Abstract
We have recently shown that aldose reductase (AR, EC 1.1.1.21) a nicotinamide adenine dinucleotide phosphate-dependent aldo–keto reductase, known to be involved in oxidative stress-signaling, prevents human colon cancer cell growth in culture as well as in nude mice xenografts. Inhibition of AR also prevents azoxymethane-induced aberrant crypt foci formation in mice. In order to understand the chemopreventive mechanism(s) of AR inhibition in colon cancer, we have investigated the role of AR in the mediation of angiogenic signals in vitro and in vivo models. Our results show that inhibition of AR significantly prevented the VEGF- and FGF -induced proliferation and expression of proliferative marker Ki67 in the human umbilical vein endothelial cells (HUVEC). Further, AR inhibition or ablation with siRNA prevented the VEGF- and FGF –induced invasion and migration in HUVEC. AR inhibition also prevented the VEGF- and FGF- induced secretion/expression of IL-6, MMP2, MMP9, ICAM, and VCAM. The anti-angiogenic feature of AR inhibition in HUVEC was associated with inactivation of PI3 K/AKT and NF-κB (p65) and suppression of VEGF receptor 2 protein levels. Most importantly, matrigel plug model of angiogenesis in rats showed that inhibition of AR prevented infiltration of blood cells, invasion, migration and formation of capillary like structures, and expression of blood vessels markers CD31 and vWF. Thus, our results demonstrate that AR inhibitors could be novel agents to prevent angiogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiogenesis, formation of new blood vessels by endothelial cells, is a highly complex and tightly regulated physiological process, implicated in various pathological diseases such as wound healing, tissue remodeling, thrombosis, rheumatoid arthritis, diabetic retinopathy and tumor growth [1–3]. Angiogenesis in tumors allows the growth and invasiveness of tumor cells leading to metastasis to distant organs [2–4]. Angiogenesis, especially in a solid tumor progression plays a critical role because when tumor mass increases beyond 2–3 mm, formation of new blood vessels is presumably essential in supplying nutrients and oxygen and removing waste products [1–3]. In angiogenesis the interaction of tumor cells with vascular endothelial cells leads to the release of various growth factors, cytokines, chemokines, etc. [4, 5]. These molecules in turn by autocrine and paracrine fashion activate inflammatory signaling leading to differentiation of vascular endothelial cells. In addition, the important concept of tumor angiogenesis is that in the tumor microenvironment tumor-associated endothelial cells are genetically unstable and show enhanced responsiveness to growth factors such as VEGF, FGF and EGF [4–6]. Therefore, antiangiogenic therapy represents one of the most promising approaches to regulate tumor growth and metastasis.
Various reports suggest that induction of angiogenic factors is triggered by various stresses, including oxidative stress [7]. For instance, reactive oxygen species (ROS) such as superoxide anions (O2−), hydroxyl radical (OH●), and H2O2 are generated via activated phagocytes under various pathological conditions, including inflammation, ischemia and reperfusion, sepsis and UV radiation [7–11]. The vascular endothelium is one of the prime targets of these inflammatory oxidants. Further, it has been shown that activation of redox sensitive transcription factors such as NF-κB and AP1 involved in transcribing various inflammatory genes that synthesize growth factors, cytokines, chemokines and matrix metalloproteases which cause endothelial cell growth, adhesion, invasion, migration and angiogenesis [7, 12–14]. NF-κB is the first eukaryotic transcription factor shown to respond directly to oxidative stress-mediated tumorigenesis and angiogenesis [12, 13]. Antioxidants such as N-acetyl cysteine, resveratrol, lycopene, green tea and epigallocatechin-3-gallate have been shown to attenuate the angiogenesis in various tumor microenvironments via inhibition of NF-κB [14–19]. Therefore, anti-angiogenic therapy by using anti-oxidants represents one of the most promising approaches to control tumor growth, invasion and angiogenesis. In fact, several antioxidants are under drug development programme and clinical trials to identify novel anti-angiogneic and anti-cancer agents. Our recent studies with human vascular umbilical endothelial cells (HUVEC) suggest that the polyol pathway enzyme- aldose reductase (AR; AKR1B1), a member of aldo–keto reductase super family, is a regulator of activation of NF-κB and expression of adhesion molecules, ICAM, VCAM induced by cytokines such as TNF-α [20, 21].
We have previously shown that AR besides reducing aldo-sugars efficiently catalyzes the reduction of lipid aldehydes such as 4-hydroxy-trans-2-nonenol (HNE) and their glutathione conjugates such as GS-HNE to 1, 4-dihydroxynonene (DHN) and GS-DHN, respectively with low (μM) Km compared to glucose with Km in mM range [22–24]. Further, we have demonstrated that inhibition of AR could prevent protein kinase C, NF-κB, and AP-1 activation and the increase in cell growth caused by HNE and GS-HNE, but not by GS-DHN [22–27]. These studies suggested that the already reduced form of glutathione-lipid aldehyde, GS-DHN is insensitive to AR inhibition and could be the main mediator of oxidative stress-induced NF-κB activation. Using human colon cancer Caco-2 cells we have demonstrated that AR inhibition as well as ablation by siRNA prevents the growth factors such as FGF- and PDGF-induced activation of NF-κB, expression of Cox-2 and production of PGE2 [22, 28]. Most remarkably, in the nude mice xenograft model, we have shown that inhibition of AR by ARsiRNA as well as by AR inhibitor, fidarestat completely prevented growth of human colon adenocarcinoma cells (SW480 and HT29) implanted subcutaneously [22, 28]. Further, recent results with azoxymethane (AOM) model in male BALB/c mice showed that the inhibition of AR by a pharmacological inhibitor as well as AR gene knockout in mice significantly prevented aberrant crypt foci formation and AOM-induced expression of inflammatory markers, iNOS and Cox-2 and preneoplastic marker proteins, cyclin D1 and beta-catenin and activation of NF-κB in mice colons [29]. However, the involvement of AR in the angiogenesis is unknown. Since NF-κB plays a key role in angiogenesis by regulating transcription of angiogenic growth factors (such as VEGF and FGF), we hypothesized that inhibition of AR could inhibit angiogenesis. We now show that inhibition of AR effectively prevents in vitro angiogenesis (capillary-like tube structure and spheroid formation, invasion and migration) of HUVEC by causing suppression of pro-angiogenic growth factor secretion and MMPs, and adhesion molecules’ expression and NF-κB activation. Further, our results show that inhibition of AR could prevent in vivo angiogenesis in a rat matrigel-plug model. These findings for the first time indicate that AR is an excellent novel therapeutic target for the prevention of angiogenesis.
