Abstract
In South Africa, the rising AIDS related mortality has increased the publicity of the HIV/AIDS epidemic and may have an impact on behavior change. We examined the association between knowing someone who has died of AIDS and self-reported behavior change, condom use at last intercourse, number of partners in the prior 12 months, and attitudes towards HIV, among South African youth aged 15–24. We found that over 40% of youth reported knowing someone who died of AIDS, most commonly a neighbor. Using multivariable logistic regression, we found that high school-educated youth who knew someone who died of AIDS were significantly more likely to report having changed their behavior as a result of HIV (OR 2.01, 95% CI: 1.32;3.06). We found no association between knowing someone who died of AIDS and other HIV prevention-related behaviors. While youth tended to have increased odds of perceiving HIV to be serious, they did not consistently perceive their risk of contracting HIV to be higher when they knew someone who died of AIDS. Our results suggest that part of the key to impacting behavior change in youth may lie in better understanding what factors increase youth’s perceived risk of contracting HIV which will help us better target our interventions. If youth are impacted by personal knowledge of an AIDS death, to the point that they change their behaviors, we must continue to encourage discourse about HIV/AIDS with the hope that persons dying from AIDS will feel more comfortable disclosing their diagnosis to youth they know and others.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Sub-Saharan African countries continue to experience some of the highest prevalences of HIV/AIDS world-wide (UNAIDS 2006; USAID 2006). South Africa is among the countries hardest hit by the epidemic (UNAIDS 2006; USAID 2006). As of 2005, the national prevalence of HIV in adults, aged 15–49, was estimated to be 16.2% according to the South African National HIV Survey (Mandela Foundation/HSRC 2005). This disease burden is not evenly distributed across gender and age groups (Mandela Foundation/HSRC 2005). In fact, the 2005 HIV prevalence in youth aged 15–24, was estimated to be 4.4% in males and 16.9% in females (Mandela Foundation/HSRC 2005). Sadly, in South Africa, it has become almost common to know someone who has HIV or who has died of AIDS. In a study of South African youth, aged 15–24, more than 40% of girls and boys reported knowing someone who died of AIDS (Pettifor et al. 2005).
As there is currently no vaccination available to prevent HIV, modifying sexual behavior is integral to preventing HIV acquisition among youth (Bloom et al. 2000; Fylkesnes et al. 2001; Kamali et al. 2000). Many have examined and tried to understand the factors that may drive behavior change. One topic that has become increasingly more relevant in many African societies is the effect of AIDS deaths on the community and its individuals (Stoneburner and Low-Beer 2004). Some have explored the specific relationship between knowing someone with HIV/AIDS or who has died of AIDS and changes in sexual behavior. Specifically, some studies have shown a positive association between knowing someone with HIV/AIDS or who has died of AIDS and protective sexual behavior such as condom use, delayed sexual debut, and decreased number of sexual partners (Gregson et al. 1997; Ijumba et al. 2004; Macintyre et al. 2001). In one study in South Africa, however, there was no association found between knowing someone with HIV or who died of AIDS and condom use at last sexual encounter (Camlin and Chimbwete 2003). The authors note that at the time of the study, the South African AIDS epidemic was still in its early stages thus there may not have yet been a dramatic impact of the epidemic on society. Also, the study did not query the relationship of the interviewee to the person they knew with HIV/AIDS. It is possible that the person with HIV/AIDS was a distant acquaintance and therefore less likely to influence the interviewee’s behavior (Camlin and Chimbwete 2003). Finally, knowing someone living with HIV who appears healthy versus knowing someone who has died of AIDS may differentially impact behavior change and should be analyzed as separate outcomes.
Application of the Availability Heuristic may prove useful in trying to understand how exposure to an AIDS death may influence behavior. According to this theory, the more easily an experience can be brought to mind, the more likely it is that this experience will be used to make a judgment about the probability of an event and to guide personal choices (Tversky and Kahneman 1982). For example, the death of a personal acquaintance, friend, or family member due to AIDS will prime a person to more readily recall the consequences of AIDS (i.e., death) making it more likely that this experience will influence their perceived risk of HIV acquisition.
