Abstract
In vitro culture of ovarian follicles isolated or enclosed in ovarian tissue fragments and grafting of isolated ovarian follicles represent a potential alternative to restore fertility in cancer patients who cannot undergo cryopreservation of embryos or oocytes or transplantation of frozen-thawed ovarian tissue. In this regard, respecting the three-dimensional (3D) architecture of isolated follicles is crucial to maintaining their proper follicular physiology. To this end, alginate hydrogel has been widely investigated using follicles from numerous animal species, yielding promising results. The goal of this review is therefore to provide an overview of alginate applications utilizing the biomaterial as a scaffold for 3D encapsulation of isolated ovarian follicles. Different methods of isolated follicle encapsulation in alginate are discussed in this review, as its use of 3D alginate culture systems as a tool for in vitro follicle analysis. Possible improvements of this matrix, namely modification with arginine-glycine-aspartic acid peptide or combination with fibrin, are also summarized. Encouraging results have been obtained in different animal models, and particularly with isolated follicles encapsulated in alginate matrices and grafted to mice. This summary is designed to guide the reader towards development of next-generation alginate scaffolds, with enhanced properties for follicle encapsulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies on in vitro culture of isolated ovarian follicles or ovarian tissue fragments and transplantation of isolated ovarian follicles have significantly increased over recent years thanks to a growing number of applications. For many decades, these techniques were largely used as a research tool to investigate folliculogenesis,49,56,81,104 a complex process that is far from being fully understood in all animal species. Now they also represent a potential alternative to restore fertility in cancer patients who cannot undergo other procedures like cryopreservation of embryos or oocytes, or transplantation of frozen-thawed ovarian tissue.4,32,103 Similarly, they can be used to obtain and exploit female gametes in preservation programs of endangered animal species.20,42,115 Finally, these techniques have also been applied in toxicological studies evaluating the impact of different chemicals and drugs on female fertility.6,24,65,73 However, identifying a system that accurately mimics the natural environment of follicles in order to understand how they develop in the original organ, react to potentially toxic chemical agents, and grow to produce viable oocytes has proved to be very challenging.
Andersen et al.8 stated that “the world around us, including the human body, is constructed in three dimensions”, so it is fair to say that the ovarian follicle is, by definition, a three-dimensional (3D) structure. Respecting its 3D architecture is therefore crucial to maintaining proper follicular physiology and obtaining responses resembling the expected behavior of follicles in vivo. Although ovarian follicles from rodents have been shown to survive and grow on flat surfaces,35 follicles from large mammals, including humans, cannot be made to develop normally in two-dimensional (2D) systems.1,43,82,102 Indeed, such in vitro culture conditions cause disruption in follicle architecture due to flattening because of granulosa cell (GC) attachment to the culture dish, which in turn interferes with their interactions among themselves and with the oocyte, leading to uncoordinated growth and differentiation of germ and somatic cells.75 For these animal species, 3D culture systems are essential, as they prevent dissociation of GCs from the oocyte, ensuring survival and correct development of isolated follicles, and providing follicular responses of biological significance.
A number of studies have reported 3D encapsulation of isolated follicles in various animal models using different scaffold materials, such as agarose,5,80 alginate,7,21,112 collagen,50,54,88,98,135 and hyaluronic acid.27 To date, the most widely applied biomaterial has been alginate, since it has yielded favorable results with follicles from numerous animal species. The goal of this review is to provide an overview of alginate use as a matrix for 3D encapsulation of isolated ovarian follicles, highlighting the most important results in different animal models. Ways of improving this matrix to optimize its application for in vitro culture or transplantation of isolated follicles will also be considered and discussed.
Characteristics of Alginate Hydrogels
Alginate is a collective term for a family of polysaccharides produced by brown algae or bacteria. Chemically, they are copolymers of 1 → 4 linked β-d-mannuronic acid (M) and α-l-guluronic acid (G) arranged in a blockwise pattern along the chain, with homopolymeric regions of M (M-block) and G (G-block) residues interspersed with regions of alternating (MG-block) structures (Fig. 1).30,45,46
Alginate has the ability to form stable hydrogels in the presence of millimolar concentrations of calcium or other divalent cations,47 like barium or strontium, that serve to crosslink G units (Fig. 2). This gelification property allows cell encapsulation under physiological conditions, with uniform distribution of cells throughout the matrix.60

Reprinted with permission from Shikanov et al.,90 Journal of Visualized Experiments (2016).
Alginate gelation characteristics. Areas with repeating G monomers, termed G-blocks, are cross-linked to form a hydrogel in the presence of divalent calcium ions.
The mechanical properties of the alginate beads are modulated by the polymer composition and/or concentration. Ouwerx et al.70 described that Young’s modulus of alginate beads formed in the presence of calcium (0.1 M) increased with the square of the alginate concentration: E = KC 2 (E = value for Young’s modulus; K = alginate specific constant; C = alginate concentration), demonstrating that alginate concentration is the parameter limiting the bead’s elasticity. Rheological analysis also showed a positive correlation between guluronic acid concentration and elastic modulus in alginate hydrogels33 and an influence of the gelling cation type70 and concentration on the alginate matrix.
Alginate is very easy to handle, as well as being biocompatible in vivo, which means its degradation products can be excreted through the urine.3 Once purified to remove endotoxins, proteins and polyphenol contaminants, it is also non-cytotoxic. For these reasons, alginate has been widely used for tissue engineering applications,34,64 including follicle encapsulation.
Encapsulation of Isolated Follicles in Alginate Beads
Encapsulation in alginate has proven to be a rapid, non-toxic and versatile procedure for cells and follicles, performed in two steps. The first involves an internal phase during which the alginate solution containing the biological material is separated into droplets, and the second, solidification of these droplets by gelling.8 The size of the droplets varies according to the amount of biological material to be encapsulated, the viscosity of the alginate solution, the system used to obtain the droplets, and the alginate flow rate.8
For follicle encapsulation, alginate droplets ranging from 5 to 60 µL in size have been investigated.52,72 Their size was not related to the number of follicles contained inside. For instance, Hornick et al.52 used 5 µL of alginate to encapsulate 1, 5 or 10 mouse primary or secondary follicles, while Amorim et al.7 embedded 4–8 human primordial-primary follicles in 20 µL of alginate.
