Abstract
Objective
Acidosis is present in several pathological conditions where vasculogenesis takes place including ischemia, tumor growth and wound healing. We have previously demonstrated that acidosis induces human CD34+ cell apoptosis. Considering that endothelial colony-forming cells (ECFC) are a subpopulation of CD34+ cells and key players in vasculogenesis, in the present study we investigated the effect of acidosis on the survival and functionality of ECFC.
Approach and results
Endothelial colony-forming cells obtained by differentiation of human cord blood CD34+ cells in endothelial growth medium-2 for 14–21 days were exposed at pH 7.4, 7.0 or 6.6. We found that acidosis failed to induce ECFC apoptosis and, although an early reduction in proliferation, chemotaxis, wound healing and capillary-like tubule formation was observed, once the medium pH was restored to 7.4, ECFC proliferation and tubulogenesis were augmented. Stromal cell derived factor-1 (SDF1)-driven migration and chemokine receptor type 4 surface expression were also increased. The maximal proangiogenic effect exerted by acidic preconditioning was observed after 6 h at pH 6.6. Furthermore, preconditioned ECFC showed an increased ability to promote tissue revascularization in a murine model of hind limb ischemia. Immunoblotting assays showed that acidosis activated AKT and ERK1/2 and inhibited p38 pathways. Proliferation rises triggered by acidic preconditioning were no longer observed after AKT or ERK1/2 inhibition, whereas p38 suppression not only mimicked but also potentiated the effect of acidosis on ECFC tubule formation abilities.
Conclusions
These results demonstrate that acidic preconditioning greatly increases ECFC-mediated angiogenesis in vitro including ECFC proliferation, tubulogenesis and SDF1-driven chemotaxis and is a positive regulator of microvessel formation in vivo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The processes of effective endothelial repair and development of new vessels appear to require the contribution of both angiogenesis, which involves the migration and proliferation of mature endothelial cells in nearby tissues, and vasculogenesis, which is a process mediated by bone marrow (BM)-derived cells that have the potential to differentiate into mature endothelial cells and are collectively referred to as endothelial progenitor cells (EPC) [1]. Different cell populations have been determined to play roles in vasculogenesis, but only one population, called endothelial colony-forming cells (ECFC) (also known as late EPC), have been shown to possess all the characteristics of true endothelial progenitors and to form neovessels in vivo [2].
Emerging evidence indicates that cell therapy with culture expanded EPC can successfully promote neovascularization in ischemic tissue and both cultured and freshly isolated EPC have been used in multicenter placebo-controlled clinical trials [3, 4]. Intracoronary infusion of cultured human EPC in patients with recent myocardial infarction was associated with improvements in global left ventricular function and microvascular function [3]. Moreover, preclinical and clinical studies have shown that EPC-based treatment, alone or in combination with traditional treatments, hold promise to cure vessel diseases in patients with atherosclerosis and diabetes, thus providing novel concepts and therapeutic strategies for the treatment of various cardiovascular diseases [5–7]. Still, the limited availability of EPC in peripheral blood and BM and the evidence that several disease states reduce EPC number and/or function, has prompted the development or improvement of several strategies to optimize therapeutic outcomes including the ex vivo expansion and differentiation of EPC.
The poor viability of the migrated and local progenitor cells within the injured tissue is an additional limitation for a proper revascularization. The microenvironment, which is supposed to provide cell contacts, soluble growth factors and other chemical signals to support engraftment, might be conducive to cellular stress and death under inflammatory conditions. Acidosis, a typical feature of the inflammatory microenvironment, represents a threat to cell survival because a decrease in extracellular pH may cause intracellular acidification and subsequent activation of various cellular responses, including cell death. In fact, a variation of 0.1 in intracellular pH (pHi) can disrupt basic biological functions including, ATP production, protein synthesis, cell proliferation, migration and apoptosis [8–10].
The physiological range of pH values in blood is maintained between 7.36 and 7.44. However, these values may drop down to 6.5–6.0 in a variety of local or systemic pathological conditions where vasculogenesis takes place, including but not limited to ischemia, tumor growth, wound healing, diabetic ketoacidosis, major trauma and burns [11–15]. In this context, we have previously demonstrated that an exposure of human CD34+ cells to an acidic medium, even for as short a period of time as 30 s induces cell cycle arrest and apoptosis [16]. Considering the fact that ECFC are a subpopulation of CD34+ cells and key players of vasculogenesis, we investigated the effect of acidosis on the survival and functionality of ECFC in the present study. We found that acidosis failed to induce ECFC apoptosis and although an early reduction in their functions was observed, once the medium pH was restored to 7.4, several ECFC proangiogenic responses were significantly augmented. This procedure, known as acidic preconditioning, exerted a maximal effect after 6 h at pH 6.6 and significantly improved ECFC proliferation, stromal cell derived factor 1 (SDF1)-driven chemotaxis and capillary-like tubule formation as well as revascularization of the post-ischemic hind limb.
Materials and methods
Reagents
Endothelial basic medium-2 (EBM2) and endothelial growth medium-2 (EGM2) were purchased from Lonza (Walkersville, MD) (cat # CC-3162). Gelatin, FITC-Annexin V Apoptosis detection kit (cat # APOAF-50TST) and phosphatase subtrate (cat # P4744) were obtained from Sigma (St Louis, MO). Boyden micro chemotaxis (24-well) chambers were purchased from Costar (Avon, France). Vascular endothelial growth factor-A (VEGF) and stromal cell-derived factor-1 (SDF-1) were obtained from Abcys (Paris, France). Matrigel (cat # 356231), KI67 antigen (cat # 612472), the flow cytometry antibodies PE mouse anti-human monoclonal VEGF receptor 2 (VGFR2/KDR) (cat # 560872), CXCR4 (cat # 557145), PECAM (cat # 553370) and the matching IgG isotypes were from BD Biosciences (San Jose, CA). Nitrocellulose membranes were obtained from GE Healthcare (Buckinghamshire, UK). Mouse anti-phospho ERK1/2 (cat # sc-7383) (Tyr 204), rabbit anti-phospho p38 (Tyr 182) (cat # sc-101759) and goat anti-rabbit HRP (cat # sc-2004) were from Santa Cruz Biotechnology (Santa Cruz, CA). Rabbit anti-phospho AKT (Tyr 308) (cat # ab38449) was purchased from Abcam (Cambridge, UK), mouse anti-β-actin from BD Biosciences (cat # 612656) and goat anti-mouse HRP from Dako (Glostrup, Denmark). Inhibitors of p38 (SB-203580, cat# BML-EI286), ERK1/2 (U-0126, cat # BML-EI-282) and AKT (LY-294002, cat # BML-ST420) were from Enzo Life Sciences International, Inc. (San Diego, CA).
