Abstract
Our previous studies have revealed the abundant expression of T-cadherin—a glycosylphosphatidylinositol (GPI)-anchored member of cadherin superfamily—in endothelial and mural cells in the heart and vasculature. The upregulation of T-cadherin in vascular proliferative disorders such as atherosclerosis and restenosis suggests the involvement of T-cadherin in vascular growth and remodeling. However, the functional significance of this molecule in the vasculature remains unknown. The effect of T-cadherin on angiogenesis in vivo was evaluated using Matrigel implant model. We demonstrate that T-cadherin overexpression in L929 cells injected in Matrigel inhibits neovascularization of the plug. In vitro T-cadherin inhibits the directional migration of endothelial cells, capillary growth, and tube formation but has no effect on endothelial cell proliferation, adhesion, or apoptosis in vitro. These data suggest that T-cadherin expressed in the stroma could act as a negative guidance cue for the ingrowing blood vessels and thus could have an important potential therapeutic application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive or insufficient angiogenesis in adult tissues contributes to many pathologies, including atherosclerosis and tumor growth. The migratory behavior of endothelial cells and their ability to form a new vascular tree plays a key role in this process. Cadherins are known to be crucial for vessel growth and maturation [1, 2]. Cadherins comprise a large superfamily of molecules responsible for Ca+-dependent cell recognition and adhesion. Classical cadherins consist of five extracellular (EC1-EC5), as well as transmembrane and cytoplasmic domains [2, 3]. During embryogenesis cadherins mediate cell sorting and segregation, cell migration, morphogenesis, axon growth, and target pathfinding. In adult organisms cadherins regulate the stable organization of solid tissues, the orderly turnover of cells in rapidly growing tissues, the physiological barrier function of bordering tissues, and selective transport of solutions and cells [3, 4]. The predominantly expressed cadherins in vascular cells, such as endothelial, pericytes and vascular smooth muscle cells (VSMC) are N-cadherin/R-cadherin and T-cadherin [1, 2, 5].
T-cadherin is an atypical member of the cadherin superfamily. While possessing the general extracellular structure of classical cadherins, T-cadherin lacks transmembrane and cytoplasmic domains and is anchored to the plasma membrane by a glycosylphosphatidylinositol (GPI) moiety [6]. Since transmembrane and cytoplasmic domains of classical cadherins are generally recognized to be crucial in maintaining stable cell–cell contacts [3], it is likely that T-cadherin is implicated in cell signaling rather than cell adhesion [5, 7, 8].
The upregulation of T-cadherin expression in vascular cells in adventitial vasa vasorum of injured arteries, in vascular proliferative disorders such as atherosclerosis and restenosis, as well as in tumor associated neovascularization, suggests the involvement of T-cadherin in pathological angiogenesis [9–12]. However, the role of T-cadherin in the vasculature is poorly understood.
In our lab, T-cadherin has been isolated as a receptor responsible for hormone-like signaling effects of low density lipoproteins (LDL) [13] and was shown to mediate LDL-induced cell signaling and cell migration in vitro [14]. Adenoviral overexpression of T-cadherin in HUVEC (human umbilical endothelial cells), facilitates spontaneous cell migration, and change of the phenotype from quiescent to promigratory [15]. It is likely that homophilic interaction of T-cadherin in endothelial cells results in activation of small G-proteins, RhoA/ROCK, and Rac pathways with subsequent reorganization of actin cytoskeleton and stress fiber formation [15]. However, in vivo effects of T-cadherin for angiogenesis remain to be investigated.
The purpose of this study was to define the role of T-cadherin in angiogenesis in vivo and to elucidate the possible mechanisms of T-cadherin functioning in the vascular system. We demonstrate that T-cadherin could act as a negative guidance cue for growing vessels. Using Matrigel implant we show that T-cadherin expression in the stroma inhibits neoangiogenesis. T-cadherin expressed on the cells surface mediates homophilic interaction and contact inhibition resulting in suppressed endothelial cell migration.
Materials and methods
Cell culture and transfection
As previously described [14, 16], L929 cells were stably transfected with T-cadherin (pcDNA 3.1) using Lipofectamin 2000 reagent. Luciferase cDNA fragment in antisense orientation was cloned into the pcDNA 3.1 vector and used as a control. T-cadherin expression in control and T-cadherin transfectants was examined using Western blotting [14]. For Matrigel experiments, L929 cell were maintained in DMEM containing 100 U/ml penicillin, 100 U/ml streptomycin, and 10% fetal bovine serum (DMEM/FBS) at 37°C and 5% CO2.
Matrigel implantation into NUDE mice
All animal work was approved by Institutional Ethical Committee (Cardiology Research Complex). 400 μl of ice-cold Matrigel matrix (BD) was premixed with 1.7 × 106 L939 cells (either expressing T-cadherin or control plasmid) in 100 μl of complete DMEM. NUDE mice of 8–12 weeks were anesthetized with by i.p. injection of 2.5% avertin. 500 μl of cell suspension in Matrigel was injected subcutaneously into the right and left sides of the mouse back (spatula region) using 22G needle. Around 3, 7, 10, and 14 days after injection mice were sacrificed and the entire Matrigel plugs were isolated. Quantification of blood vessels was achieved using immunofluorescent visualization of blood vessels on frozen Matrigel sections and by measuring the amount of hemoglobin contained in the plugs [17]. Weight measuring of the Matrigel plugs was followed by dividing each plug into two parts: one was immediately used for hemoglobin assessment and the other was placed in O.C.T. Compound (Sakura Inc., Tokyo, Japan) and frozen in liquid nitrogen for immunofluorescent analysis.
Hemoglobin assessment
Hemoglobin content was analyzed using cyanhemoglobin method (Drabkin’s method) modified by us for tissues. Briefly, fragments of Matrigel plugs were weighed and homogenized in 200 μl of 0.9% NaCl saline using electric homogenizer (Janke & Kunkel, IKA-Labor Technic) following by centrifugation at 5,000 rpm for 7 min. Supernatant was cleared by adding 100 μl of chloroform per 50 μg of Matrigel specimen with subsequent centrifugation at 13,000 rpm for 3 min. Hemoglobin in the specimen was converted to CN-derivative by adding 150 μl of Drabkin’s solution containing K3Fe(CN)6, KCN, KH2PO4, and TritonX-100; the sample was incubated at room temperature for 15 min and A594 absorbance was measured using spectrophotometer (Janako).
