Abstract
The ability to guide one’s own learning is an essential skill for the health professional. The apprenticeship model of undergraduate education offers an opportunity to engage in self-regulated learning as students work to set goals, evaluate the available opportunities and seek out those with the greatest potential for learning. A close examination of how students navigate their clinical rotations could therefore foster greater understanding of how students learn to guide their own learning. The study presented here aimed to examine undergraduate medical students’ day-to-day learning strategies in order to better understand the process of informal self-regulated learning in practice. As a secondary objective, we sought to provide a forum for students to share and critically reflect on their own self-regulated learning strategies. A series of focus groups were conducted with medical students on a surgical rotation. Participants were asked to discuss issues relating to the strategies and behaviours that they had implemented in order to maximize their educational experience. Three distinct approaches to informal self-regulated learning were identified: Participants articulated tendencies to acquiesce to a perceived lack of learning opportunities choose from available learning opportunities and create their own learning opportunities. The results are interpreted through the lens of self-regulated learning theory and implications for medical education are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The ability to guide one’s own learning is an essential skill in the training of a health professional. Successful clinicians must be able to continually adapt, change and learn in practice. Ideally, this ability to self-regulate learning should be continually refined as a student progresses from undergraduate to postgraduate education before finally entering clinical practice. Regulatory bodies such as the Royal College of Physicians and Surgeons of Canada and the Accreditation Council for Graduate Medical Education have included the concept of self-regulated learning in defining and articulating the non-medical knowledge competencies expected of a medical expert (Frank 2005).
In recent years, there has been a considerable increase in research and interest in self-regulated learning. Borrowing from the educational psychology literature, self-regulated learning may be defined as a recursive, dynamic, and active process which requires students to make decisions about task-orchestrating actions (e.g., selecting resources, making plans, etc.), about how to self-monitor learning progress, about adjusting plans and strategies when necessary, about managing motivation and emotions, and ultimately about how to self-evaluate performance (Butler 2002). Critically, learners make their decisions in a social context that involves interacting with peers and other colleagues; thus self-regulated learning should not be viewed as an entirely independent activity (Butler et al. 2008). The literature on education in the health professions now includes examples of students developing technical skills without the assistance of an expert facilitator (Nousiainen et al. 2008); curricular interventions designed to encourage students to identify and explicitly articulate their own learning objectives (Bravata et al. 2003); and attempts to evaluate self-directed learning activities (Evensen et al. 2001). However, our current understanding of self-regulated learning might be severely limited by the exclusion of at least one key issue.
The majority of studies aimed at examining how students learn to effectively regulate their own learning have focused on formal attempts at self-regulated learning, such as the introduction of educational interventions to encourage self-regulated initiatives or changes to curricular requirements that allow students more freedom in course selection (Murad and Varkey 2008). While these are important contributions to the field and can inform our understanding, the identification and exploration of informal self-regulated learning has been largely ignored. This would include attempts by students and clinicians to make their own decisions regarding their learning that are not directly mandated or structured by any administrative, academic or professional body. We would argue that self-regulated learning is a competency that permeates all aspects of practice and as such, it is applicable in all contexts. While health professions education necessarily includes formal components of training, students’ self-regulated learning in informal settings must not be overlooked.
The apprenticeship model that characterizes most medical training requires that much of the day-to-day informal learning take place in hospital wards, clinics and operating rooms. Students are typically required to complete some service to the hospital while simultaneously acquiring the skills and knowledge needed for future practice. As third- and forth- year students work to maintain a balance between service delivery and education, their daily activities become an exercise in self-regulated learning. Much like the practicing clinician, the medical student must set goals, evaluate the available opportunities and seek out those with the greatest potential for learning. A close examination of how students navigate their clinical rotations could therefore foster greater understanding of how students learn to guide their own learning and choose the events, opportunities and experiences that will help them evolve as lifelong learners.