Materials and methods
Chemicals and reagents
Ham’s F12 K, PBS, penicillin/streptomycin, trypsin, and fetal bovine serum (FBS) were purchased from Invitrogen (Carlsbad, CA). Antibodies against AKT, p65, MMP2, MMP9, VEGFR-2 and GAPDH were obtained from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA). Phospho-VEGFR-2 was purchased from Cell applications Inc (San Diego, CA). Anti-NO2-Tyr was purchased from EMD Biosciences, Gibbstown, NJ. Fidarestat was obtained as a gift from Sanwa Kagaku Kenkyusho Co. Ltd. (Japan). Cell invasion assay kit was obtained from Chemicon International Inc. (Billerica, MA). FGF and VEGF other reagents used in Western blot analysis were obtained from Sigma (St. Louis, MO). All other reagents used were of analytical grade.
Cell culture
Human umbilical vascular endothelial cells (HUVEC) were obtained from Cell Application Inc and grown in Ham’s F-12 K medium containing 10% FBS and cultured at 37°C under an atmosphere containing 5% CO2.
Measurement of cytotoxicity
HUVEC were plated in a 96-well plate at 2,500 per well and growth arrested in 0.1% FBS with or without AR inhibitor fidarestat (5 μM), or transfected with AR-siRNA or control siRNA using RNAiFect reagent (Qiagen). After 24 h, VEGF or FGF (10 ng/ml) was added to the medium and the cells were incubated for another 24 h. Cells incubated with the AR inhibitor alone served as control. Cell viability was determined by MTT assay as described earlier [22].
Tube formation assay
The endothelial cell tube-like formation assay was performed using HUVEC as described elsewhere [30, 31]. Briefly, fifty micro liters of reduced growth factors basement membrane extract (BME) solution was added to each well of 96 well plate and incubated at 37°C for 30 min to allow gel formation. HUVEC (7,500 cells/well) in Ham’s F12 K basal medium with or without VEGF/FGF (10 ng/ml) and/or AR inhibitor, fidarestat with different concentrations plated on BME gel. For AR siRNA and scrambled siRNA group, cells were transfected and plated on BME gel. After an overnight incubation, the network growth area was examined using an inverted microscope (50×).
Spheroid formation
Spheroid formation assay in HUVEC was performed as described elsewhere [30, 31]. Briefly, HUVEC (4,000/ml) were suspended in Ham’s F12 K containing 20% (v/v) methocel, seeded into non-adherent round-bottom 96-well plates and incubated overnight. The methocel used was prepared by dissolving 6 g of carboxymethylcellulose (Sigma–Aldrich) in 500 ml of Ham’s F-12 K. The spheroids were harvested by gently pipetting, centrifuged at 500 rpm for 5 min, and embedded into neutralized collagen gels with 1:1 ratio. The spheroids in collagen solution were rapidly transferred into 96-well plate and incubated at 37°C for 24 h with or without VEGF (10 ng/ml) and/or AR inhibitor, fiderestat (5 μM). The spheroid images were captured using a camera linked to an inverted microscope (50×).
Determination of Ki67 expression in HUVEC
HUVEC grown 70–80% confluent in T-25 flasks were pre-incubated for 24 h with and without fidarestat (5 μM) followed by stimulation with VEGF or FGF (10 ng/ml) for another 24 h. Expression of cell proliferation marker Ki-67 was determined by FACS analysis as per manufacturer’s instructions (BD Biosciences, San Jose, CA). HUVEC (1 × 106/ml) were fixed in 70–80% ethanol by incubating at −20°C for 2 h. Cells were washed with buffer (PBS with 1% FBS, pH7.2) and incubated with PE-conjugated ki67 mAb for 30 min. After washing HUVEC were diluted in BD Via-Probe™ cell viability solution and analyzed with a minimum of 10,000 events using Cell Quest version 3.3 software for data analysis (Becton–Dickinson, San Jose, CA).
Invasion and migration assays
Invasive assay was performed using Basement Membrane Extract. Fifty micro liters of BME solution was added on top of 8 micron polyethylene terephthalate membrane to each well of 96 well plate and incubated at 37°C for 4 h to allow gel formation. HUVEC (20,000 cells/well) in basal medium with or without VEGF (10 ng/ml) and/or AR inhibitor, fidarestat (5 μM) plated on Matrigel. After 24 h of incubation invasion of cells towards bottom side of the well was measured using Calcein-AM florescent dye. Migration of HUVEC was performed by scratch wound assay as described elsewhere [32].
Matrigel plug model in rats (in vivo angiogenesis)
Five hundred micro liters of matrigel (growth factor free) with or without VEGF (10 ng/ml) and/or fidarestat (20 μM) was injected subcutaneously (s.c.) into the dorsal tissue of Fischer 344 rats (n = 4/group) and AR inhibitor, fidarestat (16 mg/kg body weight) was given through drinking water [33]. After 1 week, rats were killed and plugs were excised and perfusion-fixed with 4% paraformaldehyde and stored in 70% ethanol. The fixed matrigels were stained with hematoxylin and eosin. Immunohistochemical analysis was performed by using monoclonal antibodies against CD31/PECAM-1 and von-Willebrand factor (vWF) using DakoCytomation LSAB + System-HRP kit. Stained sections were observed under Nikon epi-fluorescence microscope (200×).
Immunoprecipitations and Western blot analysis
To examine the expression/phosphorylation of TIMP-1, p-VEGFR2, VEGFR2, MMP2, MMP9, AKT, p-65 and GAPDH proteins, Western blot analysis was carried out. Equal amounts of protein from liver tissue extracts were subjected to 12% SDS–PAGE followed by transfer of proteins to nitrocellulose filters and probing with the indicated antibodies. The antigen–antibody complex was detected by enhanced chemiluminescence (Pierce, Piscataway, NJ). For immunoprecipitations, 50 mg of cell lysate protein was incubated overnight at 4°C with anti-nitrotyrosine antibody and the covalently coupled antigen–antibody complex were separated using Pierce classic IP kit from Thermo Scientific USA, by following the manufacturer’s instructions. The separated immune complexes were denatured at 95°C followed by SDS–PAGE and Western blotting using antibodies against AKT and PI3 K.