Although different cell types have been successfully encapsulated in alginate by means of various automated systems, such as coaxial air flow, electrostatic generators, cell electrospinning or jet cutters,8,10,55,109 procedures described in the literature to embed ovarian follicles do not make use of any instrumentation. Alginate beads are usually made by dropping the alginate solution and follicles from a pipette tip directly into a crosslinking bath consisting of calcium solution,7,21,112 or immersing a mesh containing the droplets of alginate solution inside the crosslinking bath72 (Fig. 3). Another technique involves inversing the mesh to suspend the alginate droplets followed by quick shaking or tapping, so that the droplets fall into the crosslinking bath (Fig. 3).48,52,124,129 All these alternatives are able to successfully entrap isolated follicles in the hydrogel and are gentle on the follicles, not affecting their further survival or development in vitro.

©Reprinted with permission from Park et al.,72 Springer Science + Business Media (2016).
Different strategies to prepare alginate beads. Dropping method used by Amorim’s group (a, b), where one droplet of 1% alginate solution containing isolated follicles is released into calcium solution (a) to induce polymerization (b). Immersion method developed by Park et al.,72 where an alginate drop containing a single isolated follicle is placed onto a polycarbonate insert that is then plunged into a calcium solution (c). Inversion method applied by Woodruff’s team (d–f), where a droplet of alginate solution containing one follicle is first placed onto polypropylene mesh (d), which is then inverted over a dish containing calcium solution (e) and quickly shaken, so the droplets fall into the calcium solution for polymerization (f).
Shikanov et al.90 described two different procedures to encapsulate mouse follicles in a fibrin–alginate matrix. In the first, called the drop method, isolated follicles are washed in a rinsing droplet consisting of fibrinogen–alginate solution to remove the medium, before being transferred to the encapsulation droplet, containing the same fibrinogen and alginate concentrations as the initial droplet. Each follicle is individually aspirated in 5 µL of this solution and then expelled into a polymerization bath constituted of thrombin–calcium solution (Fig. 4). In the second, known as the parafilm method, an isolated follicle is first inserted into a 7.5 µL fibrinogen–alginate droplet placed on a parafilm-coated glass slide, to which 7.5 µL of thrombin–calcium solution is then added (Fig. 4).

Reprinted with permission from Shikanov et al.,90 Journal of Visualized Experiments (2016).
Different strategies to prepare alginate–fibrin beads proposed by Shikanov et al.90 Drop method (a–d): Two drops of fibrinogen–alginate solution are prepared on a dish, one for rinsing and the other to encapsulate follicles (a). Up to 5 follicles are washed in the first drop to remove the medium (b), before being transferred to the second drop (c). Each follicle is aspirated in 5 µL of encapsulation solution and then expelled into a polymerization bath containing thrombin–calcium solution (d). Parafilm method (e–g): Fibrinogen–alginate droplets are placed on a parafilm-coated glass slide (e) and, an isolated follicle is inserted into each droplet (f). For polymerization, a droplet of thrombin–calcium solution is added to each fibrinogen–alginate droplet.
Alginate Rigidity
Alginate rigidity, which is modulated by its composition and/or concentration, has been shown to have an impact on follicle survival and development, oocyte maturation and hormone production. Jiao et al.58 reported that the rigidity of an alginate matrix could affect oocyte-specific gene expression levels in oocytes. Moreover, denser matrices could potentially limit access to hormones and other nutrients. Although diffusible signals are generally able to spread throughout the hydrogel, Heise et al.48 found inhibited delivery of follicle-stimulating hormone (FSH) to microencapsulated follicles. Follicle diameters increased with addition of FSH to the hydrogel, but still did not reach the size observed in unencapsulated controls. It is important to bear in mind that in a 3D system, the mechanical force exerted by the matrix on cells around the exterior of the follicle will be transmitted to all cells within the follicle and will influence development and maturation. It may, for instance, affect actin organization, possibly activating one or more mechanoresponsive pathways.
Studies on alginate-encapsulated follicles have demonstrated that hydrogel rigidity needs to be carefully determined, as the scaffold must be sufficiently rigid to maintain the 3D structure of the follicle, yet soft enough to expand and allow oocyte growth, GC proliferation and antrum formation. Clearly, the physical attributes of the 3D matrix selected for in vitro follicle culture need to be tailored to meet species-specific requirements and take into account follicle stage. For example, primate secondary follicles embedded in 0.25% alginate beads were able to produce angiogenic factors, notably vascular endothelial growth factor A (VEGF-A), angiopoietin (ANGPT)-1 and ANGPT-2, which were regulated by gonadotropins and oxygen tension.38 In similar culture conditions, Rodrigues et al.76 showed that survival and growth, as well as steroid and anti-Müllerian hormone (AMH) secretion, could be influenced by direct action of androgens.
Alginate matrix stiffness appears to play a role in the survival and growth of follicles from all animal species. A number of studies have reported that alginate concentrations affect mouse follicle survival,72 paracrine communication between the cellular compartments of follicles,121 oocyte development,133 and antrum formation.72 Although different alginate concentrations ranging from 0.125 to 3% have been tested for in vitro culture of mouse follicles, West-Farrell et al.122 found folliculogenesis in this species to be better supported by lower alginate concentrations.
Brito et al.18 reported that isolated preantral follicles from goats could have undergone alterations to their morphology and hormone and enzyme levels according to concentrations of alginate used for their encapsulation. These authors observed that while higher alginate concentrations (0.5 and 1.0%) improved follicle morphology, a lower dose (0.25%) favored estradiol and progesterone production.18 In sheep, Sadeghnia et al.84 found that a stiffer alginate matrix (2%) was more suitable for development of primordial follicles.
