Abstract
Clinicians who teach are essential for the health workforce but require faculty development to improve their educational skills. Curricula for faculty development programs are often based on expert frameworks without consideration of the learning priorities as defined by clinical supervisors themselves. We sought to inform these curricula by highlighting clinical supervisors own requirements through answering the research question: what do clinical supervisors identify as relative strengths and areas for improvement in their teaching practice? This mixed methods study employed a modified version of the Maastricht Clinical Teaching Questionnaire (mMCTQ) which included free-text reflections. Descriptive statistics were calculated and content analysis was conducted on textual comments. 481 (49%) of 978 clinical supervisors submitted their mMCTQs and associated reflections for the research study. Clinical supervisors self-identified relatively strong capability with interpersonal skills or attributes and indicated least capability with assisting learners to explore strengths, weaknesses and learning goals. The qualitative category ‘establishing relationships’ was the most reported strength with 224 responses. The qualitative category ‘feedback’ was the most reported area for improvement, with 151 responses. Key areas for curricular focus include: improving feedback practices; stimulating reflective and agentic learning; and managing the logistics of a clinical education environment. Clinical supervisors’ self-identified needs provide a foundation for designing engaging and relevant faculty development programs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The role of experienced clinicians in developing the future health workforce is significant and well recognised. The term ‘clinical supervision’ is often used as the role involves both oversight of patient care and trainee development activities (Fitzpatrick et al. 2012; Strand et al. 2015). Development of junior staff is linked to effective clinical supervision (de Jong et al. 2013; Kilminster and Jolly 2000). It is consequently important that clinical supervisors have skills in teaching in addition to clinical expertise. This paper focusses upon clinical supervisors’ teaching role, with the acknowledgement that this is inextricably linked with patient care.
The teaching role is sometimes uncomfortable for clinical supervisors. As one doctor noted in a 2015 qualitative study of clinical supervisors (Strand et al. 2015): I have not been educated to be a teacher, nor do I have any knowledge and interest in being a teacher …Most importantly, I have no pedagogic training at all… Clinical supervisors report the need for programs to assist in their development of education skills (Andrews and Ford 2013; Henderson and Eaton 2013; Neville and French 1991) although without specific detail regarding what they wish to learn.
We use the term ‘faculty development’ to describe programs which develop the educational proficiency of clinicians (O’Sullivan and Irby 2011; Steinert et al. 2006). There is a broad sweep of faculty development programs ranging from the short workshop to year long fellowships, which teach clinical supervisors how to teach. A 2016 systematic review indicates the value of such programs, including observed changes to teaching and some evidence that stand alone workshops in teaching can have an impact. Faculty development curricula included in this review are diverse and cover teaching performance, principles of teaching, specific teaching skills, assessment, educational design, leadership and scholarship (Steinert et al. 2016). A 2013 systematic review of medical faculty development programs noted a “move away from a focus on teaching performance alone” (Leslie et al. 2013) but this may not hold true for other professions. The type of topics included within faculty development curricula are well illustrated by the Stanford Faculty Development program, which includes: “learning climate, control of session, communication of goals, promotion of understanding and retention, evaluation, feedback and promotion of self-directed learning” (Johansson et al. 2009).
Faculty development curricula are predicated on a broad understanding as to what constitutes effective clinical teaching. They draw from diverse frameworks, scales and standards that articulate the teaching skills and attributes of excellent clinical supervisors (McLean et al. 2008). In 2001, Hesketh et al. proposed 101 specific learning outcomes for clinical supervisors. More recently, Staljmeier et al. (2010) drew from cognitive apprenticeship theories to develop a framework for clinical teaching excellence, which also serves as an assessment instrument. The Maastricht Clinical Teaching Questionnaire (MCTQ) contains 24 items within seven categories of a supervisor’s role: modelling appropriate behaviour, coaching students, scaffolding concepts, articulation of practice, encouraging reflection, exploration of goals and boundaries, and providing a general learning climate conducive to learning. In nursing and allied health, the Manchester Clinical Supervision Scale (MCCS) (Winstanley and White 2011) is designed to rate the value of “facilitated reflective discussion” within the workplace, highlighting the supervisory rather than the educative component of clinical supervision. Simultaneously, various institutional and national standards for educators have been published, such as the professional standards for medical, dental and veterinary educators published by the Academy of Medical Educators (AoME) (2014). These and similar provide implicit and explicit guidance to faculty development curricula.