Immunofluorescent staining of blood vessels
Blood vessels were visualized by immunofluorescent staining of 6 μm frozen Matrigel sections using rat anti-mouse CD31 antibody (BD Pharmigen™, 0.125 μg/ml in BSA/normal serum solution) as described previously [17, 18]. This was followed by incubation with Alexa 594-conjugated anti-rat antibody (Molecular Probes, 10 μg/ml in PBS). To assess the number of mature vessels, we performed double immunofluorescent staining with rat anti-mouse CD31 antibody combined with rabbit anti-mouse α-actin (Epitomics, 1:500) or rabbit anti-NG2 (Chemicon, 1:200) antibodies to visualize smooth muscle cell (SMCs) or pericytes, respectively. This was followed by incubation with the mixture of secondary antibody: Alexa 594-conjugated anti-rat antibody and Alexa 488-conjugated donkey anti-rabbit antibody. Cell nuclei were counterstained with DAPI (Molecular Probes). For negative controls rat or rabbit non-specific IgGs were used in appropriate concentration. Images were obtained using Zeiss Axiovert 200M microscope equipped with CCD camera AxioCam HRc and Axiovision software (Zeiss) and further processed using Adobe PhotoShop software (Adobe Systems).
Quantification of vessel density (VD) and statistical analysis
Vessel size and density was evaluated using MetaMorph 5.0 (Universal Imaging) and Adobe PhotoShop software (Adobe Systems). VD was determined as the number of CD31-positive vessels in a field normalized to the DAPI-stained area unit of each Matrigel section. For the quantification of VD, vessel numbers were counted in 4–5 fields of view (1.107 mm2) on three random sections for each Matrigel plug at 100× total magnification (10× objective). All vessels were separated into three groups: capillaries (CD31-positive vessels without lumen and with length less than 20 μm); medium vessels (CD31-positive vessels with length 20–40 μm) and large vessels (with diameter >40 μm); the number of vessels in each group was counted separately. All experiments were repeated at least three different times in triplicates. Data are expressed as mean ± SEM. Data were analyzed using Mann–Whitney U-criteria. Differences with P < 0.05 were considered as statistically significant.
HUVEC proliferation
Effect of T-cadherin on proliferation of HUVEC was analyzed either by co-cultivating HUVEC with T-cadherin-positive or T-cadherin-negative cells, or by cultivating HUVEC using conditioned medium from T-cadherin-negative or T-cadherin-positive cells. The conditioned medium from L939 was centrifuged at 1,000g for 10 min, concentrated 100 times using Centricon YM-10, Millipore filter, and supplemented with 1–10% of FBS and 200 μg/ml ECGF (RELIA Tech GmbH, Germany). For co-cultivating assay, HEK293 cells expressing GFP/T-cadherin or GFP/control plasmid [14] and HUVEC were seeded in co-culture on fibronectin (Sigma) coated cover glass in the ratio of 1:5, 1:2, and 1:1, and incubated in at 37°C in a humidified 5% CO2 for 48 h. Cells were fixed in 4% paraformaldehyde and ethanol and processed for immunofluorescent staining as described earlier. Human PCNA antigen (proliferating cell nuclear antigen) (DakoCytomation) was used as a marker of proliferating cells; this was followed by incubation with Alexa-594 conjugated secondary antibody. Proliferating HUVEC cells showed red fluorescence, while proliferating HEK293/GFP cells had double fluorescence in the green and red channels. The number of PCNA-positive HUVEC was calculated in 4–5 fields of view on each cover glass at 200× total magnification; the obtained number of PCNA-positive HUVEC cells was normalized to the total number of HUVEC for each field of view. Data were analyzed using Mann–Whitney U-criteria.
Generation of T-cadherin fragments
As described earlier, human cDNA encoding EC1 and EC5 domains of T-cadherin were obtained by PCR [19], cloned into pET-21 a(+) (Novagen) vector, and overexpressed in Escherichia coli strain BL 21 (DE3) by induction with 1 mM isopropyl-D-thiogalactopyranoside (IPTG) for 4 h. Using the procedures described by the manufacturers, the proteins were purified on a nickel affinity column (Ni-NTA agarose, Qiagen GmbH, Hilden, Germany) from the supernatant of lysed cells. T-cadherin domains were eluted from the column with 250 mM imidazole, dialyzed against PBS, and sterilized by passing through 0.22-μm filter. Protein concentration was determined by the Bradford assay with BSA (Sigma) as a standard (Bio-Rad).
HUVEC adhesion
The effect of T-cadherin on HUVEC adhesion was examined using either T-cadherin domains precoated plastic dishes or a monolayer of T-cadherin-positive or T-cadherin-negative cells. In the first case, adhesion assays were performed as described earlier with some modifications [19]. Briefly, 24-well dishes were precoated overnight at 4°C with 0.1% gelatin including EC1 or EC5 (control) recombinant domains of T-cadherin in concentration 0.1 mg/ml or BSA. After absorption the dishes were washed with sterile PBS. Prior to adhesion assay, HUVEC were incubated for 12 h at 37°C in a solution of 0.2 μg/ml fluorescently labeled acetylated low-density lipoprotein (Ac-LDL-Alexa488 (Invitrogen)) as described [20]. Specifically labeled HUVEC were seeded on the precoated plates at a density 8 × 104 cells/well and cultured (DMEM supplemented by 10% FBS (HyClone), 200 μg/ml ECGF (RELIA Tech GmbH, Germany), 5 U/ml heparin, 1 mМ sodium pyruvate (GIBCO BRL), 20 mМ HEPES (Helicon), 100 μg/ml penicillin, and 100 μg/ml streptomycin (GIBCO BRL)). In the second case, L929 T-cadherin-positive or T-cadherin-negative cells were seeded at various densities (2 × 104–105 cells/well) on 24-well dishes and cultivated until 50–100% cell monolayer. HUVEC prelabeled with Ac-LDL-Alexa488 were seeded on top of L929 T-cadherin-positive or T-cadherin-negative cells. Cells in each case were incubated at 37°C for 2 h and examined by fluorescent Axiovert 200M microscope equipped with CO2 incubator and heating stage (Zeiss). Live images were taken using CCD camera AxioCam HRc (Zeiss) at 200× total magnification in 4–5 fields of view for each well and analyzed with Axiovision software (Zeiss). All experiments were repeated at least three times in triplicates. Data are expressed as mean ± SEM. Data were analyzed using Mann–Whitney U-criteria. Differences with P < 0.05 was considered as statistically significant.