Songsasen et al.97 showed that a lower alginate concentration (0.5%) enhanced growth of canine preantral and small antral follicles more successfully than a higher concentration (1.5%). Interestingly, smaller follicles from non-human primate species cultured in more rigid alginate scaffolds performed better than those in softer alginate structures, suggesting that primate follicles may require stronger physical support.51,134 Indeed, follicle survival and morphology were optimal when primate primordial follicles were cultured in 2% alginate compared to 0.5% alginate.51 However, most studies investigating 3D in vitro culture of primary–secondary follicles from non-human primate species found low alginate concentrations (0.25%) to work best.105–107,126,127,131,134
To humans, like in non-human primates, higher alginate concentrations are generally used for smaller preantral follicles, and lower concentrations for larger follicles. Softer matrices (0.3–0.5% alginate) are able to sustain survival and development of secondary follicles during long periods of in vitro culture,94,124,136 produce oocytes with nuclear maturation competence, demonstrating that this 3D culture system allows maintenance of bidirectional communication between GCs and the oocyte,13 and create an environment conductive to oocyte growth and proper steroid production.123,124 On the other hand, Yin et al.136 showed that although follicles from different stages of development are able to survive in such low alginate concentrations, secondary follicles exhibited significantly higher survival rates compared to their primary and primordial counterparts. Moreover, they could develop up to the antral stage and become steroidogenically active.136
For smaller human preantral follicles, 1 or 1.5% alginate proved best, as these concentrations were shown to support survival and growth.7,15,21,112
Alginate-Based Matrices
Despite positive results obtained with alginate hydrogels, the biological inertness of alginate has largely hampered its use in applications where cell adhesion is essential for survival and proliferation.53 However, extracellular matrix (ECM) molecules can be combined with calcium alginate to construct synthetic ECM matrices for 3D culture without affecting their biocompatibility or stability,59–62,90,91,125,127,130,137 as detailed below.
For instance, calcium alginate containing the arginine-glycine-aspartic acid (RGD) adhesion peptide sequence showed a positive effect on hormone secretion: increasing RGD concentrations improved progesterone and estradiol secretion.62 Moreover, RGD peptide and collagen I showed to improve follicle development of secondary follicles and oocyte maturation and meiosis resumption can be promoted when fibronectin, laminin or RGD are added to the alginate matrix.60
Alginate can also be combined with fibrin, offering a dynamic mechanical environment, since both polymers contribute to initial matrix rigidity. However, fibrin is rapidly degraded by proteases secreted by growing follicles and matrix support is done exclusively by alginate. Shikanov et al. obtained 82% of meiotically competent oocytes after 12 days of culture of isolated secondary murine follicles encapsulated in a fibrin–alginate matrix, which was a significantly higher percentage than in alginate alone.90,91 Similarly, Jin et al.59 found fibrin–alginate hydrogels to be superior to alginate in terms of murine follicle growth and differentiation, yielding a larger proportion of oocytes competent for fertilization and a greater number of two-cell embryos than alginate alone.
Isolated follicles from goats19 and dogs96 were also encapsulated in a fibrin–alginate scaffold. Brito et al.19 reported that oocytes could only mature when groups of isolated secondary follicles were in vitro cultured in this matrix, proving that goat follicles can benefit from a component that facilitates cell adhesion. Fibrin was also shown to improve growth of canine secondary follicles.96 The authors hypothesized that this may be thanks to fibrin’s ability to degrade, allowing better follicle expansion than with alginate alone.
Xu et al.130 also reported that an alginate–fibrin matrix increases growth of primary follicles from macaques and in vitro production of estradiol, AMH and VEGF. A fibrin–alginate scaffold containing growth factor-reduced Matrigel, which has lower concentrations of several growth factors28 that participate in follicle development,36 also appears to be suitable for in vitro culture of baboon follicles.127
These studies show that in vitro culture of isolated preantral follicles in 3D systems can be improved and controlled through the design of ECM structural and biochemical properties. More recently, a fibrin–alginate interpenetrating network was used to evaluate toxic effects on murine ovarian follicles via a high-throughput approach, showing that fibrin degradation rate can be correlated to follicle health status: it significantly decreases or stops when follicle is damaged. The changes in proteolytic activity from the proteases secreted by functioning GCs can be measured by the optical fibrin clearance surrounding the follicle.137 Like this, Zhou et al.137 found that follicles exposed to increasing doses of doxorubicin showed decreasing survival rates, coupled with attenuated fibrin degradation.
Biological scaffolds made of ECM constituents produced by decellularization of mammalian tissues have been widely studied in recent years. Indeed, although they do not retain the 3D ultrastructure of native tissue, they still maintain in vitro and in vivo biological activity.16,25,116 Moreover, ECM hydrogels may supply signaling molecules and growth factors.93,117 Based on encouraging results obtained with alginate and its biological inertness, Chiti et al.22 hypothesized that decellularized bovine ovarian ECM (boECM) hydrogel could be mixed with alginate to provide cell anchorage patterns. A protocol was therefore developed to produce such a decellularized boECM hydrogel and the resulting matrix was used to in vitro culture encapsulated isolated murine follicles for 7 days.22 The findings showed that while boECM hydrogel alone did not promote follicular growth, it did allow follicular survival. However, when 75% of boECM was combined with 25% of 1% SLM alginate, follicle survival and growth were both observed after 7 days of in vitro culture.22
A very interesting concept for an alginate-based hydrogel for in vitro culture of isolated follicles was proposed by He’s team,2,23 whereby a matrix was prepared with a hard shell (made of alginate) and a soft core (made of collagen), mimicking the ovarian cortex and medulla respectively (Fig. 5). Encapsulation of isolated secondary follicles from deer mice in the hydrogel promoted follicle growth up to the antral stage, as well as ovulation,23 demonstrating that these microtissues can recapitulate the 3D mechanical, physiological, and anatomical ovarian environment.23

Reprinted with permission from Choi et al.,23 ©Elsevier (2016).
Matrix with a hard shell (made of alginate) and a soft core (made of collagen), mimicking the ovarian cortex and medulla, respectively (day 0). Encapsulation of isolated secondary follicles from deer mice in the hydrogels, promoting follicular growth up to the antral stage (day 9).
Using a 3D Alginate Culture System as a Tool for In Vitro Analysis
The ultimate goal of an alginate system is to promote follicle development in order to obtain healthy oocytes that can be further matured and fertilized to produce embryos for fertility restoration in cancer patients, improve conservation of wild animal species or autochthonous animal breeds, or multiply the potential of genetically superior domestic animals. Although positive results have been obtained using this matrix to in vitro culture isolated preantral follicles from various animal species, numerous studies have indicated that such outcomes can be significantly improved by optimizing different culture parameters, such as media, co-culture conditions, oxygen tension, and so on. Apart from its main application, this 3D system can also be used as an important tool to investigate follicle biology and evaluate the effect of isolation and cryopreservation protocols on the survival and development of preantral follicles.