These standards and frameworks are largely derived from expert practices such as consultation (Fluit et al. 2010; Hesketh et al. 2001; Molenaar et al. 2009; Stalmeijer et al. 2010), literature review (Fluit et al. 2010; Hesketh et al. 2001), theoretical frameworks (Fluit et al. 2010; Stalmeijer et al. 2010) and observations (Fluit et al. 2010). They provide clear aspirational direction and describe the expectations of an educational expert. However, these frameworks provide less information about the priorities and needs of the working clinical supervisor, who is keen to teach but whose primary focus is patient care and who may have little training in education principles.
O’Sullivan and Irby (2011) identify assessing the learning needs of workplaces with respect to clinical supervision as an important area for further research. It would be illuminating for faculty developers to know which facets of teaching that clinical supervisors wish to focus on or find most troublesome. This aligns with the key tenet of constructivist approach to education, which suggests that an understanding of the learners’ circumstances is necessary for effective engagement and development (Dennick 2012). Knowing supervisors’ self-perceived strengths and weaknesses promotes a learner-centred approach to program development. Furthermore, as faculty development initiatives typically constitute a single session workshop (Steinert et al. 2006), it makes sense for faculty development programs to engage learners through targeting perceived areas of greatest need.
To the best of our knowledge, there is little literature which empirically identifies the learning needs of the target audience of typical clinical supervisors from their own perspectives. This paper addresses this gap through focusing on identifying ‘on the ground’ priorities for clinical supervisors. We are aware of the limitations of self-report data, in particular it can be widely divergent from actual practice (Norman 2014). However, self-report data indicates how ‘on the ground’ clinical supervisors themselves prioritise areas for improvement. In this way, it is more closely aligned with a pedagogic strategy purpose of self-report data rather than self-assessment ability (Eva and Regehr 2008). Furthermore, self-assessment is generally concerned with comparison of self to a standard (Boud and Falchikov 1989). In this instance, the standard of performance is not the focus here, but a qualitative sense of the supervisors’ perceptions of their relative priorities.
The overall aim of this study is to identify foci for future faculty development in clinical teaching. Our research question was: what do clinical supervisors identify as relative strengths and areas for improvement in their teaching practice?
Methods
Context
Participants were given the opportunity to complete the MCTQ as part of a 4 h interprofessional and multi-institutional workshop program, called Clinical Supervision Support across Contexts (ClinSACC) (Tai et al. 2015). This program, which was funded by the Victorian Department of Health, ran from March 2012 to September 2013. There were 70 workshops, which ran regularly across this period.
Sample
978 clinical supervisors from acute and community settings in a broad geographical area within a metropolitan city in Australia were invited to participate in the research.
Instrument
The MCTQ was initially used as feedback tool for clinical supervisors from students (Stalmeijer et al. 2010). Each item is assessed with 5-point Likert scale where 1 = fully disagree, 5 = fully agree). There is an overall rating score, and space for open text comments. Several studies suggest the MCTQ may be reliable and valid as a feedback tool (Boerboom et al. 2011a; Stalmeijer et al. 2008, 2010) and it has been used as a self-assessment instrument for veterinary clinical teachers (Boerboom et al. 2011b).
The MCTQ was reworded to make it a self-report, self-evaluation tool (modified or mMCTQ) intended for a personal learning needs analysis. Two open-ended questions were included, on participants’ perceived strengths, and areas for improvement. In addition, to the research purpose of providing data regarding the self-perceived learning needs of clinical supervisors, the mMCTQ also served as a reflective tool for the participants.
Data collection
Workshop participants completed a paper version of the mMCTQ as part of a reflective activity identifying their own learning needs, after orientation to the fundamental ideas of clinical supervision and a short introduction to reflective practice. They were invited to participate in the research component of the program by the workshop facilitator. Written consent was obtained. Participants submitted mMCTQs into the study across all months of the study except March and April 2012 and April 2013. Quantitative data were entered into an Excel spreadsheet, whilst qualitative responses were photocopied for coding.
