Abstract
Despite the recognized need for culturally tailored HIV prevention interventions for gay, bisexual, and questioning youth, few studies have examined if predictors of unprotected sex vary for youth from different ethnic groups. This study reports on a sample of 189 gay, bisexual, and questioning youth (age 15–22) from three racial/ethnic backgrounds (African American, Hispanic, and White) recruited in Chicago, IL and Miami-Dade and Broward Counties, Florida. For African American youth, being in a long-term relationship, having been kicked out of the home for having sex with men, and younger age at initiation of sexual behavior were associated with unprotected sex. For Hispanic youth, higher ethnic identification and older age at initiation of sexual behavior were associated with unprotected sex. For White youth, no predictors were associated with unprotected sex. Our findings point to the importance of understanding the varying predictors of unprotected sex and integrating them into tailored prevention interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Young men who have sex with men (YMSM) continue to be at high risk of acquiring HIV through unprotected sexual encounters as indicated by the increasing incidence of HIV infection among YMSM reported in recent years (Hall et al. 2007; Wolitski et al. 2001). For instance, from 1999 to 2004 in states with HIV name reporting the number of new HIV infections among MSM aged 13–24 increased 48% (Rangel et al. 2006). YMSM who are also African American or Hispanic are at elevated risk for HIV infection above their non-minority peers (Hall et al. 2007; Harawa et al. 2004; Rhodes et al. 2006). Results from the Young Men’s Survey (a multisite HIV prevalence study) revealed that while White YMSM ages 15–22 had an overall HIV prevalence of 3.3%, African American and Hispanic YMSM had much higher rates, with 6.9% of Hispanics and 14.1% of African Americans testing positive for HIV (Valleroy et al. 2000).
Because of the increasing HIV incidence among YMSM and the disparities in HIV prevalence among YMSM who are members of ethnic minorities, there is an urgent need for HIV prevention interventions that are designed for adolescent and emerging adult YMSM (National Institute of Mental Health Multisite HIV Prevention Trial Group 2002). Adolescence and emerging adulthood are the developmental periods during which youth develop, shape and modify their personal identity (sexual, cultural, and professional) (Arnett 2000; Erikson 1968). In exploring the different facets of their identities during the life period in which risk behaviors peak (Arnett 1992, 1997, 2000; Bachman et al. 1996; O’Malley et al. 1992, 1995, 1998), youth are more willing to experience a wider range of thoughts and actions than are individuals in other life stages (Arnett 1992, 1997, 2000). For YMSM, these thoughts and actions involve participating in behaviors that are stigmatized and not accepted by the larger society (Harper and Schneider 2003; Ryan and Futterman 1998). As a result, many of these youth experience prejudice and homophobia and feel isolated from family and friends. These experiences have been linked to negative behavioral and health outcomes (e.g., drug use, unprotected sex, multiple sex partners) which put them at increased risk for becoming infected with HIV (Blake et al. 2001; Harper et al. 2004; Rosario et al. 2001; Rotheram-Borus et al. 1995; Waldo et al. 1998).
HIV prevention researchers have argued (Fernández et al. 2005; Marin 2003) that in order for HIV prevention interventions to have the largest potential impact, they must address the cultural values of the intended recipients. Despite the growing problem of HIV infection among African American and Hispanic YMSM and the recognized need for interventions to reduce its spread, few developmentally and culturally appropriate interventions designed to reduce unprotected sex among YMSM in general have been developed and tested (Blake et al. 2001). There are even fewer culturally tailored interventions designed to reach YMSM from racial and ethnic minority groups at increased risk for HIV infection. An essential step in developing effective culturally-tailored interventions is gaining an understanding of the unique cultural influences and pressures faced by African American and Hispanic YMSM and how these impact their HIV related risk behaviors.
As YMSM from racial and ethnic minority backgrounds work to develop an integrated adult identity, they face pressures not only from mainstream culture, but also from their specific culture’s expectations regarding family, sex, and gender (Díaz 1998; Peterson and Carballo-Dieguez 2000; Stokes and Peterson 1998). For example, because traditional Hispanic and African American cultures stigmatize and reject homosexual thoughts, fantasies and behaviors, many young African American and Hispanic MSM experience rejection, discrimination, and/or feel isolated from family or friends in working to define their adult sexual identity (Williams et al. 2004; Zea et al. 2003). Studies have shown that many ethnic minority MSM feel closely connected to their ethnic community, but experience lack of acceptance from their families and social networks (O’Donnell et al. 2002; Tremble et al. 1989). Furthermore, being gay counters cultural expectations regarding the role of men and the cultural importance of procreation in African American and Hispanic families (Jiminez 2003; Stokes and Peterson 1998; Whitehead 1997).