Endothelial progenitor cell culture
Umbilical cord blood was collected after normal, full-term deliveries with the informed consent of the mother and used within 24 h. This study was performed according to institutional guidelines (National Academy of Medicine, Argentina) and received prior approval by the institutional ethics committee. After collection, CD34+ cells were purified by positive immunoselection as previously described [16]. CD34+ cells (5 × 105/mL) were plated in 24-well gelatin-coated plastic culture dishes in EBM-2 containing fetal calf serum (FCS), hydrocortisone, human fibroblast growth factor (hFGF), VEGF, human long R3 insulin-like growth factor-1 (R3-IGF-1), ascorbic acid, human epidermal growth factor (hEGF), gentamicin, amphotericin-B and heparin (EGM-2). After 4 days in culture, nonadherent cells were removed by thorough washing. At day 12, when an ECFC colony became visible microscopically, cells were detached with trypsin–EDTA and expanded for further analysis. ECFC expansion and characterization was performed as previously described [17–20]. The ECFC phenotype was confirmed by the double positivity for DiI-AcLDL uptake and BS-1 lectin binding, the presence of Weibel–Palade bodies, the combined expression of endothelial markers (CD31, Tie-2, KDR, Flt-1, CD144) and the absence of leuko-monocytic markers such as CD14 and CD45. ECFC during the first 30 days of culture were used for experiments.
Endothelial colony-forming cells from peripheral blood were obtained, cultured and characterized using similar procedures, with minor modifications as previously described [21]. Briefly, PBMCs were obtained by Ficoll density gradient centrifugation from 30 ml of fresh venous peripheral blood, resuspended in EGM2 and seeded onto six-well tissue culture plates (5 × 106 cells/well) precoated with human fibronectin (1 µg/cm2). Culture medium was replaced daily and at day 18–21, when ECFC colonies became visible microscopically, cells were detached with trypsin–EDTA and expanded for further analysis.
Acidification protocol
The culture medium was acidified by addition of a precalculated volume of isotonic HCl (1 N). The pH of the medium was measured by an electrode at 37 °C and averaged 7.39 ± 0.04, 7.03 ± 0.03, 6.62 ± 0.03 (n = 3). Acid preconditioning was achieved by incubating ECFC in EGM2 at the desired pH for the indicated period of time and then the medium was replaced by fresh EGM2 adjusted to physiologic pH (7.4).
Measurement of apoptosis
Cell viability was determined by double staining with annexin V binding and propidium iodide (PI) using a commercial kit. ECFC (1.5 × 105) were washed and incubated for 30 min with FITC-labeled annexin V in binding buffer at 37 °C. After washing, cells were resuspended in a PI solution and immediately analyzed by flow cytometry [22].
Proliferation assay (pNPP)
The effect of different pH levels on ECFC proliferation was determined by measuring acid phosphatase activity after incubation with its chromogenic substrate pNPP (3 mg/ml) for 1 h at 37 °C. The reaction was stopped with NaOH (2 N) and spectrophotometrically read at 405 λ [18].
Chemotaxis assay
Chemotaxis was examined in 24-well Boyden micro chemotaxis chambers with 8-µm pore-size polyvinylpyrrolidone-free polycarbonate. ECFC (1.5 × 104) were resuspended in EBM2 supplemented with 5 % FCS (EBM2 5 % FCS) and placed in the upper chamber and allowed to migrate toward the lower chamber containing EBM2 5 % FCS (negative control), EGM2, EBM2 5 % FCS with SDF-1 or EBM2 5 % FCS with VEGF. Migration was allowed to proceed for 6 or 24 h at 37 °C with 5 % CO2. Cells remaining on the upper surface of the filters were mechanically removed and the filters were fixed with 1 % formaldehyde and stained with Giemsa. The number of migrated cells was determined by counting under a high-power microscope [17].
Scratch wound assay
Confluent ECFC monolayers were wounded by scraping with a pipette tip and the extent of cell migration into the wounded area was photographed under the microscope at different time points. The wound surface area was measured by analyzing the images with ImageJ software and the percentage of wound closure was calculated as [(wound area at 0 h − wound area at X h)/wound area at 0 h] * 100.
In vitro tube formation assay
Endothelial colony-forming cells were detached with trypsin–EDTA and seeded at a density of 1.5 × 104 cells/well on 96-well plates coated with growth factor-reduced basement membrane matrix (Matrigel). After 18 h, tubule structures were fixed with 4 % PFA for 30 min, dehydrated and then stained with Giemsa. Tube formation was examined by phase-contrast microscopy and the total number of branch points was quantified on the entire surface of each well by using ImageJ software [18].
Measurement of Ki antigen expression
Endothelial colony-forming cells were synchronized overnight in EBM2 with 1 % FCS and the simultaneous expression of the cell proliferation associated nuclear antigen Ki67 and DNA content (PI) was determined by flow cytometry [16]. The expression of Ki67 antigen is first observed during G1 and increases over the rest of the cell cycle, but is undetectable in G0 resting cells. Cells were fixed in 70 % ice-cold ethanol, washed, resuspended in EBM2 with 5 % FCS and immunostained using FITC-labeled anti-Ki67 for 30 min. After washing, cells were stained with PI (0.5 µg/ml) and immediately analyzed by flow cytometry.
Surface expression of CXCR4, KDR and PECAM
To evaluate CXCR4, KDR and PECAM expression, ECFC were stained with PE-conjugated monoclonal mouse antibodies against human KDR, CXCR4 or PECAM. Matched IgG isotypes were used as negative control. Acquisition was performed on a FACSCalibur flow cytometer and data were analyzed with FCS Express V3 software.
