Abstract
Little research has been done on the relationship between sexual compulsivity and the sexual risk behaviors of methamphetamine (meth) users. This exploratory study sought to identify correlates of sexual compulsivity in a sample of 217 HIV-positive meth-using gay and bisexual men. Participants reported a mean score of 2.4 on the Sexual Compulsivity Scale (SCS) (SD=.76, range 1–4). Sexual compulsivity was positively associated with high-risk sexual behaviors (e.g., number of unprotected sex acts with anonymous partners, total number of HIV-negative or unknown serostatus partners). In multivariate analyses, higher scores on sexual compulsivity were associated with older age, meth use before or during sex, visits to sex clubs and street corners to find sex partners, lower self-efficacy for condom use, lower levels of self-esteem, higher scores on a measure of disinhibition, and a greater number of HIV-negative or unknown serostatus partners. The results suggest that more attention should be focused on sexual compulsivity and its correlates to determine how they may contribute to resistance to sexual behavior change in this high-risk population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past twenty years, HIV prevention researchers have sought to identify personal characteristics of individuals that may help to explain participation in unprotected sexual activity despite the potential for contracting HIV and other sexually transmitted infections (STIs). Sexual compulsivity is one concept that has been examined in relation to unsafe sexual practices, particularly among gay and bisexual men. Kalichman and Rompa (1995) defined sexual compulsivity as “an insistent, repetitive, intrusive, and unwanted urge to perform specific acts often in ritualized or routinized fashions” (p. 587). The researchers argued that individuals who are preoccupied with sex and who have difficulty controlling their sexual urges will be more inclined to engage in sexual risk behavior despite the possible adverse health consequences (Kalichman & Cain, 2004).
A growing body of literature documents an association between sexual compulsivity and sexual risk behaviors among gay and bisexual men. In a study of same-gender sexually active “at risk” men, Kalichman and Rompa (1995) found significant correlations between sexual compulsivity and both insertive and receptive anal intercourse without a condom. Sexual compulsivity was also positively correlated with number of unprotected anal sex partners.
In a study of HIV-positive gay and bisexual men, Benotsch, Kalichman, and Kelly (1999) reported that participants who scored highest on a measure of sexual compulsivity engaged in more total unprotected anal and oral sex acts and had more sex partners as compared to those who had lower scores. Sexually compulsive gay and bisexual men also reported more unprotected receptive anal and oral sex acts, and they rated high-risk sexual acts as more pleasurable as compared to their less sexually compulsive counterparts. In another study of HIV-positive, mostly gay and bisexual men, Kalichman, Greenberg, and Abel (1997) reported that participants who engaged in unprotected sex with multiple partners had higher levels of sexual compulsivity as compared to men who had one or no partners.
Sexual compulsivity has also been studied in relation to the sexual risk practices of gay and bisexual male escorts in New York City (Parsons, Bimbi, & Halkitis, 2001). In this study, sexual compulsivity was associated with number of non-work sexual partners, frequency of unprotected anal receptive sex to ejaculation with both work and non-work partners, and frequency of unprotected anal insertive sex to ejaculation with work partners.
Studies of HIV-positive men and women have also demonstrated a relationship between sexual compulsivity and sexual risk behavior. Benotsch, Kalichman, and Pinkerton (2001) studied the role of sexual compulsivity as a contributing factor to HIV risk behaviors in a sample of HIV-positive inner city men and women. The researchers found that individuals who scored higher on sexual compulsivity reported more total sex partners, and more HIV-negative and unknown serostatus partners as compared to participants with lower sexual compulsivity scores. Men with higher sexual compulsivity scores also reported more unprotected insertive and receptive anal sex and more unprotected vaginal sex with non-HIV positive partners as compared to their lower scoring counterparts. Moreover, women reported more unprotected anal sex with non-positive partners as compared to women who scored lower on sexual compulsivity. Kalichman and Rompa (2001) also found positive associations between sexual compulsivity and high frequency sexual behaviors and number of sexual partners in a sample of HIV-positive inner-city men and women. Among both men and women, sexual compulsivity was associated with greater frequency of unprotected anal and oral sex, a larger number of sex partners, and more frequent masturbation. Men who scored high on sexual compulsivity also had more HIV-negative and unknown serostatus partners and were more likely to report having had an STI in the past three months. Taken together, these studies consistently document an association between sexual compulsivity and unsafe sexual practices in samples of HIV-positive and “at risk” gay and bisexual men and HIV-positive inner-city men and women.
Several demographic variables have yielded significant associations with sexual compulsivity. Men and younger persons report higher levels of sexual compulsivity (Dodge, Reece, Cole, & Standfort, 2004). Sexually compulsive individuals are also more likely to have had an STI (Benotsch et al., 1999; Kalichman & Rompa, 2001). Higher levels of sexual compulsivity have also been associated with a number of psychosocial constructs including more loneliness, lower self-esteem/self-confidence, more sexual sensation-seeking, higher levels of anxiety and depression, a history of childhood sexual abuse, greater pessimism, and higher levels of obsessive-compulsiveness (Benotsch et al., 1999; Cooper, Scherer, Boies, & Gordon, 1999; Kalichman et al., 1994; Kalichman & Rompa, 2001; Parsons et al., 2001). Researchers have also found significant positive relationships between sexual compulsivity and use of substances, including powder cocaine, use of alcohol before sex, and use of drugs in sexual contexts (Kalichman & Rompa, 1995; Benotsch et al., 1999; Benotsch et al., 2001; Kalichman & Cain, 2004). Higher levels of problem drinking have also been associated with sexual compulsivity (Benotsch et al., 1999). In our review of the literature, we were unable to find any published studies that examined sexual compulsivity in relation to the sexual venues where individuals go to find sex partners.