Apoptosis assay
The effect of recombinant fragments of T-cadherin on endothelial cells apoptosis was assessed using Сaspase-3 Colorimetric Assay (R&D Systems, CN BF3100) according to manufacturer’s instructions. Briefly, culture dishes were precoated for 12 h at +4°С with 0.2% gelatin containing either 0.1 mg/ml of EC1 or EC5 domain or 0.1 mg/ml of BSA. HUVEC were detached by trypsinisation and seeded onto precoated substrate at a density of 7 × 104 HUVEC per cm2 in the endothelium growth medium. After incubation for 18 h at 37°C, cells were detached from the plastic dish using 0.02% EDTA solution and centrifuged at 1,000g for 10 min. Cell pellet was lysed by addition of the Lysis buffer supplied with the kit. The cell lysates were added to 96 well microplate and incubated with caspase-3 substrate at 37°C for 2 h. Absorbance in wells was measured at 405 nm. As a positive control HUVECs were incubated for 18 h in the growth medium containing 1% FBS and 1nM staurosporine (Sigma) to induce apoptosis in endothelial cells. All experiments were repeated three times in triplicates. Data were expressed as mean ± SEM. Data were analyzed using Mann–Whitney U-criteria. Differences with P < 0.05 was considered as statistically significant.
Tube formation assay
The formation of vascular-like structures by HUVECs on growth factor-reduced Matrigel (BD Biosciences) was performed as previously described [21] according to the manufacturer’s instructions. Around 5 × 104 of HUVEC (passage 2–4) were seeded on Matrigel and incubated at 37°C for 24 h in the complete endothelial cells growth medium.
To evaluate the effect of immobilized T-cadherin on tube formation we polymerized Matrigel and then allowed EC1 or EC5 (control) peptide solutions (0.1 mg/ml) or PBS to infiltrate Matrigel overnight. For positive control HUVECs were allowed to form tubes in the complete endothelial cells growth medium, for negative control tubes were formed in the growth factor-reduced medium (0.5% FBS without ECGF). To assess the effect of soluble EC1 or EC5 domains, cells were incubated on polymerized Matrigel in the presence of 0.1 mg/ml soluble recombinant peptides. The average length of formed capillary-like structures was quantified by measuring the length of tubes in five randomly chosen fields from each well, using MetaMorph 5.0 (Universal Imaging) software. All experiments were repeated three times in triplicates. Data are expressed as mean ± SEM. Data were analyzed using Mann–Whitney U-criteria. Differences with P < 0.05 were considered as statistically significant.
Rat ring aorta assay
To study the action of T-cadherin on angiogenesis we used cultured aorta explants in three-dimensional matrix gels [22] with some modifications. Around 8–12-week-old Wistar male rats were sacrificed and thoracic aortas were immediately placed into a cold serum-free essential medium (RPMI1640, GIBCO). The peri-aortic fibroadipose tissue was carefully removed and 3 mm-long aortic rings (approximately 8 per aorta) were sectioned and embedded in growth factors reduced Matrigel (BD Pharmingen), containing EC1 or EC5 (control) T-cadherin domains (at various concentrations: 0.0004; 0.001; 0.002; 0.02 mg/ml) or PBS. Matrigels were kept at 37°C in a humidified incubator for 14 days and examined every second day. Experiments were repeated 4 times in triplicates. The area covered by sprouted capillaries per 1 mm of ring side, as well as average length of sprouts were analyzed using MetaMorph 5.0 (Universal Imaging) software. All experiments were repeated three times in triplicates. Data were expressed as mean ± SEM. Data were analyzed using Mann–Whitney U-criteria. Differences with P < 0.001 was considered as statistically significant.
HUVEC migration in Boyden chamber
Migration of HUVEC was assessed in Boyden chamber using 8 μm pore size membrane (NeuroProbe Inc.) as described previously [23]. Briefly, 1 × 105 serum-deprived HUVEC were suspended with 0.05% trypsin-EDTA (Invitrogen) and seeded in serum-free DMEM on top of the membrane in Boyden chamber. HUVEC were allowed to migrate for 4 hrs at 37°C using 1–10% of FBS as chemoattractant. Non-migrated cells were removed; membrane with cells was fixed in 100% ethanol and stained in Diff-Quick, scanned, and analyzed using Image-J software (National Institute of Health).
To assess the contact-dependent effect of T-cadherin on HUVEC migration, the membrane on its upper side was precoated with 0.2% gelatin solution containing 0.1 mg/ml of recombinant EC1 or EC5 (control) domains. After incubation for 12 h at 37°С the membrane was analyzed in HUVEC migration assay. HUVEC were allowed to migrate to the growth medium containing 1.5 or 10% of FBS. To analyze the effect of soluble domains, 0.1 mg/ml of peptides was added to the lower chamber.
To examine the possibility of T-cadherin shedding and the effect of the soluble T-cadherin on HUVEC migration, as a chemoattractant we used conditioned medium from T-cadherin-negative or T-cadherin-positive L939 cells in the presence of 1–10% of FBS and appropriate supplements. The conditioned medium was centrifuged at 1,000g for 10 min and concentrated 100 times using Centrycon YM-10, Millipore filter. All experiments were repeated three times in triplicates. Data are expressed as mean ± SEM. Data were analyzed using Mann–Whitney U-criteria. Differences with P < 0.05 were considered as statistically significant.
Results
Local T-cadherin overexpression in Matrigel plugs
To reveal the role of T-cadherin in the growth of blood vessels in an in vivo model, we have subcutaneously injected Matrigels containing T-cadherin-positive or T-cadherin-negative L939 cells into the spatula region of the mouse back. The cells implanted in Matrigel retained their viability up to 14 days, assuring the sustained expression of T-cadherin over the course of the entire experiment (our unpublished observations). Matrigel plugs were isolated 3, 7, 10, and 14 days after injection, and their vascularization by vessels outgrowing from a. subclavia was assessed. In all cases Matrigel implants with L939 cells overexpressing T-cadherin were smaller in size, had a yellowish color, and newly-formed vessels were smaller in diameter (Fig. 1A).