Murine model of hind limb ischemia
Seven-week-old male athymic nude mice were housed in a controlled environment with free access to water and standard diet. Animal care conformed to French guidelines (Services Vétérinaires de la Santé et de la Production Animale, Paris, France), and experiments were performed in keeping with the guidelines of the Paris-Descartes University Institutional Committee on Animal Care and Use (C75.06.02). The mice underwent surgery to induce unilateral hind limb ischemia as previously described [23, 24]. Briefly, animals were anesthetized by inhalation of isoflurane. The ligature was performed on the right femoral artery, 0.5 cm proximal to the bifurcation of the saphenous and popliteal arteries. ECFC (1 × 105) in saline solution or vehicle alone (negative control) were administered 5 h after occlusion in the retro-orbital plexus or directly into the ischemic muscle and the ischemic/normal limb blood flow ratio was determined on day 14 by using the laser Doppler perfusion imaging system PeriScan Pim3 (Perimed, Crappone, France).
Immunoblotting
Endothelial colony-forming cells were lysed with loading buffer (62.5 nM Tris–HCl pH 6.8, 25 % glycerol, 2 % SDS, 0.01 % bromophenol blue and 5 % 2-mercaptoethanol). Equal amounts of proteins were electrophoresed on a 10 % acrylamide gel by SDS-PAGE and electrotransferred to nitrocellulose membranes. After blocking, the membranes were incubated overnight at 4 °C with primary antibody (mouse anti-phospho ERK1/2 (Tyr 204), rabbit anti-phospho p38 (Tyr 182), rabbit anti-phospho AKT (Tyr 473) and mouse anti-β-actin) followed by an HRP-conjugated secondary antibody. Protein bands were visualized by using the ECL reaction. Immunoblotting results were semi-quantitated using Gel-Pro analyzer 3.1 software (Rockville, MD), and values from blot reprobes were used to normalize data for protein loads.
Statistical analysis
Data are expressed as mean ± SEM for all experiments. Significant differences (p < 0.05) were identified by ANOVA followed by Fisher’s protected least significant difference test. The GraphPad software package (PRISM Version 5.0, San Diego, CA) was used for all analyses.
Results
Dual effect of extracellular acidosis on ECFC proangiogenic functions
We have previously demonstrated that an acidic milieu is deleterious for hematopoietic progenitors (CD34+ cells) as it induces apoptosis and cell cycle arrest [16]. Based on these findings, we first analyze whether acidosis affects the lifespan of ECFC that were cultured in EGM2 adjusted to pH 7.4, 7.0 or 6.6. We found that while serum deprivation induced apoptosis of these progenitors, pH changes had no effect (Fig. 1a).
Effect of acidosis on ECFC survival and functionality. Cells were incubated in EBM2 (serum deprivation) or in EGM2 adjusted to pH 7.4, 7.0 or 6.6. a Apoptosis was measured at the indicated time points (hpi) at low pH by annexin-V and PI double staining and flow cytometric analysis (n = 4). b Angiogenic responses were determined at 6 and 24 hpi (n = 6). *p < 0.05 versus pH 7.4
We next analyzed the effect of acidosis on several proangiogenic responses such as proliferation/viability, migration, wound healing and tubulogenesis. Under these conditions, all the responses evaluated decreased in a pH-dependent manner when examined after 6 h post incubation (hpi). However, when similar responses were observed at 24 hpi, the inhibitory effect of acidosis on wound healing was less evident; the proliferation and migration were barely different from pH 7.4 and, unexpectedly, the capillary-like tubule formation was markedly augmented under acidic conditions (Fig. 1b). In the same line of evidence, flow cytometric analysis of the proliferation marker Ki67 antigen showed that while the cycle progression was markedly inhibited by low pH at 6 hpi, with an increased percentage of cells in G0 phase and a decreased percentage of cells in S/G2/M, the arrest was markedly lower at 18 hpi and completely surmounted by 24 hpi (Fig. 2a). Moreover, the proliferation of acidosis-exposed ECFC (percentage of cells in S/G2/M) was even higher than those cultured at normal pH at 48 hpi (Fig. 2a). Consistent with this observation, a significant increase in the total cell number was observed under acidic conditions after 48 h (Fig. 2b). Surprisingly, the proliferation rise was higher when cells were exposed at pH 6.6 versus pH 7.0; therefore, the rest of experiments were performed at pH 6.6.
Effect of acidosis on cell cycle progression and proliferation of ECFC. Cells were incubated in EGM2 adjusted to pH 7.4, 7.0 or 6.6. a Cell cycle progression was analyzed at indicated time points (hpi) by Ki-67 antigen and PI double staining and flow cytometry (n = 4). b Cell counts were performed using a Neubauer chamber at indicated time points (hpi) (n = 5). *p < 0.05 versus pH 7.4
Acidic preconditioning increased proliferation and capillary-like tubule formation abilities
To explain the dual effect of acidosis on ECFC functions, we next measured the pH levels in the culture medium at different time points after acidification. We found that pH levels remained steady for the first 6–8 h and then slowly increased and approached normal values at 48 h post acidification (Fig. 3a). Based on these results, we theorized that although acidosis initially induces cell arrest, once the pH is balanced, the ECFC exposed to acidic medium exhibit an increased capacity in their proangiogenic responses. To determine whether ECFC proangiogenic responses were improved by acidic preconditioning, cells were cultured in acidic EGM2 for the indicated period of time, and then the medium was replaced by fresh EGM2 at pH 7.4. We first performed a kinetic study of capillary-like tubule formation to determine the minimum time of exposure to an acid milieu required to observe the maximum proangiogenic effect. We observed that 15 min or 1 h was not enough to induce any changes in ECFC functionality (Fig. 3b). In fact, although a significant increase in tubule formation was observed after 3 h of incubation in acidic medium, the maximal proangiogenic effect was detected after 6 h (Fig. 3b). Similar results were observed when ECFC proliferation was assessed (Fig. 3c).
