life was assessed with the HIV/AIDS-Targeted Quality of Life (HAT-QoL) scale. This 34-item questionnaire assesses functioning in nine areas on a five-point scale ranging from “all of the time” (1) to “none of the time” (5) with higher scores indicating better quality of life (Holmes and Shea 1998). The nine dimensions include: Overall Functioning (6 items, Cronbach’s alpha = 0.86), Life Satisfaction (4 items, Cronbach’s alpha = 0.87), Health Worries (4 items, Cronbach’s alpha = 0.86), Financial Worries (3 items, Cronbach’s alpha = 0.89), HIV Medication Worries (5 items, Cronbach’s alpha = 0.84), HIV Mastery (i.e., comfort with how HIV was contracted; 2 items, Cronbach’s alpha = 0.85), Disclosure Worries (5 items, Cronbach’s alpha = 0.81), Provider Trust (3 items, Cronbach’s alpha = 0.80), and Sexual Function (2 items, Cronbach’s alpha = 0.90). Scores on each subscale were adjusted to range from 0 to 100.
Depressive Symptoms. The 10-item Center for Epidemiological Studies-Depression (CESD-10) scale was used to evaluate depressive symptoms (Andresen et al. 1994; Radloff 1977). Participants rate their feelings and behaviors over the past week on a four-point scale ranging from “rarely or none of the time (less than 1 day; 0)” to “most or all of the time (5–7 days; 3).” Total scale scores range from 0 to 30 with higher scores indicating more evidence of depressive symptoms (Cronbach’s alpha = 0.87).
Self-Esteem. The Rosenberg Global Self-Esteem Measure (RGSM) was used to evaluate self-esteem. Participants report how often each of six self-esteem statements applies to them using a four-point scale from “almost always true” (1) to “never true” (4) with additional options for “don’t know” and “not applicable” (Robinson and Shaver 1969). Responses are summed to create a total score with higher scores indicating greater self-esteem (Cronbach’s alpha = .81).
Social Outcomes
Social Support. The Brief Interpersonal Support Evaluation (ISEL-12) was used to measure social support. This 12-item scale assesses belonging (social connectedness), appraisal (perceived availability of confidants), and tangible (physical) support on a four-point Likert scale ranging from “definitely false” (1) to “definitely true” (4) (Cohen et al. 1985). Item responses are summed to create a total score, with higher scores indicating greater social support (Cronbach’s alpha = 0.90).
Spiritual Outcomes
The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale-Expanded (FACIT-Sp-Ex; Brady et al. 1999) is a 23-item questionnaire that assesses common themes in many spiritual traditions, including a sense of comfort, harmony and peace in life, strength of faith, and compassion, gratitude, and a sense of connectedness to others and a higher power. Participants rate each item on a five-point scale ranging from “not at all” (0) to “very much” (4). Items are summed to yield an overall score (Cronbach’s alpha = 0.95), with higher scores indicating greater spiritual well-being.
Religious Demographics
The Duke Religion Index (DUREL; Koenig et al. 1997) is a five-item index of religiousness. This study analyzed the item assessing organized religious activity (attendance at religious services) and the item assessing non-organized religious activity (meditating, praying, or religious text study). These items are rated on a six-point scale with higher scores indicating more frequent participation in religious activities. For frequency of religious service attendance, responses range from “never” (1) to “more than once a week” (6). For participation in religious activities, responses range from “rarely or never” (1) to “more than once per day” (6). The remaining three items of the DUREL were not used in these analyses.
Religious Coping
Positive Religious Coping and Spiritual Struggle. Positive religious coping strategies and spiritual struggle were measured with a shortened version of the RCOPE, the Brief RCOPE (Pargament et al. 2000). The Brief RCOPE is a 14-item scale with seven items for each dimension. Participants rate their use of individual coping strategies when dealing with difficult life situations on a four-point scale ranging from “not at all” (1) to “a great deal” (4). Positive religious coping was assessed with the Positive Religious Coping subscale of the Brief RCOPE (Cronbach’s alpha = 0.92), which includes strategies such as seeking spiritual support and benevolent religious reappraisals. Spiritual struggle was assessed with the Negative Religious Coping subscale, which contains items such as “questioned God’s love for me” and “wondered whether God had abandoned me” (Cronbach’s alpha = 0.82). Responses are summed to create subscale scores, with higher scores indicating more frequent use of the coping strategy.
