Abstract
Computerised virtual patients (VPs) are increasingly being used in medical education. With more use of this technology, there is a need to increase the knowledge of students’ experiences with VPs. The aim of the study was to elicit the nature of virtual patients in a clinical setting, taking the students’ experience as a point of departure. Thirty-one students used VPs as a mandatory part of an early clinical rotation in rheumatology. Using the qualitative approach of phenomenology, we interviewed these students and then analysed data regarding their experiences of VPs as a learning activity. The result shows that students perceived VP activities in relation to actual patients, the clinical context and other learning activities. The VPs represented typical clinical cases which encouraged clinical reasoning and allowed for decision making. The students experienced the activities as integrating biomedical knowledge and clinical experience, providing structure that prepared for the unstructured clinical environment and patient encounters under unstressful conditions. However, the VPs were experienced as lacking the emotional interactivity and complexity of actual patients. Theoretical frameworks of clinical reasoning and experiential learning are suggested as foundations for further educational integration of VPs in the clinical environment. VP activities during clinical rotations provide experiences of clinical reality and allow students to solve problems actively. These features are dependent on VP technology but are also contingent on the surrounding environment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Medical workplace learning needs pedagogical support in order to be meaningful for students (Dornan et al. 2007). Passive learning, little opportunity for reflection and limited time for clinicians to devote to teaching are some issues identified as obstacles to learning in clinical environments (Sandroni 1997; Spencer 2003). Structural changes in hospital care have also affected the teaching situation. Medical students now encounter fewer patients on wards and seldom get to follow outcomes of investigations or effects of treatments. Another educational consequence of these changes is that patients admitted to the ward need specialised care and do not always represent common diseases. Furthermore, many of them are severely ill and may be too sick or tired to participate in the training of students.
Patient cases are presented to students throughout their education as an established method for working with diagnostic reasoning and dealing with presenting symptoms (Irby 1994). These cases are commonly presented with all clinical information at once in a static manner, typically on paper. Beginning in the late 1960s educators began to develop technology for computerising patient cases into virtual patients (VPs). The VP technology is defined as an interactive computer simulation of real-life clinical scenarios for the purpose of healthcare and medical training, education, or assessment (Ellaway et al. 2008). The educational strength of VPs has been identified foremost as promoting clinical reasoning, an important aspect of clinical learning (Cook and Triola 2009).
Although the idea of VPs is not new, they are still regarded as an educational innovation and broad regular use of these has not yet come into practice (Cook and Triola 2009). In 2005, only 26 of 108 US and Canadian medical schools used VPs, partly explained by high production costs (Huang et al. 2007). There is also reason to believe that there are vague conceptions of how the technology should be used to reach its full educational potential (Berman et al. 2008; Cook and Triola 2009).
When integrating new technology into traditional educational contexts, the aims for their use and surrounding practices need to be considered (Edelbring 2010). The way we conceptualise VPs as a learning tool influences the ways in which they are used, and consequently, how students benefit from them. For this reason, there is a need to establish clear conceptions of VP use.
Most VP research concerns descriptions of the technical possibilities of the tool itself (Cook and Triola 2009), and which reports are necessary in order to raise awareness about educational innovations. Another kind of research concerns the performance outcomes of VP use, contributing knowledge about the consequences for student learning. A recent meta-analysis found VP interaction to have large positive effects when compared to no other teaching, small effects in comparison to non-computer teaching and concludes that effective VP practices need to be further understood (Cook et al. 2010). If VPs are considered to be an educational innovation, there is reason to believe that predefined performance measures in a traditional practice will not clarify their character and capacities (Cook 2005; Friedman 1994). Instead, to uncover the educational value of VPs, knowledge about how students make use of them and what qualities students ascribe to them is needed (Boud and Prosser 2002; Norman 2006). The way students experience learning situations has a decisive influence on their learning outcome (Marton and Booth 1997). A holistic and situational view of student learning with technology makes it possible to find where and when new technology contributes to learning (Colaizzi 1978; Dall’Alba and Barnacle 2005).
Few studies focus on how students approach VPs and how the students describe the learning situation using this tool. Researchers taking this approach found students perceiving that VPs are interesting and that VPs stimulate thinking and active involvement in cases. However, a common concern is that they should not replace actual patient contact (Bergin et al. 2003; Bryce et al. 1998). The collaboration aspect enhances student engagement and was favoured by most students (Bergin et al. 2003; Bryce et al. 1998). We found one VP study that took the in-depth interview approach which makes it possible to analyse data from a “lived experience” perspective (Bearman 2003). In this study the virtual patient encounter was found to evoke strong emotions and that it had the potential to introduce students to the complex clinical world. Less is known about how VPs function in the clerkship.
The aim of the current study was to elicit the nature of VPs in a clerkship context. In taking the lived experience approach, this study focuses on meaningful aspects of VPs in student use (Colaizzi 1978; Marton and Booth 1997). The research question to address was—how do virtual patients appear to students in the clinical education?