Determination of angiogenic factors-induced adhesion and matrix metalloproteinases in HUVEC by ELISA
HUVEC were grown confluent in 6 well plates and pre incubated with and without fidarestat for 24 h. Cells were treated with VEGF and FGF (10 ng/ml) for another 24 h and cell culture medium was subjected to ELISA analysis of VCAM, ICAM, IL-6, MMP2, MMP9 and IFN-γ using Ray Biotech ELISA kits as per the manufacturer’s instructions. Values were plotted against the standards obtained in the assay along with the experimental.
Determination of PI3 K activity
PI3 K activity in HUVEC was determined using a competitive ELISA kit (Echelon Biosciences, Inc., Salt Lake City, UT) as described previously [28]. Briefly, HUVEC cells were serum-starved for overnight with or without fidarestat and stimulated with VEGF (10 ng/ml) for 20 min. The cells were washed and total cell lysate was made using lysis buffer. The supernatant was incubated with anti-PI3 K p85-α antibody (5 μl antibody/sample) for 1 h at 4°C followed by protein A-agarose chromatography. The PI3 K activity in the immunoprecipitated beads was measured by incubating with phosphatidylinositol (4, 5)-biphosphate [PI(4, 5)P2] substrate (100 pmol) in kinase reaction buffer for 2 h at room temperature with shaking. The supernatant was incubated with PI-[3, 4, 5]P3 detector protein for 1 h at room temperature followed by transfer to a PI-[3, 4, 5]P3-coated detection plate for 1 h at room temperature for competitive binding. After washing with Tris buffer a peroxidase-linked secondary detector was added and developed with 3,3,5,5-tetramethylbenzidine (TMB) solution. The PI-[3, 4, 5]P3 detector protein binding to the plate was determined by measuring the absorbance at 450 nm. The colorimetric signal is inversely proportional to the amount of PI-[3,4,5]P3 produced by PI3 K.
Statistical analysis
Data are presented as mean ± S.E and the P values were determined using the unpaired Student’s t test.
Results
Inhibition of AR prevents angiogenic factors-induced proliferation of HUVEC
To test the hypothesis that AR inhibition can prevent angiogenesis, initially we determined the effects of AR inhibition on angiogenic factors-induced proliferation of HUVEC. As shown in the Fig. 1a, treatment of HUVEC with VEGF or FGF for 24 h significantly stimulated the growth as determined by MTT assay. The increase in growth was attenuated in the presence of AR inhibitor, fidarestat. In the absence of angiogenic factors, fidarestat alone did not affect the HUVEC growth. To exclude non-specific effects of a pharmacological inhibitor, we ablated the AR message by transient transfection of HUVEC with ARsiRNA. Transfection of HUVEC with ARsiRNA but not scrambled ARsiRNA caused >95% ablation of AR protein (data not shown). Consistent with our previous data, transfection of HUVEC with ARsiRNA significantly (~75%) inhibited VEGF- and FGF–induced cell growth (Fig. 1b). The inhibitory activity of fidarestat on VEGF- and FGF-induced HUVEC proliferation was also assessed by flow cytometry using PE-labeled Ki67, a proliferation marker (Fig. 1c). Treatment of HUVEC with VEGF or FGF increased the Ki67 expression, whereas AR inhibition significantly prevented it. These results suggest that AR mediates VEGF- or FGF-induced HUVEC growth.
Inhibition of AR prevents pro-angiogenic factors-induced proliferation of HUVEC. a and b Growth-arrested HUVEC were pre-incubated with fidarestat (5 μM) or transfected with ARsiRNA or scrambled ARsiRNA for 24 h followed by stimulation with VEGF or FGF (10 ng/ml) for 24 h. Cell viability was determined by MTT assay. c Expression of Ki-67 in HUVEC was determined by flow cytometry using PE-labeled Ki-67 antibodies (P2: filled histogram) and isotype control antibodies as negative control (P1: empty histogram). The data was analyzed by using Cell Quest version 3.3 software. Bar graph represents percentage of Ki 67 expressing cells compared to control. Bars represent mean ± S.E. (n = 6; two independent experiments with triplicates); * P < 0.001 vs. control and #, P < 0.001 vs. growth factor-treated cells
Inhibition of AR prevents angiogenic factors-induced capillary-like tube structure network and spheroid formation
We next examined the effect of AR inhibition on angiogenic factors-induced tube formation in HUVEC. The HUVEC were plated in a 96 well plate containing growth factor –reduced matrigel and determined the effect of AR inhibitor on VEGF- and FGF-induced capillary—like structure formation (in vitro angiogenesis). As shown in the Fig. 2a inhibition of AR by fidarestat prevented angiogenic factors such as VEGF- and FGF-induced capillary—like tube structure formation in a concentration dependent manner. The capillary-like tube structure formation by HUVEC was completely abolished at a higher concentration (10 M) of fidarestat. Consistent with our data obtained with AR inhibitor, transfection of HUVEC with AR-siRNA significantly (~85%) inhibited VEGF- and FGF-induced tube formation (Fig. 2a). We next determined the effect of fidarestat on VEGF-induced three-dimensional endothelial cell organization and morphogenesis using HUVEC spheroids, i.e., cell aggregates, embedded in a collagen gel. In the presence of VEGF, HUVEC spheroid sprouted and invaded the surrounding collagen gel forming capillary-like structures (Fig. 2b). AR inhibition prevented the VEGF-induced sprout formation in a significant manner. Collectively, these results suggest that AR inhibition prevents VEGF- and FGF-induced angiogenesis in HUVEC.
Inhibition of AR prevents angiogenic factors-induced capillary-like tube structure and spheroid formation in HUVEC. Growth-arrested HUVEC (a) or HUVEC spheroids (b) were incubated in 96 well plate with or without VEGF or FGF (10 ng/ml) and/or AR inhibitor, fidarestat. After an overnight incubation, the network growth area was examined using an inverted microscope 50× . Angiogenic effect was measured by counting the relative branch points. Spheroids were digitally quantified by measuring the cumulative length of the sprouts. Bars represent mean ± S.E. (n = 6); * P < 0.001 vs. control and #, P < 0.001 vs. growth factor-treated cells
Inhibition of AR prevents angiogenic factors-induced invasion and migration of HUVEC
Since secretion of growth factors and cytokines by tumor cells is known to cause invasion and migration of endothelial cells which cause neovascularization, we determined the effect of AR inhibition on growth factors –induced invasion of HUVEC. As shown in the Fig. 3a, treatment of HUVEC with VEGF or FGF caused pronounced invasion of endothelial cells, whereas inhibition of AR by fidarestat significantly prevented it. Next, we determined the effect of AR inhibition on VEGF- or FGF-induced migration of HUVEC using wound scratch model assay. Our Results indicate that inhibition of AR by pharmacological inhibitor or ablation of AR by using specific siRNA significantly prevented the migration of HUVEC (Fig. 3b). These results indicate that AR inhibition prevents invasion and migration of endothelial cells.