Statistical Analyses
Descriptive statistics included means, standard deviations, and proportions. Bivariate correlations were obtained between positive religious coping and spiritual struggle at baseline versus baseline outcome variables. These analyses tested the cross-sectional hypotheses that positive religious coping would be related to positive outcomes, and spiritual struggle to negative outcomes. Regression analyses were also conducted with Time 2 physiological, psychological, social, and spiritual outcome measures as the dependent variables. Analyses were conducted on 16 outcome measures and were unadjusted for multiple comparisons. For each outcome measure, we constructed two models. In the first, designated Model A, the independent variables were age, race, sex, education, sexual orientation, length of time since HIV diagnosis, religious affiliation, and the baseline score on the measure being predicted at Time 2. In the second model, designated Model B, baseline religious coping and spiritual struggle were added to Model A predictors. All reported regression coefficients are standardized coefficients.
Post-hoc, to aid interpretation of significant regression coefficients, we examined changes in outcome measures as they related to initial positive religious coping or spiritual struggle scores. These analyses examined the hypotheses that participants scoring higher on positive religious coping at baseline would report better outcomes at Time 2 than participants with lower positive religious coping scores. Conversely, participants scoring lower on spiritual struggle at baseline would report better outcomes at Time 2 than participants scoring higher on spiritual struggle. These post-hoc analyses were exploratory. Cut-offs between high and low religious coping scores were data-driven as current research and theory do not suggest specific cut-offs for comparisons.
Results
Description of Sample
The demographics of the sample generally reflect the current HIV epidemic. Participants’ mean age was 43.3 years (SD = 8.4) and 85.5% were male. The sample was evenly split racially with 52.7% African American and 47.3% Caucasian participants. Almost three quarters (73%) of participants described themselves as single. Regarding sexual orientation, 50.3% of participants endorsed “gay or lesbian,” 33.3% indicated heterosexual, and 11.4% bisexual.
Religious demographic variables indicate that this is a mild to moderately religious sample. Participants were predominately Christian (73.7%) with 25.0% identifying as Baptist, 12.4% as Roman Catholic, 9.1% as nondenominational Christian, 4.9% as Methodist, and 22.3% as “other Christian.” The remainder of the sample consisted of Jews (1.6%), Muslims (1.2%), “other” (2.8%), “none” (11.7%), and “undesignated” (9.3%). Regarding religious behaviors, approximately one-third of the sample (29.4%) reported never attending religious services. Another third of participants (32.1%) reported attending services “once a year or less” to “a few times a year” while 38.6% indicated attending religious services “a few times a month” or more. A large proportion of the sample (41.3%) reported engaging in private religious activities “rarely or never.” Approximately a quarter (26.6%) of the sample reported participating in private religious activities “a few times a month” to “two or more times a week” while 32.1% of participants engaged in such behaviors daily or more.
A total of 329 (76.7%) of the original 429 participants were available at Time 2. Participants who completed follow-up interviews were more likely to be Caucasian and had higher scores on the disclosure worries subscale of the HAT-QoL than participants who completed baseline interviews only. The two groups did not differ on other demographic, predictor, or outcome variables. For the 329 patients with follow-up data, outcome measures and religious coping values were generally similar at baseline and Time 2 (Table 1).
Aim 1: Correlations between Baseline Outcome Variables and Religious Coping Correlations between positive religious coping or spiritual struggle and outcome variables at baseline indicate that positive religious coping was associated with greater levels of spirituality and self-esteem (Table 2). The relationships between positive religious coping and quality of life were mixed. Positive religious coping was correlated with greater life satisfaction but less HIV mastery. Spiritual struggle was associated with having a detectable viral load, poorer quality of life, more bothersome HIV and depressive symptoms, lower levels of spirituality, less social support, and poorer self-esteem.