Methods
Context of the study
The study was performed at the rheumatology unit of Karolinska University Hospital during autumn 2008. This unit cares for most of its patients in the outpatient clinic and the day care clinic, where patients come in for short scheduled visits. The in-ward has ten beds for day and night care for severely ill patients. One week of training in rheumatology forms a part of the internal medicine programme and two to four students rotate every 1 or 2 weeks at the unit. The clinical rotation is hospital-based, students participate in ward rounds and participate in practice in the day care clinic or the in-ward setting. A clinician supervisor is assigned to each pair of students. The students were in their third year of a traditional curriculum with limited experience of patient encounters. During autumn 2008, 31 students were allocated to the unit, of which all were included in the present study.
VPs were established as an integral part of the clinical rotation at the unit earlier that year. During their rheumatology rotation, students worked with four cases based on authentic rheumatology patients with common rheumatic disorders (pelvospondylitis, polymyalgia rheumatica/giant cell arteritis, Sjögren’s syndrome or systemic lupus erythematosus) representing the out-patient setting. The VP cases were presented by video clips from patient interviews, images, text, clinical investigations and laboratory results. The VP software prompts the students for a diagnosis as well as differential diagnoses and the patient story evolves stepwise depending on student interaction. The software itself, ReumaCase, is based on NUDOV and shares its appearance and functionality (Wahlgren et al. 2006). The VP-equipped computer was made available together with a rheumatology textbook and Internet access. Students were encouraged to work with the VPs in pairs which most of them did, although other constellations also occurred. The VP activity was mandatory although not scheduled to any specific date or time. Most students spent around 1 hour for the first VP and typically less time, around 30 min, for each subsequent case.
Methodological considerations
Interviews were chosen as the method for data gathering in the belief that dialogue is fundamental for sharing meaning (Shotter 1993). We chose a theoretical approach that allowed the object of study to appear from a user (student) perspective less influenced by normative preconceptions and expectations. In phenomenology, theories and prior knowledge are temporarily set aside in order to “let that which shows itself be seen from itself” (Heidegger 1962, p. 58). Furthermore, the source of data is the direct personal experience as opposed to using an objective third-person perspective (Gallagher and Zahavi 2008). The phenomenological researcher breaks with the “natural attitude” using phenomenological reductions and the object of analysis is reduced to the meaning it has for the experiencer (Karlsson 1993).
In recent years Husserl’s (1859–1938) radical first-person perspective developed into empirical research methods resulting in reports on how phenomena are experienced by “empirical subjects” (Giorgi 1985; Karlsson 1993; Moustakas 1994). There are variations of empirical phenomenology as a research approach depending on the phenomenon of interest and practical circumstances (Sixsmith and Sixsmith 1987). However, two key aspects unite the different variations: (a) the researcher takes the perspective of the experiencer and (b) the analysis takes the phenomenon itself and its immediate context as sources for understanding the phenomenon.
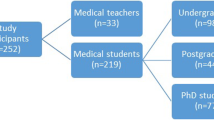
Interviews
Research participants consisted of a total of 31 students allocated to the rheumatology clinic in autumn 2008. All of them consented in writing to participate. Interviews were held at the clinic at the end of rotations. Students were interviewed individually or in groups of two to four in a total of 13 interviews. The constellations were distributed as being one (n = 3), two (n = 5), three (n = 2) and four (n = 3) students together. The length of the interviews ranged from 11 to 41 min with a median of 37 min. The interviews were conducted and recorded by SE (n = 11) and MD (n = 2). They were transcribed in full by SE. In order to get close to the students’ life world as medical students, the meetings took place directly in the clinic. An interview guide was used, with written key areas and some questions prepared in advance as an aid to keeping the session focused on the VP activity. Example areas were “learning with VPs”, “experiences of learning at the clinic”, “learning with patient encounters”, “the patient as person” and “the clinical rotation”. The participants were encouraged to talk freely in a relaxed way about these topics rather than following a question–answer protocol.
Analysis
The transcripts were analysed using the Empirical Psychological Phenomenology (EPP) method as a guideline (Karlsson 1993). This method is an implementation of the phenomenological approach divided into concrete steps dealing with transcripts. Each transcript was read once to become familiar with the respondents and the way they addressed the topic. It was then re-read and passages relating to the aim of the study were highlighted. These meaning units were then clustered together under tentative labels such as “exposure to typical cases” and “peer interaction”. The categories grew and were re-arranged as new transcripts were analysed. This first analysis was used as a basis for the next iterations where quotes were reduced in numbers. At this stage, meaning units were considered to have equal value in relation to the phenomenon of interest. A substantial number of quotes were reduced, in iterations with the full transcripts, to aspects describing students’ experiences of the VP situation. Interview quotes were translated to English illustrating the results and providing a link directly to the data.
To become aware of the researchers’ preconceptions, each of the authors wrote an account (a half page of text) of his or her assumptions of VPs as a learning tool. SE performed the analysis supported by LOD, HH and MD. Findings were discussed by all authors in relation to the transcripts.