Data analysis
Descriptive statistics were calculated for the mMCTQ items. As the focus of this study was on relative identified needs rather than self-assessment domains, items were ranked from highest score (highest belief in capability) to lowest score (lowest belief in capability).
The responses to the two open-ended questions on clinical supervision strengths and areas for improvement were qualitatively analysed using content analysis techniques (Vaismoradi et al. 2013), described as follows: Three researchers (FK, MB, JT) each inductively coded the same 100 responses (45 strengths; 55 areas of improvement) to develop a coding framework based on the manifest content of the statements. A single statement could be coded multiple times. All responses were then coded (DN, FK, MB, JT) using the framework. Uncertainties were discussed and the final framework resolved by consensus (JT, FK, MB).
Ethics
Human research ethics approval was gained from Monash University (project CF12/1064—2012000510) and Monash Health (12168L).
Results
A total of 481 (49%) workshop participants consented for their mMCTQ data to be used in the study. Professions are detailed in Table 1. While 103 (21%) reported no prior professional development, 203 (43%) had attended basic workshops or in-service training, with smaller numbers having had extensive informal training (64, 14%) or a further qualification (86, 18%).
Individual mMCTQ item means ranged from 3.50 to 4.64 and are presented in Table 2 from most frequently to least frequently performed as self-reported on the mMTCQ.
The coding framework, codes and frequency counts for the qualitative analysis of the free text data are provided in Table 3. The most reported strength, with 224 responses, was the category of ‘establishing relationships’, which included rapport building, approachability and friendliness. ‘Assessment’ was the least cited strength and the only category not identified by any respondent. Illustrative quotes describing the five most frequently reported strengths are provided in Table 4.
The most reported area for improvement, with 151 responses, was ‘feedback’. The least reported area for improvement was the theme of being ‘respectful,’ which was not identified by any respondent. Illustrative quotes describing the most frequently reported areas for improvement are provided in Table 5.
Discussion
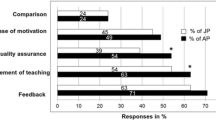
This large scale investigation of clinical supervisors' self-assessed strengths and weaknesses addresses calls for research into workplace learning needs (O’Sullivan and Irby 2011). The three most frequently performed aspects of clinical teaching identified in the mMCTQ were largely interpersonal skills or attributes, such as showing respect or interest or creating a safe environment. The four and fifth aspects most frequently identified in the mMCTQ concerned encouragement to ask questions or learn new things. The top five strengths identified in the qualitative data were: establishing relationships, clinical expertise, communication skills, enthusiasm and other individual attributes such as honesty or tact. Overall, 54% of participants nominated interpersonal skills or attributes as their strengths and 17% of free text comments specifically identified relationship building as a key strength.
Four of the five least frequently performed areas identified in the mMCTQ were prompting learners to identify and explore their strengths, weaknesses and learning goals. In addition, respondents nominated ‘taking sufficient time’ as an area of relative weakness. The top three areas for improvement identified in the qualitative data included: giving feedback, promoting reflection and insight, and developing a range of teaching strategies. Other identified areas for improvement included undertaking further skills development and considering the structure and organization of the teaching session. Overall, 49% of participants nominated some form of teaching strategy as an area for improvement and 15% specifically identified feedback as an area of focus.
This research was intended to illuminate ‘on the ground’ perspectives and priorities of clinical supervisors. The mMCTQ and the free-text data both highlight self-perceived relative strengths in interpersonal skills and attributes. It is heartening that respondents recognized the significance of relationship building skills in their clinical teaching. Kilminster and Jolly (2000) identified these type of skills or qualities as contributing to effective supervision. Frameworks in clinical education often encompass the interpersonal dimension. For example, Hesketh et al’s model (2001) includes learning outcomes such as “enthusiasm”, “empathy and interest in learners” and “respect for student” and the MCCS presents items such as: “I can discuss sensitive issues encountered during my clinical casework with my supervisor” (Winstanley and White 2011). This suggests that the importance of the interpersonal relationship in clinical education, noted previously (Clement et al. 2016) and may well be a valuable explicit point for discussing strengths and limitations of a relational approach to clinical supervision.