Unfortunately, the mainstream White gay community does not always provide a supportive environment in which ethnic minority MSM can formulate a healthy and integrated gay sexual identity. There is evidence that both adult and young ethnic minority MSM experience racism and sexual objectification from White gay men (Díaz et al. 2004; Harper et al. 2004; Williams et al. 2004). These experiences of discrimination and marginalization from both their ethnic group and the gay community lead to distress in many minority YMSM (Bonilla and Porter 1990; Harper et al. 2004; Washington 2001). Some may turn to sex or drugs as a way to cope (Díaz et al. 2005), which can increase their risk of becoming infected with HIV.
Cultural variations in attitudes towards and practices of condom use have been demonstrated among adult MSM (Harawa et al. 2004; Rhodes et al. 2006). A number of factors have been associated with inconsistent condom use among African American and Hispanic MSM; however, ethnic differences in the predictors of unprotected sex have been reported. Risky sexual practices among African American MSM have been linked to psychological distress, older age, and low socioeconomic status (Myers et al. 2003). For Hispanic MSM, use of club drugs has been linked to having more partners and more unprotected sex (Fernández et al. 2005). In the one study we found specifically examining young ethnic minority YMSM, non-supportive peer norms regarding condom use and not carrying condoms were shown to be associated with unprotected sex (Hart and Peterson 2004). Because YMSM have not yet fully developed their adult identity, it is likely that predictors of unprotected sex for YMSM are different from those identified for their adult counterparts.
Studies investigating condom use among adolescents have predominantly focused on heterosexual youth (Harper et al. 2003). Given that the Young Men’s Study (Valleroy et al. 2000) found that the predictors of HIV infection varied by racial and ethnic group, it is highly likely that predictors of unprotected sex will also vary by race and ethnicity. Specific investigation of the predictors of unprotected sex within ethnic groups is needed so that effective, culturally tailored interventions to reduce HIV risk among YMSM can be developed.
In this paper, we report on a sample of YMSM from three ethnic and racial backgrounds (Hispanic, African American, and Non-Hispanic White (referred to as “White”)) recruited from community venues who participated in a mixed methods study supported by the Adolescent Trials Network (ATN), ATN 020: Identity Development in Gay/Bisexual/ Questioning Male Youth: Implications for HIV Sexual Risk. As a first step to model building, we examined the factors associated with unprotected sex among YMSM within each of the three ethnic groups and report these findings in the current paper. In addition to demographic factors, we hypothesized that cultural (lower ethnic identification, less attachment to the gay community), developmental (younger age, younger age at initiation of sexual behavior), and relationship factors (being in a long-term relationship, having been kicked out of the home) would be associated with unprotected sex for each of the three ethnic groups. We also hypothesized that the strength of the associations would be different for each of the three racial and ethnic groups.
Methods
Participants
The goals of ATN 020 (the parent study) were to explore how development of identities (e.g., gay, ethnic and masculine) impact HIV risk and protective behaviors and to build a conceptual model that could be used to guide development of culturally and developmentally appropriate interventions to reduce risk of HIV infection. From March 2004 to September 2005, 200 participants were recruited from public venues and community agencies in Chicago (n = 97) and Miami-Dade and Broward Counties, Florida (South Florida; n = 103). Eligible youth were: (1) male; (2) 15–22 years of age; (3) self-identified as African American, Hispanic/Latino, or White non-Hispanic/European American ancestry; (4) self-identified as gay, bisexual, or questioning; (5) not known to be HIV positive; (6) lived in the metropolitan areas of Chicago or South Florida; and (7) able to read and understand English. Because the IRB in South Florida did not grant a waiver of parental consent, we did not recruit youth younger than 18 in South Florida to prevent unwarranted disclosure and protect their confidentiality. We excluded Haitian and other Caribbean non-Hispanic Black youth because they represent distinct ethnic groups who have different experiences, culture, and history than African American youth and ethnic identity was a key component of ATN 020, the parent study. In Chicago, 97 of the 124 screened were eligible and fully completed the survey. In South Florida, 103 of the 120 screened were eligible and fully completed the survey. All but one eligible youth enrolled in the study. A total of 71 African Americans (38 South Florida, 33 Chicago), 68 Hispanics (33 South Florida, 35 Chicago), and 61 Whites (32 South Florida, 29 Chicago) participated in the study. Nine youth who had not initiated sexual activity were excluded from the analyses—one African American (1.4%), three Hispanics (4.4%), and five Whites (8.2%). This paper reports on the youth who were sexually active.
Procedures
Trained, multi-ethnic research staff, who themselves were YMSM, recruited participants at community agencies that served YMSM and at public venues frequented by or that catered to these youth. At community agencies, staff made presentations describing the study and youth who were interested approached staff to be screened for study participation. In community venues, staff approached youth directly, described the study, and asked if youth were interested in being screened. In both types of venues, we identified private, safe areas in which to conduct study activities (screening, consent, completion of questionnaire). After providing informed consent or assent, participants completed a pencil-and-paper questionnaire and were compensated $25 for their time and effort. The average time for completion of the questionnaire was 40 min.