To our knowledge, there is no study to date in South African youth that has examined the association between knowing someone who has died of AIDS and sexual risk taking behavior. Given that adolescents are acquiring HIV at a young age in South Africa, it is important to examine the factors that may influence their thoughts and behaviors. This knowledge could then be used to tailor prevention messages that would have a measurable impact on diminishing HIV transmission among youth. In this study, we examined the association between knowing someone who has died of AIDS and self-reported behavior change, condom use at last intercourse, number of partners in the prior 12 months, and attitudes towards HIV, among South African youth aged 15–24, using the 2003 Reproductive Health and HIV Research Unit National Youth Survey. We hypothesized that knowing someone who died of AIDS, would be associated with increased condom use, decreased number of partners, and increased perceived risk of contracting HIV.
Methods
Participants
The 2003 Reproductive Health and HIV Research Unit (RHRU) National Youth Survey used a three stage, disproportionate, stratified sampling design to identify a nationally representative sample of young people aged 15–24, living in the nine provinces of South Africa. The 2001 national census was used as the sampling frame and census enumeration areas (EA) were the primary sampling units. Households within sampled EAs were enumerated and one eligible young person in each household was randomly selected to take part in the study.
Interview Procedures
Participants had to be willing to provide an oral specimen to test for HIV antibodies, as well as complete a private comprehensive structured face to face interview. Informed consent was obtained from all participants, including parental consent for youth aged 15–17. Interviewers aged 18–35 completed a 1-week training session and were matched to interviewees based on gender, language, and race. The interview included questions about demographics, sexual behavior, and knowledge of HIV prevention programs. The survey was translated from English into eight official South African languages: Sotho, Zulu, Tswana, Xhosa, Pedi, Venda, Tsonga, and Afrikaans, and then the responses back-translated into English. In total, 11, 904 interviews were conducted, representing an overall response rate of 68.2% (Pettifor et al. 2005).
Laboratory Methods
Oral fluid samples were collected using the Orasure HIV-1 Specimen Collection Device (Orasure Technologies, Inc.) and tested for HIV 1/2 antibodies. The study participants were advised that their HIV results would not be returned to them and were referred to the nearest HIV testing center for counseling and testing services.
Variables
Main Exposure
The binary main exposure of interest was whether the youth personally knew someone who had died of AIDS.
Outcome
There were five primary outcomes of interest. First was condom use at last intercourse (yes/no). Second, was number of sexual partners in the past 12 months, which after analysis of the distribution of the data, was dichotomized as “one partner or more than one partner.” Third was reported behavior change due to HIV (yes/no). Lastly, the adolescent’s perceived risk of contracting HIV (none–low/moderate–high) and the adolescent’s perceived seriousness of HIV (not serious/serious) were also examined.
Covariates
After literature review and consideration of the research question, a Directed Acyclic Graph (DAG) was drawn to identify covariates of interest and potential confounders (Greenland et al. 1999). Gender, HIV status, talking to a parent/guardian about HIV, talking to someone other than a parent/guardian about HIV, and participation in a loveLife program (National South African HIV prevention campaign that targets youth Pettifor et al. 2007), were all coded dichotomously. Presence or absence of electricity in the home was used as a proxy measure for socio-economic status. Race, after data exploration, was dichotomized to black versus not black. Education was coded to capture youth who had completed high school or were in school (for those 18 and under) versus those who had not completed high school or were not in school (for those 18 and under). Age, after data exploration was dichotomized to 15–19 and 20–24. Religion, after data exploration, was dichotomized as Christian or non-Christian. Province was maintained with its original coding as a nine level categorical covariate.
Statistical Analyses
The final sample was weighted to account for the differential sampling probabilities and to represent 2001 South African national census distribution of young people (aged 15–24). Analyses were conducted using Stata 9.0, allowing for sample strata, primary sampling units, and population weights.