Analysis of In Vitro Culture Conditions
Medium Supplementation
FSH has a vital role to play in folliculogenesis, as it stimulates development of antral follicles and ovulation. Because of this, it has been extensively applied in assisted reproduction techniques.114 Its addition to culture medium has been tested in alginate-encapsulated follicles from different animal species, always yielding positive results. Studies in rodents showed small two-layered murine secondary follicles to be responsive to FSH, demonstrating a positive correlation between FSH dose, follicle growth and steroid secretion,61 while larger multilayered secondary follicles are FSH-dependent, with follicle survival, growth, steroid secretion, metabolism and oocyte maturation all regulated by FSH. Interestingly, when FSH doses were superior to 25 mIU/mL, follicle survival decreased in the latter follicle class.61 An enriched culture medium supplemented not only with FSH, but also fetuin, insulin, transferrin and selenium, was found to improve growth of murine primary and early secondary follicles, allowing antrum formation.99 FSH was also shown to have a positive impact on the growth of rat secondary follicles48 and, together with insulin, promoted viability and development, as well as estradiol production, in bovine follicles.77
Songsasen et al.97 and Nagashima et al.69 reported that FSH supplementation improved development of canine follicles too. Similar results were obtained with cat follicles, which grew faster in the presence of FSH.95
In non-human primates, FSH was found to positively influence survival and development of rhesus secondary follicles.127 Conversely, FSH appeared to have a negative impact on baboon follicles encapsulated in a fibrin–alginate–Matrigel matrix, which exhibited disruption of oocyte integrity and cumulus cell connections. Follicles grown without FSH were able to produce MII-stage oocytes with a normal spindle structure.131
Luteinizing hormone (LH) is also an essential constituent during folliculogenesis, as it provides androgen substrate for estrogen synthesis, which in turn contributes to oocyte maturation.37 It was therefore also tested for in vitro culture of alginate-encapsulated follicles from dogs and monkeys. Whether or not associated with FSH, LH was shown to promote development of canine follicles.69 On the other hand, FSH alone appeared to be more effective for development of secondary follicles in rhesus monkeys compared to combined FSH–LH supplementation.134
The influence of vitamins on in vitro culture of alginate-encapsulated follicles was also corroborated by two different studies. In order to improve survival and development of mouse primary follicles, Tagler et al.100 supplemented the medium with ascorbic acid, which has been associated with ECM remodeling. The authors reported that follicle structural integrity and survival were significantly enhanced by addition of ascorbic acid and follicles were able to grow up to the antral stage.100 Xu et al.128 recently investigated the effect of low and high concentrations of vitamin D3 on rhesus secondary follicles encapsulated in alginate beads. They reported that while both doses resulted in antral follicles with a significantly greater oocyte diameter than controls, low vitamin D concentrations improved follicle survival and AMH production, and high doses yielded larger numbers of fast-growing follicles.128
Insulin and androgens have also been found to play a positive role in the survival and growth of rhesus secondary follicles, enhancing steroid production and oocyte quality.76,126 Similarly, basic fibroblast growth factor was reported to improve survival and development of human preantral follicles.119
Co-culture Systems
Since ovarian cells support folliculogenesis through secretion of key factors required for follicle development, Tingen et al.108 decided to evaluate in vitro co-culture of mouse primary and small secondary follicles encapsulated in alginate beads and investigate these cells further. They found that the ovarian stromal cell feeder layer did indeed have a positive impact on follicles, significantly increasing their survival and growth, but isolation of these cells resulted in a heterogeneous population that eventually changed over the course of culture. Tagler et al.99 therefore replaced ovarian cells with mouse embryonic fibroblasts (MEFs), hypothesizing that these cells could provide essential paracrine factors for follicle survival and development. After two weeks, follicles co-cultured with MEF showed higher survival rates than controls. Moreover, they maintained an intact structure, while follicles without MEFs showed extruded oocytes.101
Culture Environment
Apart from maintenance of their 3D structure and medium supplementation with hormones, growth factors and antioxidants, other important requirements for in vitro survival and growth of isolated follicles concern the culture environment, including aspects like oxygen tension. Although optimal oxygen concentrations have not yet been established for ovarian follicles, studies have indicated that oxygen has a significant impact on folliculogenesis and that oxygen consumption by oocytes varies during follicular development.41,44
Makanji et al.67 reported that alginate-encapsulated mouse secondary follicles showed a significant increase in survival and growth rates when in vitro cultured in lower oxygen concentrations (2.5%). They believe that such findings were due to hypoxia-mediated pyruvate production for oxidative energy metabolism, and suggest that oxygen tension levels should be lower (2–5%) during the preantral stage. In the antral phase, oxygen concentrations should increase to 15–20%, then fall again during the gonadotropin peak and ovulation.67 Xu et al.127 also found lower oxygen concentrations (5%) to deliver higher growth rates in rhesus monkey secondary follicles than did higher concentrations (20%). Using 20% oxygen, Yin et al.136 in vitro cultured alginate-encapsulated preantral follicles isolated from human ovarian medulla. While secondary follicles grew, primordial and primary follicles exhibited poor survival and did not develop to the antral stage. These results corroborate the theory of Makanji et al.,67 who speculated that higher hypoxia-mediated glycolysis may be necessary for preantral follicles.
Analysis of Isolation or Cryopreservation Procedures
To assess follicle survival and morphology, histological, immunohistochemical and ultrastructural analysis soon after isolation or thawing/warming is an important tool to calculate success rates of isolation and cryopreservation protocols. However, it is not enough to simply ascertain if a follicle will survive and resume its normal development. For in-depth ultrastructure evaluation, it is necessary to incubate follicles, allowing time for them to reveal changes in their compartments and organelles that may have been caused by isolation or cryopreservation procedures. In vitro culture therefore represents a valuable means of investigating these techniques, and 3D alginate systems have been largely applied to this end.
Aiming to develop an isolation procedure for human preantral follicles that could be used in a clinical setting, Vanacker et al.110 showed that follicles were able to successfully survive and grow after isolation with Liberase DH blendzyme and 7 days of in vitro culture. Yin et al.136 recently optimized an isolation protocol for preantral follicles enclosed in ovarian medullary tissue. To assess their survival and development, these authors used the alginate system for in vitro culture and found that while secondary follicles could survive and grow, most primordial and primary follicles died. Dong et al.31 compared two different protocols (mechanical and mechano-enzymatic) to isolate human preantral follicles. They reported that growth rates and estradiol levels were higher in mechanically isolated follicles than in follicles subjected to a combination of mechanical and enzymatic isolation.