Results
This section first introduces experiences concerning the clinical context, forming a backdrop for the aspects of VP activity that follows. The experiences reported here come from salient aspects of interview data. The quotes are labeled with fictive student names and interview numbers.
Students’ perceptions of the clinical context
Before considering experiences of VP activities themselves, we must first describe how students perceive the clinical environment within which these activities occurred.
The clinical setting was influenced by expectations of direct patient contact where physical investigations and patient management are performed. Patients and situations at the clinic gave meaning to previous knowledge by placing it into concrete situations. Students got to carry out concrete procedures themselves and, in varying degrees, took responsibility and made suggestions for decisions. This student action was regarded as more engaging and valuable passively shadowing a doctor and observing things, something that also occured at times. The time spent at the clinic was very precious and clinical rotations during this phase of education were described as short, typically 1 or 2 weeks.
That’s what central in the educational program. I’m studying now. Without the clinical rotations, the theory we’re studying would be extremely difficult to apply, and I’m really learning a lot by watching, feeling, touching and listening and taking part. There’s also more involvement all the time when you have a concrete situation to follow. I think that it’s the concrete situation that’s most important really. (Niklas, 12)
I always think that what you learn the most from is having your own patients and being given as much responsibility as possible. Being forced to become familiar with the sort of things you think are tough and don’t understand. That’s what you absolutely learn the most from. (Lena, 2)
You’re never forced to really think on these wards; instead, you follow and… try to be active. Not that you really have to think. (Camilla, 13)
Meeting patients and dealing with concrete situations gave a sense of overall advancement in their professional education. However, patient contact was not experienced as easy or as constructive learning situations, and sometimes students felt awkward in front of patients. It turned out to be more difficult than expected to get information about patients’ symptoms directly from the patients. Patients were perceived as disorganised, talking about irrelevant aspects and only giving fragments of their history and illness progression.
The students also felt pressure to appear knowledgeable in front of patients. Physical investigations could thus be intimidating. The time available for the actual patient meeting was also perceived as being too short.
Often, they’ve been lying in bed with the bedclothes up to here (illustrates with her hands just below her chin) so you haven’t seen them, and not seen them move that much or walk and so on, so you don’t have a picture in your mind to link it to. (Rita, 4)
I often think when one’s carrying out a physical examination of the patient, that you don’t do everything because it could feel… I’m so timid that I don’t want to trouble the patient by asking him to do certain things during the physical examination. So you think: well, they’re going to examine that anyway, or they’ve just examined it, or oh, I don’t want to press on the patient’s stomach again because it’s tough for the patient if they’ve just done it on the round or something. (Yvonne, 8)
Patients at the clinic represented snapshots of different stages of diseases. However, one and the same patient could not be followed over time, from diagnosis to treatment. Rheumatology investigations were described as time consuming where it can take months before a diagnosis can be reached.
It’s often a lengthy process on the wards. Since we’re only here a week, we’re not here long enough to know what will happen and what the diagnosis will be. (Veronica, 6)
Experiences of VP activity
The concept of a virtual patient was fairly new to the students and they approached studying with VPs in several ways. Overall, it was a satisfying experience and time spent with VPs was believed to enhance the educational value of the clinical placement. The first aspects relate to the “how” of the situation and the latter more to the “what” characteristics of the VP encounters.
Responsibility to regulate VP work
Even if the VP activity was a mandatory part of the rotation, responsibility of when to do it lay with students themselves. They sometimes had to face the dilemma of prioritising between VP study and patient work at the ward, clinical time being precious. The lack of teacher control surprised the students; in particular they had expected to discuss cases with clinicial teachers.
[You should] follow up the case work afterwards. I’m really surprised that we don’t review them afterwards, together with a teacher. The answers can be found in the computer program, but nobody checks whether we’ve done this. We could have… Now we haven’t written anything on the computer. We do have sheets of paper we can show and also review. But generally speaking, we could have just clicked through the cases./…/[You should] follow it up. Because the computer can never replace a human even if it’s very good. (Elin, 6)
You missed patient work on the ward in order to do web patients, it felt a bit odd. (Susanne, 2)
I would have preferred a set time to do it and to sit a couple of hours so it doesn’t turn into rushing through a case. (Veronica, 6)
More than software interaction
The VP activity was not experienced only as interaction with the VP software. Some of the clinical problems that were raised when working with the VPs required students to turn to other sources such as the textbook, medical Internet sites and to professionals at the clinic.
But here you need to reflect more, you need to look up things in books more. (Roger, 13)
What I thought was good was that it got you to take out the books because I wouldn’t have done that otherwise. (Lotten, 5)
VPs contribute to a case repertoire
Some aspects of students’ experiences with the VPs can be attributed not only to the software structure and study setting, but also to patient cases themselves. Many students commented on the specialised nature of the clinic, where they meet patients with unusual diagnoses, but not always the ones that represented the common rheumatology disorder spectrum in the population. After working with the VP cases, they felt that they got a richer picture of the rheumatology illness panorama, since the VP cases were more representative of the population than the actual patients they met during the rotation. The VP cases were perceived as incorporated side by side with their experiences with actual patients.