Interpersonal skills are also hallmarks of effective and professional clinical practice. One perceived strength which did not have an interpersonal aspect was ‘clinical expertise’. Taken together, we suggest that respondents are most confident in skills that they practice daily as part of their primary role as a health professional. It makes sense to draw from one form of expertise to build another. Faculty development programs may find value in allowing clinical supervisors exploring these two distinctive roles—clinical practice and teaching practice—and how they overlap or diverge.
Clinical supervisors also described convergent priorities for development. The mMCTQ and free-text data identifies three broad areas for improvement: (1) feedback (2) promoting learners’ explorations of their own strengths and weaknesses and (3) logistical issues such as time management and planning. These will be discussed in turn.
It is not surprising that clinical supervisors wish to develop their feedback practices, with many wanting to improve delivery of ‘constructive’ or ‘negative’ messages. This discomfort in revealing learner deficits as part of the feedback encounter is commonly noted with supervisors undertaking avoidant behaviours such as incomplete or ‘vanishing’ (Ende 1983) performance information to protect the feelings of the learner. Teaching feedback skills is generally present in curricula and most expert frameworks mention ‘feedback’ (Academy of Medical Educators 2014; Stalmeijer et al. 2010) or related such as ‘counsel’ (Hesketh et al. 2001) or ‘guidance’ (Winstanley and White 2011). There are three points that are useful here. Firstly, faculty development which specifically targets feedback may be a way of motivating and engaging busy health care professionals. Secondly, providing feedback in challenging situations may cause dissonance with the perceived humanistic and interpersonal strengths, and this may be worth explicit exploration. Finally, general conceptions of feedback have shifted enormously in the last 5 years or so, from information provision to a dialogic approach which facilitates learner reflection and insight (Ajjawi and Boud 2015). Teaching feedback skills has now developed beyond providing information on performance gaps (Ende 1983), it has become a significant teaching strategy in its own right (Boud and Molloy 2013).
The mMCTQ and the free-text data indicated that clinical supervisors felt they had least capacity around promoting reflective practice or similar activities. In contrast to the self-identified strengths of interpersonal skills, prompting reflective practice does not align well with many clinical roles. This may mean that the clinical supervisors are challenged by letting students take responsibility for their own learning. This is illustrated by comparing the most frequently performed items of the mMCTQ—“I show respect to the students”, “I am genuinely interested in the students” and “I create a safe learning environment”—with the least frequently = “I stimulate students to explore their strengths and weaknesses”, “I stimulate students to consider how they could improve their strengths and weaknesses” and “I encourage students to formulate learning goals”. The former positions the educator as the teacher who bestows respect, interest and safety, while the latter positions the learners as responsible for their own learning.
Promoting independent learning requires a toolbox of specific teaching strategies, including feedback. These may feel foreign to working clinicians, as is indicated by the 49% who nominated this as an area for improvement. This lack of comfort is supported by previous studies of clinical educators working with underperforming learners where ‘more of the same’ is a common remediation strategy (Bearman et al. 2013; Cleland et al. 2013). Only a very few of our sample reported strengths in specific teaching strategies, such as ‘scaffolding’ and ‘observation’ and these tended to be teacher-driven. Other more learner-centred techniques—such as dialogic feedback, peer learning, role-play and self or peer assessment—were unidentified. While frameworks and curricula acknowledge the importance of reflective practice (Academy of Medical Educators 2014; Winstanley and White 2011) or self-directed learning (Johansson et al. 2009), it is unknown what learner-centred teaching strategies are provided within faculty development curricula. This study suggests that specific focus on practical learner-centred techniques may be very beneficial to clinical supervisors.
The reported challenge of logistics is a key finding with implications for both faculty development programs and expert frameworks. Some frameworks do not specifically target the capacity to navigate these types of competing demands (Hesketh et al. 2001), others make implicit mention of it (Academy of Medical Educators 2014; Stalmeijer et al. 2010) and others focus on it (Winstanley and White 2011). Logistical concerns such as structuring a placement, allocation of teaching time and orientation to the placement environment together comprised 14% of free-text comments describing areas for improvement. Similarly ‘taking time to teach’ was rated as an area of least capability. While it may seem easy to brush off as a problem that is not related to education, this does not take account of the real challenges faced by clinical supervisors juggling complex service roles as well as teaching duties. As Steinert et al. (2016) note in their recent review, “the majority of faculty development interventions targeted practicing clinicians”. Of all the findings, this indicates the biggest gap between expert frameworks and the views of clinical supervisors and is a useful reminder that ‘on the ground’ priorities can markedly differ from expert ones.