To date, no studies have investigated the relationship between sexual compulsivity and sexual risk in a sample of meth users. The link between meth use and participation in risky sexual activities has been well established in a both gay and non-gay populations (e.g., Reback, 1997; Semple, Patterson, & Grant, 2004). Early studies of meth-using gay and bisexual men in the western United States reported high rates of sexual risk behaviors, including multiple partners and unprotected anal sex (Reback, 1997; Semple, Patterson, & Grant, 2002). More recently, Halkitis, Shrem, and Martin (2005) reported high rates of unprotected insertive and receptive anal sex among meth-using gay and bisexual men in New York City. Halkitis, Fischgrund, and Parsons (2005) also found that HIV-positive gay and bisexual meth users were more likely to report using meth for sexual reasons, whereas their HIV-negative counterparts reported greater use of meth for social reasons. In another study of gay and bisexual meth users in Miami, Kurtz (2005) found a relationship between continued use of meth and involvement in sexual risk behavior that placed men at risk for HIV and other STIs. In a study of young, gay men in British Columbia, Canada, researchers found a positive association between meth use and unprotected anal sex, and reported that meth was more likely to be used by HIV-positive men as compared to control subjects (Schilder, Lampinen, Miller, & Hogg, 2005).
Given the substantial body of research on the link between meth use and high risk sex among gay and bisexual men, it is not unreasonable to suggest that those who have higher levels of sexual compulsivity will potentially engage in even more frequent or more risky sexual behaviors as compared to their less sexually compulsive counterparts. Furthermore, if a meth user is sexually compulsive and HIV-positive, the risk of HIV transmission to uninfected sex partners may be significantly increased, thereby contributing to the growing number of new cases of HIV among gay and bisexual men in the United States. Research that enhances our understanding of sexual compulsivity in the target population has the potential to help explain continued unsafe sexual practices among HIV-positive, meth-using gay and bisexual men. Moreover, identification of the correlates of sexual compulsivity in the target population could provide clues as to effective treatment strategies, which might involve psychotherapy, behavioral self-management strategies, pharmacological treatments, or a combination of treatment approaches.
The primary objective of this research was to investigate sexual compulsivity in a sample of HIV-positive meth-using gay and bisexual men. Exploratory analyses were used to address three research questions: (a) What is the degree of variability in sexual compulsivity in a sample of HIV-positive meth-using gay and bisexual men?; (b) Is sexual compulsivity associated with high-risk sexual behaviors in this population?; and (c) Is sexual compulsivity associated with demographic variables, drug and alcohol variables, sexual venue variables, and psychosocial factors?
Method
Participants and procedures
The present analyses used baseline data from a sample of 217 HIV-positive gay and bisexual men who were enrolled in the EDGE research project at the University of California, San Diego (UCSD). The EDGE is a theory-based sexual risk reduction intervention designed specifically for HIV-positive Men Who Have Sex with Men (MSM) who are active users of methamphetamine. Eligibility was based on the following criteria: male; HIV-positive serostatus; had unprotected anal or oral sex with an HIV-negative or unknown serostatus male partner during the previous two months; and used methamphetamine at least twice in the past two months. Methamphetamine-using men who had HIV-positive partners only and those who consistently used condoms with all HIV-negative and unknown serostatus partners over the previous two months were excluded from study participation because the intervention was designed to reduce HIV transmission risk to uninfected individuals. Additional exclusion criteria included: knowing HIV-positive serostatus for less than two months; current psychotic or suicidal symptoms; and current enrollment in a methamphetamine treatment program.
Data were collected through face-to-face interviews by trained project personnel. The interview took approximately 90 min to complete and covered a range of topics including sociodemographic characteristics, current and past patterns of methamphetamine use, use of alcohol and illicit drugs, sexual risk behaviors, social network factors, social support, social cognitive factors, and physical and psychiatric health variables. Participants were randomly assigned to either a five session safer sex counseling condition or a time–equivalent, diet and exercise attention-control condition. Followup assessments were conducted at 4, 8, and 12 months post-baseline. Participants were paid $30 for their baseline assessment and first counseling session. Data were gathered between June 2001 and August 2004. The present analyses used data from participants' baseline interview.
Primary recruitment strategies on the EDGE project involved street outreach, large-scale poster campaigns, advertisements in the media, referrals from care providers (e.g., physicians, case managers), and referrals from enrolled participants. Recruitment sources from within the community included gay organizations and groups, HIV specialty health clinics, and gay-identified events and venues (e.g., gay pride, bars, dance clubs). The EDGE was advertised as a university-sponsored program for HIV-positive MSM who wanted to learn more about safer sex practices. In the present sample, 31.5% of participants were recruited through the poster/media campaign, 4.9% were recruited through outreach workers, 38.1% were referrals from care providers and community-based agencies, and 25.5% were recruited through referrals from friends, family members, and enrolled participants.
Measures
Demographic variables
Age was coded as a continuous variable. Ethnicity, education, income, living arrangement, and sexual orientation were coded as categorical variables: ethnicity (1: Caucasian, 2: African American, 3: Hispanic, 4: Other); education (1: Some high school or less, 2: High school or equivalent, 3: Some college, 4: College degree, 5: Advanced degree); income ($19,999 or less/year = 0, more than $19,999/year = 1); living arrangement (1: live with spouse, 2: living with steady partner, 3: live with other adult(s), 4: live alone, 5: homeless, 6: other) and sexual orientation (1: gay/homosexual, 2: heterosexual, 3: bisexual, 4: not sure). The Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA-II/Section G) was used to determine the severity of participants' use of methamphetamine (Bucholz et al., 1994, 1995).