Matrigel plugs. (A) Macroscopic view of representative Matrigel plugs containing L939 cells: T-cadherin-negative cells (control) or T-cadherin positive cells. (B) Hemoglobin content in Matrigel implants measured by cyanhemoglobin method at 3, 7, and 10 days. Data presented as mean ± SEM from 14 plugs; *P < 0.05
At the day 14, plugs with T-cadherin expressing cells were significantly smaller in weight (0.28 ± 0.02 vs. 0.45 ± 0.02 in control, P < 0.01), which was accounted for by the clearly pronounced difference in vascularization. The hemoglobin content normalized to the weight of the analyzed fragment of Matrigel was significantly lower in T-cadherin plugs (0.74 ± 0.04 vs. 1.17 ± 0.08 in control, P < 0.05). The difference in hemoglobin content, reflecting the blood flow, becomes evident at the day 10, the time normally required for the Matrigel plug to develop a vascular network [17, 24]. Dynamic analysis over the whole period of incubation (from day 3–day 14) demonstrated that the hemoglobin content in Matrigel plugs overexpressing T-cadherin was lower at all tested time points (Fig. 1B). Thus, injection of cells overexpressing T-cadherin suppresses vessel ingrowth into the Matrigel implant.
T-cadherin overexpression suppresses capillaries but not mature vessels
To clarify which stage of vessel growth or maturation is affected by T-cadherin expressed in the surrounding tissue, we have analyzed the vessel density, size, and the type/quality of blood vessels. Matrigel sections were taken from various parts of the plug and stained with antibody against endothelial marker CD31 (Fig. 2A, B). There was no difference in the vascular density for large vessels (with lumen diameter >40 μm) between control and T-cadherin plugs (1.25 ± 0.22 vs. 1.27 ± 0.33; P > 0.05), whereas for small vessels (with lumen diameter <40 μm and length >20 μm) the vessel density was significantly lower in the plugs overexpressing T-cadherin (91.5 ± 7,2 vs. 207.6 ± 9.7; P < 0.05). The density of capillaries (vessels without visible lumen or with length <20 μm) was also significantly lower in the plugs overexpressing T-cadherin compared to control (Fig. 2E). In Matrigel plugs with control L929 cell vast majority of vessels expressed T-cadherin. However, in Matrigel plugs with T-cadherin expressing L929 cells, the number of T-cadherin-positive vessels was significantly lower (Fig. 2C, D, F).
Vascularization of Matrigel plugs. (A, B) Immunofluorescent staining of frozen Matrigel section with antibodies against endothelial marker CD31 (red fluorescence). Large vessels are indicated by the arrowheads, small vessels—by double arrows and capillaries—by single arrows. Scale bars—100 μm. (C, D) Double immunofluorescent staining of T-cadherin (green fluorescence) and CD31 (red fluorescence) on sections of control Matrigel plug (C) and Matrigel with T-cadherin expressing cells (D). Yellow staining represents blood vessels expressing T-cadherin, while red staining—vessels which do not express T-cadherin. Nuclei are counterstained with DAPI. (E) The density of capillaries was determined as the number of CD31-positive vessels in a field normalized to the DAPI-stained area unit of each Matrigel section. (F) The proportion of capillaries expressing T-cadherin was determined as the number of double stained vessels (CD31/T-cadherin) to the total number of vessels (CD31). Data present as mean ± SEM of 42 sections; *P < 0.05. Scale bars—20 μm
One of the possible reasons for the reduced vessel density of capillaries and small vessels in the plugs with T-cadherin-positive cells could be an impaired stabilization of the newly-forming vessels. To find out if local expression of T-cadherin by L929 fibroblasts in the Matrigel affects maturation of blood vessels we evaluated the density of vessels surrounded by mural cells. Mature vessels were revealed by double immunostaining with antibodies against endothelial (CD31) combined with antibody against α-SM actin (SMCs) or antibody against pericytes (NG2 antigen) [25, 26]. There was no difference in vessel density of double positive CD31/α-SM actin or CD31/NG2 vascular structures (Fig. 3), indicating that T-cadherin overexpression exerts no effect on vessel maturation in Matrigel implants.
Mature and nascent blood vessels in Matrigel plugs. (A, B) Double immunofluorescent staining of frozen Matrigel section with antibodies against endothelial marker CD31 (red fluorescence) and smooth muscle α-actin (green fluorescence). (C, D) Double immunofluorescent staining of frozen Matrigel section with antibodies against endothelial marker CD31 (red fluorescence) and NG2 pericyte antigen (green fluorescence). (E) Vessel density of CD31-positive vascular structures, α-actin-positive or both antigens-positive vessels on sections normalized to the DAPI-stained section area. (F) Vessel density of double positive CD31 and NG2 vascular structures on sections normalized to the DAPI-stained section area. Data present as mean ± SEM of 42 sections. Data present as mean ± SEM of 42 sections. *P ( 0.05. Scale bars—20 μm
Cadherin recombinant fragments are used extensively for in vitro evaluation of cadherin effects on cell adhesion, proliferation, and cell sorting [19, 27]. To reveal the role of T-cadherin in endothelial cell adhesion, proliferation, apoptosis, and migration we used its recombinant fragments in our in vitro experiments.
Recombinant N-terminal domain of T-cadherin inhibits angiogenesis in vitro
To confirm that T-cadherin acts as angiogenesis inhibitor we tested the ability of recombinant T-cadherin fragments to inhibit the formation and growth of capillary network in the Matrigel tube and rat ring aorta assays in vitro. Amino-terminal EC1 and juxtamembrane EC5 extracellular domains of T-cadherin were aseptically purified in LPS-free system. We have previously characterized and used recombinant T-cadherin and its domains in a number of studies to mimic T-cadherin action [19]. EC1 domain of cadherins is known to be crucial for cell recognition and formation of cell–cell contacts, while EC5 domain is frequently used as a negative control [27]. Incubation of HUVEC, which endogenously expresses T-cadherin, in the presence of soluble EC1 or EC5 domains in 0.1 mg/ml concentration in the media did not affect formation of capillary-like structures in the capillary tube assay (Fig. 4). However, immobilization of EC1, but not of EC5 domain, on Matrigel suppressed tubulogenesis (Fig. 4). Consistent with this, in the rat aortic ring assay the immobilization of EC1 on Matrigel resulted in a marked reduction (2–3-fold) of capillary growth and sprouting compared to EC5 domain. The effect of EC1 was evident at all time points (from 3 days to 14 days) and was dose-dependent (Fig. 5). These data indicate that in contrast to soluble T-cadherin fragments, immobilized EC1 domain of T-cadherin, which mimics homophilic cell–cell interactions [25], significantly suppresses angiogenesis in in vitro models.