Each of the 11 covariates was first assessed for effect measure modification, by testing an interaction term between the covariate and the main exposure; if the P value for the interaction term was less than 0.10 the covariate was retained as an effect measure modifier. Then, the remaining covariates were assessed for confounding by examining the association between the covariate and each outcome amongst those unexposed to the main exposure and the association between each covariate and the main exposure (Rothman and Greenland 1998). Covariates were retained as potential confounders if they were strongly associated (OR ≤ 0.5 or OR ≥ 2.0) with the exposure and outcome and if they were confounders based on the DAG or if they were a priori of substantive interest.
Multivariable logistic regression was used to examine the relationship between the main exposure and each of the outcomes, including the covariates found to be confounders and effect measure modifiers based on the procedures described above. Logistic regression was used to estimate odds ratios due to the cross sectional nature of the data. A process of manual backwards elimination was used to assess for counfounding amongst the non-effect measure modifiers. A change in point estimate of greater than 10% was considered evidence of confounding, using the natural log confounding OR (Kleinbaum et al. 1988; Selvin 2004; Sonis 1998). If an effect measure modifier was present, confounding was assessed within each stratum and if the change in the natural log OR was greater than 10% in any one of the strata, the covariate was retained as a confounder. Covariates that were assessed for all models included: age, gender, race, socio-economic status, exposure to loveLife programs, religion, education level, HIV status, talking to a parent/guardian about HIV, talking to someone other than a parent/guardian about HIV, and province of residence. Age and gender were retained in all models either as an effect measure modifier or a confounder, based on their a priori importance.
The analysis of the outcomes: condom use at last intercourse and number of partners in the past 12 months, were restricted to the subset of the population that was sexually active. To account for this subpopulation analysis, the subpopulation commands in Stata were used for multivariable logistic regression modeling.
Results
Descriptive Analyses
Table 1 shows the univariate distributions of the main exposure, each outcome, and the covariates stratified by gender. Forty percent of males and fifty percent of females reported personally knowing someone who had died of AIDS. The most commonly reported relationship to the person who had died of AIDS was a neighbor (45.5%) followed by a non-first degree relative (25.2%) (Table 2). Few youth reported that the person they knew who had died of AIDS was a first degree relative or a sexual partner. Sixty-seven percent of males and sixty-eight percent of females reported having had sex. Forty-eight percent of sexually active females and fifty-seven percent of sexually active males reported using a condom at last sex. More than one sexual partner in the prior 12 months was reported by 44% of sexually active males and 12% of sexually active females. More than 60% of all youth reported behavior change due to HIV. Twenty-two percent of males and thirty-one percent of females reported their risk of contracting HIV to be moderate to high. Greater than 90% of all youth reported HIV to be serious.
Bivariate Analyses
Table 3 shows the bivariate associations between potential confounders and each of the five outcomes, as well as the crude OR between the main exposure and each outcome. Sexually active youth who knew someone who died of AIDS had 1.35 times the odds of using a condom at last intercourse as those who did not (95% CI: 0.95; 1.91); and 1.22 times the odds of having more than one partner as those who did not (95% CI: 1.02; 1.47). For all youth, those who knew someone who died of AIDS had 2.12 times the odds of reporting behavior change due to HIV as those who did not (95% CI: 1.40; 3.20). For all youth, those who knew someone who died of AIDS had 1.23 times the odds of perceiving risk of contracting HIV to be moderate to high as those who did not (95% CI: 1.04; 1.44); and 3.06 times the odds of perceiving HIV to be serious as those who did not (95% CI: 1.90; 4.95).
Multivariate Analyses
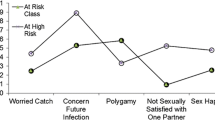
The results of the multivariate analyses are reported in Table 4. The association between knowing someone who died of AIDS and condom use at last intercourse was stratified by race, which was an effect measure modifier. The odds of condom use at last intercourse were slightly increased for black youth, who knew someone who died of AIDS (OR = 1.35, 95% CI: 0.97; 1.91), but there was no association seen in non blacks (OR = 0.75, 95% CI: 0.49; 1.13).