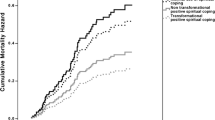
Aim 2: Main Effect of Baseline Religious Coping on Time 2 Outcome Measures Model A significantly predicted all 16 outcome variables (see Table 3 for correlations between predictor variables and outcome measures). Model B and the change in R2 from Model A to Model B were significant for overall function, HIV mastery, depressive symptoms, spirituality, and log CD4 (Table 4). The changes in R2 for these outcomes variables, while statistically significant, were modest in magnitude. The change in R2 from Model A to Model B was not significant for the remaining outcome measures. The dependent variables at baseline were significant predictors in all regression analyses, with higher levels of baseline variables associated with higher levels at Time 2. In addition, years since HIV diagnosis (β = −0.12, p < .01; Table 4) and religious affiliation (β = −0.06, p < .05; Table 4) were significant predictors of log CD4. No other demographic variables emerged as significant predictors.
Positive religious coping was a significant predictor (β = 0.12, p < .05) of FACIT-Sp-Ex scores at Time 2 after controlling for FACIT-Sp-Ex scores at baseline, spiritual struggle, and demographic variables. For all participants, average FACIT-Sp-Ex scores increased from baseline to Time 2 (Table 1). However, participants with lower positive religious coping scores (<14; 25.6% of total sample) had average increases in FACIT-Sp-Ex scores of 0.42 points, while those participants with higher positive religious coping scores (≥14; 74.4% of current sample) increased on average by 0.80 points.
Spiritual struggle was a significant predictor (β = −0.13, p < .05) of overall function scores at Time 2 after controlling for baseline overall function scores, positive religious coping, and demographic variables. Across the sample, participants showed an average increase in scores on overall function from baseline to Time 2 (Table 1). However, while participants with low to moderate spiritual struggle scores showed a small average increase in overall function scores of 0.36, those with the highest spiritual struggle scores (>19; 4.9% of total sample) showed an average decrease in overall function of 5.73 points.
Spiritual struggle was a significant predictor (β = −0.12, p < .05) of HIV mastery at Time 2 after controlling for baseline HIV mastery, positive religious coping, and demographic variables. Across all participants, average HIV mastery scores increased from baseline to Time 2 (Table 1). However, while participants with low or moderate spiritual struggle scores averaged an increase in HIV mastery of 3.53, those with the highest spiritual struggle scores (>19; 4.9% of total sample) decreased in HIV mastery on average by 14.00 points.
Spiritual struggle was also a significant predictor (β = 0.12, p < .01) of depressive symptoms at Time 2 after controlling for baseline depressive symptoms, positive religious coping, and demographic variables. Across all participants, average depressive symptom scores decreased from baseline to Time 2 (Table 1). However, while participants with low or moderate spiritual struggle scores showed average decreases in CESD-10 scores of 0.33 points, those with the highest spiritual struggle scores (>19; 4.9% of total sample) on average increased in CESD-10 scores by 1.29 points.
Finally, spiritual struggle was a significant predictor (β = −0.09, p < .01) of log CD4 at Time 2 after controlling for baseline log CD4, positive religious coping, and demographic variables. Across all participants, average log CD4 scores increased from baseline to Time 2 (Table 1). However, while participants with low or moderate spiritual struggle scores (<11; 67.9% of total sample) had mean increases in log CD4 of 0.13 points, those with the high spiritual struggle scores (≥12; 32.1% of total sample) had average decreases in log CD4 of 0.01 points.
Discussion
Religious coping by individuals with HIV/AIDS has not been extensively explored and previous research has various methodological limitations. This study expands on previous research by investigating the cross-sectional and longitudinal relationships between positive religious coping and spiritual struggle versus various indices of psychological, physiological, social, and spiritual well-being in patients with HIV/AIDS. Consistent with our hypotheses, cross-sectional analyses showed that positive religious coping was associated with positive outcomes, including greater self-esteem and spirituality. Spiritual struggle was associated with negative outcomes, such as poorer quality of life, higher levels of HIV symptoms, and higher levels of depressive symptoms. In addition, the longitudinal analyses indicated that participants scoring relatively high on positive religious coping reported improvements in well-being over time whereas participants scoring high on spiritual struggle reported declines over time, even when controlling for demographic variables. Though the magnitudes of these effects were modest, the findings were consistent across various outcomes, including depressive symptoms, quality of life, spiritual well-being, and clinical indicators of disease severity.