Following this line of inquiry, our primary study objective was to directly examine undergraduate medical students’ day-to-day learning strategies in order to better understand the process of informal self-regulated learning in practice. Our secondary study objective stemmed from our role as educators rather than researchers. We sought to provide a forum for students to share and critically reflect on their own self-regulated learning strategies. Research has highlighted the importance of fostering a sense of responsibility for learning and a general attitude of self-control and inherent power in students (Scardamalia and Bereiter 2003; Schunk and Zimmerman 2001; Zimmerman 1989). However, in the context of undergraduate medical education, the subordinate nature of the students’ role has been shown to lead students to overlook and undervalue their capacity to adapt their activities in the context of every day learning (Mylopoulos and Regehr 2009). Thus, although the most common systems of medical education may set the stage for students to engage in informal self-regulated learning as early as the third year of medical school, the extent to which students recognize the value and importance of this form of engagement while on a clinical rotation remains in doubt. As we continue to explore the nature of informal self-regulated learning, our ultimate goal as educators will be to foster students’ engagement in informal self-regulation as a vital part of their development into lifelong learners.
Methods
Setting
This research took place over an 11-month period in the undergraduate medical education program in the Department of Surgery, at a large, urban Canadian University and its affiliated teaching hospitals.
Participants
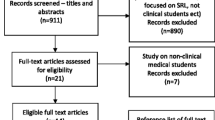
313 medical students enrolled in their third and fourth years of medical training participated in the study. During their third and fourth years of training (‘the clerkship’), medical students rotate through different medical specialties (‘rotations’) in six-week periods. We employed a purposive criterion sampling strategy (Patton 1990), narrowing our recruitment to include only medical students who had just completed their surgery rotation at each of the three hospitals affiliated with the undergraduate program in the Department of Surgery.
Data collection
At the end of each six-week surgery rotation, the Department of Surgery traditionally holds mandatory 45 min debriefing sessions, asking students to discuss their experiences with their clinical teachers (staff surgeons and residents in the Department of Surgery) and identify areas of improvement for surgical clerkship rotations. After receiving approval from the university’s Research Ethics Board, we invited students to voluntarily stay for an additional 45 min focus group session at the end of this mandatory debriefing session. To address the primary study objective of understanding informal self-regulated learning, participants in the focus groups were asked to discuss issues relating to the strategies and behaviours that they had implemented in order to maximize their educational experience. In total we conducted 21 focus groups over the 11-month course of the study. While qualitative research guidelines suggest that saturation can be achieved after 6-8 sampling units (Kuzel 1999), because the second objective of our project was to ensure that all students were provided with the opportunity to participate in this forum, data collection continued throughout the academic year.
Focus groups were chosen as the method of data collection for two reasons; first, the debriefing sessions were already an established practice in the Department of Surgery, offering an opportunity to directly invite all students completing their surgical rotations at each hospital to participate in our focus group sessions. Second, the use of focus groups enabled discussion and critical reflection among students who had different experiences in their rotations across hospitals. In order to foster open discussion, a moderator was chosen from outside the Department of Surgery and encouraged participants to discuss each others’ strategies and behaviours without fear of evaluation from within the Department. With participants’ permission, the focus group sessions were audio-taped.
Data analysis
We conducted a thematic analysis to fulfil our aim of ‘discovering and understanding’ (Merriam 1998) the phenomenon of informal self-regulated learning as it is enacted in the daily learning activities of third and fourth year medical students. The audio-taped sessions were transcribed and entered into NVivo qualitative data analysis software to facilitate the analysis. The thematic structure was developed by the research team through a constant comparative approach in that preliminary categories were identified by during data collection, allowing us to iteratively focus on emerging themes in subsequent focus groups and to purposefully explore negative-case examples. The final data analysis was conducted by one researcher using a process of relating and grouping the emerging thematic structure through repeated readings of the focus-group transcripts. The development of themes at every stage of data analysis was carefully documented and reviewed by the entire research team.
Results
The primary objective of this study was to understand the phenomenon of informal self-regulated learning as it is enacted in the daily learning activities of third and fourth year medical students. Our participants described four key learning activities that they engaged in during their time on the surgical rotation;
-
Time Management; ensuring that their time was spent in activities that would optimize their learning.
-
Setting learning objectives; clearly articulating learning objectives for the rotation to themselves and/or their supervisors on the rotation.
-
Defining their role; establishing a recognized role with associated responsibilities while on the rotation.
-
Adhering to an education strategy; maintaining long-term education goals while in the context of the current rotation.