The association between knowing someone who died of AIDS and number of partners in the past 12 months was stratified by education attained, which was an effect measure modifier. The odds of more than one partner in the prior 12 months were increased and significant for non-educated youth, who knew someone who died of AIDS (OR = 2.00, 95% CI: 1.47; 2.73), as compared to those who did not; but there was no association seen in those with more education (OR = 1.12, 95% CI: 0.89; 1.40).
The association between knowing someone who died of AIDS and self-reported behavior change due to HIV was stratified by education, an effect measure modifier. Amongst the non-educated youth, who knew someone who died of AIDS, there was an increased odds of reporting behavior change due to HIV (OR = 1.47, 95% CI: 0.84; 2.58), as compared to those who did not; and this association was stronger and significant amongst the educated youth (OR = 2.01, 95% CI: 1.32; 3.06).
The association between knowing someone who died of AIDS and reporting that HIV is serious was stratified by education and participation in a loveLife program, which were effect measure modifiers. The odds of reporting that HIV was serious were the greatest amongst youth with low educational attainment but who had participated in a loveLife program (OR = 9.31, 95% CI: 3.40; 25.46) and the association less strong amongst those who were educated and participated in loveLife (OR = 3.13, 95% CI: 1.51; 6.50).
The association between knowing someone who died of AIDS and self reported risk of contracting HIV was stratified by HIV status and race, which were effect measure modifiers. For non-black, HIV negative youth, knowing someone who died of AIDS significantly increased the odds of perceiving risk of HIV to be high (OR = 1.61, 95% CI: 1.13; 2.28), as compared to those who did not; but for the other strata, there was no strong association seen.
Discussion
There are several key findings from this study. First, over 40% of all youth personally knew someone who had died of AIDS. Most commonly, this person was reported to be the youth’s neighbor; less commonly this was the youth’s relative; and least commonly this person was an immediate family member, friend, or sexual partner. It is not surprising that youth did not report many friends dying of AIDS, because in South Africa, AIDS related deaths are highest among adults age 25 and older, who are not likely to be within the peer group of those sampled in the study (Hosegood et al. 2004; UNAIDS 2006). Also, given the stigma that still surrounds HIV/AIDS, youth may be reluctant to disclose information about close family members that have HIV/AIDS.
Second, we found that youth who reported knowing someone who died of AIDS had an increased odds of reporting that they changed their behavior due to HIV. This association was stronger for educated youth and weaker for less educated youth but was in the same direction irrespective of educational attainment. This is an important finding as this indicates that the AIDS deaths may be catalyzing changes in youth behavior. In addition, our results confirm the importance of secondary education for youth. From a public health standpoint, these findings indicate that we should encourage persons living with AIDS to share their stories with youth that they know, given that this exposure may motivate the youth to change his/her behavior.
In addition to measuring reported changes in overall behavior as a result of HIV, we measured specific behaviors that are known to reduce HIV risk as well. We found a slightly increased odds of condom use at last intercourse in black youth who knew someone who died of AIDS. This finding has important prevention implications as well. As stated previously, if youth are impacted by personal knowledge of an AIDS death, to the point that they change their actual behaviors, we must continue to encourage discourse about HIV/AIDS with the hope that persons dying from AIDS will feel more comfortable disclosing their diagnosis to youth they know and others.