In vitro formation of capillary-like structures by HUVEC in Matrigel containing either EC1 or EC5 domains of T-cadherin. (A, B) Representative views of wells with HUVEC seeded on Matrigel with inclusion of indicated domains. (C) Average tube length calculated from four independent experiments performed in triplicates. Data presented as mean ± SEM; *P < 0.05. Scale bars—50 μm
Suppression of vessel outgrowth by EC1 domain of T-cadherin from rat aorta rings. (A) Representative views of aorta rings placed in Matrigel with inclusion of indicated domains of T-cadherin after 3 and 14 days of incubation. (B) Average length of outgrowing microvessels calculated from 12 wells in four independent experiments. (C) Dose-dependent suppression of vessel outgrowth calculated in % from control in three independent experiments. Data presented as mean ± SEM; *P < 0.001. Scale bars—650 μm
T-cadherin specifically targets endothelial cell migration, but not proliferation, apoptosis or cell sorting
To further investigate the mechanism of the inhibitory effect of T-cadherin on angiogenesis we examined its action on endothelial cell proliferation, apoptosis, and migration. Co-culturing of either L939 or HEK293 (T-cadherin-positive or control cells) with HUVEC exerted no effect on the number of PCNA-positive endothelial cells (Fig. 6A). There was also no inhibitory effect of T-cadherin on HUVEC adhesion, since no significant difference in the number of adherent HUVEC seeded on EC1 or EC5 domains or BSA precoated plastic was registered. Similarly, T-cadherin expression on the cell surface did not interfere with HUVEC adhesion onto a monolayer of L929 cells (data not shown). Furthermore, seeding HUVEC on plastic coated with gelatin including EC1 domain (0.1 mg/ml) did not cause the activation of caspase-3, a key switch of the apoptosis in HUVEC (Fig. 6B). These data suggest that the inhibitory effect of T-cadherin is not related to the down-regulation of endothelial cell proliferation or adhesion or apoptosis induction.
Effects of T-cadherin on HUVEC. (A) Proliferation of HUVEC in co-culture with HEK cells overexpressing T-cadherin (HEK293+) or control cells (HEK293−) calculated by the number of PCNA-positive cells. (B) Caspase-3 activity in HUVEC cultured on EC1 precoated dishes as assessed by colorimetric assay. Data present as mean of three independent experiments performed in six repeats each ±SEM; P = 0.05. (C) Migration of HUVEC in Boyden chamber through the membrane coated by recombinant domains of T-cadherin. EC1-aminoterminal extracellular domain of T-cadherin; EC5—juxtamembrane extracellular domain. Data presented as mean of three independent experiments performed in six repeats each ± SEM; *P < 0.05
However, the migration of HUVEC in Boyden chamber through the membrane coated with EC1 domain, important for cell–cell interaction, was reduced by 2-folds compared to control (EC5) domain (Fig. 6C), indicating that T-cadherin could act as an inhibitor of endothelial cell migration. This assumption is also supported by the results of the capillary tube (Fig. 4) and rat aortic ring (Fig. 5) assays, where EC1 domain in the Matrigel mimics cell–cell interactions and suppresses migration-dependent processes such as tubulogenesis, capillary growth, and sprouting. In summary, the key findings of this study are that T-cadherin down-regulates angiogenesis in vivo and in vitro and that the mechanism of its action lies in the inhibition of endothelial cell migration.
Discussion
In normal adult organisms, most of the vasculature is quiescent. Excessive or insufficient vascular growth contributes to non-neoplastic disorders, abnormal vessel remodeling, or tumor angiogenesis. Since tumor growth is dependent on recruiting new vessels, the inhibition of tumor angiogenesis is an effective method to suppress cancer [28, 29].
T-cadherin is endogenously expressed in the human vasculature in endothelial cells, smooth muscle cells, pericytes, and cardiomyocytes [9]. Moreover, T-cadherin expression is upregulated in a set of pathological conditions associated with excessive angiogenesis [9–12]. However, the physiological role of T-cadherin in vascular system remains largely elusive.
Our previous studies have implicated T-cadherin in vascular wall remodeling associated with excessive angiogenesis in restenosis and atherosclerosis [9, 10]. The present data provide the first evidence that T-cadherin specifically inhibits endothelial cell migration and capillary formation. This interaction requires endothelial cell contacts with T-cadherin expressing stromal cells or with immobilized EC1 domain, which mimics such cell–cell interactions [19, 30]. Our present data suggest that T-cadherin when abundantly expressed in microenvironment suppresses angiogenesis.