However, the way students engaged in these learning activities differed greatly. The thematic analysis revealed three distinct learning approaches that informed our understanding of the ways in which informal self-regulated learning is enacted through daily learning activities: acquiescing to a perceived lack of learning opportunities, choosing from available learning opportunities and creating new learning opportunities (see Table 1).
Acquiescing to a lack of learning opportunities
In the context of discussing how to maximize learning opportunities, one approach to learning was described as acquiescence to a perceived lack of learning opportunities during the rotation. This approach emphasized the systemic barriers that students felt they experienced as they sought to use their time on the rotation effectively;
I would like to think that at this level, we are all very proactive learners. I think the problem is within the system where, no matter how proactive you are, if people are not willing to take you there, they’re not going to take you there. And you can be as keen as you want, you can do as much as you want, but what it comes down to is the fact that we are so low in the bottom of this hierarchy that you can’t help but think there’s nothing for us to do.
This resulted in participants feeling that the time spent on the rotation did not optimize their learning;
I just feel anything that I’ve learned in the surgical rotation is on my own time. Going to the hospital makes me dumber than staying home.
Their perception that spending time in the wards was a waste of learning time was reflected in unsuccessful attempts to set objectives with their seniors/staff;
I think it was probably one of my biggest mistakes was when my senior asked me where I was going at the end of the year and I think I said, “I’m not sure yet but maybe Family (Medicine)”. I immediately was dismissed.
As a result, the role participants were forced to play on the rotation was limited and demoralizing for them;
It’s very demoralizing, because feel like I paid my tuition to learn and not to run around and look like a monkey when I’m doing it.
Interestingly, this approach to learning was viewed as part of an overarching education strategy focused on doing whatever necessary on the rotation with the primary aim of getting a good evaluation;
Read up as much as you can in general surgery before the first day and then when you’re in the O.R. you can impress your staff by pointing out an anatomy or answering their questions. And when you’re doing scut work, just keep your mouth shut and your head to the ground and don’t complain, just do it. Do what you’re told, do it fast, don’t make mistakes and take any abuses coming to you.
Choosing learning opportunities
The second approach to learning articulated in the data, while still delimited by the opportunities offered by the rotation, also included an important element of choice that participants were careful to cultivate in their relationships with residents and staff;
I found it was really important to try very hard not to waste time and I think we all felt a certain element of obligation to be in certain settings. And in some areas that was very valuable but it was useful to constantly question whether or not something was valuable to our education. And I found a lot of the Residents were receptive to that and if something wasn’t important, I could just ask them, would my time be better spent in this other setting?
This learning approach was reflected in time management strategies aimed at balancing time as necessary to fulfil different, imposed learning demands. In doing so, they recognized that their time was not always being used optimally, but accepted this cost as part of a balanced approach to learning during the rotation;
You need to put in a lot of crappy watching time because you never know when the good stuff’s going to come up. So if you always take the chance to say, “we’re just going to go study for the exam and go and do something else”, you’re going to miss out on some of the things that are the most interesting.
Students described a particular focus on good communication in terms of setting objectives between themselves and their clinical teachers in order for clinical teachers to be able to provide advice and opportunities to enable optimal learning;
I think it’s important to say you don’t want surgery and relay back to the staff and say, no, I want to do a lot of clinic time, I want to learn how to read this sort of x-ray or whatever it is, so that they can tailor your learning experience.
Students’ were able to find learning opportunities within the role prescribed for them during the rotation;
Just writing orders is definitely a learning experience. So anytime you have the opportunity to do it I think it’s a good idea to try at least. Sometimes you have to wait around to make sure that they’re right, you need someone to check them, but I definitely think you’re going to learn from that.
This approach to learning was epitomized by an education strategy focused on maintaining a balance between the learning demands of the rotation and the accompanying requirements for evaluation. Inherent in this approach was the recognition that while learning was not optimized at every point in time, overall evaluation outcomes were of paramount importance. This was conceptualized as a process of strategic compliance;
I think the goal is to get a good grade and a third of the mark going towards all of this. And then the other two-thirds is going towards the OSCE and exams. So, you have to find time to study for that and to learn all the stuff that you want to learn for surgery. And if that means that some people are staying here until 7:00 pm and just standing and waiting for things, so for a third of the mark you’re spending most of your time here and probably not learning as much as you should be.