Development of an optimal cryopreservation procedure has been the goal of numerous studies, as it is a crucial aspect of fertility restoration and preservation of genetic material. In mice, Asgari et al.12 used an alginate culture system to compare slow freezing and vitrification protocols. Their results suggest that vitrification is superior for cryopreservation of mouse ovaries, as follicles exhibited better antrum formation than follicles from frozen-thawed ovarian tissue. On the other hand, Sadeghnia et al.84 reported that viability and growth of follicles isolated from vitrified-warmed sheep ovarian tissue were significantly inferior to fresh follicles.
Zelinski’s group conducted a number of studies to assess the impact of cryopreservation on the survival and development of preantral follicles from rhesus monkeys. In their first paper, they compared slow-freezing and vitrification, demonstrating that after isolation and in vitro culture in alginate beads, follicles from vitrified-warmed tissue had greater capacity to form an antrum than follicles from frozen-thawed tissue.106 Looking to optimize their vitrification protocol, they conducted further investigations, showing that shorter periods of incubation of ovarian tissue in a vitrification solution containing synthetic polymers resulted in follicle survival rates similar to controls.107 Finally, the team assessed the ability of ovarian tissue to be successfully vitrified in a closed system.105 They found that although their protocol preserved tissue and follicle morphology, it had a negative effect on follicle development in vitro and antrum formation rates.105
In vitro culture in a 3D alginate system by our team showed that isolation of human preantral follicles before or after cryopreservation had a similar impact on follicle survival and growth.112 Interestingly, some authors were able to successfully cryopreserve isolated follicles embedded in alginate beads.15,21,112,118 According to Ji et al.,57 hydrogel encapsulation offers the best protection for isolated cells with low cryotolerance. Although primordial follicles have been showed to be cryoresistant,89 alginate encapsulation was still beneficial, as it maintained their 3D structure, thus preserving connections between GCs and the oocyte during freezing and thawing procedures.21 Moreover, it may decrease exposure to cryoprotectant and prevent damage due to ice formation,57,87 protecting follicles during cryopreservation. Indeed, once polymerized, the alginate barrier organizes the extracellular fluid, limiting deleterious ice crystal formation during cooling and warming.14 These studies show that alginate encapsulation is not only a precious tool for in vitro culture of isolated follicles, but also for their cryopreservation.
Alginate for In Vitro Culture of Follicles from Different Animal Species
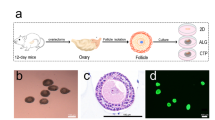
As previously mentioned, alginate matrices have been successfully used to in vitro culture isolated follicles from a number of animal species. Figure 6 summarizes studies from the literature on alginate-encapsulated follicles from rodents, ruminants, carnivores, and primates.
Isolated follicles from rodent species have been shown to develop in 2D systems, but they have also been found to survive and grow in alginate scaffolds. Pangas et al.71 were the first to apply this system to in vitro culture of isolated follicles from 12-day-old mice. Follicles were embedded in alginate beads, and morphological and ultrastructural studies suggested that alginate does not interfere with oocyte or GC development, as there was no evidence of this over 10 days of in vitro culture.71 Mouse secondary follicles were also able to develop up to the antral stage,67,72 producing oocytes capable of reaching the MII stage after in vitro maturation,12,94,101,123 or even ovulating.94
The reason why high-quality cultured oocytes can be obtained from mice is probably thanks to maintenance of vital corridors of communication between the two cellular compartments of the alginate matrix. Indeed, using a similar model, Heise et al.48 demonstrated the presence of connections between GCs and oocytes in isolated rat preantral follicles cultured in alginate, which may have been due to preservation of their unique morphology supported by the alginate matrix.85 Moreover, Mainigi et al.66 reported that murine oocytes developing in vitro in an alginate-based culture system undergo normal transition to transcriptional quiescence, and the transcriptome of these oocytes is very similar (99.5%) to that of oocytes that develop in vivo. However, they also revealed that the developmental competence of these oocytes is compromised, as evidenced by the very low rate of fertilization following in vitro maturation and insemination, due to an increased incidence of abnormal spindle formation and chromosome alignment, as well as abnormal cortical granule biogenesis and failure to emit the first polar body. Nevertheless, Xu et al.129 obtained viable offspring after encapsulation and in vitro culture of isolated mouse follicles.
Caprine follicles exhibited a greater follicle diameter and better oocyte integrity when encapsulated in alginate beads compared to 2D in vitro culture.74 Silva et al.92 showed that 0.5% alginate allowed survival and development of isolated caprine preantral follicles for up to 12 days, producing MII oocytes. Follicles from other ruminant species have been also isolated and encapsulated in alginate beads for further in vitro culture. Araújo et al.11 demonstrated that isolated cow secondary follicles were able to grow up to the antral stage in 0.25% alginate, and their estradiol production increased when growth hormone was added to the culture medium.
Looking to improve conservation of wild canids, Songsasen’s group showed that alginate was capable of supporting in vitro growth of isolated preantral and antral follicles from dogs and cats. This team used 0.5% alginate and FSH to in vitro culture isolated cat preantral and antral follicles. Their results revealed that follicles maintained their 3D structure in alginate beads and their growth was significantly superior when the culture medium was supplemented with FSH.95
Non-human primate ovarian follicles have also been successfully cultured in calcium alginate beads. Apart from one study on baboon secondary follicles,127 all have essentially focused on rhesus monkey follicles at different stages of development.51,68,106,127,130 Other have used alginate-encapsulated follicles from non-human primates to test different cryopreservation protocols for ovarian tissue,105–107 in vitro culture medium supplements,76,125,127,131 or the effects of diet,132 proving that these animals can successfully serve as a model for humans. Oocytes retrieved from in vitro-grown primate follicles were also able to reinitiate meiosis for fertilization, and hence early embryonic cleavage.127
In vitro development of isolated human preantral follicles is an alternative to use cryopreserved ovarian tissue instead of transplantation. Human preantral follicles have indeed been effectively cultured in calcium alginate hydrogels by numerous teams (Fig. 6).7,21,63,112,118,119,124,136 Although Laronda et al.63 and Yin et al.136 reported that their isolated human primordial follicles died after a few days of in vitro culture, Amorim’s group showed that these follicles are not only able to survive in vitro, but actually grow (Fig. 7).7,21,112 Such a discrepancy in the results may have been due to the alginate concentration used to encapsulate the follicles, or the protocol applied for their isolation.