Measures
Demographic and other Descriptive Factors
Participants reported their age, place of birth, and their self-reported sexual orientation (gay, bisexual, questioning). They also reported whether or not they: (1) were currently involved in a long-term relationship that has lasted more than a year, (2) had ever received public aid (i.e., food stamps or reduced price school lunches), (3) had ever been kicked out of home because of sexual orientation, and (4) had ever spent the night in a shelter because they were without a place to sleep.
Alcohol and other Drugs
To assess use of alcohol and other drugs, participants indicated if they had ever used alcohol, marijuana, or street drugs (defined as cocaine, crack cocaine, methamphetamine, ecstasy, rohypnol, GHB, and hallucinogens), and the age at which they had first used these substances. In addition, participants reported if they had used these substances in the last 90 days.
Sexual Behaviors
Participants reported their sexual behaviors with men and women separately in two timeframes. For both lifetime and the past 90 days, participants indicated whether or not they had had insertive anal sex with a man, had receptive anal sex with a man, performed oral sex on a man, had vaginal or anal sex with a woman, or had performed oral sex on a woman. Participants also indicated the age at initiation of each type of sex act. For the last 90 days only, participants stated the frequency with which they had used condoms for each type of sex act they reported. They also reported if substances had ever led them to engage in sexual behavior they had not intended to.
Ethnic Identity
The Multi-Ethnic Identity Measure (MEIM) (Phinney 1992) was used to assess ethnic identity. The MEIM is a 24 item scale designed to assess level of identification with the participant’s most salient cultural affiliation. Sample items include “I am happy that I am a member of the group I belong to” and “I have a lot of pride in my ethnic group”. The MEIM has been used in multiple studies with African American, Latino/Hispanic and White youth and has consistently shown good reliability, with alpha coefficient above 0.80 across a wide range of ethnic groups and ages (Roberts et al. 1999).
Gay Community Attachment
We used the identification and involvement with the Gay Community Scale (Vanable et al. 1992) to assess gay community attachment. This scale consists of 8 Likert-scale items, assessing attitudes towards self-identification and association with the gay community (four items), utilization of gay oriented media services and establishments (three items), and number of gay friends. Sample items include “being gay makes me feel part of a community” and “it is very important to me that at least some of my friends are bisexual or gay”. The scale was validated on White and African American gay men with reliability ranging from 0.74 to 0.78.
Dependent Variables
The main dependent variable was unprotected anal sex with a man; consequently, youth who had not initiated sexual activity (n = 9) were excluded from the analyses. Two participants were excluded because of missing data (due to frequently refusing to answer survey questions). Therefore, the final analytic sample size consisted of 189 participants in the three groups: 69 African American, 64 Hispanic, 56 White. We classified youth as having had unprotected sex if they reported less than 100% condom use during anal sex in the past 90 days. We classified youth as not having had unprotected sex if they used condoms 100% of the time or did not have anal sex in the past 90 days. Using this definition, 30.4% (21/69) of African Americans, 28.1% (18/64) of Hispanics, and 26.8% (15/56) of White YMSM were classified as having had unprotected sex.
Data Analyses
First, we used chi-square tests and ANOVA to assess the differences in demographic, psychosocial, sexual behavior, and drug use factors across the three ethnic groups (African American, Hispanic, White) using post-hoc tests and Bonferroni’s correction to further investigate statistically significant group-level differences. Next, we conducted within group comparisons at the univariate level to identify predictors to include in each of the three logistic regression models. We examined the associations between the hypothesized risk factors (age, born in the US, in long-term relationship, received public aid, kicked out because of sexual orientation, spent night in a shelter, ever used alcohol, ever used marijuana, ever used drugs, ethnic identity, gay community attachment, and age at initiation of sexual behavior) and unprotected sex within each group using chi-square and Student’s t-tests. We then fit three separate logistic regression models (one per ethnic group) to test the hypothesized associations between the independent variables and unprotected sex at the multivariate level. Following the recommendations of Hosmer and Lemeshow (2000), we identified variables with p values of 0.20 or lower for each ethnic group because use of more traditional significance levels (e.g., 0.05) might fail to identify important relationships. To facilitate interpretation of the results, we included all identified factors as candidate predictors in each of the three logistic regressions. We included site (Chicago versus South Florida) as a control variable in these regressions to account for potential site differences. There was evidence of collinearity between having been born in the U.S. and the Multi-Ethnic Identity Measure. We used the Multi-Ethnic Identity Measure in the logistic regressions because it was statistically significant for both African Americans and Hispanics whereas having been born in the U.S. was only significant for Hispanics.