Despite these findings, we found no association between personally knowing someone who died of AIDS and several other behaviors. These behaviors included condom use at last intercourse in non-black youth and decreased number of sexual partners in educated youth. It is not entirely clear why knowing someone who died of AIDS affects certain behaviors in some groups but not in others. A likely explanation is that although youth have changed their behavior in some ways, it was not enough to be protective based on our measures of condom use at last intercourse and number of partners. Also, we must consider the relationship of the youth to the person they knew who died of AIDS. It is possible that this contact was not someone the youth felt emotionally close to or identified with, so the death did not catalyze significant behavior change. From the Availability Heuristic, we would predict that recall of an event and the similarity between the event and the situation under consideration would influence the choice that the adolescent would make (Tversky and Kahneman 1982). So, although we asked youth about personal knowledge of a contact who died of AIDS, an older neighbor, for example, may not impact the youth’s behavior pattern the same way that an age matched peer would (Camlin and Chimbwete 2003). Finally, to some extent, these measures depend on consistent behavior change and so are likely influenced by self-efficacy for condom use and sexual autonomy. Youth, in each sexual encounter must have autonomy to make decisions about sexual activity as well as self-efficacy for condom use, in order to engage in protective behaviors (Bryan et al. 2006; Camlin and Chimbwete 2003; Harrison et al. 2006; Pettifor et al. 2004; Sayles et al. 2006). Also, it is important to note that youth, especially women, may acknowledge their risk and desire safer behavior, but may not have the power to change their behavior, due to societal structure and relationship norms.
Next, we found that the odds of having more that one partner were increased for non-educated youth who knew someone who had died of AIDS. This finding is surprising, in the face of our hypothesized direction of change, and warrants further discussion. First, it is possible that un-educated youth who knew someone who died of AIDS are inherently at greater risk of contracting HIV based on their peer group HIV prevalence and norms for risky sexual behavior. This inherent higher risk is what led the youth both to know someone who died of AIDS and to engage in higher risk sexual behavior. In fact, this high-risk peer group participation may represent an unmeasured confounder. Also, given the cross sectional nature of the data, it is impossible to establish the temporal relationship between the exposure and the outcome and to detect changes over time. For example, if an adolescent, who is part of a high-risk peer group, engaged in high risk behavior and subsequently knew a contact to die of AIDS, he/she may thereafter change his/her behavior. However, with cross sectional data, this temporality and change over time will not be captured. We tried to limit this problem by using data regarding recent behaviors, but could not eliminate this issue.
Finally, we found that almost all youth who knew someone who died of AIDS had an increased odds of reporting that HIV is serious. This, however, was not the case for the perceived risk of contracting HIV. In fact, for most youth, there was no association between knowing someone who died of AIDS and perceived risk of contracting HIV. This is opposite of what we would expect, and according to the Availability Heuristic, an experience, such as knowing someone who died of AIDS, should increase the belief that this event could happen to that person. In the absence of increased risk perception, despite increased severity perception, the likelihood of behavior change may be less. In fact others have examined this relationship between behavior change and perceived risk, and found that behavior change results from a series of complex thoughts, of which one of the most important is often the individual’s perceived risk of contracting HIV (Bryan et al. 2006; Dononvan and Ross 2000; Helleringer and Kohler 2005; Macintyre et al. 2004; Smith and Watkins 2005). In thinking about HIV risk perception, there are many factors that can lead to personal decreased risk perception such as the “othering” phenomenon, whereby individuals perceive others to be inherently at higher risk than themselves, due to a variety of often pre-conceived notions (Bryan et al. 2006; Petros et al. 2006). This is often coupled with a personal notion of invincibility, which is frequently the case with adolescents (Macintyre et al. 2004). Next, it is perhaps difficult for an adolescent to comprehend risk today for an infection that may cause symptoms 5–10 years after acquisition (Macintyre et al. 2004). Also, admitting vulnerability or risk of contracting HIV means that an individual is endorsing the idea that he/she fits into the categories or engages in behaviors that may be stigmatized within the community (Macintyre et al. 2004; Petros et al. 2006). Finally, even in settings where the risk of HIV is high, as in South Africa, and when there is personal knowledge of someone who died of AIDS, individuals may deny their risk as a way of distancing themselves from the very real threat of infection (Macintyre et al. 2004; Petros et al. 2006; Varga 2001). These findings regarding adolescent perceived risk of contracting HIV present the most opportunity for further research.