Alginate to Transplant Follicles
In recent years, the possibility of transplanting isolated preantral follicles inside an artificial ovary has been investigated6 with the aim of restoring endocrine activity and fertility in cancer patients. A key challenge for construction of such an artificial ovary is identifying an optimal matrix to support these grafted follicles. To this end, the growing field of tissue engineering, which exploits and combines cells, materials, and biological signals, could offer indispensable help. All engineered tissue has different requirements related to metabolism, growth factors, the ECM, and mechanical characteristics, and novel techniques have been developed to meet these needs.120 Nevertheless, creating the right microenvironment for an artificial ovary to support isolated ovarian follicle development in vivo is a task that presents unique challenges, while offering countless opportunities.120
To graft isolated follicles and ovarian cells, an artificial ovary must provide structural support for the cells and follicles until complete restructuration of the stromal ovarian tissue matrix. The main goal of the artificial ovary is to offer an environment that allows follicle survival and development, mimicking conditions encountered in a natural ovary. Furthermore, as human ovarian follicles are exceptional in that they can grow to around 600 times their size during folliculogenesis, the artificial ovary, unlike other artificial organs, should also be biodegradable. Because of these requirements and the favorable results obtained with in vitro culture of isolated follicles encapsulated in alginate, this polymer looks to be a promising candidate for the artificial ovary matrix.
Vanacker et al.113 conducted a first study conceived as a starting point for construction of a transplantable artificial ovary. They set out to develop a biodegradable artificial scaffold that offers an environment in which follicles and OCs are able to survive and grow. First, they autografted isolated mouse OCs encapsulated in a biodegradable matrix made of alginate and matrigel to a pocket created in the internal part of the mouse peritoneum. After one week of grafting, they demonstrated that an alginate-based matrix was able to degrade, allowed vascularization, and supported cell survival and proliferation. Moreover, it elicited a low inflammatory response.
Encouraged by these results, the authors performed a second study, this time to graft not only OCs, but also isolated preantral follicles. Based on tests showing that 1% SLM alginate completely degrades after 4 weeks of grafting (Vanacker et al., unpublished results), this material was selected to encapsulate the follicles and cells. In this new study, Vanacker et al.111 autografted isolated mouse preantral follicles and OCs enclosed in a 1% SLM alginate matrix to a peritoneal pocket. After one week, they reported a follicle recovery rate of 22%, with isolated follicles able to reach the antral stage. Moreover, grafted OCs survived and proliferated, and vessels were formed. As observed in the previous study,113 the inflammatory response was low. These findings indicate that an alginate-based artificial ovary may well be capable of restoring endocrine function and fertility in patients suffering from cancer that carries a high risk of ovarian involvement.
Conclusions and Future Perspectives
Since the first study on encapsulation of isolated ovarian follicles in alginate,71 a considerable amount of research has been conducted to test and optimize not only the matrix itself, but also different variables (culture media, stage of follicle development, cryopreservation protocols, etc.). In this review, we have summarized all studies performed in different animal species, underscoring our knowledge and understanding of use of such an artificial scaffold for ovarian follicles. These studies provide important insights into how alginate-based matrices help follicles to survive and grow in vitro and in vivo, and can thus make a great impact in the fields of reproductive medicine, biotechnology, and animal conservation.
However, although alginate appears to be a promising biomaterial for follicle encapsulation, it may be not sufficient by itself. Indeed, the biological inertness of alginate has largely hampered its use in applications where cell adhesion is essential for survival and proliferation,53 which is why it should be combined with other molecules. For instance, to induce cell interaction, bioactive peptide sequences known to bind to receptors on cell surfaces can be covalently linked to alginate39,78,79 without affecting its biocompatibility.60–62,90,91,125,137 These bioactive peptides mimic both the adhesive properties of ECM proteins containing these sequences and stimulation of cellular responses like differentiation and proliferation. A variety of such peptides have been identified and used in cell attachment studies, particularly the RGD tripeptide sequence because of its abundance in adhesion proteins (e.g. fibronectin, laminin, fibrinogen, vitronectin) and its ability to bind to a wide variety of integrins.83
Alginate modifications with bioactive peptides are traditionally achieved by carbodiimide chemistry and have been shown to yield around 0.1–1.0% mol of peptide per mol of uronate monomer.40,79,86 Although peptide densities in this concentration range are known to induce attachment of myoblasts,79,86 olfactory ensheathing cells,86 mesenchymal stem cells39 and endothelial cells,17 greater peptide densities influence the impact on cell attachment and differentiation.29,79 Increasing the degree of peptide substitution is relevant for use of peptide–alginate combined with non-substituted alginates to form bioactive hydrogels.9 Carbodiimide chemistry also contributes to the destruction of gelling properties without the addition of bioactive compounds.86
An alternative method has recently been described for high-efficiency coupling of bioactive peptides to alginates by means of periodate oxidation followed by reductive amination.26 Alginates with covalently attached fibronectin-derived Gly-Arg-Gly-Asp-Ser-Pro (GRGDSP) peptide were used to demonstrate the activity of the material and impact of high peptide densities on attachment of mouse skeletal myoblasts and human dental stem cells to peptide–alginate hydrogels.26 The authors showed that enhanced functionalization of alginate was crucial, as dental stem cells only adhered to alginate gels containing the highest concentrations of peptide, in contrast to myoblasts.26
Taken together, the most recent advances in alginate modifications have yielded promising results in different cell types. These studies should facilitate the development of next-generation alginate scaffolds specifically tailored for follicle encapsulation. Determining and engineering the structural and biochemical aspects of the alginate matrix for each stage of follicle development will therefore represent some of the future challenges and opportunities in this field.
Abbreviations
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- AMH:
-
Anti-Müllerian hormone
- ANGPT-1:
-
Angiopoietin-1
- ANGPT-2:
-
Angiopoietin-2
- boECM:
-
Bovine decellularized ovarian extracellular matrix
- ECM:
-
Extracellular matrix
- FSH:
-
Follicle-stimulating hormone
- GC:
-
Granulosa cell
- LH:
-
Luteinizing hormone
- MEF:
-
Mouse embryonic fibroblast
- RGD:
-
Arginine-glycine-aspartic acid
- VEGF:
-
Vascular endothelial growth factor
References
Abir, R., S. Franks, M. A. Mobberley, P. A. Moore, R. A. Margara, and R. M. Winston. Mechanical isolation and in vitro growth of preantral and small antral human follicles. Fertil. Steril. 68:682–688, 1997.