Inhibition of AR prevents angiogenic factors-induced invasion and migration of HUVEC. a Invasion assay in HUVEC was performed in 96 well plate using basement membrane extract. Invasion of cells towards bottom side of the well was measured using Calcein-AM florescent dye at 485/520 nm excitation/emission. b Inhibition of AR prevents growth factors-induced migration of HUVEC in a scratch wound assay. Wound scratches were made with a sterile pipette tip in the wells at the sub-confluent stage. After 24 h of incubation with and without AR inhibitor, the migration of cells was observed and photographs were taken using Nikon camera fixed to inverted microscope (40 × and 100 ×). The white arrow indicates the area of scratch and HUVEC migration. Bars represent mean ± S.E. (n = 6); * P < 0.001 vs. control and #, P < 0.001 vs. growth factor-treated cells
Inhibition of AR prevents angiogenic factors-induced secretion/expression of ICAM, VCAM, MMP2, MMP9 and IL-6 in HUVEC
VEGF and FGF are known to play an important role in the angiogenesis by inducing secretion of adhesion molecules, matrix metallo proteinases, and cytokines, which are known to be involved in endothelial cell proliferation, migration, and differentiation. Therefore, to gain insights into the mechanism(s) by which AR inhibition prevents angiogenesis, we determined the effect of AR inhibition on VEGF- and FGF-induced secretion/expression of ICAM, VCAM, MMP2, MMP9 and IL-6 in HUVEC (Fig. 4a). Treatment of HUVEC with VEGF or FGF caused pronounced increase in the secretion of ICAM, VCAM, MMP2, MMP9 and IL-6 and inhibition of significantly prevented the release of these proteins into the culture media. Similarly, AR inhibition also prevented the expression of ICAM, VCAM, MMP2 and MMP9 proteins (Fig. 4b), suggesting AR inhibition prevents invasion and migration of HUVEC by inhibiting the expression of MMPs. Since the activities of MMPs are regulated by the physiological inhibitor proteins, TIMPs, we next examined the effect of AR inhibition on growth factor-induced expression of TIMP-1, a specific regulator of MMP-9 and a well-established prognostic marker for colon cancer, in HUVEC cells. The levels of TIMP-1 are not detectable by Western blot analysis (data not shown). Similarly, inhibition of AR increased the secretion of IFN-γ (Fig. 4a), an anti-proliferative and anti-angiogenic cytokine, which decreased in the presence of VEGF or FGF suggesting that AR inhibition prevents proliferation as well as angiogenesis of endothelial cells. The VEGF mediated pro-survival signal transduction to the nucleus is caused by its interaction with receptors such as VEGF-R1, VEGF-R2, and VEGF-R3. Among the three VEGF receptors, VEGF-R2 is known to play an important role in angiogenesis [36]. Next, we tested whether AR inhibition mediated prevention of HUVEC migration and tube formation was caused by a decrease in the protein level of VEGF-R2. As shown in the Fig. 4b, inhibition of AR significantly prevented the VEGF-induced expression its receptor VEGF-R2 at 24 h. We next measured the effect of AR inhibition on VEGF-induced phosphorylation of VEGF-R2 in a time dependent manner. Our results shown in Fig. 4c indicate that VEGF caused phosphorylation of VEGF-R2 and inhibition of AR prevented the VEGF-induced phosphorylation. The total levels of VEGF-R2 were not affected up to 2 h of VEGF-treatment.
Inhibition of AR prevents angiogenic factors-induced secretion of ICAM, VCAM, MMP2, MMP9 and IL-6 in HUVEC. a Growth arrested HUVEC were treated with VEGF or FGF (10 ng/ml) and/or fidarestat (5 μM) for 24 h and cell culture medium was subjected to ELISA analysis using RayBiotech ELISA kits as per manufacturer’s instructions. b After 24 h stimulation of HUVEC with VEGF, Western blot analysis performed using antibodies against VEGF-R2, MMP-2, MMP-9, and GAPDH. c Western blot analysis of VEGF-R2 phosphorylation was determined using Phospho specific VEGF-R2 antibodies. Fold change was quantified by using Kodak Image station 2000R loaded with Kodak 1-dimensional image-analysis software (Kodak, Rochester, NY). Bars represent mean ± S.E. (n = 4); * P < 0.001 vs. control and #, P < 0.001 vs. growth factor-treated cells
Inhibition of AR prevents VEGF-induced formation of capillary-like tube structure network in matrigel plugs in vivo
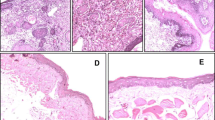
The effect of AR inhibition on endothelial cell invasion and organization into capillary-like structures was investigated using the in vivo matrigel plugs assay, performed in rats. Rats were subcutaneously injected in the dorsal midline with growth factor-reduced matrigel containing VEGF and/or fidarestat. After 1 week, plugs were excised and analyzed to assess the presence of endothelial cells and neovascularization. As shown in the Fig. 5a, H&E staining the maximal localization of cells organized in capillary-like structures occurred in plugs containing VEGF-treated group. Immunohistochemistry with anti-CD31 and anti-vWF antibodies showed that infiltrating cells were endothelial cells and that VEGF enhanced the angiogenesis with respect to control (Fig. 5a). Presence of red blood cells in some of these capillaries indicates that they were functional. We have also quantitated the newly vascularized vessels in the entire plug counted under a light microscope. The average of counts from four plugs per group was plotted in the graph shown in Fig. 5b. The VEGF-induced increase in the number of capillary structures was significantly reduced in rats treated with fidarestat. Our results thus indicate that VEGF-induced increase of capillary-like structures formation, infiltration of endothelial cells and red blood cells was significantly inhibited by co-treatment with VEGF and fidarestat which was not observed in specimens treated with fidarestat alone. These findings suggest that AR inhibition could prevent VEGF activity on endothelial cells migration and invasion in vivo also.