It ensures that you get to see these typical patients. If you’re not fortunate enough to see them in real life, you at least get to see them in this program. (Linus, 7)
Although I still have to, we haven’t met… any patient like this these 2 weeks. And that’s also why I think that this program… I would have preferred to work more with it and have more cases because I think it was really good. (Camilla, 13)
Structured cases in an unstructured reality
The VP cases were perceived as structured regarding symptoms and how these became apparent during the VP interaction. This structure was regarded as helpful, being a smooth transition from the stereotypical textbook cases to interaction with “unstructured” actual patients. But for a learning activity they appeared as too stereotyped, clear and brief. One VP that was more ambiguous in terms of symptoms was said to lead to a better learning experience.
Because I think that case one, Tyko, in particular was good for me. Because he had very unclear symptoms and some symptoms indicated one disease while some indicated another and then I thought that he had both, and I sat and puzzled over it. So I thought he worked, taught me most. Even if I was mostly wrong about him, he taught me most. (Lukas, 4)
It was actually really good for learning the theory, the basics, but it’s very important to be on the ward and see the real cases, which are often a bit more complicated. I felt that these [cases] were like those in the textbook, yes, exactly, he had exactly the same symptoms as those described in the textbook. (Siw, 5)
The VP activity was here experienced in relation to the reality of clinical practice. This relationship was somewhat ambiguous. On the one hand, VPs provided useful representations of diagnoses, the clinical reality and the medical context. On the other hand, the cases appeared too constructed, neat and well-ordered. Dimensions of complexity, presence and emotional response were missing in the VP experiences when contrasted to actual patients.
These are very compliant patients that live in this computer system and say exactly what they are expected to. If you ask—How are things at home? You might get a narrative in 4 mins by a real patient. These are very obedient. But that’s very good, a structured way to take it in. (Linnea, 4)
It ought to be the same, but I think that it’s just my own feeling that it’s not really the same thing, that some sort of “contact” is missing in some way, you don’t get feedback in the same way. (Titti, 3)
But there are no emotions involved. When you meet a real patient, it’s very much about emotions and responding to them. In the computer system, you don’t need to respond to any emotions. (Ellen, 2)
Unstressful patient encounter allowing for reasoning with peers
The VP encounters appeared in many respects similar to actual patient encounters albeit less dramatic and emotional. The VP situations allowed for reasoning in front of the virtual patient in a relaxed way, posing one question at a time, repeating questions and browsing the textbook. This was not considered possible in front of an actual patient. Peer interaction, especially in pairs, also made the situation active and the cases more open to exploration.
This is so good for learning the routine and that you become comfortable with it so it doesn’t get in your way when you meet a real patient. (Rita, 4)
Therese: But here it’s very positive right now when we really don’t know everything about rheumatic diseases, that we can sit with our books at the same time as we have a patient in front of us
Lotten: It would never be allowed otherwise… (mimes turning the pages of an imaginary medical textbook) ‘give me 5 min’… (bursts out laughing)
Therese: And that you don’t have to be so… when we meet patients, we’re really focused, sometimes it’s almost like having a memory lapse afterwards because you’ve been so incredibly focused during the visit. And here you didn’t need to be as focused; instead, you could really accept not being a full fledged doctor, you don’t know everything and so on. (Therese and Lotten, 5)
You get so much more from the situation when you discuss things with someone else, than if you would be working alone (Camilla, 13)
You grasp the facts in another way when you discuss things with others around you than if you were to sit there yourself. (Sandra, 7)
Wanting to feel smart in front of the computer
Although there was no external pressure from actual patients in the VP situation, the students were not totally relaxed. They wanted to appear knowledgeable and not lose face in the situation. Some students described it as a competitive mode, almost like a computer game, competing with the specialist managing the patient.
You get the list of what the specialist would have done, and depending on how many you managed to get right and how you value those you got right, you value your degree of competency. This is the game thing. (Titti, 3)
Interviewer: Do you feel that way [that you have to be right] against the specialist?
Camilla: Absolutely. We checked thoroughly so that we weighed all of our differential diagnoses.
Roger: Well, I felt a little stupid in front of the program, or before the questions. I didn’t have the theoretical foundation and I dislike strongly not knowing enough. (Camilla and Roger, 13)
Preparatory function for clinical work
The VP situation was experienced as preparatory, making work during the rotation more meaningful. Prominent features in the learning experience were structured patient interviews, terminology and procedures specific to the speciality and to a lesser degree, biomedical facts.
The VP experience appeared as an entry point to the rheumatology context. The interview structure in the VPs became a tool to relate to actual patients at the clinic in a beneficial manner. Also procedures and special terminology were recognised from the VP activity when encountered in the clinicial practice.