Agarwal, P., J. K. Choi, H. Huang, S. Zhao, J. Dumbleton, J. Li, and X. He. A biomimetic core-shell platform for miniaturized 3D cell and tissue engineering. Part. Part. Syst. Charact. 32:809–816, 2015.
Al-Shamkhani, A., and R. Duncan. Radioiodination of alginate via covalently-bound tyrosinamide allows monitoring of its fate in vivo. J. Bioact. Compat. Polym. 10:4–13, 1995.
Amorim, C. A. Artificial ovary. In: Gonadal Tissue Cryopreservation in Fertility, edited by N. Suzuki, and J. Donnez. New York: Springer, 2016, pp. 175–192.
Amorim, C. A., D. Rondina, C. M. Lucci, A. Giorgetti, J. R. de Figueiredo, and P. B. Goncalves. Cryopreservation of sheep primordial follicles. Reprod. Domest. Anim. 42:53–57, 2007.
Amorim, C. A., and A. Shikanov. The artificial ovary: current status and future perspectives. Future Oncol. 12:2323–2332, 2016.
Amorim, C. A., A. Van Langendonckt, A. David, M. M. Dolmans, and J. Donnez. Survival of human pre-antral follicles after cryopreservation of ovarian tissue, follicular isolation and in vitro culture in a calcium alginate matrix. Hum. Reprod. 24:92–99, 2009.
Andersen, T., P. Auk-Emblem, and M. Dornish. 3D cell culture in alginate hydrogels. Microarrays (Basel) 4:133–161, 2015.
Andersen, T., C. Markussen, M. Dornish, H. Heier-Baardson, J. E. Melvik, E. Alsberg, and B. E. Christensen. In situ gelation for cell immobilization and culture in alginate foam scaffolds. Tissue Eng. A 20:600–610, 2014.
Andreu, N., D. Thomas, L. Saraiva, N. Ward, K. Gustafsson, S. N. Jayasinghe, and B. D. Robertson. In vitro and in vivo interrogation of bio-sprayed cells. Small 8:2495–2500, 2012.
Araújo, V. R., M. O. Gastal, A. Wischral, J. R. Figueiredo, and E. R. Gastal. In vitro development of bovine secondary follicles in two- and three-dimensional culture systems using vascular endothelial growth factor, insulin-like growth factor-1, and growth hormone. Theriogenology 82:1246–1253, 2014.
Asgari, F., M. R. Valojerdi, B. Ebrahimi, and R. Fatehi. Three dimensional in vitro culture of preantral follicles following slow-freezing and vitrification of mouse ovarian tissue. Cryobiology 71:529–536, 2015.
Barrett, S. L., L. D. Shea, and T. K. Woodruff. Noninvasive index of cryorecovery and growth potential for human follicles in vitro. Biol. Reprod. 82:1180–1189, 2010.
Bhakta, G., K. H. Lee, R. Magalhães, F. Wen, S. S. Gouk, D. W. Hutmacher, and L. L. Kuleshova. Cryopreservation of alginate-fibrin beads involving bone marrow derived mesenchymal stromal cells by vitrification. Biomaterials 30:336–343, 2009.
Bian, J., T. Li, C. Ding, W. Xin, B. Zhu, and C. Zhou. Vitreous cryopreservation of human preantral follicles encapsulated in alginate beads with mini mesh cups. J. Reprod. Dev. 59:288–295, 2013.
Bible, E., F. Dell’Acqua, B. Solanky, A. Balducci, P. M. Crapo, S. F. Badylak, E. T. Ahrens, and M. Modo. Non-invasive imaging of transplanted human neural stem cells and ECM scaffold remodeling in the stroke-damaged rat brain by (19)F- and diffusion-MRI. Biomaterials 33:2858–2871, 2012.
Bidarra, S. J., C. C. Barrias, K. B. Fonseca, M. A. Barbosa, R. A. Soares, and P. L. Granja. Injectable in situ crosslinkable RGD-modified alginate matrix for endothelial cells delivery. Biomaterials 32:7897–7904, 2011.
Brito, I. R., C. M. Silva, A. B. Duarte, I. M. Lima, G. Q. Rodrigues, R. Rossetto, A. D. Sales, C. H. Lobo, M. P. Bernuci, A. C. Rosa-E-Silva, C. C. Campello, M. Xu, and J. R. Figueiredo. Alginate hydrogel matrix stiffness influences the in vitro development of caprine preantral follicles. Mol. Reprod. Dev. 81:636–645, 2014.
Brito, I. R., G. M. Silva, A. D. Sales, C. H. Lobo, G. Q. Rodrigues, R. F. Sousa, A. Moura, C. Calderón, M. Bertolini, C. C. Campello, J. Smitz, and J. R. Figueiredo. Fibrin-alginate hydrogel supports steroidogenesis, in vitro maturation of oocytes and parthenotes production from caprine preantral follicles cultured in group. Reprod. Domest. Anim. 51:997–1009, 2016.
Butcher, L., and S. L. Ullmann. Culture of preantral ovarian follicles in the grey, short-tailed opossum, Monodelphis domestica. Reprod. Fertil. Dev. 8:535–539, 1996.
Camboni, A., A. Van Langendonckt, J. Donnez, J. Vanacker, M. M. Dolmans, and C. A. Amorim. Alginate beads as a tool to handle, cryopreserve and culture isolated human primordial/primary follicles. Cryobiology 67:64–69, 2013.
Chiti, C., A. Viswanath, J. Vanacker, L. Germain, L. J. White, M. M. Dolmans, A. Des Rieux and C. A. Amorim. Hydrogel from bovine decellularized ovarian extracellular matrix supports mouse follicle survival in vitro. Front. Bioeng. Biotechnol. Conference Abstract: 10th World Biomaterials Congress. doi: 10.3389/conf.FBIOE.2016.01.00014.
Choi, J. K., P. Agarwal, H. Huang, S. Zhao, and X. He. The crucial role of mechanical heterogeneity in regulating follicle development and ovulation with engineered ovarian microtissue. Biomaterials 35:5122–5128, 2014.