The cross-sectional findings support two potential interpretations of the relationship between religious coping and well-being. First, poorer health status and well-being may lead to spiritual struggle by challenging the individual’s worldview and creating confusion about spiritual matters. Empirical evidence for this interpretation is limited. However, mental health practitioners have reported that the quality of patients’ relationships with God declines with the onset of psychological problems and improves following successful treatment (e.g., Jones 1991; Rizzuto 1979).
A second possible interpretation is that spiritual struggle leads to lower levels of psychological, physiological, social, and spiritual well-being and positive religious coping leads to greater well-being. This second interpretation is supported by the longitudinal results of this study. Specifically, high levels of spiritual struggle were associated with declines in physical function and psychological and spiritual well-being over time, while high levels of positive religious coping were associated with improvements in well-being and spirituality over time. These longitudinal findings also corroborate previous research (Fitchett et al. 1999; Pargament et al. 2004). Of course, both interpretations may be applicable. For example, declines in health status and well-being may cause spiritual struggle, which then leads to further deterioration of well-being.
These results have practical implications for improving well-being in patients with HIV/AIDS through religious coping. First, this study suggests that assessing positive religious coping and spiritual struggle in patients with HIV/AIDS is important. Positive religious coping techniques may be beneficial to patients with HIV/AIDS. Therefore, individuals who are utilizing religious resources should be supported and encouraged in their religious coping efforts. In addition, health professionals should be open to further incorporating positive religious coping techniques into individuals’ treatment. Perhaps more importantly, early identification of individuals experiencing spiritual struggle could allow professionals to intervene and perhaps avert the detrimental effects of spiritual struggle. Appropriate interventions may include discussing religious or spiritual beliefs, referring to a pastoral counselor or religious clergy, or referring for psychotherapy to address spiritual struggle (Fitchett et al. 1999, 2004; Pargament et al. 2004).
Second, these results suggest that psycho-spiritual interventions that promote positive religious coping and target spiritual struggle may improve psychological, physiological, and spiritual well-being in individuals with HIV/AIDS. Research on psycho-spiritual interventions is in its infancy (Pargament et al. 2005). However, manualized psycho-spiritual interventions for HIV/AIDS patients have been developed. For example, “Lighting the Way: A Spiritual Journey to Wholeness,” is a nondenominational group intervention for women with HIV (Pargament et al. 2004) that addresses existential issues relevant to women with HIV and incorporates discussions of spiritual resources and spiritual struggle. A second intervention offers participants the opportunity to identify personally relevant positive religious coping strategies and express their spiritual struggle (Tarakeshwar et al. 2005). Preliminary assessment of this intervention indicated that participants experienced increases in self-rated religiosity and positive religious coping and decreases in spiritual struggle and depression over the course of the intervention. A third intervention taught participants to repeat a silent mantram, a word or phrase with a spiritual association, throughout the day. Participation in the intervention was associated with declines in intrusive thoughts and anger and improvements in quality of life and spirituality (Bormann et al. 2006). Finally, a psycho-spiritual intervention to increase motivation for HIV prevention in drug users has also been designed and evaluated. Initial results indicate that this intervention increases motivation to prevent HIV and reduces HIV risk behavior (Avants et al. 2005; Margolin et al. 2006). The preliminary success of these interventions suggests that psycho-spiritual treatments can be relevant and beneficial to individuals with HIV/AIDS. However, additional research on their effectiveness is needed.