Drug and alcohol variables
Two items assessed how often during the past 2 months the participant had consumed alcohol and became intoxicated from drinking alcohol. Response categories ranged from 0 (Never) to 3 (Very Often). Illicit drug use was measured with a 12-item scale developed by Temoshok and Nannis (1992). Participants were asked how often during the past two months they had taken the following illicit drugs: marijuana or hashish, powder cocaine, crack cocaine, amyl or butylnitrates (poppers), ecstasy, hallucinogens, heroin, Ketamine (Special K), Gamma Hydroxybutyrate (GHB), steroids (obtained illegally), inhalants, and other. Response categories ranged from 0 (Never) to 3 (Very Often). Total number of illicit drugs used during the past two months was used in these analyses. In addition, three questions assessed participants' use of alcohol, meth, and drugs other than meth before or during sex (e.g., “During the past 2 months, how often did you use meth before or during sex?”). Response categories ranged from 0 (Never) to 3 (Very Often). Binge use of meth was defined in the following way: “By binge user, I mean you keep using large quantities of meth for a period of time—until you run out or just can't physically do it anymore.” Response categories were 1 = yes and 0 = no. Injection use of meth was assessed using the following question: “In the past two months, how often did you inject meth or some combination of meth?” Response categories ranged from 0 (Never) to 3 (Very Often).
Sexual venue variables
Participants were presented with a list of twelve venues and asked the following question: “During the past two months, when you were high on meth, did you go to any of the following places to find sex partners?” A dichotomous response category was utilized (Yes = 1, No = 0). The list of sexual venues was compiled during the qualitative phase of the EDGE research project (Semple et al., 2002), and included private (e.g., sex in own home or sex partner's home), commercial (i.e., bathhouse, sex club, adult bookstore, gay theater, bar, dance club, afterhours club), and public locations (i.e., park, public restroom, street corner).
Psychosocial variables
Self-esteem was measured using the 40-item Self Esteem Rating Scale (SERS; Nugent & Thomas, 1993). The SERS is a global measure of self-esteem that taps into multiple areas of self-evaluation including self-worth, social competence, intellectual ability, physical attractiveness, self-competence, and worth to others. Half of the items are worded negatively (e.g., “I feel that I am ugly”) and half are worded positively (“I feel good about myself”). Response categories range from 1 (Never) to 7 (Always). Summary scores ranged from 40 to 280. Cronbach's alpha for the SERS was .96. The Sensation Seeking Inventory (Zuckerman, 1971) was used to assess risk taking tendency (10 items, alpha = .78) and disinhibition (10 items, alpha = .68). Risk taking is the desire to seek new experiences by choosing non-conventional friends, activities, and lifestyles (Sample item: “I often wish I could be a mountain climber” versus “I can't understand people who risk their necks climbing mountains”). Participants were instructed to circle the choice that best describes their likes or feelings. The disinhibition subscale measures the need to disinhibit behavior in a social context through such activities as drinking, partying, and varied sexual experiences (Sample item: “I like wild uninhibited parties” versus “I prefer quiet parties with good conversation”). Social stigma was measured by six items (alpha = .87). Participants were asked to report on actual experiences of rejection, ranging from minor slights to major life events, such as the loss of friends and family members (e.g., “I have lost friends because they found out about my meth use”). Items were measured on a 4-point scale, ranging from 1 (Strongly Disagree) to 4 (Strongly Agree). Self-efficacy for condom use was comprised of four items with an alpha of .76 (e.g., “I can use a condom in any situation; with different partners or in different places”). Self-efficacy for negotiation of safer sex consisted of three items with an alpha of .79 (e.g., “I can negotiate condom use with any sexual partner”). Self-efficacy for disclosure was assessed by three items with an alpha of .82 (e.g., “I can bring up the topic of my HIV-positive serostatus with any sexual partner”). The Beck Depression Inventory (BDI) was used to assess depressive symptoms (Beck, 1967, 1976). The BDI consists of 21 items, each having four graded statements that are ordered (0–3) to show increasing depressive symptoms. Summary scores ranged from 0 to 63. Cronbach alpha for the BDI was .89.
Sexual risk variables
Sexual risk behavior was defined as unprotected anal, oral, or vaginal sex with HIV-negative or unknown serostatus partners and HIV-positive partners. Three categories of partner type were assessed. Steady partner(s) were defined as person(s) with whom the participant had sex with on a regular basis (e.g., spouse, primary partner, or boyfriend). Casual partner(s) were defined as a person(s) with whom the participant was acquainted, and had a one-night stand or had sex with only once or twice. Anonymous partner(s) were defined as person(s) whom the participant did not know (e.g., hustler, someone encountered at a bathhouse or park). For each category of partner type, we calculated the total number of unprotected sex acts (i.e., anal, vaginal, and oral) over the previous two-month period.
Sexual compulsivity
This measure was defined as the dependent variable in these analyses. We utilized the 10-item sexual compulsivity scale developed by Kalichman et al. (1994). The sexual compulsivity scale consists of items that “reflect obsessive preoccupations with sexual acts and encounters” (p. 588; Kalichman & Rompa, 1995). Sample items include “My sexual appetite has gotten in the way of my relationships” and “I feel that sexual thoughts and feelings are stronger than I am.” Items are measured on a 4-point Likert-type scale, ranging from 1 (Not at all like me) to 4 (Very much like me). A summary variable was created by averaging participants' scores on the 10-item scale. Internal consistency reliability of the scale using the present sample was .92.