Inhibition of AR prevents VEGF-induced angiogenesis in rat matrigel plug model. a Five hundred μl of growth factor-free matrigel with or without VEGF (10 ng/ml) and/or fidarestat (20 μM) was injected subcutaneously (s.c.) into the dorsal tissue of Fischer 344 rats (n = 4) and AR inhibitor, fidarestat (16 mg/kg body weight) was given through drinking water. After 1 week, rats were killed and plugs were excised and fixed with 4% paraformaldehyde. Serial sections (5 μm thick) of matrigel plugs were stained with hematoxylin/eosin, anti-CD31/PECAM-1 and anti-Von Willebrandt factor and observed under the microscope (400 ×). b The graph shows the number of newly vascularized vessels in the entire plug counted under light microscope. Bars represent mean ± S.E. (n = 4); * P < 0.001 vs. control and #, P < 0.001 vs. growth factor-treated cells
Inhibition of AR prevents activation of PI3 K/AKT and NF-κB in HUVEC cells
Since activation of PI3 K/AKT is known to be involved in endothelial cell survival and VEGF-induced migration and differentiation [34, 35], we next measured the effect of AR inhibition on the VEGF-induced activation of PI3 K and AKT. As shown in the Fig. 6a, VEGF stimulated PI3 K activity approximately 2.0 folds as compared to control and inhibition of AR significantly (~65%) prevented it. Similarly, inhibition of AR significantly prevented the VEGF-induced phosphorylation of AKT (Fig. 6b). To examine if AR inhibition prevented the AKT and PI3 K activity by regulating the nitrosation of AKT and PI3 K, we have determined nitro-AKT and nitro-PI3 K levels by using immunoprecipitation studies. Our results shown in Fig. 6c demonstrate that AR inhibition prevents nitrosation of both AKT and PI3 K suggesting that AR inhibition prevents nitrosation of these kinases. Collectively, these results suggest that inhibition of AR could prevent VEGF-induced activation of PI3 K/AKT pathway. Further, to determine the downstream signals of PI3 K/AKT pathway leading to activation of NF-κB, we next determined the effect of AR inhibition on the phosphorylation of p65, a hetero-dimer subunit of NF-κB. As shown in the Fig. 6b, inhibition of AR by fidarestat prevented the phosphorylation of p65 suggesting that inhibition of AR could prevent NF-κB activation by inhibiting the activation of PI3 K/AKT in HUVEC. Since NF-κB is a redox sensitive transcription factor and increased oxidative stress is known to activate the NF-κB [12], we next measured the efficacy of AR in preventing the generation of protein-HNE adducts, as a marker for oxidative stress, in HUVEC cells. Our results indicate that AR inhibition significantly prevented the formation of protein-HNE adducts in growth-factor treated HUVEC (Fig. 6c).
Inhibition of AR prevents VEGF-induced activation of PI3 K/AKT, NF-κB and expression of VEGF-R2 and matrix metalloproteinases in HUVEC. Growth-arrested HUVEC were pre-incubated with fidarestat (5 μM) or carrier for 24 h followed by stimulation with VEGF (10 ng/ml) for (a) 20 min to determine PI3 K activity as described in materials and methods and (b) Western blots were developed using antibodies against p-AKT, p-p65 and GAPDH. c Equal amount of time dependent VEGF induced HUVEC cell lysates were immunoprecipitated with anti-NO2-tyr antibodies and immunocomplexes were separated using Pierce classic IP kit as described in methods. The immune complexes were subjected to Western blot analysis and probed with anti-AKT, anti-PI3 K p85 and protein-HNE antibodies. Fold change was quantified by using Kodak Image station 2000R loaded with Kodak 1-dimensional image-analysis software (Kodak, Rochester, NY). Bars represent mean ± SE (n = 4); * P < 0.001 compared with control and #, P < 0.001 compared with cells treated with growth factor
Discussion
Angiogenesis involves endothelial cell survival, invasion, proliferation, migration and differentiation [1–4]. Potent pro-angiogenic growth factors such as VEGF, FGF and some extracellular matrix proteins via NF-κB can trigger signaling pathways involved in the differentiation of endothelial cells [37–39]. Since AR mediates oxidative stress-induced signals that increase transcription of inflammatory markers [22–26], which play a significant role in diseases such as cardiomyopathy, hypertension, wound healing, tissue remodeling, diabetic retinopathy and cancer which require increased blood supply, we determined the possible role of AR in angiogenesis. The present study for the first time reveals that AR mediates angiogenic features of HUVEC in vitro as well as in vivo, and suggest novel anti-angiogenic efficacy of AR inhibitors.
Various reports show that oxidative stress plays an important role in the initiation of inflammatory signaling in the vasculature of organs [7, 10]. For example, ROS have also been implicated in ischemic and reperfusion injury to a large variety of tissue [40]. Yasuda et al. [41] showed that exposure of endothelial cells to lower concentrations of H2O2 stimulates angiogenesis. Further, they demonstrated that cancer cells produce ROS which could be one of the triggers of the angiogenic process in endothelial cells. The ROS cause up-regulation of proangiogenic growth factors such as VEGF, FGF via transcriptional activation of NF-κB, AP-1, Sp1 and Sp3 [14, 42]. The NOX family of NAD(P)H oxidases is a good source of ROS that could influence tumor cell proliferation via the redox-regulated transcription factor NF-κB which in turn regulates numerous genes involved in apoptosis, cell proliferation, metastasis and angiogenesis [8, 42]. We have shown previously that inhibition of AR can prevent growth factors-, cytokines-, chemokines- and hyperglycemia-induced ROS signals via inhibition of redox-sensitive transcriptions factors, NF-κB and AP-1 activation [22–27]. Several experimental data suggest that antioxidants such as green tea, quercetin, resveratrol and lycopene consumption significantly inhibit angiogenesis [15–19]. For example, epigallocatechin gallate (EGCG), a putative chemopreventive agent and an important component of green tea, was found to inhibit tumor invasion and the angiogenesis processes that are essential for tumor growth [19]. Evidence suggests that increased ROS and lipid peroxidation derived products such as HNE, induce transcription of fibrogenic cytokines, chemokines and growth factors, etc. which in autocrine/paracrine fashion play a pivotal role in many biological processes, including immune response, recruitment of inflammatory cells, cytotoxicity, antiviral activity, wound repair, angiogenesis, and apoptosis [14, 43].