Results
Table 1 presents the comparisons of the demographic and psychosocial variables across the three groups. Hispanic participants were more likely to have been born outside of the United States than were members of the other two groups (χ 2 2df = 33.1; p < 0.01). White participants were less likely than both African Americans and Hispanics to have received public assistance in the form of food stamps or reduced price school lunches (χ 22df = 21.5; p < 0.01). African American participants had a lower level of attachment to the gay community (F(2,184) = 4.5; p < 0.05) and a higher level of identification with their racial/ethnic group (F(2,184) = 4.4; p < 0.05) than did White participants.
Drug use comparisons across the three ethnic groups are presented in Table 2. Whites were more likely to have used marijuana (χ 22df = 15.5; p < 0.01) and street drugs (χ 22df = 15.7; p < 0.01) than Hispanics and African Americans. African Americans were less likely to report cocaine use (χ 22df = 11.5; p < 0.01) or methamphetamine use (χ 22df = 9.87; p < 0.05) in the last 90 days than either Hispanics or Whites. Ecstasy use in the last 90 days was higher among Whites than African Americans (χ 22df = 11.4; p < 0.01).
Table 3 presents the sexual behavior comparisons across the three ethnic groups. The average age at initiation of sexual behavior ranged from 14.5 to 14.8 years. African American participants were more likely than Whites to have ever had vaginal sex (χ 22df = 6.1; p < 0.05), and were less likely than Whites to have ever done something sexual they had not intended to do because of alcohol (χ 22df = 7.5; p < 0.05) or drug use (χ 22df = 14.1; p < 0.05). African American participants were also less likely than Hispanics to have ever had receptive anal sex (χ 22df = 6.0; p < 0.05).
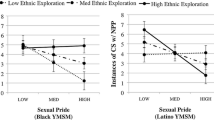
The results of the univariate analyses within racial/ethnic groups are presented in Table 4 and the within group multivariate logistic regression results are presented in Table 5. Variables that were entered into the multivariate logistic regression models were: age, being in a long-term relationship, being kicked out of the home, ever used street drugs, ethnic identity, and age at initiation of sexual behavior (see Table 4 for p-values achieved for entry). In the final multivariate logistic regressions, for African Americans, unprotected sex was associated with: being in a long-term relationship (OR = 7.1, 95% CI: 1.4, 35.7; p < 0.05), having been previously kicked out of their home because of their sexual orientation (OR = 4.5, 95% CI: 1.1, 18.9; p < 0.05), and younger age at initiation of sexual behavior (OR = 0.7, 95% CI: 0.6, 0.9; p < 0.01). For Hispanics, unprotected sex was associated with increased Hispanic ethnic identification (OR = 5.6, 95% CI: 1.2, 26.3; p < 0.05) and older age at initiation of sexual behavior (OR = 1.6, 95% CI: 1.1, 2.3; p < 0.05). For Whites, no predictors were statistically significant; however, younger age at initiation of sexual behavior was of borderline significance (OR = 0.8, 95% CI: 0.6, 1.0; p = 0.08).
To ensure the soundness of our decision to include all identified factors as candidate predictors in each of the three logistic regressions, we conducted post-hoc analyses within each ethnic group using only the factors significant at the 0.20 level for that particular ethnic group. The findings of the post-hoc regressions mirrored the results of the primary analyses in both significance and direction. All variables that were statistically significant in the primary analyses remained significant in the post-hoc models and all directional associations stayed the same.
Discussion
This study supports the need to tailor HIV prevention interventions to fit an individual’s racial and ethnic identity. As anticipated, each ethnic group had a different set of factors that were associated with unprotected sex. However, we did not anticipate that the direction of association would vary by ethnic group (as was the case for age at initiation of sexual behavior). For African American youth, the statistically significant associations were in the hypothesized direction; unprotected sex was associated with being in a long-term relationship, having been kicked out of home, and younger age at initiation of sexual behavior. For Hispanic youth, the associations were in the opposite direction of what was hypothesized; unprotected sex was associated with more ethnic identity and older age at initiation of sexual behavior. For White youth, no statistically significant associations with unprotected sex were found. These findings highlight the importance of considering racial and ethnic factors during development of tailored HIV prevention interventions.