Creating learning opportunities
The final approach to learning that we identified in our data was articulated as a purposeful effort to consistently maximize learning by creating opportunities to learn on the rotation;
I think it’s important to figure out what you want out of a rotation and then go do it. So, for example, if you want a lot of OR time or experience, then go into the OR and scrub in. And if you want to do more clinic-based, primary care, then you have to go do it. But a lot of it I find that you need to self-initiate. No one is going to tell you where to go.
In enacting this approach to learning, students would allocate their time independently without external feedback, effectively designing their own learning plan;
Nobody’s going to tell you what your schedule is for the day and what they expect you to do and where you should be and that you need to take the initiative to go do stuff. So find stuff to do and find stuff that’s beneficial to your learning because nobody’s going to tell you.
Setting objectives within this approach was described as an independent activity of deciding on learning objectives and asking specifically for the opportunity to participate in what was considered most beneficial at any given point on the rotation;
I believe advocating for yourself is always important, if you were in clinic all day yesterday and then today they suggest to you, well, why don’t you go to clinic, you could always ask politely, would there be any opportunity in O.R. because I was in clinic yesterday?
Interestingly, the student role within this approach to learning was best understood as that of a ‘team member’;
In the first week it’s good to watch everyone as they communicate with the patient and see what kinds of questions they’re asking. And then once you feel comfortable you can say, can I conduct the history and find out how the patient is doing today? And in the meantime, you can always go and grab the chart and at least be the person writing the progress note, which is a useful task in finding where to find everything on the chart and then being able to become efficient at that. Because then you’re helpful to the group.
Students’ education strategy consisted of a consistent effort to ensure that learning was maximized at every moment, through strategic positioning;
One thing that comes to mind is for example, on Friday mornings residents had teaching. So Friday mornings are good if you want to go to the O.R. and be a little closer to the action because there are usually less residents there. All the juniors would be gone and usually I would be first assist in an operation on Friday morning.
Discussion
Unlike the formal self-regulated learning interventions in the existing literature, the current study aimed to systematically investigate how students regulate their own learning on an informal basis and to provide a forum for clinical clerks to share those activities with their peers. The focus group format of the study fulfilled the secondary objective, allowing students to share their attempts at self-regulated learning in an open forum, free from administrative control. In addressing the primary objective, three distinct approaches to informal self-regulated learning were identified. Participants articulated a tendency to ‘acquiesce to a perceived lack of opportunities’, focusing on the systemic and environmental barriers and the hierarchy inherent in the system that impede self-regulation. In contrast, participants also described having the ability to ‘choose learning opportunities’ once they focused on the balance and communication of different learning needs with the expectation that some time must be spent on service rather than learning. Finally, participants were able to ‘create learning opportunities’ by focusing on their independence and making an attempt to optimize the amount of learning achieved in all situations.
When the results are interpreted through the lens of self-regulated learning theory, there are two themes of particular interest that emerge from these data: the notable lack of critical self-reflection in students’ self-regulated learning activities and the different ways that the interaction between students and their environment impacted informal self-regulated learning. With respect to the absence of student self-reflection in our results, it has been argued that within any one instance of self-regulation, three cyclical phases occur: forethought, volitional control and self-reflection (Zimmerman 2000). The four key learning activities identified students in our data (Table 1) fall primarily in the phases of forethought (setting learning objectives, defining their role) and volitional control (time management, adhering to an education strategy). Strikingly absent is the description of any self-reflective activity. The apparent failure to close this loop may be attributed to two sources: the lack of systemic structures that promote reflective activities and students’ inability to utilize self-reflection. A potential explanation for this inability is students’ lack of education regarding the interplay between personal and environmental factors in daily practice. Interventions like our focus group sessions may improve this ability by creating a forum for students to educate each other and share their successful and failed attempts at self-regulated learning.
Our second theme is identified when we hone in on the patterns of interaction between students and their environment evident in our results. Social-cognitive theorists suggest that self-regulated learning involves reciprocal interactions between environmental variables, personal variables, and behaviour. This ‘triadic reciprocality’ is evident when students adaptively change their environment and those changes, in turn, affect perceptions of personal and behavioural variables (Bandura 1986; Schunk and Zimmerman, 2001). Consequently, self-regulated learning requires that students fine-tune their responses to the affordances and constraints in their environment (Evensen et al. 2001). The three learning approaches articulated in our data highlight the different ways in which students interact with the environment in the context of informal self-regulated learning.