Acidic preconditioning increased proliferation and capillary-like tubule formation abilities. a Cells were incubated in EGM2 adjusted to pH 7.4 or 6.6 and pH levels were measured at different hpi using a pHmeter (n = 3). b Cells were cultured in normal or acidic EGM2 for the indicated time and then seeded on matrigel in fresh EGM2 adjusted to pH 7.4. After 24 h, the number of branch points was measured by analyzing the images with ImageJ. *p < 0.05 versus pH 7.4 (n = 6). c Cells were cultured in acidic EGM2 for the indicated time and then the medium was replaced by fresh EGM2 adjusted to pH 7.4. After 48 h, cell proliferation was determined by the colorimetric pNPP assay (n = 3). *p < 0.05 vs pH 7.4
SDF1 induced chemotaxis and CXCR4 expression are augmented in preconditioned ECFC
Having determined the optimal time of exposure to low pH, we next evaluated other ECFC proangiogenic functions under these conditions. Figure 4a shows that acidic preconditioning failed to modulate migration in response to EGM2 or VEGF alone. Considering that the interaction between the chemokine receptor type 4 (CXCR4) and its ligand SDF1 plays a pivotal role in precursor cell migration and homing and have been involved in the acidosis-mediated proangiogenic effect [25], we next examined the effect of low pH on SDF1-driven chemotaxis. In contrast to EGM2 or VEGF, SDF1-induced chemotaxis was highly augmented in ECFC exposed to an acidic extracellular medium (Fig. 4a). Consistent with these observations, a significant increase in the expression of the SDF1 receptor CXCR4, but not in the VEGF receptor KDR or PECAM, was observed after acidic preconditioning (Fig. 4b).
SDF1-induced chemotaxis and CXCR4 expression are increased in preconditioned ECFC. Cells were incubated in EGM2 adjusted to pH 7.4 or 6.6 for 6 h and then the medium was replaced by fresh EGM2 at pH 7.4. a Migration in response to EGM2, SDF1 (20 ng/mL) and VEGF (20 ng/mL) were determined by seeding the cells in Boyden chemotaxis chambers. After 24 h, the number of migrated cells was counted under the light microscope (n = 4–5). b Expression of CXCR4, KDR and PECAM was determined after 24 h by flow cytometry (n = 4). *p < 0.05 versus pH 7.4
Peripheral blood-derived ECFC also showed an increased angiogenic activity after acidic preconditioning
Although there is a general consensus that ECFC derived from cord blood display the most robust clonal proliferative potential and generate more durable and functional blood vessels in vivo than peripheral blood ECFC [26, 27], the possibility to produce a good amount of autologous EPC with an enhanced therapeutic potential remains a challenge. To elucidate whether the proangiogenic effect of acidosis was also effective in adult ECFC, we performed experiments with ECFC isolated from peripheral blood. Although the proliferation rate of these progenitors was lower than the cord blood-derived cells, a slight but significant increase in total cell number was induced by acidic preconditioning (Fig. 5a). Moreover, tubulogenesis and SDF1-mediated chemotaxis were also highly augmented when these progenitors were exposed at pH 6.6 vs. pH 7.4 (Fig. 5b, c).
Acidic preconditioning improved peripheral blood-derived ECFC angiogenic activity. Cells were incubated in EGM2 adjusted to pH 7.4 or 6.6 for 6 h and then the medium was replaced by fresh EGM2 at pH 7.4. a Cell counts were performed using a Neubauer chamber at indicated time points (hpi) (n = 4). b Cells were seeded on matrigel and the number of branch points was measured after 24 h by analyzing the images with ImageJ (n = 3). c Migration in response to SDF1 (20 ng/mL) was determined by seeding the cells in Boyden chemotaxis chambers. After 24 h, the number of migrated cells was counted under the light microscope (n = 3). *p < 0.05 versus pH 7.4
Acidic preconditioning increased ECFC-mediated revascularization of the postischemic hind limb
Zemani et al. [17] showed that cord blood-derived ECFC are capable of enhancing neovascularization in a murine hind limb ischemia model. The results presented so far, which demonstrated that in vitro ECFC proangiogenic responses were augmented by acidic preconditioning, prompted us to evaluate the regenerative potential of ECFC in vivo. Although untreated control animals showed poor hind limb perfusion after ischemia (relative perfusion: 27.5 ± 4.5 %), the intravenous administration of ECFC improved relative limb perfusion to 37.2 ± 6.5 % (Fig. 6a). Most important, animals displayed even further and significant improvements in limb perfusion after systemic infusion of preconditioned ECFC (55.5 ± 4.1 %, p < 0.05 vs. control, p < 0.05 vs. untreated ECFC) (Fig. 6a). In order to elucidate whether these progenitors were more angiogenic or the increased blood perfusion in the ischemic muscle was associated to a difference in cell homing, were repeated the experiments by performing intramuscular injection of ECFC. As shown in Fig. 6, similar results were observed regardless the administration route (intramuscular injection of ECFC at pH 7.4: 45.1 ± 4.2 %, ECFC at pH 6.6: 64.7 ± 7.2 % p < 0.05) (Fig. 6b).
Acidic preconditioning enhanced ECFC-mediated neovascularization in hind limb ischemia. Cells were incubated in EGM2 adjusted to pH 7.4 or 6.6 for 6 h and then detached, washed and resuspended in saline solution before transplantation. Saline solution, ECFC preincubated at pH 7.4, or ECFC preincubated at pH 6.6 were administered intravenously (a) or intramuscularly (b) and Doppler analysis was performed after 14 days. Representative photomicrographs and quantitative analysis (perfusion index) are shown. Values are expressed as the mean ± SEM (n = 6 per group). *p < 0.05 versus ECFC (pH 7.4)
Intracellular signaling pathways involved in the proangiogenic effect of acidosis
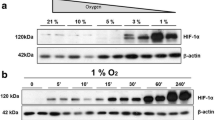
To analyze the mechanism involved in the proangiogenic effects of acidic preconditioning, some of the classical intracellular signaling pathways involved in angiogenic functions of endothelial cells including ERK1/2, PI3 K/AKT and p38 were studied [28–30]. Figure 7a shows that the exposure of ECFC to an acid growth factor-deprived basic medium (EBM2) induced higher phosphorylation levels of AKT and ERK1/2, but not p38, than those observed in ECFC at pH 7.4 (Fig. 7a). Furthermore, preconditioned ECFC potentiated the activation of both pathways triggered by EGM2, whereas p38 phosphorylation was completely suppressed (Fig. 7a). These data led us to hypothesize that the proangiogenic effects of acidic preconditioning is mediated by AKT and ERK1/2 activation as well as an inhibitory action on p38.