Although the analytic approach selected does not allow us to statistically compare the results of the multivariate logistic regressions, discussing the three models in light of each other may be useful for intervention development efforts. It is noteworthy that being in a long-term relationship was associated with unprotected sex for African Americans only, despite having been demonstrated in older Hispanic and White MSM (Díaz et al. 1999; Carballo-Diéguez et al. 1997). Because of the level of trust and acceptance typical of a long-term relationship, the association between being in a relationship and unprotected sex is not unexpected; what was surprising was that this association did not emerge for Hispanic and White YMSM. Twice as many African American as Hispanic or White youth were in long-term relationships. Since the p-value of the association for Hispanic youth trended towards significance (Wald χ2 1df = 1.9; p = 0.168) and only seven Hispanic YMSM reported being in a long-term relationship, this lack of association could be due to limited sample size. This was not the case for White youth, given the p-value of 0.931. Unfortunately, we did not link reports of unprotected sex with partner type; therefore, we are unable to determine if unprotected sex was with their primary partner or a casual partner. Nonetheless, our findings could suggest that prevention messages are not effectively reaching African American youth and conveying the importance of protecting oneself, even within a long-term relationship (Rhodes et al. 2006).
The finding that having been kicked out of home because of sexual orientation was correlated with unprotected sex only among African Americans could be reflective of the importance of a sense of community and belonging within the African American community, especially with respect to family (Williams et al. 2004; Jiminez 2003; Stokes and Peterson 1998; Whitehead 1997; Billingsley and Caldwell 1991). Being kicked out of home could be perceived as a double rejection by both their family and their previously tight-knit community, and could lead African American youth to subsequently seek acceptance and intimacy through not using condoms, as has been shown among adult African American MSM (Williams et al. 2004). In addition, individuals who have been kicked out of their home are no longer able to receive parent–adolescent communication about sexual risk behaviors, which has been shown to promote safe sex among minority adolescents (Kotchick et al. 1999). These youth are also likely to be more lonely than youth who have not been kicked out of their homes, a recognized risk factor for unprotected sex among African American youth (DiClemente et al. 1996).
It was surprising that higher ethnic identification was associated with risk rather than protection for Hispanic YMSM. Some have argued that traditional Hispanic cultural values (e.g., machismo, fatalismo, sexual silence) can impede frank and open discussions regarding condom use and increase HIV risk (Makulowich 1998; Marin et al. 1993). Machista attitudes include a sense of invincibility and need for domination, which has been shown for heterosexual Hispanic men to be tied to decreased willingness to use condoms (Schutt-Aine and Maddaleno 2002; Sternberg 2000). Fatalistic attitudes are reflected in notions of the inevitability of HIV infection and the placement of all things into “God’s hands,” which has also been tied to decreased willingness to use condoms (Organista et al. 2000; Díaz and Ayala 1999). While there is a large literature linking increased level of acculturation with increased risk behaviors among Hispanic adolescents in the U.S., it is important to note that ethnic identification and acculturation are separate constructs and the association between acculturation and risk is complex. For instance, in one of our previous studies with Hispanic MSM, we used a multi-dimensional measure of acculturation, and found it was lower orientation to Hispanic culture (Hispanicism) rather than higher orientation to American culture (Americanism) per se that was significantly associated with drug use (OR = 0.82, p = 0.01 vs OR = 1.01, p = 0.22) (Fernández et al. 2007). We did not find this to be the case for unprotected sex. Future studies should further examine the impact of ethnic identity on HIV risk and protection and its association with acculturation.
The most surprising result for young Hispanic MSM, and one that is contrary to what has been previously reported in the literature (e.g., Koyle et al. 1989), was the relationship between older age at initiation of sexual behavior and unprotected sex. This was not the case for African American youth, for whom younger age at initiation was associated with unprotected sex, or White youth, for whom younger age at initiation trended towards significance with respect to unprotected sex. It could be that when initiating at an older age, Hispanic youth were more likely to have internalized the cultural values of machismo and fatalism and were therefore less likely to use condoms than youth who initiated at a younger age before such values had been fully adopted. This finding in particular merits further investigation to see if the results can be replicated and if so, to explore the underlying relationship.
The results of this study should be interpreted within the framework of the study’s design and limitations. Although we recruited in two large, metropolitan areas, our sample size was moderate and not designed to be representative of the population of YMSM. Because of the hidden nature of the population, however, obtaining a representative sample would be difficult and costly. We did not conduct an omnibus model because we did not have sufficient sample size for such a model and we wanted to examine predictors of unprotected sex within each ethnic group. The relatively small sample size per ethnic group did not permit statistical analyses directly comparing the three groups; therefore, the comparisons made in this paper should be viewed within the context of this limitation. While we recognize that the study’s sample size and the resulting analytical approach selected does not allow for statistical comparisons of the predictors to be made across the groups, it offers an important first step in understanding racial and ethnic differences in predictors of unprotected sex and may lay the groundwork for future study in this area. Our assessment did not include questions about condom use while high; therefore, the lack of relationship demonstrated between drug use and unprotected sex could be attributed to measurement issues. Because our assessment of number of partners was specific to each type of sex act, we are not able to report a total number of partners in the past 90 days. This prevented this potential covariate from being included in the analyses.