There are several limitations to this study. As discussed above, the study’s cross sectional nature which, although an excellent means to examine the attitudes and behaviors at one point in time of many individuals, limits the ability to interpret the temporal relationship between the exposure and outcome and changes over time. Also, issues about sexual behavior are sensitive in most societies, and certainly so in South Africa. This presents concerns of social desirability bias in the responses. Although we tried to minimize this by using young interviewers (age 18–35) and gender, language, and race matching the interviewers and interviewees, this is still likely of some concern. However, with a study survey response rate of 68.2%, the probability of error due to non-response bias is likely low.
In conclusion, although it is unfortunate that AIDS deaths continue to increase in South Africa, our findings represent, perhaps, an unintended positive consequence. We found that subgroups of youth who knew someone who died of AIDS had a significantly increased odds of reporting that HIV is serious and significantly increased odds of stating that they had changed their behavior because of HIV, as compared to those who did not know someone who died of AIDS. Interestingly, we also found that despite these reported changes in behavior and perceived seriousness of HIV, most youth who knew someone who died of AIDS did not have an increased perceived risk of personally contracting HIV. It is possible that as deaths from AIDS continue in South Africa, more youth will lose those close to them, risk perception will increase, and/or there will be greater changes in behavior. Certainly, future studies should be done to better elucidate the thought processes and behavior patterns in youth and should more closely examine the determinants of perceived susceptibility to HIV among youth. We believe that the answer to these questions may hold a part of the solution to promoting behavior change among South African youth.
References
Bloom, S., Banda, C., Songolo, G., Mulendema, S., Cunningham, A., & Boerma, T. (2000). Looking for change in response to the AIDS epidemic: Trends in AIDS knowledge and sexual behavior in Zambia, 1990–1998. Journal of Acquired Immune Deficiency Syndromes, 25, 77–85.
Bryan, A., Kagee, A., & Broaddus, M. R. (2006). Condom use among South African adolescents: Developing and testing theoretical models of intentions and behavior. AIDS and Behavior, 10(4), 387–397.
Camlin, C., & Chimbwete, C. (2003). Does knowing someone with AIDS affect condom use? An analysis from South Africa. AIDS Education and Prevention, 15(3), 231–244.
Dononvan, B., & Ross, M. W. (2000). Preventing HIV: Determinants of sexual behavior. The Lancet, 255, 1897–1901.
Fylkesnes, K., Musonda, R., Sichone, M., Tembo, F., & Monze, M. (2001). Declining HIV prevalence and risk behaviors in Zambi: Evidence from surveillance and population based surveys. AIDS, 15, 907–916.
Greenland, S., Pearl, J., & Robins, J. M. (1999). Causal diagrams for epidemiological research. Epidemiology, 10(1), 37–48.
Gregson, S., Zhuwaiui, T., Anderson, R. M., & Chandiwana, S. K. (1997). Is there evidence for behavior change in response to AIDS in rural Zimbabwe? Social Science and Medicine, 46(3), 321–330.
Harrison, A., O’Sullivan, L. F., Hoffman, S., Dolezal, C., & Morrell, R. (2006). Gender role and relationship norms among young adults in South Africa: Measuring the context of masculinity and HIV risk. Journal of Urban Health, 83(4), 709–722.
Helleringer, S., & Kohler, H. P. (2005). Social networks, perceptions of risk, and changing attitudes towards HIV/AIDS: New evidence from a longitudinal study using fixed effects. Population Studies, 99(3), 265–282.
Hosegood, V., Vanneste, A. M., & Tiameus, I. M. (2004). Levels and causes of adult mortality in rural South Africa: The impact of AIDS. AIDS, 18, 663–671.
Human Sciences Research Counsel and Nelson Mandela Foundation. South African National HIV Prevalence, HIV Incidence, Behavior, and Communication Survey, 2005. Fact Sheet 2.
Ijumba, K., Gamieldien, R., Myer, L., & Morroni, C. (2004). Sexual risk behaviors are influenced by knowing someone with HIV/AIDS. South African Medical Journal, 94(7), 522–523.