The entire sequence of events of angiogenesis or neovascularization is mediated by various types of cells, including macrophages, lymphocytes, mast cells, platelets, and polymorphonuclear leukocyte [9, 14]. In RAW264.7 murine macrophages, we have shown that inhibition of AR prevents the lipopolysaccharide-induced release of inflammatory cytokines, chemokines, nitric oxide and ROS [43]. AR inhibition has also shown to prevent hyperglycemia–induced oxidative stress in retinal endothelial cells and expression of VEGF in diabetic rats [44]. These results suggest that AR plays an important role in oxidative stress-mediated inflammatory pathologies, including angiogenesis. Endothelial migration and wound healing are commonly observed under hyperglycemic conditions and may contribute to vascular dysfunction in diabetics [45]. A recent study of D’Souza et al. [46] suggest that inhibition of AR by alrestatin and ablation by AR-siRNA improved wound healing in endothelial cells treated with high glucose. These studies indicate that inhibition of AR could normalize dysfunctional vessels and improve vascular remodeling and angiogenesis under hyperglycemic conditions.
The biological functions of VEGF, and FGF, triggered by external stimuli, are initiated through the activation of intracellular signal cascades involving specific kinases [47]. Formation of a receptor complex between VEGF and its tyrosine kinase receptor VEGF-R2 plays an important role in coordinating the effects of VEGF on cell adhesion and cell motility [36]. Among the VEGF receptors (VEGF-R1, R2, and R3), VEGF-R2 is believed to play an important role in angiogenesis. VEGF-R2 is a receptor tyrosine kinase, which, on activation by ligand binding, phosphorylates and activates secondary messengers, including AKT, to regulate endothelial cell proliferation and migration [36]. In this context, our results show that exposure of HUVEC to AR inhibitor, fidarestat results in suppression of PI3 K/AKT/NF-κB activation as well as down-regulation of VEGF-R2 protein levels.
AKT, a serine-threonine kinase, a homologue of a retroviral oncoprotein v-Akt, is recruited during signal transduction from growth factor receptors and intracellular pathways [28, 34, 35]. Vascular homeostasis and angiogenesis by different stimuli, including VEGF, and angiopoietin-1, is regulated by the activation of AKT [34, 35]. Various reports show that activation of AKT and its upstream kinase phosphatidylinositol 3-kinase (PI3 K) induce angiogenesis in vitro and in vivo. The expression of VEGF in endothelial cells is also regulated by the PI3 K-AKT signaling axis. AKT activation not only promotes endothelial cell survival but also regulates vasomotor responses via phosphorylation of endothelial nitric oxide synthase and VEGF-stimulated endothelial cell migration and differentiation [34, 35]. Our results show that the antiangiogenic effect of AR inhibition is closely associated with inhibition of AKT kinase. Activation of AKT is mediated by receptor tyrosine kinases that, on ligand binding, are autophosphorylated and cause activation of PI3 K. Activated PI3 K generates lipid second messengers, which facilitate recruitment of AKT to the plasma membrane and activation [35]. In HUVEC it is possible that AR inhibition causes inhibition of PI3 K to inhibit Ser473 phosphorylation (activation) of AKT. The AR inhibition-caused suppression of AKT/PI3 K/NF-κB activation is not restricted to HUVEC because similar effects are evident in various cell lines including VSMC, HLEC, human colon cancer SW480, and HT29 cells [22–27]. Further, we have also examined the effect of AR inhibition in regulation of nitrosation of AKT and PI3 K which is generally observed under stress conditions. Our results indicate that AR inhibition prevents AKT and PI3 K activities probably by preventing their nitrosations.
Recent studies have implicated that multiple growth factors and cytokines, chemokines, adhesion factors, matrix metalloproteinases are involved in various stages of angiogenesis [26, 30, 35]. For instance, IL-17 increases angiogenic activity and in vivo growth of human non–small lung cancer cells in severe combined immuno-deficient mice [48]. Similarly, G-CSF promotes tumor angiogenesis by increasing circulating endothelial progenitor cells [49]. Degradation of the extracellular matrix is a critical component of tumor metastasis, which is orchestrated by zinc-dependent proteolytic enzymes such as MMPs [12, 13]. Of these, MMP2 and 9, in particular, are believed to have an important role in the initial steps of tumor invasion and metastasis [30]. Expression of MMPs is associated with the expression of physiological inhibitor proteins TIMPs. However, the expression level of TIMP-1 in HUVEC is not detectable in our studies. Similarly, Liu et al. [50] have shown that TIMP-1 levels are not detectable in HUVEC but co-culture of fibroblasts with HUVEC leads to increased TIMP-1 expression. Further, our results also show that AR inhibition significantly prevents the expression of adhesion molecules in HUVEC cells. This is inconsistent with our previous studies in the context to the vascular inflammation and atherosclerosis which show that the inhibition of AR prevents cytokines such as TNF-α–induced ICAM, VCAM expression and apoptosis in HUVEC via inhibiting the activation of NF-κB. NF-κB is a redox sensitive transcription factor, whose expression is elevated under oxidative stress conditions [51]. Activation of NF-κB has been shown to increase the expression of various angiogenic factors including VEGF. Several studies indicate that inhibition of NF-κB prevents angiogenesis [52]. Thus our current studies indicate that AR inhibition prevents angiogenesis by preventing growth factors-induced oxidative stress, activation of AKT/PI3 K and NF-κB and expression of angiogenic proteins.
In conclusion, the present study shows that inhibition of AR prevents angiogenesis in vitro and in vivo. The AR inhibition-caused suppression of endothelial cell differentiation, invasion, and migration is associated with inactivation of AKT, suppression of pro-angiogenic growth factors, and down-regulation of VEGF-R2 protein expression. Thus, our studies indicate a novel role of AR in regulation of angiogenic process and therefore, inhibition of AR could prevent cancer growth and metastasis by ameliorating the angiogenesis.