It’s like a very efficient… that is… the first step that takes you very far. Being at the ward up there just doesn’t give as much. And just the fact that you’re better equipped to identify and understand things afterwards. (Maj, 13)
…and we encountered a lot of complicated terms. We had to sit and repeat out loud: “Polymyalgia rheumatica” and “Ankylosing spondylitis” (laugh). (Therese, 5)
Maybe we didn’t learn so many new things… well, in some cases I learned concrete things from the program. But above all when a diagnosis turned up that I didn’t really agree with, or the result of, for example, a salivary gland biopsy that came up according to the grading, grade IV, I didn’t know what it was and then I looked it up in the book. (Ulrik, 11)
Yesterday we had our own patients and I felt that after accompanying a doctor for a couple of days and using this computer program that I could exclude inflammatory system disease [from inflammatory joint disease] through bombarding the patients with these questions, comparing answers and physical examinations (Therese, 5)
Knowledge contextualisation
Working through the cases reactivated the biomedical knowledge that students brought to the clinic. Things fell into place when facts were applied to a situation and connected to actual cases. The VP work supported the transition from knowing medical facts about diseases and symptoms, to actually putting this knowledge and the procedures into practice in a situation. In this process, previously known pieces of a jigsaw puzzle came together forming a comprehensible whole.
Glimpses of the life world of the VP cases also stimulated forming ideas about patients’ personalities and their life situations. The names of the four cases were remembered at the time of the interview although students mostly referred to them by their respective diagnoses.
You get connections, because I myself think now, when I’ve heard all these diseases this week, I’ve heard of many of them but I can’t quite remember what distinguishes them and what… And then it’s always good to have a patient to connect it to. (Rita, 4)
I guess I’ve learnt above all about symptoms and how patients describe their symptoms and their diseases. (Susanne, 2)
They got to talk themselves about how difficult it is in their everyday life. (Moa, 9)
Structuring and focusing the patient encounter
With the VPs, students developed a sense of structure for interaction with patients during the placement. This concerns in particular interview questions but also lab tests, examinations and an overall clinical thinking. The structured character of the VPs steered the focus towards what was believed to be important when working with patients at the clinic.
It becomes really clear which patient questions one raises and which ones are good. Because when you’re at the ward everything runs by quickly and maybe it’s not a first-time visit and you don’t go into detail with all the questions. So it is more useful to learn what questions are good to ask and clearer in that way… it is very… well… it covers very much, it is very comprehensive in the cases. (Tine, 7)
And then it’s so easy to go in and see what tests you need and what differential diagnoses we have. Because when we have real patients, everything is so muddled. You don’t really know… well… and you never find out what it really was. You do here. I think that’s good. (Veronica, 6)
Yesterday, we were working with an SLE patient with butterfly rash, and that’s fairly typical for SLE and certain characteristics of rashes. Then [with VP] you get the picture of them and a description. But on the other hand, if you meet a patient, you don’t really notice this sort of thing that easily; instead, there’s a focus [on what is clinically relevant] in some way. (Lukas, 4)
Training clinical thinking
The students felt that the VPs stimulated reflection on clinical work. Furthermore, it induced assessment of information and required active decision making. Reaching a diagnosis was a set goal, but the process of getting there was equally important. Different methods of reaching a diagnosis were actualized in this process. When describing this aspect, some of the students used the metaphor of “playing detective”. However, some of them felt that their knowledge of and skills in rheumatology were insufficient to benefit from the simulated physical examination parts of the VPs.
But the problem-solving approach, it’s the same; you get a whole lot of information, mainly from the patient interview and the physical examination. And then combining it with lab tests and trying to get some sort of overall picture. In this way, the problem-solving aspect is the same as in the real clinical situation. (Lars, 3)
Sometimes we have seminars with patient cases where we’re given a sheet of paper with a short description and then we have to make a diagnosis. Here, it was also the actual course of events. You carry out the interview and physical examinations. ‘What tests do you want to order?’ (Lotten, 5)
VPs as a learning tool—similar but different
When students were asked to describe VPs as a learning tool, they did not readily find the words for labeling it, although they had strong feelings about the situation. Neither did they approach it with clear expectations beforehand. To describe the VP activity they referred to other learning situations such as textbook reading, seminars and bedside teaching. The VP learning tool related to all of these, but its use was singled out as having its own specific characteristics. Compared with reading a book, the use of VPs was considered to trigger more activity and having an extra dimension with video clips of patient presentations and physical examinations. It was also more time-efficient than interacting with real patients or participating in case seminars. The variation in learning activity, studying in a different way as compared to traditional situations, was also perceived as having an overall value for learning in their education.