Intracellular signaling pathways involved in the proangiogenic effect of acidosis. a Cells were previously incubated in EGM2 adjusted to pH 7.4 or 6.6 for 6 h and then the medium was replaced by fresh EBM2 or EGM2 at pH 7.4. The phosphorylation levels of ERK1/2, AKT or p38 were detected after 2 min by immunoblotting. Each membrane was reprobed with anti-actin antibody to calculate the relative IOD using Gel-Pro software (n = 3–5). *p < 0.05 versus EBM2 at pH 7.4, # p < 0.05 versus EBM2 at pH 6.6 and & p < 0.05 versus EGM2 at pH 7.4. b, c, d Cells were incubated in EGM2 adjusted to pH 7.4 or 6.6 for 6 h in the presence or absence of the inhibitors of ERK1/2 (U0126), AKT (LY294002) or p38 (SB203580). Proliferation and capillary-like tubule formation were determined after 48 and 24 h, respectively (n = 4–6). *p < 0.05 versus EGM2 at pH 7.4, # p < 0.05 versus EGM2 at pH 6.6
To test this hypothesis, the next set of experiments were performed with acidic preconditioning in the presence of the pharmacological inhibitors of AKT (LY294002), ERK1/2 (U0126) or p38 (SB203580), and after 6 h, the culture medium was replaced by fresh EGM2 to remove the inhibitory compounds and to restore the pH level to 7.4. The drug concentration used effectively suppressed phosphorylation of the corresponding kinases and no significant differences in their inhibitory activity were observed between normal and acidic conditions (data not shown). We found that while AKT and ERK1/2 suppression significantly inhibited ECFC proliferation activity at pH 7.4, p38 blockade had no effect (Fig. 7b). Interestingly, the increased cell proliferation triggered by acidic preconditioning was no longer observed after the inhibition of AKT or ERK1/2, but not p38 (Fig. 7b), indicating that these two pathways are the main mediators of positive regulation for ECFC proliferation triggered by acidosis.
In contrast, ECFC capillary-like tubule formation capability was not mediated by AKT or ERK1/2 and it was negatively regulated by the p38 pathway. The suppression of p38 not only mimicked the effect of acidic preconditioning by augmenting the number of branch points at pH 7.4 but also potentiated the proangiogenic effect of acidosis by further increasing the tubule formation abilities of preconditioned ECFC (Fig. 7c, d). Altogether, these data indicate that acidic preconditioning of ECFC significantly improves their proangiogenic responses, such as proliferation and capillary-like tubule formation, through AKT and ERK1/2 activation and p38 suppression, respectively.
Discussion
The present study shows that exposure of ECFC to an acidic medium has a dual effect on cell function. While incubation of ECFC in low pH conditions initially induces reduction in proliferation, chemotaxis, wound healing and capillary-like tubule formation, a limited exposure of ECFC to an acidic milieu followed by restoration of the pH values to 7.4 (a procedure known as acidic preconditioning) results in more efficient ex vivo expansion of ECFC, which then exhibit enhanced chemotactic response to SDF1, capillary-like tubule formation abilities in vitro and therapeutic potential as demonstrated in a murine model of hind limb ischemia.
We here found that several angiogenic responses were decreased during the first hour of incubation at low pH, including EGM2-induced migration, wound healing, capillary-like tubule formation and proliferation, reflected by a reduction in the phosphatase acid activity and a drastic cell cycle arrest. A similar cytostatic effect has been reported by D’Arcangelo D. et al. in bovine aortic endothelial cells that were exposed to pH 7.0 for 20 min, which was accompanied by an extensive inhibition of endothelial angiogenic behavior [31]. Conversely, our findings indicated that the early ECFC functional impairment exerted by acidosis is fully reversible, because proliferation as well as other angiogenic properties was significantly augmented once the medium pH is balanced an approaches normal values.
Cell preconditioning is an endogenous protective mechanism where tissues can sense and adapt to the environment by changing their cellular phenotype and function through the exposure to a particular stress, such as hypoxia, anoxia, acidosis, heat shock, cytokines and pharmacological treatments, prior to cell injection into the damaged tissue [25]. It has been adopted as a strategy to improve the therapeutic potential of all sorts of stem and progenitor cells including ECFC [19]. Brief episodes of acidosis are known to limit ischemia/reperfusion injury in the heart [32] and lung [33] in vivo, and to exert antiapoptotic effects on endothelial cells [34, 35] and neurons [36], in vitro. Studies examining acidic preconditioning of stem and progenitor cells are scarce and controversial. In agreement with our present findings, Cencioni et al. [37] demonstrated that while apoptosis was induced in murine BM-derived hematopoietic progenitor (cKit+) cells by a long exposure (3–5 days) to an acidic extracellular medium, a shorter period of acidosis (24 h) increased chemotaxis, transendothelial migration, differentiation toward endothelial lineage in vitro and accelerated blood flow recovery in a mouse model of hind limb ischemia. In contrast, we have previously shown that the exposure of human hematopoietic progenitor (CD34+) cells to an acidic environment for as little as 30 s was sufficient to trigger apoptosis, and restoration of pH to the physiologic value of 7.4 failed to rescue them from death and had no beneficial effects on CD34+ cell functions [16]. These results are in contrast not only with the study performed with murine progenitors, where the discrepancies are most likely due to differences between species, but also with our present data showing that acidosis not only failed to induce ECFC apoptosis but also enhanced their proangiogenic properties. These data suggest that although ECFC are a subpopulation of CD34 + cells, the most advanced stage of differentiation toward the endothelial lineage most likely confers greater resistance to the cytotoxic effects of a low pH environment.