Abbreviations
- AP1:
-
Activator protein
- AR:
-
Aldose reductase
- DHN:
-
1,4-dihydroxynonene
- FGF:
-
Basic fibroblast growth factor
- Fid:
-
Fidarestat
- GSH:
-
Glutathione
- GS-HNE:
-
Glutathionyl-4-hydroxynonenal
- GS-DHN:
-
Glutathionyl-1,4-dihydroxynonene
- HNE:
-
4-hydroxy-trans-2-nonenal
- HUVEC:
-
Human umbilical vascular endothelial cells
- MMP:
-
Matrix metalloproteinases
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- NF-κB:
-
Nuclear factor kappa B
- ROS:
-
Reactive oxygen species
- siRNA:
-
Small interfering RNA
- VEGF:
-
Vascular endothelial growth factor
- VSMC:
-
Vascular smooth muscle cells
- vWF:
-
Von-Willebrand factor
References
Ferrara N, Kerbel RS (2005) Angiogenesis as a therapeutic target. Nature 438:967–974
Chiodoni C, Colombo MP, Sangaletti S (2010) Matricellular proteins: from homeostasis to inflammation, cancer, and metastasis. Cancer Metastasis Rev 29:295–307
Carmeliet P (2005) Angiogenesis in life, disease and medicine. Nature 438:932–936
Jamie MH, Stacey LB, Jason EB (2008) Comparison of angiogenesis-related factor expression in primary tumor cultures under normal and hypoxic growth conditions. Cancer Cell International 8:11
Ben-Baruch A (2003) Host microenvironment in breast cancer development. Inflammatory cells, cytokines and chemokines in breast cancer progression: reciprocal tumor–microenvironment interactions. Breast Cancer Res 5:31–36
Ann H, Bart L, Martin S, Highley H, Wildiers AT, Van O, Ernst A, Bruijn D (2004) Vascular Endothelial Growth Factor and Angiogenesis. Pharmacol Rev 56:549–580
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB (2010) Oxidative stress, inflammation, and cancer: How are they linked? Free Radic Biol Med 49:1603–1616
Chan EC, Jiang F, Peshavariya HM, Dusting GJ (2009) Regulation of cell proliferation by NADPH oxidase-mediated signaling: potential roles in tissue repair, regenerative medicine and tissue engineering. Pharmacol Ther 122:97–108
Bräsen JH, Kivelä A, Röser K, Rissanen TT, Niemi M, Luft FC, Donath K, Ylä-Herttuala S (2001) Angiogenesis, vascular endothelial growth factor and platelet-derived growth factor-BB expression, iron deposition, and oxidation-specific epitopes in stented human coronary arteries. Arterioscler Thromb Vasc Biol 21:1720–1726
Edirisinghe I, Rahman I (2010) Cigarette smoke-mediated oxidative stress, shear stress, and endothelial dysfunction: role of VEGFR2. Ann N Y Acad Sci 1203:66–72
Rabbani ZN, Mi J, Zhang Y, Delong M, Jackson IL, Fleckenstein K, Salahuddin FK, Zhang X, Clary B, Anscher MS, Vujaskovic Z (2010) Hypoxia inducible factor 1alpha signaling in fractionated radiation-induced lung injury: role of oxidative stress and tissue hypoxia. Radiat Res 173:165–174
Yang Z, Li C, Wang X, Zhai C, Yi Z, Wang L, Liu B, Du B, Wu H, Guo X, Liu M, Li D, Luo J (2010) Dauricine induces apoptosis, inhibits proliferation and invasion through inhibiting NF-kappaB signaling pathway in colon cancer cells. J Cell Physiol 225:266–275
Cezar-de-Mello PF, Vieira AM, Nascimento-Silva V, Villela CG, Barja-Fidalgo C, Fierro IM (2008) ATL-1, an analogue of aspirin-triggered lipoxin A4, is a potent inhibitor of several steps in angiogenesis induced by vascular endothelial growth factor. Br J Pharmacol 153:956–965
Wu WS (2006) The signaling mechanism of ROS in tumor progression. Cancer Metastasis Rev 25:695–705
Borek C (2004) Dietary antioxidants and human cancer. Integr Cancer Ther 3:333–341
Rajamanickam S, Velmurugan B, Kaur M, Singh RP, Agarwal R (2010) Chemoprevention of intestinal tumorigenesis in APCmin/+ mice by silibinin. Cancer Res 70:2368–2378
Fuggetta MP, Lanzilli G, Tricarico M, Cottarelli A, Falchetti R, Ravagnan G, Bonmassar E (2006) Effect of resveratrol on proliferation and telomerase activity of human colon cancer cells in vitro. J Exp Clin Cancer Res 25:189–193
Singh SV, Powolny AA, Stan SD, Xiao D, Arlotti JA, Warin R, Hahm ER, Marynowski SW, Bommareddy A, Potter DM, Dhir R (2008) Garlic constituent diallyl trisulfide prevents development of poorly differentiated prostate cancer and pulmonary metastasis multiplicity in TRAMP mice. Cancer Res 68:9503–9511
Cao Y, Cao R (1999) Angiogenesis inhibited by drinking tea. Nature 398:381
Ramana KV, Bhatnagar A, Srivastava SK (2004) Aldose reductase regulates TNF-alpha-induced cell signaling and apoptosis in vascular endothelial cells. FEBS Lett 570:189–194
Chandra D, Ramana KV, Friedrich B, Srivastava S, Bhatnagar A, Srivastava SK (2003) Role of aldose reductase in TNF-alpha-induced apoptosis of vascular endothelial cells. Chem Biol Interact 143–144:605–612
Tammali R, Ramana KV, Singhal SS, Awasthi S, Srivastava SK (2006) Aldose reductase regulates growth factor-induced cyclooxygenase-2 expression and prostaglandin E2 production in human colon cancer cells. Cancer Res 66:9705–9713
Tammali R, Ramana KV, Srivastava SK (2007) Aldose reductase regulates TNF-alpha-induced PGE2 production in human colon cancer cells. Cancer Lett 252:299–306
Srivastava SK, Ramana KV, Bhatnagar A (2005) Role of aldose reductase and oxidative damage in diabetes and the consequent potential for therapeutic options. Endocr Rev 26:380–392
Ramana KV, Chandra D, Srivastava S, Bhatnagar A, Aggarwal BB, Srivastava SK (2002) Aldose reductase mediates mitogenic signaling in vascular smooth muscle cells. J Biol Chem 277:32063–32070
Ramana KV, Willis MS, White MD, Horton JW, DiMaio JM, Srivastava D, Bhatnagar A, Srivastava SK (2006) Endotoxin-induced cardiomyopathy and systemic inflammation in mice is prevented by aldose reductase inhibition. Circulation 114:1838–1846
Ramana KV, Bhatnagar A, Srivastava S, Yadav UC, Awasthi S, Awasthi YC, Srivastava SK (2006) Mitogenic responses of vascular smooth muscle cells to lipid peroxidation-derived aldehyde 4-hydroxy-trans-2-nonenal (HNE): role of aldose reductase-catalyzed reduction of the HNE-glutathione conjugates in regulating cell growth. J Biol Chem 281:17652–17660