There are often no easy answers in managing complex situations such as competing demands within limited time. Faculty development workshops can acknowledge the challenges presented by departmental and institutional constraints. Prompting clinical supervisors to specifically address their logistics may be beneficial. This may require orientation to thinking about placements as a whole, rather than only focusing on the micro-skills of the interpersonal exchange. For example, if clinical supervisors prepare learners in establishing and articulating expectations at the beginning of the placement (i.e. the purpose behind processes), then this may assist in optimizing use of available time.
Finally, it is worth noting ‘assessment of learning’ was barely mentioned. This may be a response to the orientation provided by the MCTQ, however we wonder if clinical supervisors, faculty developers and medical education experts see assessment and facilitating learning as being separate endeavors. Certainly they are frequently indicated as separate domains (Academy of Medical Educators 2014). However, we suggest that assessment, or making judgements about students’ work is often inextricably linked to feedback and hence facilitating learning. We suggest that promoting judgements about work within learning may be a practical means of introducing ‘assessment for learning’ (Schuwirth and van der Vleuten 2011).
Strengths, limitations and future research
The data set in this study is drawn from a relatively large number of clinical supervisors from many professional groups, practice settings and institutions. The commonality of qualitative themes is notable, and more remarkable for the diverse group of respondents. Future research is needed to provide insight into the nuances of specific learning needs of particular professional groups and practice settings. This may be particularly important around promoting management of the logistics of teaching. It may be valuable to consider specific case studies of excellent ‘on the ground’ educators, to see how they manage clinical education within local constraints.
The limitations associated with the data assist with understanding its future applications. Clinical supervisors were participating in a faculty development workshop, which implies a stronger level of interest in our sample than in the general population. While participants were present as part of their work roles and often were elected by their workplaces to attend, it is fair to say this sample represents the more willing clinical supervisors, with an interest in education. Additionally, just over half of the workshop participants agreed to release their data for research purposes and any systematic reasons for refusal are not known.
There are limitations surrounding the use of the mMCTQ. Reporting of relatively ranked items is not aligned with its original purpose as a scale although this is mitigated by interpretation as qualitative trends rather than statistical manipulation. The mMCTQ and introductory materials provided orientation to some of the notions of clinical supervision which may have ‘primed’ certain responses; however this also means that respondents had a broad introduction to the general domain. Finally, all clinical supervisors were drawn from a single geographical location and so the sample may not represent international trends. A future multinational study would provide a more global perspective.
Conclusions
This research provides a broad empirical sample of what clinical supervisors think they need or are lacking in when it comes to teaching practice in the workplace. The areas where supervisors feel most adept are those aspects of practice which are associated with clinical expertise. The areas where supervisors wish most for development are those aspects of practice least aligned with their clinical roles, particularly teaching strategies to assist learners to take responsibility for their own learning.
Overall, the data provide a helpful counterpoint to clinical teaching frameworks. While the MCTQ and similar instruments provides a comprehensive understanding of the constituent parts of expert clinical teaching, the learning needs analysis orients us to what clinical supervisors may find most helpful. The short list is: feedback skills, teaching strategies which promote learner agency and managing the logistics of clinical teaching. This provides direction and focus for those setting the faculty development agenda.
References
Academy of Medical Educators, Professional Standards. (2014). http://www.medicaleducators.org/write/MediaManager/AOME_Professional_Standards_2014.pdf. Retrieved 16 March 2017.
Ajjawi, R., & Boud, D. (2015). Researching feedback dialogue: An interactional analysis approach. Assessment and Evaluation in Higher Education, 1–14. doi: 10.1080/02602938.2015.1102863.
Andrews, C. E., & Ford, K. (2013). Clinical facilitator learning and development needs: Exploring the why, what and how. Nurse Education in Practice, 13, 413–417. doi:10.1016/j.nepr.2013.01.002.