The results of this study are limited by characteristics of the sample and measures. First, the sample was limited to Caucasian and African American participants with primarily Judeo-Christian religious affiliations. Therefore, these results cannot be generalized to individuals of other ethnicities and religious denominations. Second, data were collected at east coast and Midwest locations, limiting generalizability to other regions of the country. Third, participants in this study were outpatients with access to state-of-the-art HIV/AIDS treatments: 76.2% were receiving highly active antiretroviral therapy and 51.7% had HIV viral loads below detectable limits. As a result, the findings of this study may not generalize to individuals who do not have access to treatment or who are not benefiting from treatment. Finally, the large number of outcome measures is also a limitation and may have increased the experiment-wise error. However, it is important to note that the number of significant changes from Model A to Model B was greater than expected by chance.
Despite these limitations, the results of this study suggest that positive religious coping is associated with small but significant improvements in well-being in individuals with HIV/AIDS over time, whereas spiritual struggle is associated with small but significant declines in well-being over time. Therefore, assessing positive religious coping and spiritual struggle in patients with HIV/AIDS may help health professionals identify and support patients using positive religious coping methods while targeting those individuals whose spiritual struggle may adversely affect their well-being.
References
Andresen, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventative Medicine, 10, 77–84.
Avants, S. K., Beitel, M., & Margolin, A. (2005). Making the shift from ‘addict self’ to ‘spiritual self’: Results from a stage I study of Spiritual Self-Schema (3-S) therapy for the treatment of addiction and HIV risk behavior. Mental Health, Religion and Culture, 8, 167–177.
Bormann, J. E., Gifford, A. L., Shively, M., Smith, T. L., Redwine, L., Kelly, A., et al. (2006). Effects of spiritual mantram repetition on HIV outcomes: A randomized controlled trial. Journal of Behavioral Medicine, 29, 359–376.
Brady, M. J., Peterman, A. H., Fitchett, G., & Cella, D. (1999). The expanded version of the functional assessment of chronic illness therapy – spiritual well-being scale (FACIT-SP-Ex): Initial report of psychometric properties. Annals of Behavioral Medicine, 21, 129.
Cohen, S., Mermelstein, R., Kamarck, T., & Hoberman, S. (1985). Measuring the functional components of social support. In I. Sarason & B. Sarason (Eds.), Social support: Theory, research, and applications (pp. 73–94). The Hague, Netherlands: Martinus Nijhoff.
Coleman, C. L. (2004). The contribution of religious and existential well-being to depression among African American heterosexuals with HIV infection. Issues in Mental Health Nursing, 25, 103–110.
Corless, I. B. (2002). The HIV-AIDS patient: Holier than thou. In R. B. Gilbert (Ed.), Health care and spirituality: Listening, assessing, caring (pp. 189–200). Amityville: Baywood Publishing Company, Inc.
Cotton, S., Puchalski, C. M., Sherman, S. N., Mrus, J. M., Peterman, A. H., Feinberg, J., et al. (2006). Spirituality and religion in patients with HIV/AIDS. Journal of General Internal Medicine, 21, S5–S13.
Cotton, S., Tsevat, J., Szaflarski, M., Kudel, I., Sherman, S. N., Feinberg, J., et al. (2006). Changes in religiousness and spirituality attributed to HIV/AIDS: Are there sex and race differences? Journal of General Internal Medicine, 21(Supplement 5), S14–S20.
Fitchett, G., Murphy, P. E., Kim, J., Gibbons, J. L., Cameron, J. R., & Davis, J. A. (2004). Religious struggle: Prevalence, correlates, and mental health risks in diabetic, congestive heart failure, and oncology patients. International Journal of Psychiatry in Medicine, 34, 179–196.
Fitchett, G., Rybarczyk, B. D., DeMarco, G. A., & Nicholas, J. J. (1999). The role of religion in medical rehabilitation outcomes: A longitudinal study. Rehabilitation Psychology, 44, 333–353.
Flannelly, L. T., & Inouye, J. (2001). Relationships of religion, health status, and socioeconomic status to the quality of life of individuals who are HIV positive. Issues in Mental Health Nursing, 22, 253–272.
Frame, M. W., Uphold, C. R., Shehan, C. L., & Reid, K. J. (2005). Effects of spirituality on health-related quality of life in men with HIV/AIDS: Implications for counseling. Counseling and Values, 50, 5–19.