This study is an important first step towards developing tailored HIV prevention interventions. Because the strength and the direction of association of predictors varied by ethnic group, culturally-sensitive interventions should target the specific needs, expectations, and social pressures faced by youth within their individual cultural realities, and the impact this may have on condom use.
References
Arnett, J. J. (1992). Reckless behavior in adolescence: A developmental perspective. Developmental Review, 12, 339–373.
Arnett, J. J. (1997). Young people’s conceptions of the transition to adulthood. Youth and Society, 29, 3–23.
Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55, 469–480.
Bachman, J. G., Johnston, L. D., O’Malley, P., & Schulenberg, J. (1996). Transitions in drug use during late adolescence, young adulthood. In J. A. Graber, J. Brooks-Gunn, & A. C. Petersen (Eds.), Transitions through adolescence: Interpersonal domains and context (pp. 111–140). Mahwah, NJ: Erlbaum.
Billingsley, A., & Caldwell, C. H. (1991). The church, the family, and the school in the African American community. Journal of Negro Education, 60, 427–440.
Blake, S. M., Ledsky, R., Lehman, T., Goodenow, C., Sawyer, R., & Hack, T. (2001). Preventing sexual risk behaviors among gay, lesbian, and bisexual adolescents: The benefits of gay-sensitive HIV instruction in schools. American Journal of Public Health, 91, 940–946.
Bonilla, L., & Porter, J. (1990). A comparison of Latino, Black, and non-Hispanic White attitudes towards homosexuality. Hispanic Journal of Behavioral Sciences, 12, 437–452.
Carballo-Dieguez, A., Remien, R., Dolezal, C., & Wagner, G. (1997). Unsafe sex in the primary relationships of Puerto Rican men who have sex with men. AIDS and Behavior, 1, 9–17.
Díaz, R. M. (1998). Latino gay men and HIV: Culture, sexuality, and risk behavior. New York: Routledge.
Díaz, R. M., & Ayala, G. (1999). Love, passion, and rebellion: Ideologies of HIV risk among Latino gay men in the USA. Culture, Health, and Sexuality, 1, 277–293.
Díaz, R. M., Ayala, G., & Bein, E. (2004). Sexual risk as an outcome of social oppression: Data from a probability sample of Latino gay men in three U.S. cities. Cultural Diversity and Ethnic Minority Psychology, 10, 255–267.
Díaz, R. M., Heckert, A. L., & Sanchez, J. (2005). Reasons for stimulant use among Latino gay men in San Francisco: A comparison between methamphetamine and cocaine users. Journal of Urban Health, 82, i71–i78.
Díaz, R. M., Moralis, E. S., Bein, E., DIlan, E., & Rodriguez, R. A. (1999). Predictors of sexual risk in Latino gay/bisexual men: The role of demographic, developmental, social cognitive, and behavioral variables. Hispanic Journal of Behavioral Sciences, 21, 480–501.
DiClemente, R. J., Lodico, M., Grinstead, O. A., Harper, G., Rickman, R. L., Evans, P. E., & Coates, T. J. (1996). African-American adolescents residing in high-risk urban environments do use condoms: Correlates and predictors of condom use among adolescents in public housing developments. Pediatrics, 98, 269–278.
Erikson, E. H. (1968). Identity, youth, and crisis. New York: Norton.
Fernández, M. I., Bowen, G. S., Varga, L. M., Collazo, J. B., Hernandez, N., Perrino, T., & Rehbein, A. (2005). High rates of club drug use and risky sexual practices among Hispanic men who have sex with men in Miami, Florida. Substance Use and Misuse, 40, 1347–1362.
Fernández, M. I., Bowen, G. S., Warren, J. C., Ibañez, G. E., Hernandez, N., Harper, G. W., & Prado, G. (2007). Crystal methamphetamine: A source of added sexual risk for Hispanic men who have sex with men? Drug and Alcohol Dependence, 86, 245–252.
Hall, H. I., Byers, R. H., Ling, Q., & Espinoza, L. (2007). Racial/ethnic and age disparities in HIV prevalence and disease progression among men who have sex with men in the United States. American Journal of Public Health, 97, 1060–1066.
Harawa, N. T., Greenland, S., Bingham, T. A., Johnson, D. F., Cochran, S. D., Cunningham, W. E., Celentano, D. D., Koblin, B. A., LaLota, M., MacKellar, D. A., McFarland, W., Shehan, D., Stoyanoff, S., Thiede, H., Torian, L., & Valleroy, L. A. (2004). Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the United States. Journal of Acquired Immune Deficiency Syndromes, 35, 526–536.