The ‘acquiescence’ approach suggests that students might have difficulty integrating environmental and personal variables to reduce cognitive or affective burdens. Consequently, they are unable to shed their identity as ‘student’ and persevere passively in this role rather than working toward a ‘clinical problem solver’ identity (Evensen et al. 2001). As a result, their learning goals and activities are dictated by the educational system, leaving little opportunity to adaptively self-regulate their learning.
In contrast, the ‘choosing’ learning approach suggests that students may also construct their goals to reduce and/or avoid academic risks (Evensen et al. 2001). While this is certainly productive within the constraints of a specific clerkship rotation, these goals point toward a performance orientation, rather than a more globally effective mastery orientation (Paris et al. 2001). That is, students choose opportunities that will lead to a favourable evaluation of their performance on the current rotation, rather than setting goals to enhance self-competence and a deeper understanding of daily practice. The emphasis on strategic compliance links well with short-term performance and demonstrates the important balance between personal goals and environmental constraints. At the same time, however, the approach does not link well with long-term goals of achieving mastery in the ability to navigate the clinical context.
The ‘creating’ learning approach approximates what Evensen et al. (2001) identify as the behaviours of a capitalizing student. Students can take the time to step back and assess both their own personal learning goals and the affordances in the environment and adjust their behaviour accordingly. Strategically positioning oneself to be considered part of the team and to capitalize on personally appropriate learning opportunities is the hallmark of effective self-regulation (Schunk and Zimmerman 2001). Students are able to recognize the importance of adapting to their environment and use this knowledge to achieve specific learning objectives, while also pursuing greater participation with the clinical community and an identity as a ‘clinical problem solver’ (Evensen et al. 2001).
Implications and future directions
In meeting the primary study objective, we have identified and presented three approaches to informal self-regulated learning. The data emphasize a view of self-regulated learning that grows beyond the social-cognitive perspective by considering the situative perspective, in which external forces and students’ interpretations combine to influence student behaviour (Evensen et al. 2001). The resulting actions of acquiescing, choosing or creating learning opportunities are not mutually exclusive personality traits. Rather, all three approaches can be under-taken by the same individual depending on the learning context. In some instances, students will choose their own learning activities adaptively. At other times, they will focus on the environment’s affordances and constraints. Preceptors could intervene by taking the time to highlight those environmental characteristics directly, or by guiding the student to the necessary resources. Informal self-regulated learning might therefore be better conceptualized as a collaborative process in which a ‘more capable other’ (Vygotsky 1978) helps the student to design their own learning. Brydges et al. (2010)have recently defined such an approach as directed self-guided learning. In the clinical context, preceptors can direct students toward a more interactive stance (Evensen et al. 2001) both in the way that students perceive their personal interaction with the environment and in the way they interact with more capable others. The best form of direction notwithstanding, we recommend that future research continue to probe the directed self-guided learning concept to determine its effectiveness for improving students’ informal self-regulated learning in practice.
Along the same lines, it has been argued that students learn self-regulatory skills by observing and emulating more capable others (Zimmerman 2000). In the education literature, the ability to self-regulate learning is described as an advanced skill, yet the current rotational system seems to expect students to operate at this advanced level immediately upon entering the clerkship. This approach of placing students ‘in the middle of things’, may contribute to students’ inability to grow from student observers into competent self-regulators. The single-institution design of this study is it’s most important limitation because we cannot generalize our findings to other clinical specialties or to other models of undergraduate education such as longitudinal clerkships.
While we started the investigation into informal self-regulation by documenting the student perspective on their own learning, future studies should address the opinions of faculty members who are in a position to evaluate the appropriateness of student actions and shed light on the effect student efforts towards self-direction can have on the rest of the clinical team (cf. Ginsburg et al. 2010). The identified lack of self-reflection on the part of participants in this study also suggests a need to promote activities that go beyond a final debrief, encouraging students to consider their approach to learning long before the clinical rotation is over. Self-regulated learning is a skill that continues to evolve throughout education and practice. While it is by definition in the hands of the individual to engage in self-regulated activities, medical teachers and school systems play an active role in ensuring that students are equipped to do so.