Guillory, J. A., Sowell, R., Moneyham, L., & Seals, B. (1997). An exploration of the meaning and use of spirituality among women with HIV/AIDS. Alternative Therapies in Health and Medicine, 3, 55–60.
Hall, B. A. (1998). Patterns of spirituality in persons with advanced HIV disease. Research in Nursing and Health, 21, 143–153.
Harrison, M. O., Koenig, H. G., Hays, J. C., Eme-Akwari, A. G., & Pargament, K. I. (2001). The epidemiology of religious coping: A review of recent literature. International Review of Psychiatry, 13, 86–93.
Holmes, W. C., & Shea, J. A. (1998). A new HIV/AIDS-targeted quality of life (HAT-QoL) instrument: Development, reliability, and validity. Medical Care, 36, 138–154.
Holt, J. L., Houg, B. L., & Romano, J. L. (1999). Spiritual wellness for clients HIV/AIDS: Review of counseling issues. Journal of Counseling and Development, 77, 160–170.
Ironson, G., Stuezle, R., & Fletcher, M. A. (2006). An increase in religiousness/spirituality occurs after HIV diagnosis and predicts slower disease progression over 4 years in people with HIV. Journal of General Internal Medicine, 21, S62–S68.
Ironson, G., Stuezle, R., Fletcher, M. A., & Ironson, D. (2006). View of god is associated with disease progression in HIV [abstract]. Annuls of Behavioral Medicine, 31(Suppl), S074.
Jacobson, C. J. Jr., Luckhaupt, S. E., Delaney, S., & Tsevat, J. (2006). Religio-biography, coping, and meaning-making among persons with HIV/AIDS. Journal for the Scientific Study of Religion, 45, 39–56.
Jenkins, R. A. (1995). Religion and HIV: Implications for research and intervention. Journal of Social Issues, 51, 131–144.
Jones, J. W. (1991). Contemporary psychoanalysis and religion: Transference and transcendence. New Haven: Yale University Press.
Justice, A. C., Holmes, W., Gifford, A. L., Rabeneck, L., Zackin, R., Sinclair, G., et al. (2001). Development and validation of a self-completed HIV symptom index. Journal of Clinical Epidemiology, 54(supplement), S77–S90.
Koenig, H., Parkerson, G. R., & Meador, K. G. (1997). Religion index for psychiatric research. American Journal of Psychiatry, 154, 885–886.
Margolin, A., Beitel, M., Schuman-Olivier, Z., & Avants, S. K. (2006). A controlled study of a spiritually-focused intervention for increasing motivation for HIV prevention among drug users. AIDS Education and Prevention, 18, 311–322.
Meisenhelder, J. B., & Marcum, J. P. (2004). Responses of clergy to 9/11: Posttraumatic stress, coping, and religious outcomes. Journal for the Scientific Study of Religion, 43, 547–554.
Menz, R. L. (1987). Aiding those with AIDS: A mission for the church. Journal of Psychology and Christianity, 6, 5–18.
Pargament, K. I. (1997). The psychology of religion and coping: Theory, research, practice. New York: The Guilford Press.
Pargament, K. I., Koenig, H. G., & Perez, L. M. (2000). The many methods of religious coping: Development and initial validation of the RCOPE. Journal of Clinical Psychology, 56, 519–543.
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2004). Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A longitudinal study. Journal of Health Psychology, 9, 713–730.
Pargament, K. I., McCarthy, S., Shah, P., Ano, G., Tarakeshwar, N., Wachholtz, A., et al. (2004). Religion and HIV: A review of the literature and clinical implications. Southern Medical Journal, 97, 1201–1209.
Pargament, K. I., Murray-Swank, N., Magyar, G. M., & Ano, G. (2005). Spiritual struggle: A phenomenon of interest to psychology and religion. In W. R. Miller & H. D. Delaney (Eds.), Judeo-Christian perspectives on psychology: Human nature, motivation, and change (pp. 245–268). Washington: American Psychological Association.