Data analysis
Univariate associations between sexual compulsivity and variables of interest were examined using Pearson correlation coefficients and independent sample t-tests. To correct for multiple comparisons, alpha was set to p < .01. Multiple regression analysis was used to examine multivariate relationships. Multiple regression permits an assessment of the direct effects of independent variables on the dependent variable while controlling for variables such as age. Regression coefficients (e.g., betas) reveal the strength of the association between the independent variables and the dependent variable. Regression coefficients are tested for statistical significance. The unique proportion of variance accounted for by each independent variable is expressed as sr 2. This indicator helps to determine the overall importance of each independent variable to the regression model. The R 2 reveals the proportion of variance in the dependent variable explained by the overall regression model. For more detail on the use of multiple regression methods in the behavioral sciences, see Cohen and Cohen (1983).
Results
Sample characteristics
By design, all participants were men who reported having unprotected sex with at least one HIV-negative or unknown serostatus male partner during the previous two months. Sample characteristics are presented in Table 1 below.
Univariate analyses
Participants' scores on the sexual compulsivity scale ranged from 1 to 4 with a mean of 2.4 (SD=.76) and a median of 2.4. Sexual compulsivity was examined in relation to five broad categories of variables: demographic variables; drug and alcohol use variables; sexual venue variables; psychosocial variables; and sexual risk variables. Variables that were significant at the univariate level were examined further using multivariate methods.
Sexual compulsivity and demographic variables
Sexual compulsivity was examined in relation to six demographic variables. A significant positive relationship was found between age and sexual compulsivity. As age increased, mean scores on sexual compulsivity increased, r(216)=.23, p < .01. No significant associations were found between sexual compulsivity and ethnicity, education, income, living arrangement or sexual orientation.
Sexual compulsivity and drug and alcohol variables
We found significant relationships between sexual compulsivity and all of the drug and alcohol variables examined in this research. Sexual compulsivity was positively associated with use of meth before or during sex, r(216)=.30, p < .01, number of illicit drugs used in the past two months, r(216)=.15, p < .01, use of alcohol before or during sex, r(215)=.16, p < .01, and becoming drunk from drinking alcohol, r(215)=.17, p < .01. In addition, binge users of meth had significantly higher sexual compulsivity scores as compared to non-binge users, 2.6 vs. 2.3, t(214)=2.8, p < .01, and injection users of meth scored higher on sexual compulsivity as compared to non-injectors, 2.6 vs. 2.2, t(214)=2.9, p < .01.
Sexual compulsivity and sexual venue variables
Sexual compulsivity was examined in relation to the venues where meth-using gay and bisexual men go to find sexual partners. Five venues were significantly associated with sexual compulsivity. Participants who reported going to the following venues to find sexual partners had higher mean scores on sexual compulsivity as compared to their counterparts who did not attend these venues: sex club, 2.8 vs. 2.3, t(214)=3.9, p < .01; adult bookstore, 2.6 vs. 2.3, t(212)=2.7, p < .01; public park, 2.6 vs. 2.2, t(214)=3.3, p < .01; public restroom, 2.8 vs. 2.3, t(214)=3.5, p < .01; and street corner, 2.9 vs. 2.3, t(214)=4.6, p < .01, respectively.
Sexual compulsivity and psychosocial variables
Sexual compulsivity was positively correlated with depressive symptoms, r(217)=.29, p < .01, disinhibition, r(215)= .33, p < .01, and social stigma, r(216)=.24, p < .01, but was inversely related to self-esteem, r(216)=−.32, p < .01, self-efficacy for condom use, r(216)=−.31, p < .01, and self-efficacy for disclosure of HIV serostatus, r(217)=−.26, p < .01. Sexual compulsivity was not associated with self-efficacy for negotiation of safer sex practices.
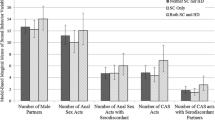
Sexual compulsivity and sexual risk behavior
Sexual compulsivity was examined in relation to six sexual risk variables, including number of HIV-negative or unknown serostatus partners, number of HIV-positive partners, total number of unprotected sex acts with steady partners, total number of unprotected sex acts with casual partners, total number of unprotected sex acts with anonymous sex partners, and number of STIs. All sexual risk variables were measured using the 2-month timeframe preceding baseline interview. Sexual compulsivity was significantly correlated with total number of HIV-negative or unknown serostatus partners, r(215)=.24, p < .01 and total unprotected sex with anonymous partners, r(118)=.21, p < .01. Sexual compulsivity was not related to the other sexual risk variables examined in this research.
Multivariate analyses
Regression of sexual compulsivity on drug and alcohol variables
Sexual compulsivity was regressed on the six drug and alcohol variables that were found to be significant in univariate analyses. Table 2 displays the regression results. As shown, greater use of methamphetamine before or during sex was associated with higher levels of sexual compulsivity. Binge use of methamphetamine was also significantly associated with higher levels of sexual compulsivity. Frequency of alcohol use, use of alcohol before and during sex, number of illicit drugs used, and injection use of methamphetamine during the past two months were not associated with sexual compulsivity in multivariate analyses.