Overexpression of T-cadherin using adenoviral or plasmid transfection promotes HUVEC proliferation [19, 31, 32] and facilitates spontaneous cells migration of endothelial and other cells [14, 16]. In HUVEC, overexpression of T-cadherin protects cells from apoptosis and increases survival after exposure to oxidative stress [33]. These findings are in line with in vivo studies on T-cadherin expression in tumor vessels. In Lewis carcinoma lung metastasis, Т-cadherin is upregulated in blood vessels penetrating the tumor, while in the surrounding tissue T-cadherin is not detected [11]. Similarly, in hepatocellular carcinoma (HCC) T-cadherin expression is increased in intratumoral capillary endothelial cells during neovascularization, whereas in the surrounding tumor tissue as well as in normal liver Т-cadherin is not detected [12]. Together, this evidence indicates that T-cadherin expression in endothelial cells in vitro or in growing vessels in vivo correlates with enhanced angiogenesis. However, in these models the role of T-cadherin expression by stromal cells in neoangiogenesis is not considered. In contrast, in our Matrigel model, L929 cells when injected into the plug, create the microenvironment with high level of T-cadherin. In these settings migrating endothelial cell, which naturally express T-cadherin contact T-cadherin positive stromal cells and this interaction results in suppressed blood vessel growth. This effect of T-cadherin is dependent upon the concentration of T-cadherin expressing cells injected into the Matrigel (data not shown). Consistently, suppression of vessel outgrowth in rat ring aorta assay is also dependent upon the concentration of EC1 domain in the Matrigel. These data suggest that homophilic interaction between T-cadherins on the cell surface could mediate the contact inhibition of endothelial cell invasion of the Matrigel stroma. This assumption has been further confirmed by quantitative and qualitative analysis of blood vessels of the Matrigel plugs. The amount of large blood vessels is not affected by the presence of T-cadherin in the Matrigel, while the number of small vessels and capillaries is dramatically reduced, suggesting that the early stages of neoangiogenesis has been affected. Furthermore, small vessels and capillaries having invaded the Matrigel plug with high level of T-cadherin do not express T-cadherin. Conceivably, T-cadherin expression in the stroma regulates qualitative composition of blood vessels infiltrating the tissue either by negative guiding of T-cadherin expressing vascular endothelial cells or by downregulation of T-cadherin expression in the growing vessels, or both. This would explain why T-cadherin was suggested to function as a tumor-suppressor factor [11, 34, 35] and why downregulation of Т-cadherin in stroma cells of such tumors as basal сеll carcinoma, cutaneous squamous carcinoma, non-small сеll lung carcinoma (NSCLC), ovarian cancer, pancreatic cancer, and colorectal cancer [36–41] correlates with cancer progression.
The mechanism of T-cadherin mediated blood vessel growth suppression could be analogous to contact inhibition observed in the nervous system where T-cadherin acts as a negative guidance cue. There is now substantial evidence for а cross-talk between the vascular and nervous systems and that the same guiding molecules participate in neuronal and vascular growth [42]. At least four families of guidance molecules, which mediate repulsive or attractive behavior are known: netrins and their receptors DCC/neogenin and Unc5, slit ligands, and their roundabout (Robo) receptors, semaphorins, and their receptors plexin and neuropilin, ephrins and ephrin receptors [43, 44]. T-cadherin is another molecule, which guides blood vessels and growing axons through the complex environment to their targets by selecting pathways and choosing directions (Fig. 7). Ephrins and their Eph receptors are known to be involved both in guidance in the developing nervous system, and in embryonic and tumor angiogenesis [45, 46]. Interestingly, Ephrins A are also anchored to the plasma membrane via a GPI anchor [45, 46], suggesting a potential analogy between Ephrins A and T-cadherin. Interaction of ephrins with their receptors can result either in attraction, adhesion and invasion, or decreased adhesion and repulsion. The mechanisms of GPI-anchored ephrin signaling are still obscure but probably involve ligand clustering within lipid rafts and interaction with adaptor proteins. Even less is known about T-cadherin signaling partners, yet some signaling mechanism of GPI-anchored Ephrins A and T-cadherin could be similar.
In the developing nervous system T-cadherin expresses neural crest cells, growing ахоns, and axons projecting through the somitic sclerotome avoid T-cadherin expressing tissues [6, 47, 48]. Thus, we speculate that T-cadherin acts as a negative guidance cue and that the general mechanism of T-cadherin mediated repulsion could involve homophilic T-cadherin interaction and contact inhibition. This assumption has been confirmed in our in vitro experiments utilizing immobilized EC1 domain, which is responsible for homophilic T-cadherin interaction of contacting cells [19]. The migration of endothelial cell, which endogenously express T-cadherin [16] is inhibited by immobilized EC1 in Boyden chamber assay, ring aorta, and capillary tube in vitro assays in contrast to soluble T-cadherin domains. In vivo T-cadherin expression in the microenvironment of Matrigel plugs inhibits the ingrowth of small vessels and capillaries but does not affect pericyte recruitment and the maturation of blood vessels. Dynamic evaluation of hemoglobin content in Matrigel supports the assumption that T-cadherin inhibits angiogenesis by suppressing directed endothelial cell migration and vessel invasion into the plug. Interestingly, T-cadherin does not affect endothelial cell proliferation, adhesion, or apoptosis.
Our data demonstrate for the first time that T-cadherin expression in the microenvironment suppresses the growth of blood vessels. Tumor stroma is not just an inert environment [49] and “activated fibroblasts” of the tumor at the site of metastasis promote cancer cell proliferation and also support the initiation of angiogenesis; while normal fibroblasts, when injected into the tumor stroma can inhibit cancer progression [50]. Thus, application of cells constitutively expressing T-cadherin might serve as a novel therapeutic approach in cancer.