Harper, G. W., Hosek, S. G., Contreras, R., & Doll, M. (2003). Psychosocial factors impacting adolescent condom use: A review and theoretical integration. Journal of HIV/AIDS Prevention and Education for Children and Adolescents, 5(3), 33–69.
Harper, G. W., Jernewall, N., & Zea, M. C. (2004). Giving voice to emerging science and theory for lesbian, gay, and bisexual people of color. Cultural Diversity and Ethnic Minority Psychology, 10, 187–199.
Harper, G. W., & Schneider, M. (2003). Oppression and discrimination among lesbian, gay, bisexual, and transgendered people and communities: A challenge for community psychology. American Journal of Community Psychology, 31(3/4), 243–252.
Hart, T., & Peterson, J. L. (2004). Predictors of risky sexual behavior among young African-American men who have sex with men. American Journal of Public Health, 94, 1122–1123.
Hosmer, D. W., & Lemeshow, S. (2000). Applied logistic regression. New York: Wiley.
Jiminez, A. (2003). Triple jeopardy: Targeting older men of color who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 33, 222–225.
Kotchick, B. A., Dorsey, S., Miller, K. S., & Foreman, R. (1999). Adolescent sexual risk-taking behavior in single-parent ethnic minority families. Journal of Family Psychology, 13, 93–102.
Koyle, P., Jensen, L., & Olsen, J. (1989). Comparison of sexual behaviors among adolescents having an early, middle and late first intercourse experience. Youth and Society, 20, 461–476.
Makulowich, G. S. (1998). HIV and STD prevention update. AIDS Patient Care and STDs, 12, 71–73.
Marin, B. V. (2003). HIV prevention in the Hispanic community: Sex, culture, and empowerment. Journal of Transcultural Nursing, 14, 186–192.
Marin, B. V., Gomez, C. A., & Tschann, J. M. (1993). Condom use among Hispanic men with secondary female sexual partners. Public Health Reports, 108, 742–750.
Myers, H. F., Javanbakht, M., Martinez, M., & Obediah, S. (2003). Psychosocial predictors of risky sexual behaviors in African American men: Implications for prevention. AIDS Education and Prevention, 15, 66–79.
National Institute of Mental Health Multisite HIV Prevention Trial Group. (2002). Predictors of sexual behavior patterns over one year among persons at high risk for HIV. Archives of Sexual Behavior, 31, 165–176.
O’Donnell, L., Agronick, G., San Doval, A., Duran, R., Myint-U, A., & Stueve, A. (2002). Ethnic and gay community attachments and sexual risk behaviors among urban Latino young men who have sex with men. AIDS Education and Prevention, 14, 457–471.
O’Malley, P. M., Johnston, L. D., & Bachman, J. G. (1992). Adolescent substance use and addictions: Epidemiology, current trends, and public policy. Adolescent Medicine: State of the Art Reviews, 4, 227–248.
O’Malley, P. M., Johnston, L. D., & Bachman, J. G. (1995). Adolescent substance use: Epidemiology and implications for public policy. Substance Abuse, 42, 241–260.
O’Malley, P. M., Johnston, L. D., & Bachman, J. G. (1998). Alcohol use among adolescents. Alcohol Research and Health, 22, 85–93.
Organista, K. C., Organista, P. B., Bola, J. R., Javier, E., de Alba, G. G., & Moran, M. A. C. (2000). Predictors of condom use in Mexican migrant laborers. American Journal of Community Psychology, 28, 245–265.
Peterson, J. L., & Carballo-Dieguez, A. (2000). HIV prevention among African American and Latino men who have sex with men. In J. L. Peterson & R. D. DiClemente (Eds.), Handbook of HIV prevention (pp. 217–224). New York: Kluwer Academic/Plenum Publishers.
Phinney, J. (1992). The Multigroup Ethnic Identity Measure: A new scale for use with adolescents and young adults from diverse groups. Journal of Adolescent Research, 7, 156–176.
Rangel, M., Gavin, L., Reed, C., Fowler, M., & Lee, L. (2006). Epidemiology of HIV and AIDS among adolescents and young adults in the U.S Journal of Adolescent Health, 39, 156–163.
Rhodes, S. D., Yee, L. J., & Hergenrather, K. C. (2006). A community-based rapid assessment of HIV behavioral risk disparities within a large sample of gay men in southeastern USA: A comparison of African American, Latino and White men. AIDS Care, 18, 1018–1024.
Roberts, R., Phinney, J., Masse, L., Chen, Y., Roberts, C., & Romero, A. (1999). The structure of ethnic identity in young adolescents from diverse ethnocultural groups. Journal of Early Adolescence, 19, 301–322.
Rosario, M., Hunter, J., Maguen, S., Gwadz, M., & Smith, R. (2001). The coming-out process and its adaptational and health-related associations among gay, lesbian, and bisexual youths: Stipulation and exploration of a model. American Journal of Community Psychology, 29(1), 113–160.