Regression of sexual compulsivity on sexual venue variables
In univariate analyses, five sexual venue variables were associated with sexual compulsivity. The relationship between sexual compulsivity and sexual venues was examined further using multivariate analyses. As shown in Table 3, sexual compulsivity was regressed on five sexual venue variables. Two variables were statistically significant. The direction of regression coefficients indicated that participants who went to sex clubs and those who used street corners to find sex partners had significantly higher levels of sexual compulsivity.
Regression of sexual compulsivity on psychosocial variables
Table 4 displays the results of a multivariate analysis with sexual compulsivity regressed on the six psychosocial variables that were found to be significant in the univariate analysis. As shown, self-efficacy for condom use and global self-esteem were inversely related to sexual compulsivity. Social stigma and disinhibition were positively related to sexual compulsivity.
Regression of sexual compulsivity on sexual risk variables
As shown in Table 5, sexual compulsivity was regressed on two sexual risk variables that were significant in the univariate analyses. Number of HIV-negative or unknown serostatus partners was positively associated with sexual compulsivity.
Final regression model: sexual compulsivity regressed on drug and alcohol variables, sexual venue variables, psychosocial variables, and sexual risk variables
In this model, sexual compulsivity was regressed on all the variables that were significant in the four separate regression analyses described above. Independent variables were entered in four steps according to each category of variables, with age included in the equation. Correlations among independent variables in the final regression equation ranged from .01 to .32. Regression results are presented in Table 6. In step 1, two drug and alcohol use variables were entered into the regression equation along with age. All three variables were statistically significant. Age, use of meth before and during sex, and binge use of meth were positively associated with sexual compulsivity and together accounted for a significant 18% of the variance in sexual compulsivity. In step 2, two sexual venue variables were entered into the equation. Attending sex clubs and going to street corners to find sex partners were both significantly associated with sexual compulsivity in a positive direction. Sexual venue variables accounted for an additional 7% of total variance in the dependent variable. Older age, use of meth before or during sex, and binge use of meth remained significant at this step. In step 3, psychosocial variables were entered into the equation. All four variables were statistically significant and together accounted for 18% of total explained variance in sexual compulsivity. Self-efficacy for condom use and self-esteem were inversely related to sexual compulsivity, whereas social stigma and disinhibition were positively associated with sexual compulsivity. Binge use of meth was no longer a significant predictor at this step in the regression. In step 4, number of HIV-negative or unknown serostatus partners was entered into the regression equation. This variable was positively associated with sexual compulsivity and accounted for an additional 2% of explained variance. Thus, in the final regression model, higher levels of sexual compulsivity among HIV-positive meth-using gay and bisexual men were associated with older age, using meth before or during sex, going to sex clubs and street corners to find sex partners, having lower self-efficacy for condom use, having lower levels of self-esteem, being more disinhibited, and having a larger number of HIV-negative or unknown serostatus partners.
Discussion
This research examined the relationship between sexual compulsivity and sexual risk behavior in a sample of HIV-positive meth-using gay and bisexual men. We sought to characterize sexually compulsive meth-using gay and bisexual men by identifying specific demographic, contextual, social, sexual, and psychological correlates of sexual compulsivity. Our findings provide a preliminary understanding of the characteristics of HIV-positive, meth-using gay and bisexual men who score high on sexual compulsivity. This research is important because a growing number of HIV-positive individuals in the United States use meth, and sexual compulsivity may help to explain continued unsafe sexual practices among some men in the target population (Parsons et al., 2001).
Sexual compulsivity was evaluated using the SCS—a non-clinical instrument (Kalichman & Cain, 2004). An examination of the distribution of participants' scores on the SCS revealed considerable variability in terms of individual scores. Fifty-one percent of participants had scores below the midpoint of the possible range of SCS scores, thereby suggesting that a considerable percentage of the meth-using gay and bisexual men in our sample did not report uncontrollable sexual urges and preoccupation with sexual thoughts. Since this study did not have a comparison group of non-meth-using HIV-positive gay and bisexual men, we cannot make any definitive statements regarding the impact of meth use on the levels of sexual compulsivity reported in our sample. However, since other studies have used the SCS with HIV-positive gay and bisexual men, we can offer a preliminary comparison, with the important caveat that other samples are not directly comparable. At least one study has used the SCS with HIV-positive gay and bisexual men who were not meth users. Benotsch et al. (1999) reported that the mean score on the SCS in their sample was 1.87 (SD=.66). In comparison, the mean score on the SCS for our sample of meth-using HIV-positive gay and bisexual men was 2.4 (SD=.76). This comparison suggests that meth use may contribute to elevated levels of sexual compulsivity.
Univariate analyses of the relationship between sexual compulsivity and sexual risk behaviors revealed that higher scores on sexual compulsivity were significantly associated with having a larger number of HIV-negative or unknown serostatus partners and engaging in more unprotected sex with anonymous sex partners. These findings are consistent with previous research that has examined sexual compulsivity in relation to partner-specific sexual behaviors. Kalichman and Cain (2004) reported that high versus low sexual compulsivity groups were not different in terms of sexual behavior data with main partners; however, individuals with higher SCS scores had higher rates of unprotected sex with casual or one-time sex partners. Although we identified only two statistically significant relationships between sexual compulsivity and sexual risk, the specificity associated with our findings has implications for HIV prevention research, primarily because these two factors carry some of the highest levels of sexual risk. For the participant this entails a high risk for HIV re-infection or infection with another sexually transmitted disease, while the participant's sex partners are placed at high risk for HIV transmission by engaging in unprotected sex with an HIV-positive individual who has had multiple partners (Golden, Brewer, Kurth, Holmes, & Handsfield, 2004). Individuals who engage in the highest levels of risk may not be good candidates for standard sexual risk reduction interventions because, as suggested by Benotsch et al. (1999), individuals who score high on sexual compulsivity may be willing to accept risks that most others judge to be too high. Thus, intervention strategies that are effective with the majority of HIV-positive gay and bisexual men may not be effective with sexually compulsive individuals. This suggests the need for tailored interventions that address the relationship between sexual compulsivity and highly risky sexual behaviors.