Ramana KV, Tammali R, Srivastava SK (2010) Inhibition of aldose reductase prevents growth factor-induced G1-S phase transition through the AKT/phosphoinositide 3-kinase/E2F–1 pathway in human colon cancer cells. Mol Cancer Ther 9:813–824
Tammali R, Reddy AB, Ramana KV, Petrash JM, Srivastava SK (2009) Aldose reductase deficiency in mice prevents azoxymethane-induced colonic preneoplastic aberrant crypt foci formation. Carcinogenesis 30:799–807
Salani D, Taraboletti G, Rosanò L, Di Castro V, Borsotti P, Giavazzi R, Bagnato A (2000) Endothelin-1 induces an angiogenic phenotype in cultured endothelial cells and stimulates neovascularization in vivo. Am J Pathol 157:1703–1711
Burger M, Hartmann T, Burger JA, Schraufstatter I (2005) KSHV-GPCR and CXCR2 transforming capacity and angiogenic responses are mediated through a JAK2-STAT3-dependent pathway. Oncogene 24:2067–2075
Karkoulis PK, Stravopodis DJ, Margaritis LH, Voutsinas GE (2010) 17-Allylamino-17-demethoxygeldanamycin induces downregulation of critical Hsp90 protein clients and results in cell cycle arrest and apoptosis of human urinary bladder cancer cells. BMC Cancer 10:481
Pang X, Yi Z, Zhang J, Lu B, Sung B, Qu W, Aggarwal BB, Liu M (2010) Celastrol suppresses angiogenesis-mediated tumor growth through inhibition of AKT/mammalian target of rapamycin pathway. Cancer Res 70:1951–1959
Jiang BH, Zheng JZ, Aoki M, Vogt PK (2000) Phosphatidylinositol 3-kinase signaling mediates angiogenesis and expression of vascular endothelial growth factor in endothelial cells. Proc Natl Acad Sci USA 97:1749–1753
Brader S, Eccles SA (2004) Phosphoinositide 3-kinase signalling pathways in tumor progression, invasion and angiogenesis. Tumori 90:2–8
Xiao D, Li M, Herman-Antosiewicz A, Antosiewicz J, Xiao H, Lew KL, Zeng Y, Marynowski SW, Singh SV (2006) Diallyl trisulfide inhibits angiogenic features of human umbilical vein endothelial cells by causing Akt inactivation and down-regulation of VEGF and VEGF-R2. Nutr Cancer 55:94–107
Shono T, Ono M, Izumi H, Jimi SI, Matsushima K, Okamoto T, Kohno K, Kuwano M (1996) Involvement of the transcription factor NF-kB in tubular morphogenesis of human microvascular endothelial cells by oxidative stress. Mol Cell Biol 16:4231–4239
Morais C, Gobe G, Johnson DW, Healy H (2009) Anti-angiogenic actions of pyrrolidine dithiocarbamate, a nuclear factor kappa B inhibitor. Angiogenesis 12:365–379
Tabruyn SP, Mémet S, Avé P, Verhaeghe C, Mayo KH, Struman I, Martial JA, Griffioen AW (2009) NF-kappaB activation in endothelial cells is critical for the activity of angiostatic agents. Mol Cancer Ther 8:2645–2654
Nijmeh J, Moldobaeva A, Wagner EM (2010) Role of ROS in ischemia-induced lung angiogenesis. Am J Physiol Lung Cell Mol Physiol 299:L535–L541
Yasuda M, Ohzeki Y, Shimizu S, Naito S, Ohtsuru A, Yamamoto T, Kuroiwa Y (1999) Stimulation of in vitro angiogenesis by hydrogen peroxide and the relation with ETS-1 in endothelial cells. Life Sci 64:249–258
Schafer G, Cramer T, Suske G, Kemmner W, Wiedenmann B, Hocker M (2003) Oxidative stress regulates vascular endothelial growth factor-A gene transcription through Sp1- and Sp3-dependent activation of two proximal GC-rich promoter elements. J Biol Chem 278:8190–8198
Ramana KV, Fadl AA, Tammali R, Reddy AB, Chopra AK, Srivastava SK (2006) Aldose reductase mediates the lipopolysaccharide-induced release of inflammatory mediators in RAW264.7 murine macrophages. J Biol Chem 281:33019–33029
Obrosova IG, Minchenko AG, Vasupuram R, White L, Abatan OI, Kumagai AK, Frank RN, Stevens MJ (2003) Aldose reductase inhibitor fidarestat prevents retinal oxidative stress and vascular endothelial growth factor overexpression in streptozotocin-diabetic rats. Diabetes 52:864–871
Hamuro M, Polan J, Natarajan M, Mohan S (2002) High glucose induced nuclear factor kappa B mediated inhibition of endothelial cell migration. Atherosclerosis. 162:277–287
D’Souza DR, Salib MM, Bennett J, Mochin-Peters M, Asrani K, Goldblum SE, Renoud KJ, Shapiro P, Passaniti A (2009) Hyperglycemia regulates RUNX2 activation and cellular wound healing through the aldose reductase polyol pathway. J Biol Chem. 284(27):17947–17955
Shiojima I, Walsh K (2002) Role of Akt signaling in vascular homeostasis and angiogenesis. Circ Res 90:1243–1250
Numasaki M, Watanabe M, Suzuki T, Takahashi H, Nakamura A, McAllister F, Hishinuma T, Goto J, Lotze MT, Kolls JK, Sasaki H (2005) IL-17 enhances the net angiogenic activity and in vivo growth of human non-small cell lung cancer in SCID mice through promoting CXCR-2-dependent angiogenesis. J Immunol 175:6177–6189
Goette A, Wolfram O, Jentsch-Ullrich K, Martens-Lobenhoffer J, Scalera F, Lendeckel U, Bode-Böger SM (2010) The effects of G-CSF-induced mobilization of progenitor cells are limited by ADMA. Int J Cardiol 143:264–270
Liu H, Chen B, Lilly B (2008) Fibroblasts potentiate blood vessel formation partially through secreted factor TIMP-1. Angiogenesis 11:223–234
Gloire G, Legrand-Poels S, Piette J (2006) NF-kappaB activation by reactive oxygen species: fifteen years later. Biochem Pharmacol 72:1493–1505
Xiao D, Singh SV (2007) Phenethyl isothiocyanate inhibits angiogenesis in vitro and ex vivo. Cancer Res 67:2239–2246
Acknowledgments
Supported by in parts by NIH grants CA129383 and DK36118 (SKS) and GM71036 (KVR). Satish Srivastava is a William Bowes Senior Fellow of the American Asthma Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
R. Tammali and A. B. M. Reddy have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Tammali, R., Reddy, A.B.M., Srivastava, S.K. et al. Inhibition of aldose reductase prevents angiogenesis in vitro and in vivo. Angiogenesis 14, 209–221 (2011). https://doi.org/10.1007/s10456-011-9206-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-011-9206-4