References
Cavallaro U, Leibner S, Dejana E (2006) Endothelial cadherins and tumor angiogenesis. Exp Cell Res 312:659–667
George SJ, Beeching CA (2006) Cadherin:catenin complex: a novel regulator of vascular smooth muscle cells behaviour. Atherosclerosis 188:1–11
Gumbiner BM (2005) Regulation of cadherin-mediated adhesion in morphogenesis. Nature Rev Mol Cell Biol 6:622–634
Perez-Moreno M, Jamora C, Fuchs E (2003) Sticky business: orchestrating cellular signals at adherens junctions. Cell 112:535–548
Rubina KA, Kalinina NI, Bochkov VN, Parfyonova YeV, Tkachuk VA (2005) T-cadherin as an antiadhesive and guidance molecule interacting with low density lipoproteins. Annals EAS 1–14
Ranscht B, Dours-Zimmermann MT (1991) T-cadherin, a novel cadherin cell adhesion molecule in the nervous system lacks the conserved cytoplasmic region. Neuron 7:391–402
Rubina KA, Tkachuk VA (2004) Antiadhesive molecule T-cadherin is an atypical low-density lipoprotein receptor in vascular cells. RJ Physiol 90:968–986
Philippova MP, Bochkov VN, Stambolsky DV, Tkachuk VA, Resink T (1998) T-cadherin and signal-transducing molecules co-localize in caveolin-rich membrane domain of vascular smooth muscle cells. FEBS Lett 129:201–210
Ivanov D, Philippova M, Antropova J, Gubaeva F, Iljinskaya O, Tararak E, Bochkov V, Erne P, Resink T, Tkachuk V (2001) Expression of cell adhesion molecule T-cadherin in the human vasculature. Histochem Cell Biol 115:231–242
Kudrjashova E, Bashtrikov P, Bochkov V, Parfyonova Y, Tkachuk V, Antropova J, Iljinskaya O, Tararak E, Erne P, Ivanov D, Philippova M, Resink TJ (2002) Expression of adhesion molecule T-cadherin is increased during neointima formation in experimental restenosis. Histochem Cell Biol 118:281–290
Wyder L, Vitaliti A, Schneider H, Hebbrand LW, Moritz DR, Wittmer M, Ajmo M, Klemenz R (2000) Increased expression of H/T-cadherin in tumor-penetrating vessels. Cancer Res 60:4682–4688
Adachi Y, Takeuchi T, Sonobe H, Ohtsuki Y (2005) An adiponectin receptor, T-cadherin, was selectively expressed in intratumoral capillary endothelial cells in hepatocellular carcinoma: possible cross talk between T-cadherin and FGF-2 pathways. Virchows Arch 5:1–8
Tkachuk VA, Bochkov VN, Philippova MP, Stambolsky DV, Kuzmenko ES, Sidorova MV, Molokoedov AS, Spirov VG, Resink TJ (1998) Identification of an atypical lipoprotein-binding protein from human aortic smooth muscle as T-cadherin. FEBS Lett 421:208–212
Rubina K, Talovskaya E, Cherenkov V, Ivanov D, Stambolsky D, Storozhevykh T, Pinelis V, Shevelev A, Parfyonova Ye, Resink T, Erne P, Tkachuk V (2005) LDL induces intracellular signaling via atypical LDL-binding protein T-cadherin. Mol Cell Biochem 273:33–41
Philippova M, Ivanov D, Allenspach R, Takuwa Y, Erne P, Resink T (2005) RhoA and Rac mediate endothelial cell polarization and detachment induced by T-cadherin. FASEB J 19:588–590
Philippova M, Ivanov D, Tkachuk V, Erne P, Resink TJ (2003) Polarisation of T-cadherin to the leading edge of migrating vascular cells in vitro: a function in vascular cell motility? Histochem Cell Biol 120:353–360
Passaniti A, Taylor RM, Pili R, Guo Y, Long PV, Haney JA, Pauly RR, Grant DS, Martin GR (1992) A simple quantitative method for assessing angiogenesis and antiangiogenic agents using reconstituted basement membrane, heparin, and fibroblast growth factor. Lab Invest 67:519–528
Staton CA, Stribbling SM, Tazzyman S, Hughes R, Brown NJ, Lewis CE (2004) Current methods for assaying angiogenesis in vitro and in vivo. Int J Exp Path 85:233–248
Ivanov D, Philippova M, Tkachuk V, Erne P, Resink T (2004) Cell adhesion molecule T-cadherin regulates vascular cell adhesion, phenotype and motility. Exp Cell Res 293:207–218
Gifford SM, Grummer MA, Pierre SA, Austin JL, Zheng J, Bird IM (2004) Functional characterization of HUVEC-CS: Ca2+ signaling, ERK 1/2 activation, mitogenesis and vasodilator production. J Endocrinol 182:485–499
Nagata D, Mogi M, Walsh K (2003) AMP-activated protein kinase (AMPK) signaling in endothelial cells is essential for angiogenesis in response to hypoxic stress. J Biol Chem 278:31000–31006
Nicosia RF, Ottinetti A (1990) Modulation of microvascular growth and morphogenesis by reconstituted basement membrane gel in three-dimensional cultures of rat aorta: a comparative study of angiogenesis in matrigel, collagen, fibrin, and plasma clot. In Vitro Cell Dev Biol 26:119–128
Kim KS, Hong YK, Joe YA, Lee Y, Shin JY, Park HE, Lee IH, Lee SY, Kang DK, Chang SI, Chung SI (2003) Antiangiogenic activity of the recombinant kringle domain of urokinase and its specific entry into endothelial cells. J Biol Chem 278:11449–11456
Stieger SM, Bloch SH, Foreman O, Wisner ER, Ferrara KW, Dayton PA (2006) Ultrasound assessment of angiogenesis in a Matrigel model in rats. Ultrasound Med Biol 32:673–681
Gerhardt H, Betsholtz C (2003) Endothelial-pericyte interactions in angiogenesis. Cell Tissue Res 314:15–23
Bergers G, Song S (2005) The role of pericytes in blood-vessel formation and maintenance. Neuro-Oncology 7:452–464
Niessen CM, Gumbiner BV (2002) Cadherin-mediated cell sorting not determined by binding or adhesion specificity. J Cell Biol 156:389–399
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285:1182–1186
Cao Y (2005) Tumor angiogenesis and therapy. Biomed Pharmacother 9:340–343
Zhong Y, Lopez Barcons L, Haigentz M, Ling YH, Perez-Soler R (2004) Exogenous expression of H-cadherin in CHO cells regulates contact inhibition of cell growth by inducing p21 expression. Int J Oncol 24:1573–1579
Ivanov D, Philippova M, Allenspach R, Erne P, Resink T (2004) T-cadherin upregulation correlates with cells-cycle progression and promotes proliferation of vascular cells. Cardiovasc Res 64:132–143
Philippova M, Banfi A, Ivanov D, Gianni-Barrera R, Allenspach Erne P, Resink T (2006) Atypical GPI-anchored T-cadherin stimulates angiogenesis in vitro and in vivo. Artherioscler ThrombVasc Biol 26:2222–2223
Joshi MB, Philippova M, Ivanov D, Allenspach R, Erne P, Resink TJ (2005) T-cadherin protects endothelisl cells from oxidative stress-induced apoptosis. FASEB J 19:1737–1739