References
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ, US: Prentice-Hall, Inc.
Bravata, D. M., Huot, S. J., Abernathy, H. S., & Skeff, K. M. (2003). The development and implementation of a curriculum to improve clinicians’ self-directed learning skills: A pilot project. BMC Med Educ, 3, 7.
Brydges, R., Dubrowski, A., & Regehr, G. (2010). A new concept of unsupervised learning: Directed self-guided learning in the health professions. Academic Medicine, 85(10 Suppl), S49–S55.
Butler, D. L. (2002). Qualitative approaches to investigating self-regulated learning: Contributions and challenges. Educational Psychologist, 37(1), 59–63.
Butler, D. L., Schnellert, L., & Cartier, S. (2008). Layers of self-regulation: Teachers working strategically to improve practice so as to foster students’ self-regulation. Paper presented at the annual meetings of the American Educational Research Association (AERA), New York.
Evensen, D. H., Salisbury-Glennon, J. D., & Glenn, J. (2001). A qualitative study of six medical students in a problem-based curriculum: Toward a situated model of self-regulation. Journal of Educational Psychology, 93(4), 659–676.
Frank, J. R. (Ed.). (2005). The CanMEDS 2005 physician competency framework. Better standard s. Better physicians. Better care. Ottawa: The Royal College of Physicians and Surgeons of Canada.
Ginsburg, S., McIlroy, J., Oulanova, O., Eva, K., & Regehr, G. (2010). Toward authentic clinical evaluation: Pitfalls in the pursuit of competency. Academic Medicine, 85(5), 780–786.
Kuzel, A. J. (1999). Sampling in qualitative inquiry. In B. F. Crabtree & W. L. Miller (Eds.), Doing qualitative research (2nd ed.). Thousand Oaks, California: Sage Publications Inc.
Merriam, S. B. (1998). Qualitative research and case study applications in education. San Francisco: Jossey-Bass.
Murad, M. H., & Varkey, P. (2008). Self-directed learning in health professions education. Annals of the Academy of Medicine, Singapore, 37(7), 580–590.
Mylopoulos, M., & Regehr, G. (2009). How student models of expertise and innovation impact the development of adaptive expertise in medicine. Medical Education, 43(2), 127–132.
Nousiainen, M., Brydges, R., Backstein, D., & Dubrowski, A. (2008). Comparison of expert instruction and computer-based video training in teaching fundamental surgical skills to medical students. Surgery, 143(4), 539–544.
Paris, S. G., Byrnes, J. P., Paris, A. H., Zimmerman, B. J., & Schunk, D. H. (2001). Constructing theories, identities, and actions of self-regulated learners. In: Self-regulated learning and academic achievement: Theoretical perspectives (2nd ed., pp. 253–287). Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers.
Patton, M. Q. (1990). Qualitative evaluation and research methods. Newbury Park, CA: Sage Publications, Inc.
Scardamalia, M., & Bereiter, C. (2003). Knowledge building. In encyclopaedia of education vol 2nd (pp. 1370–1373). New York, USA: Macmillan Reference.
Schunk, D. H., & Zimmerman, B. J. (2001). Social cognitive theory and self-regulated learning. In: Self-regulated learning and academic achievement: Theoretical perspectives (2nd ed.). (pp. 125–151). Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers.
Vygotsky, L. (1978). Interaction between learning and development (trans: M. Cole). In: M. Cole, V. John-Steiner, S. Scribner & E. Souberman (Eds.), Mind in Society: The development of higher psychological processes. L.S. Vygotsky (pp. 79–91). Cambridge, Mass: Harvard U Press.
Zimmerman, B. J. (1989). A social cognitive view of self-regulated academic learning. Journal of Educational Psychology, 81(3), 329–339.
Zimmerman, B. J. (2000). Self-efficacy: An essential motive to learn. Contemporary Educational Psychology, 25(1), 82–91.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woods, N.N., Mylopoulos, M. & Brydges, R. Informal self-regulated learning on a surgical rotation: uncovering student experiences in context. Adv in Health Sci Educ 16, 643–653 (2011). https://doi.org/10.1007/s10459-011-9285-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-011-9285-4