Pargament, K. I., Smith, B. W., Koenig, H. G., & Perez, L. (1998). Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion, 37, 710–724.
Parsons, S. K., Cruise, P. L., Davenport, W. M., & Jones, V. (2006). Religious beliefs, practices and treatment adherence among individuals with HIV in the sourthern United States. AIDS Patient Care and STDs, 20, 97–111.
Prest, L. A., & Robinson, W. D. (2006). Systemic assessment and treatment of depression and anxiety in families. Journal of Systemic Therapies, 25, 4–24.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401.
Ramer, L., Johnson, D., Chan, L., & Barrett, M. T. (2006). The effect of HIV/AIDS disease progression on spirituality and self-transcendence in a multicultural population. Journal of Transcultural Nursing, 17, 280–289.
Rizzuto, A. M. (1979). The birth of the living God: A psychoanalytic study. Chicago: University of Chicago Press.
Robinson, J., & Shaver, P. R. (1969). Measuring Social Psychological Attitudes. Ann Arbor: Institute for Social Research.
Simoni, J. M., Martone, M. G., & Kerwin, J. F. (2002). Spirituality and psychological adaptation among women with HIV/AIDS: Implications for counseling. Journal of Counseling Psychology, 49, 139–147.
Simoni, J. M., & Ortiz, M. Z. (2003). Mediational models of spirituality and depressive symptomatology among HIV-positive Puerto Rican women. Cultural Diversity and Ethnic Minority Psychology, 9, 3–15.
Somlai, A. M., Heckman, T. G. (2000). Correlates of spirituality and well-being in a community sample of people living with HIV disease. Mental Health, Religion, and Culture, 3, 57–70.
Sowell, R., Moneyham, L., Hennessy, M., Guillory, J., Demi, A., & Seals, B. (2000). Spiritual activities as a resistance resource for women with human immunodeficiency virus. Nursing Research, 49, 73–82.
Szaflarski, M., Ritchey, P. N., Leonard, A. C., Mrus, J. M., Peterman, A. H., Ellison, C. G., et al. (2006). Modeling the effects of spirituality/religion on patients’ perceptions of living with HIV/AIDS. Journal of General Internal Medicine, 21, S28–S38.
Tarakeshwar, N., Khan, N., & Sikkema, K. J. (2006). A relationship-based framework of spirituality for individuals with HIV. AIDS and Behavior, 10, 59–70.
Tarakeshwar, N., & Pargament, K. I. (2001). Religious coping in families of children with autism. Focus on Autism and Other Developmental Disabilities, 16, 247–260.
Tarakeshwar, N., Pearce, M. J., & Sikkema, K. J. (2005). Development and implementation of a spiritual coping group intervention for adults living with HIV/AIDS: A pilot study. Mental Health, Religion, and Culture, 8, 179–190.
Woods, T. E., Antoni, M. H., Ironson, G. H., & Kling, D. W. (1999). Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. Journal of Psychosomatic Research, 46, 165–176.
Woodward, E. K., & Sowell, R. (2001). God in control: Women's perspectives on managing HIV infection. Clinical Nursing Research, 10, 233–250.
Wright, L. M., Watson, W. L., & Bell, J. M. (1996). Breaking the patterns of depression. New York: Doubleday.
Yarhouse, M. A., & Anderson, G. (2002). Persons with HIV/AIDS. Journal of Psychology and Christianity, 21, 333-340.
Yi, M. S., Mrus, J. M., Wade, T. J., Ho, M. L., Hornung, R. W., Cotton, S., et al. (2006). Religion, spirituality, and depressive symptoms in patients with HIV/AIDS. Journal of General Internal Medicine, 21, S21–S27.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first author was previously published as Kelly M. McConnell.
Rights and permissions
About this article
Cite this article
Trevino, K.M., Pargament, K.I., Cotton, S. et al. Religious Coping and Physiological, Psychological, Social, and Spiritual Outcomes in Patients with HIV/AIDS: Cross-sectional and Longitudinal Findings. AIDS Behav 14, 379–389 (2010). https://doi.org/10.1007/s10461-007-9332-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-007-9332-6