Our final regression model yielded a number of substantive findings regarding the correlates of sexual compulsivity. One such factor was the age of the participant. In this study, age was positively associated with sexual compulsivity. This finding is in contrast to at least one other study, which found an inverse relationship between age and sexual compulsivity. Hyde and DeLamater (2004) have suggested that sexual compulsivity is a developmental phenomenon; that is, levels of sexual compulsivity are highest at younger ages when hormone levels that control sexual urges are high and subject to fluctuations. Our finding does not support a developmental or biological model of sexual compulsivity. If sexual compulsivity increases with age as revealed in our data, it would suggest that something other than biological forces are operative—perhaps social or personality factors. More research is needed to determine if the relationship between age and sexual compulsivity varies according to characteristics of the population.
Sexual compulsivity was also associated with greater use of meth before and during sex. This finding supports the work of others who have reported that use of substances (e.g., cocaine, alcohol) in sexual contexts was associated with higher levels of sexual compulsivity (Kalichman & Cain, 2004). In this research, it was not the amount or frequency of meth use that was associated with sexual compulsivity. Rather, the link between meth use and sexual compulsivity was specific to using meth (and thus being high) before or during a sexual encounter. This suggests that the stimulant quality of meth may exacerbate existing impulse control problems (Benotsch et al., 1999). Future research should examine whether meth use before or during sex is an underlying mechanism whereby sexual compulsivity affects sexual risk behavior.
Sexual venue was another variable that was associated with sexual compulsivity in the multivariate analyses. To date, very little research has focused on this contextual variable. In this research, adult bookstores and public parks were the most popular locations for seeking out sex partners. Approximately 43% of the sample sought partners in each of these locations. In contrast, less than 20% of the sample reported going to a public restroom, sex club, or street corner to find partners. Among those men who reported going to sex clubs and street corners to find sex partners, approximately 45% went to one location or the other; only 10% reported going to both locations during the previous two months. As reported in previous work, sex with anonymous partners in public settings, although dangerous and socially risky, is perceived as exciting and stimulating (Binson et al., 2001; Parsons & Halkitis, 2002; Semple, Grant, Zians, & Patterson, 2005). Sex clubs and street corners may also offer an environment of excitement and stimulation for the sexually compulsive individual. These environments may enhance the individual's sexual experiences. Researchers need a better understanding of the context of sexual encounters.
Our finding that self-esteem was inversely associated with sexual compulsivity is consistent with previous research. Parsons et al. (2001) reported that sexual compulsivity was associated with lower levels of self-confidence. Other studies have also reported an inverse relationship between sexual compulsivity and self-esteem (Kalichman & Rompa, 1995; Benotsch et al., 1999). Based on our clinic experience, we have learned that sexually compulsive individuals who have difficulty controlling sexual urges engage in behaviors that often make them feel ashamed or guilty after the fact. For example, an HIV-positive person who engages in unprotected sex with an anonymous partner may feel badly about the possibility of having infected another person, or he may feel guilty about having exposed himself to possible reinfection. If this behavior persists over time, it could chip away at the individual's sense of self-worth or self-esteem (Gruenewald, Kemeny, Aziz, & Fahey, 2004). Alternatively, persons with low self-esteem may give in to sexual urges because they do not value themselves or their health. Longitudinal data would be necessary to disentangle any causal relationship between sexual compulsivity and self-esteem.
Self-efficacy for condom use was also inversely related to sexual compulsivity. This finding was not surprising given that sexual compulsivity was associated with attendance at risky sexual venues and being under the influence of meth during sexual encounters. Both of these factors could contribute to the individual's perceived lack of ability or skill to use a condom with sex partners. Previous research has shown that self-efficacy for condom use can be enhanced by teaching drug users the skills to use condoms properly and by practicing and rehearsing this behavior through the use of roleplays (van Empelen et al., 2003). This finding indicates the importance of incorporating social cognitive strategies for enhancing self-efficacy in relation to condom use into the design of behavioral interventions for sexually compulsive meth-users.
Disinhibition was another characteristic of HIV-positive meth-using men who scored higher on our measure of sexual compulsivity. Previous research has documented an association between disinhibition and impulsivity (Acton, 2003). Although sexual compulsivity and impulsivity are purported to be distinct concepts (Acton, 2003), they may represent disorders on a broader spectrum of obsessive-compulsive disorders (Bancroft & Vukadinovic, 2004; Williams, 2005). If so, the hypothesized neurobiology of sexually compulsivity is that disruptions in monoamine transmitters (e.g., norepinephrine, dopamine, serotonin) can affect human sexual functioning and other aspects of human behavior, including impulsivity, compulsivity, and behavioral disinhibition (Williams, 2005). This perspective would suggest that treating symptoms with pharmacological drugs (e.g., serotonin enhancing drugs) could reduce symptoms of sexual compulsivity and disinhibition (i.e., the tendency to act without regard for consequences).