In the present work, we observed that acidic preconditioning failed to modulate either ECFC migration in response to EGM2 or VEGF alone or the expression levels of the VEGF receptor KDR. These results are consistent with those published by Goerges et al. [38], which showed that surface expression of VEGF receptors 1 and 2 (KDR) in bovine aortic endothelial cells is not modified by changes in extracellular pH. Moreover, we demonstrated that acidic preconditioning enhanced ECFC migration in response to the chemokine SDF1; this effect was associated with a higher surface expression of its receptor, CXCR4. In agreement with our findings, it has been reported that the exposure of murine BM hematopoietic progenitor (ckit+) cells to an acidic extracellular medium enhanced their proangiogenic responses and therapeutic potential through an increase in SDF1 and CXCR4 expression [37]. Although the role of the SDF-1/CXCR4 in hypoxic preconditioning of stem and progenitor cells has been recognized in several studies [25], we here elucidated for the first time that this signaling pathway is involved in the proangiogenic effect of acidic preconditioning in human ECFC.
While it has been extensively described that acidic preconditioning effectively protects organs/cells against ischemia [32–35], the molecular mechanisms involved are not completely understood. Our results showed that acidic preconditioning of ECFC increased ERK1/2 and AKT phosphorylation and that both pathways were responsible for increased ECFC proliferative activity, because the pharmacological inhibition of these molecules resulted in a complete blockade of the mitogenic effect triggered by low pH. Interestingly, the activation of these two kinases by acidification has been previously reported in coronary endothelial cells although it was linked to the antiapoptotic effect of acidosis [34, 35]. In agreement with our data, upregulation of ERK1/2 and PI3 K/AKT phosphorylation by several proliferation-inducing ligands has been extensively described in several cell types including EPC [28, 39, 40]. In contrast, we found that the p38 activation by EGM2 was fully blocked at pH 6.6. However, pretreatment with the p38 inhibitor SB203580, had no effect on ECFC proliferation. In this sense, although the role of p38 on the proliferation of EPC is still controversial, most of the studies using SB203580, in vitro and in vivo, have described a negative effect of this drug not only on cell growth and survival but also on tubulogenesis [41–44]. Interestingly, we also found that p38 blockade increased tubulogenesis in vitro at pH 7.4, suggesting that p38 pathway is a negative regulator of ECFC tubule formation and the fact that this molecule was completely suppressed in preconditioned ECFC explained, at least in part, the positive regulation of acidic preconditioning on microvessel formation.
The relevance of our in vitro findings was confirmed by the in vivo experiments. In fact, although the infusion of ECFC significantly ameliorates blood flow in an experimental model of limb-ischemia, acidic preconditioning of the cells further improved neovascularization. Our data showing that a similar perfusion rate was observed in the ischemic tissue after systemic (intravenous) or local (intramuscular) infusion of ECFC suggest that preconditioned ECFC display a high proangiogenic activity that contributes directly to neovessel formation in the ischemic tissue regardless their homing ability. On the other hand, whether the ECFC contribute structurally to the ischemic muscle revascularization or through a paracrine effect remains to be determined. EPC can support neovessel formation in vivo through three different mechanisms [45]: (1) they form new vessels by themselves, (2) they insert into the murine endothelial lining of the murine vasculature, or (3) they exert a paracrine effect. Since we have previously demonstrated in the same model of ischemia that ECFC are integrated into the new murine vessels [46], it is conceivable that preconditioned ECFC exhibit a similar behavior and contribute structurally to this process. Nevertheless, although it has been reported that late outgrowth EPC such as ECFC exert no significant paracrine angiogenic effect [26, 45] the possibility that acidosis increases the paracrine action of these cells is being currently studied in our laboratory.
In conclusion, our results show that a limited exposure of ECFC to low pH levels augment the angiogenic activity of these progenitor cells through upregulation of ERK1/2 and AKT pathways and inhibition of the p38 pathway. In addition to suggesting a possible compensating pathophysiologic mechanism that occurs during several inflammatory conditions, our findings could offer a new strategy for regenerative medicine. In this context, cell therapy is a promising tool to treat ischemic diseases; however, much work still needs to be done to overcome the transplant limitations. It is well known that the number and function of EPC are reduced in patients with cardiovascular diseases and by the hostile milieu surrounding the ischemic tissues. Multiple strategies are currently focused on improving cell number, survival, angiogenic properties and engraftment (e.g., several preconditioning protocols, genetic modifications, drug administration). We here show that acidic preconditioning represents a simple, inexpensive and clinically applicable strategy to improve ex vivo expansion of ECFC, which in turn exhibit a greater therapeutic potential. Moreover, our data showing that acidosis positively regulates ECFC functionality derived not only from cord blood but also from peripheral blood point out acidic preconditioning as a useful procedure for improving the angiogenic activity of autologous ECFC. Nevertheless, whether this approach increases the functionality of EPC of cardiovascular risk patients remains to be determined. Additionally, our findings highlight the use of pharmacological drugs targeting p38 blockade as a potential strategy for improving neovascularization.