You get to meet the patients more interactively and see film clips of patients being investigated and decide yourself what to do with the patients, establish a diagnosis. It is much better than a seminar. It is difficult to summarise a somewhat new way of studying, there are no defined… well… (Niklas, 12)
This is between sitting in your room studying and meeting patients together with other doctors. So it is somewhere in between, a substitute. (Roger, 13)
You can either compare with real patient encounters or compare with reading a book in order to learn. In that way it is closer to reality with this software than studying a book. In that sense, it provides another way of learning than studying with a book. (Ella, 10)
It is like thinking in another way. Reading a book can be as interesting, but then you only get facts all of the time. Here, you need to think about what questions you need to ask and see where they lead. (Linus, 7)
It’s like meeting regular patients only faster, we can meet four in three hours. (Magnus, 11)
The essence of the VP activities
The experiences of the VP activities during the clinical rotation were multifaceted, covering situational aspects, structural possibilities of the technology and factual knowledge in VP cases. Based on interview data and illustrated by aspects and quotes above, the essence of the VP activities appears as formal study activities about which students have vague expectations beforehand. Despite the vague expectations, the VP interaction appeared as study situations with their own characteristics. The VPs provided possibilities to make decisions and solve problems in the students’ future profession. They actualised theoretical knowledge, introduced specific problems and contextualised situations. The phenomenon of VPs as a study activity appears dependent on software technology but is contingent on the situational aspects in its meaningful use.
Discussion
This study adds to knowledge about what VPs are and how they are experienced in the clinical context by getting close to students’ life-world. The VP content, technology design and the clinical situation were seen as providing meaning as a whole (Dall’Alba and Barnacle 2005). Questions about boundaries between VP software and the surrounding context need to be directed towards what function the technology has in the situation (Brown et al. 1989). It became apparent that the VP activity was intertwined with other activities, performed together with peers and professionals.
Students perceived the clinical reality as unstructured, not yet held in a firm grasp. Against this background the core function of the VP activities appeared as intermediating between the students’ factual knowledge and the clinical environment. The VP situation provided experience of typical cases, longitudinal overviews of the progess of diseases and procedures used in the rheumatology speciality. Furthermore, the VP design structured and focused the conception of the patient encounter on what was judged to be clinically important. In this way it catalysed the process of discerning what professionals see in their work on the ward. Consequently, the importance of the VP activities does not lie in contributing new substance, but in making other activities during the clinical placement more understandable and meaningful.
The VP situations were also characterised by active engagement in reasoning and problem solving. Students got to make decisions from “the driver’s seat”. This student action seemed to be more salient when working in pairs where debate also took place. In comparison with actual patients, the VP activities were performed in a safe neutral zone, where stress, the demands of patients and the busy clinical everyday situation were temporarily put on hold. Adapting the cognitive load is regarded beneficial during the learning process (Merriënboer and Sweller 2010). In this sense VPs can be seen as a transitory step in coping with clinical complexity.
With the VPs, students clearly interacted with relevant situations, and not primarily with juxtaposed biomedical facts or abstract clinical puzzles. The situation was not in itself the clinical reality, but provided pseudo patient encounters and vicarious clinical experience that activated structures for handling the clinical reality. The VPs as persons made an impression on the students when aspects of the patients’ life world became visible. Despite this and although these cases were based on authentic patients, students found them to be too artificial, lacking true interactivity and emotional response. Similar findings have been reported in other settings where students report a gap between prefabricated interaction and how real patient encounters occur (Bearman 2003). Text-based cases have caused concern for contributing to detatchment of students from the patient as a person (Kenny and Beagan 2004). With VP technology there are ample opportunities to counter this risk by enriching cases. Obviously there is still room for improvement in this direction, probably regarding case authoring more than technology development. A recurrent finding in VP studies, ours included, is the fear of replacing real patient contact with VPs (Cook et al. 2010). A more fruitful future VP conceptualisation would be seeing VPs as an artificial learning tool aimed at specific tasks rather than making the intuitive comparison with real patients.
What does this imply for further development of VP use in clinical settings? VP integration in medical education has, to date, largely been performed pragmatically, with no solid foundation in learning theory. In the light of our findings, two aspects of learning theory could provide frameworks to further strengthen student learning with VPs in clinical settings. One of these is experiential learning (Kolb 1984; Boud and Walker 1993) where VP activity contributes opportunities both to fill gaps in clinical exposure and to digest and process “what’s going on out there” in a directed way. Experience and case exposure do not by themselves lead directly to learning; students need guided reflection on experience (Boud and Walker 1993; Bowen 2006).
The other framework is learning theories of clinical reasoning (Bowen 2006; Norman 2005). Here VPs function as an arena where students actively test different decision tracks forming clinical problem-solving capacities. This potential of VPs has been emphasised earlier (Cook and Triola 2009) and our findings about the nature of VP activities support this prospect. The VPs confront students with situations and their interactivity should make them ideal for problem-solving situations. However, teachers and researchers need to be aware of the stereotypical nature of the VP situations compared with the complexity of “unstructured” actual patients that students need to face. Lessons learned from years of assessment of this competence with patient management problems and simulations should also be taken into account (Newble et al. 2000).
Workplace learning needs pedagogical support to function well (Dornan et al. 2007) and VPs could fit well into that strategy. The meaning of the VP activities appeared as intertwined with the clinical setting. Consequently the VP setting needs to be integrated with the overall pedagogical structure (Berman et al. 2009). In practical terms this means that students need somewhere to work with VPs, allocated time to work through cases, and a climate at the ward that acknowledges the value of the VP activity.