In the final regression analysis, we found a positive association between sexual compulsivity and number of HIV-negative or unknown serostatus partners in the previous two months. This finding may reflect the propensity of sexually compulsive meth users to engage in sex with anonymous partners whose serostatus is less likely to be known to the participant. More research is needed to disentangle the interrelationships among sexual compulsivity, partner type, and partner serostatus.
The findings from this exploratory study contribute to our understanding of sexual compulsivity in a sample of HIV-positive meth-using gay and bisexual men. We identified a subgroup of men who could be characterized as sexually compulsive, and we demonstrated a positive relationship between higher levels of compulsivity and sexually risky behaviors. In addition, we identified demographic, contextual, social, sexual, and psychological correlates of sexual compulsivity in this population. These findings will help to guide future research, and they provide a starting point for the development of behavioral interventions that target sexually compulsive HIV-positive meth-using gay and bisexual men.
However, despite these contributions, this research has a number of limitations that warrant discussion. Foremost, the findings are based on a convenience sample of HIV-positive, meth-using gay and bisexual men, and thus should not be considered representative of the population of interest. Study participants were also volunteers in a sexual risk reduction intervention. It is possible that those who volunteered were more concerned about their sexual risk behaviors, including uncontrollable sexual urges and preoccupations with sex. Because of the volunteer nature of the sample, we cannot generalize these findings to the more global population of HIV-positive meth-using gay and bisexual men.
Our data were also cross-sectional, which precludes drawing conclusions regarding causality among the variables examined in this study. For example, we cannot determine if sexual compulsivity leads to sexual risk behavior or if engaging in risky behavior makes a person more sexually compulsive. Longitudinal data are needed to disentangle causal relationships.
Another limitation is that sexual risk behavior and sexual compulsivity were self-reported. The socially sensitive nature of the sex questions may have resulted in some participants' underreporting their risk behaviors, while others may have exaggerated their behaviors or reported them inaccurately as a result of incomplete memories associated with meth-induced memory impairment. Participants may also have underreported sexual compulsivity because of the social stigma likely to be associated with the admission that one has uncontrollable sexual urges and a preoccupation with sex.
From a design perspective, this research is limited by the absence of a comparison group of HIV-positive non-meth-using gay and bisexual men. Without a comparison group, we cannot make statements regarding the role of meth as a contributing factor to variations in levels of sexual compulsivity.
It should also be stated that the SCS is not a diagnostic instrument. There are no cutpoints that would identify clinical levels of sexual compulsivity. However, there is a growing body of literature that has used the SCS and agrees that a score of 24 or greater is an adequate value for classifying individuals as high in sexual compulsivity (Benotsch et al., 1999; Parsons et al., 2001).
Finally, this research was exploratory. The results need further evaluation in larger and more representative sample of HIV-positive meth-using gay and bisexual men.
These findings suggest the need for specialized prevention interventions that address sexual compulsivity in relation to the sexual risk behaviors of HIV-positive, meth-using gay and bisexual men. Interventions should: (a) evaluate levels of sexually compulsivity; (b) address how sexually compulsivity impacts sexual risk behavior; and (c) offer strategies for controlling impulsive sexual urges and other behavioral indicators of sexual compulsivity. For example, behavioral self-management strategies would likely be an important element of a sexual risk reduction intervention for HIV-positive meth-using men who have high scores on sexual compulsivity. In addition to behavioral strategies, pharmacological treatments that have been used with obsessive-compulsive spectrum disorders might also be effective for treating sexually compulsive individuals (Gold & Heffner, 1998). The availability of varied treatment approaches suggests the importance of performing clinical assessments and diagnoses when high levels of sexual compulsivity are identified through use of non-clinical assessment tools such as the SCS. Lastly, our data support the work of Kalichman and Cain (2004), who advocate that interventions for sexually compulsive individuals should incorporate multi-faceted treatment approaches, including elements of substance abuse treatment, sexual risk reduction, and mental health.
References
Acton, G. S. (2003). Measurement of impulsivity in a hierarchical model of personality traits: Implications for substance use. Substance Use and Misuse, 38, 67–83.
Bancroft, J., & Vukadinovic, Z. (2004). Sexual addiction, sexual compulsivity, or what? Toward a theoretical model. Journal of Sex Research, 41, 225–234.
Beck, A. T. (1967). Depression: Clinical, Experimental and Theoretical Aspects. New York: Harper and Row.
Beck, A. T. (1976). Cognitive Therapy and Emotional Disorder. New York: Hoeber.
Benotsch, E. G., Kalichman, S. C., & Kelly, J. A. (1999). Sexual compulsivity and substance use in HIV-seropositive men who have sex with men: Prevalence and predictors of high risk behaviors. Addictive Behaviors, 24, 857–868.
Benotsch, E. G., Kalichman, S. C., & Pinkerton, S. D. (2001). Sexual compulsivity in HIV-positive men and women: Prevalence, predictors, and consequences of high-risk behaviors. Sexual Addiction and Compulsivity, 8, 83–99.
Binson, D., Woods, W., Pollack, L., Paul, J., Stall, R., & Catania, J. (2001). Differential HIV risk in bathhouses and public cruising areas. American Journal of Public Health, 91, 1482–1486.
Bucholz, K. K., Cadoret, R., Cloninger, R. D., Dinwiddie, S. H., Hesselbrock, V. M., Nurnberger, J. I., et al. (1994). A new semi-structured psychiatric interview for use in genetic linkage studies. A report on the reliability of the SSAGA. Journal of Studies on Alcohol, 55, 149–158.