Bearman, M., Molloy, E., Ajjawi, R., & Keating, J. (2013). ‘Is there a Plan B?’ Clinical educators supporting underperforming students in practice settings. Teaching in Higher Education, 18, 531–544. doi:10.1080/13562517.2012.752732.
Boerboom, T. B. B., Dolmans, D. H. J. M., Jaarsma, A. D. C., Muijtjens, A. M. M., Van Beukelen, P., & Scherpbier, A. J. J. A. (2011a). Exploring the validity and reliability of a questionnaire for evaluating veterinary clinical teachers’ supervisory skills during clinical rotations. Medical Teacher, 33, e84–e91. doi:10.3109/0142159X.2011.536277.
Boerboom, T. B. B., Jaarsma, D., Dolmans, D. H. J. M., Scherpbier, A. J. J. A., Mastenbroek, N. J. J. M., & Van Beukelen, P. (2011b). Peer group reflection helps clinical teachers to critically reflect on their teaching. Medical Teacher, 33, e615–e623. doi:10.3109/0142159X.2011.610840.
Boud, D., & Falchikov, N. (1989). Quantitative studies of student self-assessment in higher education: A critical analysis of findings. Higher Education, 18, 529–549. doi:10.1007/bf00138746.
Boud, D., & Molloy, E. (2013). Rethinking models of feedback for learning: The challenge of design. Assessment and Evaluation in Higher Education, 38, 698–712. doi:10.1080/02602938.2012.691462.
Cleland, J., Leggett, H., Sandars, J., Costa, M. J., Patel, R., & Moffat, M. (2013). The remediation challenge: Theoretical and methodological insights from a systematic review. Medical Education, 47, 242–251. doi:10.1111/medu.12052.
Clement, T., Brown, J., Morrison, J., & Nestel, D. (2016). Ad hoc supervision of general practice registrars as a ‘community of practice’: Analysis, interpretation and re-presentation. Advances in Health Sciences Education, 21, 415–437. doi:10.1007/s10459-015-9639-4.
de Jong, J., Visser, M., Van Dijk, N., van der Vleuten, C., & Wieringa-de Waard, M. (2013). A systematic review of the relationship between patient mix and learning in work-based clinical settings. A BEME systematic review: BEME Guide No. 24. Medical Teacher, 35, e1181–e1196. doi:10.3109/0142159X.2013.797570.
Dennick, R. (2012). Twelve tips for incorporating educational theory into teaching practices. Medical Teacher, 34, 618–624. doi:10.3109/0142159X.2012.668244.
Ende, J. (1983). FEedback in clinical medical education. JAMA, 250, 777–781. doi:10.1001/jama.1983.03340060055026.
Eva, K. W., & Regehr, G. (2008). “I’ll never play professional football” and other fallacies of self-assessment. Journal of Continuing Education in the Health Professions, 28, 14–19. doi:10.1002/chp.150.
Fitzpatrick, S., Smith, M., & Wilding, C. (2012). Quality allied health clinical supervision policy in Australia: a literature review. Australian Health Review, 36, 461–465. doi:10.1071/AH11053.
Fluit, C. R. M. G., Bolhuis, S., Grol, R., Laan, R., & Wensing, M. (2010). Assessing the quality of clinical teachers. Journal of General Internal Medicine, 25, 1337–1345. doi:10.1007/s11606-010-1458-y.
Henderson, A., & Eaton, E. (2013). Assisting nurses to facilitate student and new graduate learning in practice settings: What ‘support’ do nurses at the bedside need? Nurse Education in Practice, 13, 197–201. doi:10.1016/j.nepr.2012.09.005.
Hesketh, E. A., Bagnall, G., Buckley, E. G., Friedman, M., Goodall, E., Harden, R. M., et al. (2001). A framework for developing excellence as a clinical educator. Medical Education, 35, 555–564. doi:10.1046/j.1365-2923.2001.00920.x.
Johansson, J., Skeff, K., & Stratos, G. (2009). Clinical teaching improvement: The transportability of the Stanford Faculty Development Program. Medical Teacher, 31, e377–e382. doi:10.1080/01421590802638055.
Kilminster, S. M., & Jolly, B. C. (2000). Effective supervision in clinical practice settings: A literature review. Medical Education, 34, 827–840. doi:10.1046/j.1365-2923.2000.00758.x.