In our study most students felt that working in pairs broadened their reasoning. The results suggest that collaboration in pairs differs from individual and larger groups and that peer interaction enhanced the reflection and problem-solving functions in the VP situation. Collaboration in the small-group setting with general computer applications is beneficial for learning achievements (Lou et al. 2001). Triad settings have been compared with individual learning with VPs with no significant differences in case elaboration (de Leng et al. 2009). Our results indicate that it would be worthwhile to study the pairwise setting more closely.
The difficulty for students to label the VP activity confirms the impression from VP research that the phenomenon is not yet conceptually established. Additional VP research with an interest of understanding and clarification (Cook et al. 2008) could contribute to further establish both educators’ and students’ conceptions of the tool and its use.
Methods
Some limitations influenced the phenomenological analysis. Students were not interviewed extensively or repeatedly, which would have made it possible to obtain even richer data on their experience of the phenomenon. Neither were all the students interviewed individually, which could have contributed to a wider spread of experiences of the phenomenon in the data (Fern 1982). Instead students were mostly interviewed in pairs or groups of four, which probably contributed to more commonly shared experiences to be expressed. The relaxed and open interview setting contributed to a rich set of data for the analysis. There was, however, a tendency for students to evaluate aspects of the VP activity in terms of good/bad rather than sharing their experiences in order to elicit its meaning and structure. The connection in time and space to the clinic may have contributed to this tendency. The benefit of this connection was the close relation to respondents’ life-world as students at the clinic. The richness of data in conjunction with the phenomenological attitude contributes to the internal validity in this respect.
This study was performed in a clinical rheumatology setting with students in their early clinical years. To what extent are the results reported here valid in other contexts? There are technical variations in VPs and how these are implemented (Huwendiek et al. 2009). The essence and attributes found here do not necessarily appear in other contexts, where also other possible attributes may appear. External validity in this kind of research is contingent on context similarity where the reader forms a part of the validating process (Larsson 2009). We believe that this study context has sufficient similarities with other clinical contexts to contribute to a further understanding of VPs as an educational tool.
References
Bearman, M. (2003). Is virtual the same as real? Medical students’ experiences of a virtual patient. Academic Medicine, 78(5), 538–545.
Bergin, R., Youngblood, P., Ayers, M. K., Boberg, J., Bolander, K., Courteille, O., et al. (2003). Interactive simulated patient: Experiences with collaborative e-learning in medicine. Journal of Educational Computing Research, 29(3), 387–400.
Berman, N. B., Fall, L. H., Maloney, C. G., & Levine, D. A. (2008). Computer-assisted instruction in clinical education: a roadmap to increasing CAI implementation. Advances in Health Sciences Education Theory and Practice, 13(3), 373–383.
Berman, N., Fall, L. H., Smith, S., Levine, D. A., Maloney, C. G., Potts, M., et al. (2009). Integration strategies for using virtual patients in clinical clerkships. Academic Medicine, 84(7), 942–949.
Boud, D., & Prosser, M. (2002). Appraising new technologies for learning: A framework for development. Educational Media International, 39, 237–245.
Boud, D., & Walker, D. (1993). Barriers to reflection on experience. In D. Boud, R. Cohen, & D. Walker (Eds.), Using experience for learning. Bristol: Society for Research into Higher Education and Open University Press.
Bowen, J. L. (2006). Educational strategies to promote clinical diagnostic reasoning. New England Journal of Medicine, 355(21), 2217–2225.
Brown, J. S., Collins, A., & Duguid, P. (1989). Situated cognition and the culture of learning. Educational Researcher, 18(1), 32–42.
Bryce, D. A., King, N. J., Graebner, C. F., Myers, J. H. (1998). Evaluation of a diagnostic reasoning program (DxR): Exploring student perceptions and addressing faculty concerns. Journal of Interactive Media in Education, 98(1).
Colaizzi, P. F. (1978). Learning and existence. In R. S. Valle & M. King (Eds.), Existential-phenomenological alternatives for psychology (pp. 119–135). New York: Oxford U.P.
Cook, D. A. (2005). The research we still are not doing: An agenda for the study of computer-based learning. Academic Medicine, 80(6), 541–548.
Cook, D. A., Bordage, G., & Schmidt, H. G. (2008). Description, justification and clarification: A framework for classifying the purposes of research in medical education. Medical Education, 42(2), 128–133.
Cook, D. A., Erwin, P. J., & Triola, M. M. (2010). Computerized virtual patients in health professions education: A systematic review and meta-analysis. Academic Medicine, 85(10), 1589–1602.
Cook, D. A., & Triola, M. M. (2009). Virtual patients: A critical literature review and proposed next steps. Medical Education, 43(4), 303–311.