Bucholz, K. K., Hesselbrock, V. M., Shayka, J. J., Nurnberger, J. I., Schuckit, M. A., Schmidt, I., et al. (1995). Reliability of individual diagnostic criterion items for psychoactive substance dependence and the impact on diagnosis. Journal of Studies on Alcohol, 56, 500–505.
Cohen, J., & Cohen, P. (1983). Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates.
Cooper, A., Scherer, C. R., Boies, S., & Gordon, B. (1999). Sexuality on the internet: From sexual exploration to pathological expression. Professional Psychology: Research and Practice, 30, 154–164.
Dodge, B., Reece, M., Cole, S. L., & Standfort, T. G. M. (2004). Sexual compulsivity among heterosexual college students. Journal of Sex Research, 41, 343–350.
Gold, S. N., & Heffner, C. L. (1998). Sexual addiction: Many conceptions, minimal data. Clinical Psychology Review, 18, 367–381.
Golden, M. R., Brewer, D. D., Kurth, A., Holmes, K. K., & Handsfield, H. H. (2004). United States: Importance of sex partner HIV status in HIV risk assessment among men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 36, 734–742.
Gruenewald, T. L., Kemeny, M. E., Aziz, N., & Fahey, J. L. (2004). Acute threat to the social self: shame, social self-esteem, and cortisol activity. Psychosomatic Medicine, 66, 915–924.
Halkitis, P. N., Fischgrund, B. N., & Parsons, J. T. (2005). Explanations for methamphetamine use among gay and bisexual men in New York City. Substance Use and Misuse, 40, 1331–1345.
Halkitis, P. N., Shrem, M. T., & Martin, F. W. (2005). Sexual behavior patterns of methamphetamine-using gay and bisexual men. Substance Use and Misuse, 40, 703–719.
Hyde, J. S., & DeLamater, J. D. (2004). Understanding human sexuality. Boston: McGraw-Hill Higher Education.
Kalichman, S. C., & Cain, D. (2004). The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. Journal of Sex Research, 41, 235–241.
Kalichman, S. C., Greenberg, J., & Abel, G. G. (1997). HIV-seropositive men who engage in high risk sexual behavior: Psychological characteristics and implications for prevention. AIDS Care, 9, 441–450.
Kalichman, S. C., Johnson, J. R., Adair, V., Rompa, D., Multhauf, K., & Kelly, J. A. (1994). Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. Journal of Personality Assessment, 62, 385–397.
Kalichman, S. C., & Rompa, D. (1995). Sexual sensation seeking and sexual compulsivity scales: Reliability, validity, and predicting HIV risk behavior. Journal of Personality Assessment, 65, 586–601.
Kalichman, S. C., & Rompa, D. (2001). The sexual compulsivity scale: Further development and use with HIV-positive persons. Journal of Personality Assessment, 76, 379–395.
Kurtz, S. P. (2005). Post-circuit blues: motivations and consequences of crystal meth use among gay men in Miami. AIDS and Behavior, 9, 63–72.
Nugent, W. R., & Thomas, J. W. (1993). Validation of a clinical measure of self-esteem. Research on Social Work Practice, 3, 191–207.
Parsons, J. T., Bimbi, D., & Halkitis, P. N. (2001). Sexual compulsivity among gay/bisexual male escorts who advertise on the internet. Sexual Addiction and Compulsivity, 8, 101–112.
Parsons, J. T. and Halkitis, P. N. (2002). Sexual and drug-using practices of HIV-positive men who frequent public and commercial sex environments. AIDS Care, 14, 815–826.
Reback, C. J. (1997). The social construction of a gay drug: Methamphetamine use among gay and bisexual males in Los Angeles. Executive Summary. City of Los Angeles: AIDS Coordinator.
Schilder, A. J., Lampinen, T. M., Miller, M. L., & Hogg, R. S. (2005). Crystal methamphetamine and ecstasy differ in relation to unsafe sex among young gay men. Canadian Journal of Public Health, 96, 340–343.
Semple, S. J., Grant, I., Zians, J., & Patterson, T. L. (2005). HIV-positive methamphetamine users: Psychosocial and behavioral factors associated with sexual venues. Unpublished manuscript, University of California, San Diego.
Semple, S. J., Patterson, T. L., & Grant, I. (2002). Motivations associated with methamphetamine use among HIV+ men who have sex with men. Journal of Substance Abuse Treatment, 22, 149–156.
Semple, S. J., Patterson, T. L., & Grant, I. (2004). The context of sexual risk behavior among heterosexual methamphetamine users. Addictive Behaviors, 29, 807–810.
Temoshok, L., & Nannis, E. D. (1992). Tri-Service Biopsychosocial Study Protocol. The Rockville, MD: Military Medical Consortium for Applied Retroviral Research.
van Empelen, P., Kok, G., van Kesteren, N. M., van den Borne, B., Bos, A. E., & Schaalma, H. P. (2003). Effective methods to change sex-risk among drug users: a review of psychological interventions. Social Science and Medicine, 57, 1593–1608.
Williams, M. (2005). Medication treatment for sexual compulsivity. Accessed from http://www.brainphysics.com/paraphilia.php on October 16, 2005.
Zuckerman, M. (1971). Dimensions of sensation seeking. Journal of Consulting and Clinical Psychology, 36, 45–52.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Semple, S.J., Zians, J., Grant, I. et al. Sexual Compulsivity in a Sample of HIV-Positive Methamphetamine-using Gay and Bisexual Men. AIDS Behav 10, 587–598 (2006). https://doi.org/10.1007/s10461-006-9127-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-006-9127-1