Takeuchi T, Misaki A, Liang SB, Tachibana A, Hayashi N, Sonobe H, Ohtsuki Y (2000) Expression of T-cadherin (CDH13, H-cadherin) in human brain and its characteristics as a negative growth regulator of epidermal growth factor in neuroblastoma cells. J Neurochem 74:1489–1497
Takeuchi T, Ohtsuki Y (2001) Recent progress in T-cadherin (CDH13, H-cadherin) research. Histol Histopathol 16:1287–1293
Kawakami M, Staub J, Clibi W, Hartmann L, Smith DI, Shridhar V (1999) Involvement of H-cadherin (CDH13) on 16q in the region of frequent deletion in ovarian cancer. Int J Oncol 15:715–720
Takeuchi T, Liang S-B, Ohtsuki Y (2002) Downregulation of expression of a novel cadherin molecule, T-cadherin, in basal cell carcinoma of the skin. Mol Cancerogen 35:173–179
Hibi K, Nakayama H, Kodera K, Ito K, Akiyama S, Nakao A (2004) CDH13 promoter region is specifically methylated in poorly differentiated colorectal cancer. Brit J Cancer 90:1030–1033
Sakai M, Hibi K, Koshikawa K, Inoue S, Takeda S, Kaneko T, Nakao A (2004) Frequent promoter methylation and gene silencing of CDH13 in pancreatic cancer. Cancer Sci 95:588–591
Kim JS, Han J, Shim YM, Park J, Kim DH (2005) Abberant methylation of H-cadherin (CDH13) promoter is associated with tumor progression in primary nonsmall cell lung carcinoma. Cancer 104:1825–1833
Mukoyama Y, Zhou S, Miyachi Y, Matsuyoshi N (2005) T-cadherin negatively regulates the proliferation of cutaneous squamous carcinoma cells. J Invest Dermatol 124:833–838
Carmeliet P (2003) Blood vessels and nerves: common signals, pathways and diseases. Nature Genet 4:710–720
Weinstein BM (2005) Vessels and nerves: marching to the same tune. Cell 120:299–302
Eichmann A, Makinen T, Alitalo K (2006) Neural guidance molecules regulate vascular remodeling and vessel navigation. Genes Dev 19:1013–1021
Poliakov A, Cortina M, Wilkinson DG (2004) Diverse roles of Eph receptors and Ephrins in the regulation of cell migration and tissue assembly. Dev Cell 7:465–480
Davy A, Soriano P (2005) Ephrins in vivo: look both ways. Dev Dynamics 232:1–10
Fredette BJ, Ranscht B (1994) T-cadherin expression delineates specific regions of the developing motoraxon-hindlimb projection pathway. J Neurosci 14:7331–7346
Fredette BJ, Miller J, Ranscht B (1996) Inhibition of motor axon growth by T-cadherin substrata. Development 122:3163–3171
Desmouliere A, Guyot C, Gabbiani G (2004) The stroma reaction myofibroblast: a key player in the control of tumor behavior. Int J Dev Biol 48:509–517
Kalluri R, Zeisberg M (2006) Fibroblasts in cancer. Nature Rev Cancer 6:392–401
Resink TJ, Kuzmenko YS, Kern F, Stambosly D, Bochkov VN, Tkachuk VA, Erne P, Niermann T (1999) LDL binds to surface expressed human T-cadherin in transfected HEK293 cells and influences homophilic adhesive interactions. FEBS Lett 463:29–34
Vestal DJ, Ranscht B (1992) Glycosyl phosphatidylinositol-anchored T-cadherin mediates calcium-dependent, homophilic cell adhesion. J Cell Biol 119:451–461
Acknowledgments
This work was supported by Welcome Trust grant # 075154 and Russian Foundation for Basic Research # 04-04-49399. We thank Dr. Olga Antonova for HUVEC culture, Vasiliy Cherenkov for purifying recombinant T-cadherin domains, Elizaveta Ratner for technical support and Elena Malinina for double immunofluorescent staining of Matrigel cryosections.
Author information
Authors and Affiliations
Corresponding author
Additional information
Kseniya Rubina and Natalia Kalinina have contributed equally to the work.
Electronic supplementary material
Below is the link to the electronic supplementary material
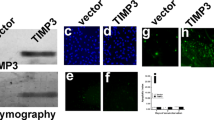
Fig. 8
Time-lapse live-cell fluorescence imaging. Representative views. (A, C) 4 days in co-culture of control HEK293 with HEK293 cells expressing GFP and T-cadherin (combined GFP and relief contrast image). (B, D) 2 days in co-culture of L929 cells expressing T-cadherin with control L929 cells labeled with CellTracker Green (combined CMFDA and relief contrast image). Scale bars – 50 μm
Appendices
Appendix
It was previously shown that T-cadherin could mediate weak homophilic adhesion in aggregation assays in vitro [51, 52]. To analyze whether T-cadherin is involved in adhesion that underlies cell sorting, we performed time-lapse live-cell fluoresce imaging. For these experiments we co-cultured control HEK293 cells with HEK293 cells co-expressing GFP and T-cadherin [14]; or CellTracker labeled control L929 cells with L929 cells expressing T-cadherin. Cells intermingled equally and we could detect no difference in the number, size, or distribution of fluorescently labeled cells in the aggregates (data not shown). There was also neither cell sorting nor T-cadherin-mediated repulsive or adhesive effects observed over a period of 2–4 days in time-lapse living cell experiments (Figure I, movie).
Materials and methods
Time-lapse live-cell fluorescence imaging
Time-lapse observations were performed using a DeltaVision Olympus IX70 inverted microscope with a ×20/0.40 NA objective lens with relief contrast optics. Cells were suspended with cell-dissociation buffer (Invitrogen, Gibco) before the experiment and plated in fibronectin-coated Lab-Tek Chambered #1.0 coverglass systems in 1:1 proportion. The total concentration of cells was 35.000/cm2. The cells were observed during 2–4 days in a 37°C environmental chamber. Each image was acquired with 4-min exposure of the CCD camera.
Labeling of cells with CellTracker reagent
Cells were labeled using CellTracker Green CMFDA reagent (Invitrogen, Molecular Probes) according to manufacturer instructions. In brief, the cells were incubated with 10 μM CMFDA for 15 min followed by incubation in fresh pre-warmed medium for another 30 min at 37°C.
Rights and permissions
About this article
Cite this article
Rubina, K., Kalinina, N., Potekhina, A. et al. T-cadherin suppresses angiogenesis in vivo by inhibiting migration of endothelial cells. Angiogenesis 10, 183–195 (2007). https://doi.org/10.1007/s10456-007-9072-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-007-9072-2