Dall’Alba, G., & Barnacle, R. (2005). Embodied knowing in online environments. Educational Philosophy and Theory, 37(5), 719–744.
de Leng, B. A., Muijtjens, A. M., & van der Vleuten, C. P. (2009). The effect of face-to-face collaborative learning on the elaboration of computer-based simulated cases. Simulation in Healthcare, 4(4), 217–222.
Dornan, T., Boshuizen, H., King, N., & Scherpbier, A. (2007). Experience-based learning: A model linking the processes and outcomes of medical students’ workplace learning. Medical Education, 41(1), 84–91.
Edelbring, S. (2010). A threefold framework for relating to innovations and technology in education: Learning from, with and about technology. In A. Bromage, L. Clouder, J. Thistlethwaite, & F. Gordon (Eds.), Interprofessional e-learning and collaborative work: Practices and technologies. Hershey: IGI Global.
Ellaway, R., Poulton, T., Fors, U., McGee, J. B., & Albright, S. (2008). Building a virtual patient commons. Medical Teacher, 30(2), 170–174.
Fern, E. F. (1982). The use of focus groups for idea generation: The effects of group size, acquaintanceship, and moderator on response quantity and quality. Journal of Marketing Research, 19(1), 1–13.
Friedman, C. P. (1994). The research we should be doing. Academic Medicine, 69(6), 455–457.
Gallagher, S., & Zahavi, D. (2008). The phenomenological mind: An introduction to philosophy of mind and cognitive science. London, New York: Routledge.
Giorgi, A. (1985). Phenomenology and psychological research. Pittsburgh: Duquesne University Press.
Heidegger, M. (1962). Being and time (1 English ed.). Oxford: Blackwell.
Huang, G. M. D., Reynolds, R. M. P. A., & Candler, C. M. D. (2007). Virtual patient simulation at US and Canadian medical schools. Academic Medicine, 82(5), 446–451.
Huwendiek, S., De Leng, B. A., Zary, N., Fischer, M. R., Ruiz, J. G., & Ellaway, R. (2009). Towards a typology of virtual patients. Medical Teacher, 31(8), 743–748.
Irby, D. M. (1994). Three exemplary models of case-based teaching. Academic Medicine, 69(12), 947–953.
Karlsson, G. (1993). Psychological qualitative research from a phenomenological perspective. Stockholm: Almqvist & Wiksell International.
Kenny, N. P., & Beagan, B. L. (2004). The patient as text: A challenge for problem-based learning. Medical Education, 38(10), 1071–1079.
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, N.J.: Prentice-Hall.
Larsson, S. (2009). A pluralist view of generalization in qualitative research. International Journal of Research & Method in Education, 32(1), 25–38.
Lou, Y., Abrami, P. C., & d’Apollonia, S. (2001). Small group and individual learning with technology: A meta-analysis. Review of Educational Research, 71(3), 449–521.
Marton, F., & Booth, S. (1997). Learning and awareness. Mahwah, N.J.: Erlbaum.
Merriënboer, J. J. V., & Sweller, J. (2010). Cognitive load theory in health professional education: Design principles and strategies. Medical Education, 44(1), 85–93.
Moustakas, C. (1994). Phenomenological research methods. Thousand Oaks: Sage.
Newble, D., Norman, G., & van der Vleuten, C. (2000). Assessing clinical reasoning. In J. Higgs & M. A. Jones (Eds.), Clinical reasoning in the health professions (2nd ed., pp. 156–168). Oxford: Butterworth-Heinemann.
Norman, G. (2005). Research in clinical reasoning: Past history and current trends. Medical Education, 39(4), 418–427.
Norman, G. (2006). Editorial—Less is more. Advances in Health Science Education Theory and Practice, 11(2), 111–114.
Sandroni, S. (1997). Enhancing clinical teaching with information technologies: What can we do right now? Academic Medicine, 72(9), 770–774.
Shotter, J. (1993). Conversational realities: Constructing life through language. London: Sage.
Sixsmith, J. A., & Sixsmith, A. J. (1987). Empirical phenomenology: Principles and method. Quality & Quantity, 21(3), 313–333.
Spencer, J. (2003). Learning and teaching in the clinical environment. BMJ, 326(7389), 591–594.
Wahlgren, C. F., Edelbring, S., Fors, U., Hindbeck, H., & Stahle, M. (2006). Evaluation of an interactive case simulation system in dermatology and venereology for medical students. BMC Medical Education, 6, 40.
Acknowledgments
We would like to thank Marika Kvarnström who managed the rotations and facilitaded the interview sessions. The first author wishes to acknowledge the constructive feedback on earlier drafts given by C. Van der Vleuten and J. Van Merriënboer at Maastricht University and at the CME doctoral seminar at Karolinska Institutet. Part of the analysis was presented at the AMEE conference in Malaga in 2009. This study has been made possible through the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Edelbring, S., Dastmalchi, M., Hult, H. et al. Experiencing virtual patients in clinical learning: a phenomenological study. Adv in Health Sci Educ 16, 331–345 (2011). https://doi.org/10.1007/s10459-010-9265-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-010-9265-0