Abbreviations
- CXCR4:
-
Chemokine receptor type 4
- EBM-2:
-
Endothelial basic medium-2
- ECFC:
-
Endothelial colony-forming cells
- EGM-2:
-
Endothelial growth medium-2
- EPC:
-
Endothelial progenitor cells
- Hpi:
-
Hours post incubation
- SDF-1:
-
Stromal cell derived factor-1
- VEGF:
-
Vascular endothelial growth factor
References
Jujo K, Ii M, Losordo DW (2008) Endothelial progenitor cells in neovascularization of infarcted myocardium. J Mol Cell Cardiol 45:530–544
Critser PJ, Yoder MC (2010) Endothelial colony-forming cell role in neoangiogenesis and tissue repair. Curr Opin Organ Transplant 15:68–72
Assmus B, Schachinger V, Teupe C, Britten M, Lehmann R, Dobert N, Grunwald F, Aicher A, Urbich C, Martin H, Hoelzer D, Dimmeler S, Zeiher AM (2002) Transplantation of progenitor cells and regeneration enhancement in acute myocardial infarction (TOPCARE-AMI). Circulation 106:3009–3017
Sinha S, Poh KK, Sodano D, Flanagan J, Ouilette C, Kearney M, Heyd L, Wollins J, Losordo D, Weinstein R (2006) Safety and efficacy of peripheral blood progenitor cell mobilization and collection in patients with advanced coronary heart disease. J Clin Apher 21:116–120
Fadini GP, Avogaro A (2010) Potential manipulation of endothelial progenitor cells in diabetes and its complications. Diabetes Obes Metab 12:570–583
Werner N, Priller J, Laufs U, Endres M, Bohm M, Dirnagl U, Nickenig G (2002) Bone marrow-derived progenitor cells modulate vascular reendothelialization and neointimal formation: effect of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibition. Arterioscler Thromb Vasc Biol 22:1567–1572
Raval Z, Losordo DW (2013) Cell therapy of peripheral arterial disease: from experimental findings to clinical trials. Circ Res 112:1288–1302
Trevani AS, Andonegui G, Giordano M, Lopez DH, Gamberale R, Minucci F, Geffner JR (1999) Extracellular acidification induces human neutrophil activation. J Immunol 162:4849–4857
Serrano CV Jr, Fraticelli A, Paniccia R, Teti A, Noble B, Corda S, Faraggiana T, Ziegelstein RC, Zweier JL, Capogrossi MC (1996) pH dependence of neutrophil-endothelial cell adhesion and adhesion molecule expression. Am J Physiol 271:C962–C970
Martinez D, Vermeulen M, von Euw E, Sabatte J, Maggini J, Ceballos A, Trevani A, Nahmod K, Salamone G, Barrio M, Giordano M, Amigorena S, Geffner J (2007) Extracellular acidosis triggers the maturation of human dendritic cells and the production of IL-12. J Immunol 179:1950–1959
DeClerck K, Elble RC (2010) The role of hypoxia and acidosis in promoting metastasis and resistance to chemotherapy. Front Biosci (Landmark Ed) 15:213–225
Huang Y, McNamara JO (2004) Ischemic stroke: “acidotoxicity” is a perpetrator. Cell 118:665–666
Lim S (2007) Metabolic acidosis. Acta Med Indones 39:145–150
Cronberg T, Rytter A, Asztely F, Soder A, Wieloch T (2004) Glucose but not lactate in combination with acidosis aggravates ischemic neuronal death in vitro. Stroke 35:753–757
Smith ML, von Hanwehr R, Siesjo BK (1986) Changes in extra- and intracellular pH in the brain during and following ischemia in hyperglycemic and in moderately hypoglycemic rats. J Cereb Blood Flow Metab 6:574–583
D’Atri LP, Etulain J, Romaniuk MA, Torres O, Negrotto S, Schattner M (2011) The low viability of human CD34+ cells under acidic conditions is improved by exposure to thrombopoietin, stem cell factor, interleukin-3, or increased cyclic adenosine monophosphate levels. Transfusion 51:1784–1795
Zemani F, Benisvy D, Galy-Fauroux I, Lokajczyk A, Colliec-Jouault S, Uzan G, Fischer AM, Boisson-Vidal C (2005) Low-molecular-weight fucoidan enhances the proangiogenic phenotype of endothelial progenitor cells. Biochem Pharmacol 70:1167–1175
Benslimane-Ahmim Z, Heymann D, Dizier B, Lokajczyk A, Brion R, Laurendeau I, Bieche I, Smadja DM, Galy-Fauroux I, Colliec-Jouault S, Fischer AM, Boisson-Vidal C (2011) Osteoprotegerin, a new actor in vasculogenesis, stimulates endothelial colony-forming cells properties. J Thromb Haemost 9:834–843
Zemani F, Silvestre JS, Fauvel-Lafeve F, Bruel A, Vilar J, Bieche I, Laurendeau I, Galy-Fauroux I, Fischer AM, Boisson-Vidal C (2008) Ex vivo priming of endothelial progenitor cells with SDF-1 before transplantation could increase their proangiogenic potential. Arterioscler Thromb Vasc Biol 28:644–650
Benslimane-Ahmim Z, Poirier F, Delomenie C, Lokajczyk A, Grelac F, Galy-Fauroux I, Mohamedi A, Fischer AM, Heymann D, Lutomski D, Boisson-Vidal C (2013) Mechanistic study of the proangiogenic effect of osteoprotegerin. Angiogenesis 16:575–593
Della Bella S, Taddeo A, Calabro ML, Brambilla L, Bellinvia M, Bergamo E, Clerici M, Villa ML (2008) Peripheral blood endothelial progenitors as potential reservoirs of Kaposi’s sarcoma-associated herpesvirus. PLoS One 3:e1520
Negrotto S, Pacienza N, D’Atri LP, Pozner RG, Malaver E, Torres O, Lazzari MA, Gomez RM, Schattner M (2006) Activation of cyclic AMP pathway prevents CD34(+) cell apoptosis. Exp Hematol 34:1420–1428
Foubert P, Silvestre JS, Souttou B, Barateau V, Martin C, Ebrahimian TG, Lere-Dean C, Contreres JO, Sulpice E, Levy BI, Plouet J, Tobelem G, Le Ricousse-Roussanne S (2007) PSGL-1-mediated activation of EphB4 increases the proangiogenic potential of endothelial progenitor cells. J Clin Invest 117:1527–1537
Sarlon G, Zemani F, David L, Duong Van Huyen JP, Dizier B, Grelac F, Colliec-Jouault S, Galy-Fauroux I, Bruneval P, Fischer AM, Emmerich J, Boisson-Vidal C (2012) Therapeutic effect of fucoidan-stimulated endothelial colony-forming cells in peripheral ischemia. J Thromb Haemost 10:38–48
Cencioni C, Capogrossi MC, Napolitano M (2012) The SDF-1/CXCR4 axis in stem cell preconditioning. Cardiovasc Res 94:400–407