Rotheram-Borus, M. J., Reid, H., Rosario, M., & Kasen, S. (1995). Determinants of safer sex patterns among gay/bisexual male adolescents. Journal of Adolescence, 18(1), 3–15.
Ryan, C., & Futterman, D. (1998). Lesbian and gay youth: Care and counseling. New York: Columbia University Press.
Schutt-Aine, J., & Maddaleno, M. (2002). Addressing machismo with adolescent males—a new approach to HIV/AIDS prevention. Poster presented at the XIV International AIDS Conference. Barcelona, Spain, July 7–12, 2006. Abstract D11104.
Sternberg, P. (2000). Challenging machismo: Promoting sexual and reproductive health with Nicaraguan men. Gender and Development, 8, 89–99.
Stokes, J. P., & Peterson, J. L. (1998). Homophobia, self-esteem, and risk for HIV among African American men who have sex with men. AIDS Education and Prevention, 10, 278–292.
Tremble, B., Schneider, M., & Appathurai, C. (1989). Growing up gay or lesbian in a multicultural context. Journal of Homosexuality, 17, 253–267.
Valleroy, L. A., MacKellar, D. A., Karon, J. M., Rosen, D. H., McFarland, W., Shehan, D. A., Stoyanoff, S. R., LaLota, M., Celentano, D. D., Koblin, B. A., Thiede, H., Katz, M. H., Torian, L. V., & Janssen, R. S. (2000). HIV prevalence and associated risks in young men who have sex with men. Journal of the American Medical Association, 284, 198–204.
Vanable, P. S., McKirnan, D. J., & Stokes, J. P. (1992). Identification and involvement with the gay community scale [IGCS]. In Handbook of sexuality – related measures (pp. 407–409). Thousand Oaks, California: Sage Publications.
Waldo, C. R., Hesson-McInnis, M. S., & D’Augelli, A. R. (1998). Antecedents and consequences of victimization of lesbian, gay, and bisexual young people: A structural model comparing rural university and urban samples. American Journal of Community Psychology, 26(2), 307–334.
Washington, P. (2001). Who gets to drink from the fountain of freedom? Homophobia in communities of color. Journal of Gay and Lesbian Social Services, 13, 117–131.
Whitehead, T. (1997). Urban low-income African American men, HIV/AIDS, and gender identity. Medical Anthropology Quarterly, 11, 411–447.
Williams, J. K., Wyatt, G. E., Resell, J., Peterson, J., & Asuan-O’Brien, A. (2004). Psychosocial issues among gay and non-gay identifying HIV-seropositive African American and Latino MSM. Cultural Diversity and Ethnic Minority Psychology, 10, 268–286.
Wolitski, R. J., Valdiserri, R. O., Denning, P. H., & Levine, W. C. (2001). Are we headed for a resurgence in the HIV epidemic among men who have sex with men? American Journal of Public Health, 91, 883–888.
Zea, M. C., Reisen, C. A., & Díaz, R. M. (2003). Methodological issues in research on sexual behavior with Latino gay and bisexual men. American Journal of Community Psychology, 31, 281–291.
Acknowledgments
The Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) is funded by grant No. U01 HD40506-01 from the National Institutes of Health through the National Institute of Child Health and Human Development (Bill Kappogianis, MD; Sonia Lee, PhD) with supplemental funding from the National Institutes on Drug Abuse (Nicolette Borek, PhD) and Mental Health (Susannah Allison, PhD; Pim Brouwers, PhD). We would like to thank Larry Friedman, MD, PI of the Miami Adolescent Trials Unit and the staff of the Behavioral Health Promotion Program (Cesar deFuentes, Luis Alzamora, Cristobal Plaza, and Leah Varga) and participating staff at DePaul University (Bianca Wilson). ATN 020 has been scientifically reviewed by the ATN’s Behavioral Leadership Group. We would also like to thank individuals from the ATN Data and Operations Center (Westat, Inc.) including Jim Korelitz, PhD; Barbara Driver, RN, MS; and individuals from the ATN Coordinating Center at the University of Alabama including Craig Wilson, MD; Cindy Partlow, MEd; Marcia Berck, BA; and Pam Gore. Additionally, we would like to acknowledge the thoughtful input given by participants of our national and local Youth Community Advisory Boards. Finally, we would like to thank the young men who participated in this study, whose willingness to share their own stories makes our work possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Warren, J.C., Fernández, M.I., Harper, G.W. et al. Predictors of Unprotected Sex among Young Sexually Active African American, Hispanic, and White MSM: The Importance of Ethnicity and Culture. AIDS Behav 12, 459–468 (2008). https://doi.org/10.1007/s10461-007-9291-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-007-9291-y