Kamali, A., Carpenter, L., Whitworth, J., Pool, R., Ruberatwari, A., & Ojwiya, A. (2000). Seven-year trends in HIV-1 infection rates and changes in sexual behavior, among adults in rural Uganda. AIDS, 14, 427–434.
Kleinbaum, D. G., Kupper, L. L., & Muller, K. E. (1988). Applied regression analysis and other multivariable methods (2nd ed.). Boston: PWS-Kent Publishing Company.
Macintyre, K., Brown, L., & Sosler, S. (2001). It’s not what you know, but who you knew: Examining the relationship between behavior change and AIDS related mortality in Africa. AIDS Education and Prevention, 13(2), 160–174.
Macintyre, K., Rutenberg, N., Brown, L., & Karim, A. (2004). Understanding perceptions of HIV risk among adolescents in KwaZulu-Natal. AIDS and Behavior, 8(3), 237–250.
Petros, G., Airhihenbuwa, C. O., Simbayi, L., Ramlagan, S., & Brown, B. (2006). HIV/AIDS and othering in South Africa: The blame goes on. Culture, Health and Sexuality, 8(1), 67–77.
Pettifor, A. E., Macphail, C., Bertozzi, S., & Rees, H. (2007). The challenge of evaluating a national HIV prevention program: The case of loveLife, South Africa. Sexually Transmitted Infection, online, doi: 10.1136/sti.2006.023689.
Pettifor, A. E., Measham, D. K., Rees, H. V., & Padian, N. S. (2004). Sexual power and HIV risk, South Africa. Emerging Infectious Diseases, 10(11), 1996–2004.
Pettifor, A. E., Rees, H. V., Kleinschmidt, I., Steffenson, A. E., MacPhail, C., Hlongwa-Madikizela, L., Vermaak, K., & Padian, N. S. (2005). Young people’s sexual health in South Africa: HIV prevalence and sexual behavior from a nationally representative household survey. AIDS, 19, 1525–1534.
Rothman, K. J., & Greenland, S. (1998). Introduction to stratified analyses. In K. J. Rothman & S. Greenland (Eds.), Modern epidemiology (2nd ed., pp. 253–280). Philadelphia: Lippincott Williams and Wilkins.
Sayles, J. N., Pettifor, A., Wong, M. D., MacPhail, C., Lee, S. J., Hendriksen, E., Rees, H. V., & Coates, T. (2006). Factors associated with self-efficacy for condom use and sexual negotiation among South African youth. Epidemiology and Social Science, 43(2), 226–233.
Selvin, S. (2004). Statistical analysis (3rd ed.) New York: Oxford University Press.
Smith, K. P., & Watkins, S. C. (2005). Perceptions of risk and strategies for prevention: Responses to HIV/AIDS in rural Malawi. Social Science and Medicine, 60, 649–660.
Sonis, J. (1998). A closer look at confounding. Family Medicine, 30(8), 584–588.
Stoneburner, R., & Low-Beer, D. (2004). Population-level HIV declines and behavioral risk avoidance in Uganda. Science, 304, 714–718.
Tversky, A., & Kahneman, D. (1982). Availability: A heuristic for judging frequency and probability. In D. Kahnehman, P. Slovic, & A. Tversky (Eds.), Judgment under uncertainty: Heuristics and biases (pp. 163–179). Cambridge: Cambridge University Press.
UNAIDS (December 2006). AIDS Epidemic Update, 1–96.
USAID (2006). Health Profile: Africa, 1–4.
Varga, C. A. (2001). Coping with HIV/AIDS in Durban’s commercial sex industry. AIDS Care, 13(3), 351–365.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palekar, R., Pettifor, A., Behets, F. et al. Association Between Knowing Someone Who Died of AIDS and Behavior Change Among South African Youth. AIDS Behav 12, 903–912 (2008). https://doi.org/10.1007/s10461-007-9325-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-007-9325-5