Leslie, K., Baker, L., Egan-Lee, E., Esdaile, M., & Reeves, S. (2013). Advancing Faculty Development in Medical Education: A systematic review. Academic Medicine, 88, 1038–1045. doi:10.1097/ACM.0b013e318294fd29.
McLean, M., Cilliers, F., & Van Wyk, J. M. (2008). Faculty development: Yesterday, today and tomorrow. Medical Teacher, 30, 555–584. doi:10.1080/01421590802109834.
Molenaar, W. M., Zanting, A., van Beukelen, P., de Grave, W., Baane, J. A., Bustraan, J. A., et al. (2009). A framework of teaching competencies across the medical education continuum. Medical Teacher, 31, 390–396. doi:10.1080/01421590902845881.
Neville, S., & French, S. (1991). Clinical education: Students’ and clinical tutors’ views. Physiotherapy, 77, 351–354. doi:10.1016/S0031-9406(10)61803-2.
Norman, G. (2014). Data dredging, salami-slicing, and other successful strategies to ensure rejection: Twelve tips on how to not get your paper published. Advances in Health Sciences Education, 19, 1–5.
O’Sullivan, P. S. E., & Irby, D. M. P. (2011). Reframing Research on Faculty Development. Academic Medicine, 86, 421–428.
Schuwirth, L., & van der Vleuten, C. (2011). Programmatic assessment: From assessment of learning to assessment for learning. Medical Teacher, 33, 478–485.
Stalmeijer, R. E., Dolmans, D. H. J. M., Wolfhagen, I. H. A. P., Muijtjens, A. M. M., & Scherpbier, A. J. J. A. (2008). The development of an instrument for evaluating clinical teachers: Involving stakeholders to determine content validity. Medical Teacher, 30, e272–e277. doi:10.1080/01421590802258904.
Stalmeijer, R. E., Dolmans, D. H. J. M., Wolfhagen, I. H. A. P., Muijtjens, A. M. M., & Scherpbier, A. J. J. A. (2010). The Maastricht Clinical Teaching Questionnaire (MCTQ) as a valid and reliable instrument for the evaluation of clinical teachers. Academic Medicine, 85, 1732–1738. doi:10.1097/ACM.0b013e3181f554d6.
Steinert, Y., Mann, K., Anderson, B., Barnett, B. M., Centeno, A., Naismith, L., et al. (2016). A systematic review of faculty development initiatives designed to enhance teaching effectiveness: A 10-year update—BEME Guide No. 40. Medical Teacher, 38, 769–786. doi:10.1080/0142159X.2016.1181851.
Steinert, Y., Mann, K., Centeno, A., Dolmans, D., Spencer, J., Gelula, M., et al. (2006). A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Medical Teacher, 28, 497–526. doi:10.1080/01421590600902976.
Strand, P., Edgren, G., Borna, P., Lindgren, S., Wichmann-Hansen, G., & Stalmeijer, R. (2015). Conceptions of how a learning or teaching curriculum, workplace culture and agency of individuals shape medical student learning and supervisory practices in the clinical workplace. Advances in Health Sciences Education, 20, 531–557. doi:10.1007/s10459-014-9546-0.
Tai, J., Bearman, M., Edouard, V., Kent, F., Nestel, D., & Molloy, E. (2015). Clinical supervision training across contexts. The Clinical Teacher. doi:10.1111/tct.12432.
Vaismoradi, M., Turunen, H., & Bondas, T. (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing and Health Sciences, 15, 398–405. doi:10.1111/nhs.12048.
Winstanley, J., & White, E. (2011). The MCSS-26©: Revision of the Manchester Clinical Supervision Scale© Using the Rasch Measurement Model. Journal of Nursing Measurement, 19, 160–178. doi:10.1891/1061-3749.19.3.160.
Acknowledgements
The Clinical Supervision Support across Contexts program was supported by the Victorian Government. We would like to acknowledge Dr. Rola Ajjawi for her helpful feedback on earlier versions of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bearman, M., Tai, J., Kent, F. et al. What should we teach the teachers? Identifying the learning priorities of clinical supervisors. Adv in Health Sci Educ 23, 29–41 (2018). https://doi.org/10.1007/s10459-017-9772-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-017-9772-3