Yoder MC, Mead LE, Prater D, Krier TR, Mroueh KN, Li F, Krasich R, Temm CJ, Prchal JT, Ingram DA (2007) Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood 109:1801–1809
Au P, Daheron LM, Duda DG, Cohen KS, Tyrrell JA, Lanning RM, Fukumura D, Scadden DT, Jain RK (2008) Differential in vivo potential of endothelial progenitor cells from human umbilical cord blood and adult peripheral blood to form functional long-lasting vessels. Blood 111:1302–1305
Cross MJ, Claesson-Welsh L (2001) FGF and VEGF function in angiogenesis: signalling pathways, biological responses and therapeutic inhibition. Trends Pharmacol Sci 22:201–207
Morello F, Perino A, Hirsch E (2009) Phosphoinositide 3-kinase signalling in the vascular system. Cardiovasc Res 82:261–271
Gerwins P, Skoldenberg E, Claesson-Welsh L (2000) Function of fibroblast growth factors and vascular endothelial growth factors and their receptors in angiogenesis. Crit Rev Oncol Hematol 34:185–194
D’Arcangelo D, Facchiano F, Barlucchi LM, Melillo G, Illi B, Testolin L, Gaetano C, Capogrossi MC (2000) Acidosis inhibits endothelial cell apoptosis and function and induces basic fibroblast growth factor and vascular endothelial growth factor expression. Circ Res 86:312–318
Fujita M, Asanuma H, Hirata A, Wakeno M, Takahama H, Sasaki H, Kim J, Takashima S, Tsukamoto O, Minamino T, Shinozaki Y, Tomoike H, Hori M, Kitakaze M (2007) Prolonged transient acidosis during early reperfusion contributes to the cardioprotective effects of postconditioning. Am J Physiol Heart Circ Physiol 292:H2004–H2008
Costello J, Higgins B, Contreras M, Chonghaile MN, Hassett P, O’Toole D, Laffey JG (2009) Hypercapnic acidosis attenuates shock and lung injury in early and prolonged systemic sepsis. Crit Care Med 37:2412–2420
Flacke JP, Kumar S, Kostin S, Reusch HP, Ladilov Y (2009) Acidic preconditioning protects endothelial cells against apoptosis through p38- and Akt-dependent Bcl-xL overexpression. Apoptosis 14:90–96
Kumar S, Reusch HP, Ladilov Y (2008) Acidic pre-conditioning suppresses apoptosis and increases expression of Bcl-xL in coronary endothelial cells under simulated ischaemia. J Cell Mol Med 12:1584–1592
Froyland E, Skjaeret C, Wright MS, Dalen ML, Cvancarova M, Kasi C, Rootwelt T (2008) Inflammatory receptors and pathways in human NT2-N neurons during hypoxia and reoxygenation. Impact of acidosis. Brain Res 1217:37–49
Cencioni C, Melchionna R, Straino S, Romani M, Cappuzzello C, Annese V, Wu JC, Pompilio G, Santoni A, Gaetano C, Napolitano M, Capogrossi MC (2011) Ex vivo acidic preconditioning enhances bone marrow ckit+ cell therapeutic potential via increased CXCR4 expression. Eur Heart J 34:2007–2016
Goerges AL, Nugent MA (2003) Regulation of vascular endothelial growth factor binding and activity by extracellular pH. J Biol Chem 278:19518–19525
Kucia M, Jankowski K, Reca R, Wysoczynski M, Bandura L, Allendorf DJ, Zhang J, Ratajczak J, Ratajczak MZ (2004) CXCR4-SDF-1 signalling, locomotion, chemotaxis and adhesion. J Mol Histol 35:233–245
Everaert BR, Van Craenenbroeck EM, Hoymans VY, Haine SE, Van Nassauw L, Conraads VM, Timmermans JP, Vrints CJ (2010) Current perspective of pathophysiological and interventional effects on endothelial progenitor cell biology: focus on PI3K/AKT/eNOS pathway. Int J Cardiol 144:350–366
Seeger FH, Haendeler J, Walter DH, Rochwalsky U, Reinhold J, Urbich C, Rossig L, Corbaz A, Chvatchko Y, Zeiher AM, Dimmeler S (2005) p38 mitogen-activated protein kinase downregulates endothelial progenitor cells. Circulation 111:1184–1191
Wu Y, Wang Q, Cheng L, Wang J, Lu G (2009) Effect of oxidized low-density lipoprotein on survival and function of endothelial progenitor cell mediated by p38 signal pathway. J Cardiovasc Pharmacol 53:151–156
Kuki S, Imanishi T, Kobayashi K, Matsuo Y, Obana M, Akasaka T (2006) Hyperglycemia accelerated endothelial progenitor cell senescence via the activation of p38 mitogen-activated protein kinase. Circ J 70:1076–1081
Huh JE, Nam DW, Baek YH, Kang JW, Park DS, Choi DY, Lee JD (2011) Formononetin accelerates wound repair by the regulation of early growth response factor-1 transcription factor through the phosphorylation of the ERK and p38 MAPK pathways. Int Immunopharmacol 11:46–54
Sieveking DP, Buckle A, Celermajer DS, Ng MK (2008) Strikingly different angiogenic properties of endothelial progenitor cell subpopulations: insights from a novel human angiogenesis assay. J Am Coll Cardiol 51:660–668
Bouvard C, Gafsou B, Dizier B, Galy-Fauroux I, Lokajczyk A, Boisson-Vidal C, Fischer AM, Helley D (2010) Alpha6-integrin subunit plays a major role in the proangiogenic properties of endothelial progenitor cells. Arterioscler Thromb Vasc Biol 30:1569–1575
Acknowledgments
We thank C. Martin and the technicians from the IMTCE animal facilities (Paris Descartes University). We are also indebted to the nursing services of Hôpital des Diaconnesses (Paris) for providing umbilical cord blood samples. SN is financially supported by ANPCyT (PICT 1393/10) and CONICET (PIP 1142009010016301) and MS by ANPCyT (PICT 0733/11). CNRS pays the salary of C. Boisson-Vidal.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Mirta Schattner and Soledad Negrotto jointly supervised this study.
Rights and permissions
About this article
Cite this article
Mena, H.A., Lokajczyk, A., Dizier, B. et al. Acidic preconditioning improves the proangiogenic responses of endothelial colony forming cells. Angiogenesis 17, 867–879 (2014). https://doi.org/10.1007/s10456-014-9434-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-014-9434-5