Cortvrindt, R. G., and J. E. Smitz. Follicle culture in reproductive toxicology: a tool for in vitro testing of ovarian function? Hum. Reprod. Update 8:243–254, 2002.
Crapo, P. M., S. Tottey, P. F. Slivka, and S. F. Badylak. Effects of biologic scaffolds on human stem cells and implications for CNS tissue engineering. Tissue Eng. A 20:313–323, 2014.
Dalheim, M. Ø., J. Vanacker, M. A. Najmi, F. L. Aachmann, B. L. Strand, and B. E. Christensen. Efficient functionalization of alginate biomaterials. Biomaterials 80:146–156, 2016.
Desai, N., F. Abdelhafez, A. Calabro, and T. Falcone. Three dimensional culture of fresh and vitrified mouse pre-antral follicles in a hyaluronan-based hydrogel: a preliminary investigation of a novel biomaterial for in vitro follicle maturation. Reprod. Biol. Endocrinol. 10:29, 2012.
Desai, B. J., H. E. Gruber, and E. N. Hanley, Jr. The influence of Matrigel or growth factor reduced Matrigel on human intervertebral disc cell growth and proliferation. Histol. Histopathol. 14:359–368, 1999.
Dhoot, N. O., C. A. Tobias, I. Fischer, and M. A. Wheatley. Peptide-modified alginate surfaces as a growth permissive substrate for neurite outgrowth. J. Biomed. Mater. Res. A. 71:191–200, 2004.
Donati, I., Y. A. Mørch, B. L. Strand, G. Skjåk-Braek, and S. Paoletti. Effect of elongation of alternating sequences on swelling behavior and large deformation properties of natural alginate gels. J. Phys. Chem. B. 113:12916–12922, 2009.
Dong, F. L., L. Ma, S. L. Shi, S. J. Dai, X. G. Liu, Y. C. Su, Y. H. Guo, F. Wang, and Y. P. Sun. An research on the isolation methods of frozen-thawed human ovarian preantral follicles. Int. J. Clin. Exp. Med. 7:2298–2303, 2014.
Donnez, J., and M. M. Dolmans. Fertility preservation in women. Nat. Rev. Endocrinol. 9:735–749, 2013.
Draget, K. I., G. Skjåk Bræk, and O. Smidsrød. Alginic acid gels: the effect of alginate chemical composition and molecular weight. Carbohydr. Polym. 25:31–38, 1994.
Drury, J. L., and D. J. Mooney. Hydrogels for tissue engineering: scaffold design variables and applications. Biomaterials 24:4337–4351, 2003.
Eppig, J. J., and M. J. O’Brien. Development in vitro of mouse oocytes from primordial follicles. Biol. Reprod. 54:197–207, 1996.
Evron, A., Z. Blumenfeld, and E. Y. Adashi. The role of growth factors in ovarian function and development. Glob. Libr. Women’s Med., (ISSN: 1756-2228) 2015; DOI 10.3843/GLOWM.10288.
Filicori, M. The role of luteinizing hormone in folliculogenesis and ovulation induction. Fertil. Steril. 71:405–414, 1999.
Fisher, T. E., T. A. Molskness, A. Villeda, M. B. Zelinski, R. L. Stouffer, and J. Xu. Vascular endothelial growth factor and angiopoietin production by primate follicles during culture is a function of growth rate, gonadotrophin exposure and oxygen milieu. Hum. Reprod. 28:3263–3270, 2013.
Fonseca, K. B., S. J. Bidarra, M. J. Oliveira, P. L. Granja, and C. C. Barrias. Molecularly designed alginate hydrogels susceptible to local proteolysis as three-dimensional cellular microenvironments. Acta Biomater. 7:1674–1682, 2011.
Formo, K., C. H. Cho, L. Vallier, and B. L. Strand. Culture of hESC-derived pancreatic progenitors in alginate-based scaffolds. J. Biomed. Mater. Res. A 103:3717–3726, 2015.
Gigli, I., D. D. Byrd, and J. E. Fortune. Effects of oxygen tension and supplements to the culture medium on activation and development of bovine follicles in vitro. Theriogenology 66:344–353, 2006.
Gupta, P. S. P., H. S. Ramesh, B. M. Manjunatha, S. Nandi, and J. P. Ravindra. Production of buffalo embryos using oocytes from in vitro grown preantral follicles. Zygote 16:57–63, 2008.
Gutierrez, C. G., J. H. Ralph, E. E. Telfer, I. Wilmut, and R. Webb. Growth and antrum formation of bovine preantral follicles in long-term culture in vitro. Biol. Reprod. 62:1322–1328, 2000.
Harris, S. E., H. J. Leese, R. G. Gosden, and H. M. Picton. Pyruvate and oxygen consumption throughout the growth and development of murine oocytes. Mol. Reprod. Dev. 76:231–238, 2009.
Haug, A., and B. Larsen. Quantitative determination of the uronic acid composition of alginates. Acta Chem. Scand. 16:1908–1918, 1962.
Haug, A., B. Larsen, and O. Smidsrod. Studies of the sequence of uronic acid residues in alginic acid. Acta Chem. Scand. 21:691–704, 1967.
Haug, A., and O. Smidsrod. Strontium-calcium selectivity of alginates. Nature 215:757, 1967.
Heise, M., R. Koepsel, A. J. Russell, and E. A. McGee. Calcium alginate microencapsulation of ovarian follicles impacts FSH delivery and follicle morphology. Reprod. Biol. Endocrinol. 3:47, 2005.
Hemamalini, N. C., B. S. Rao, G. Tamilmani, D. Amarnath, R. Vagdevi, K. S. Naidu, K. K. Reddy, and V. H. Rao. Influence of transforming growth factor-α, insulin-like growth factor-II, epidermal growth factor or follicle stimulating hormone on in vitro development of preantral follicles in sheep. Small Rumin. Res. 50:11–22, 2003.
Hirao, Y., T. Nagai, M. Kubo, T. Miyano, M. Miyake, and S. Kato. In vitro growth and maturation of pig oocytes. J. Reprod. Fertil. 100:333–339, 1994.
Hornick, J. E., F. E. Duncan, L. D. Shea, and T. K. Woodruff. Isolated primate primordial follicles require a rigid physical environment to survive and grow in vitro. Hum. Reprod. 27:1801–1810, 2012.
Hornick, J. E., F. E. Duncan, L. D. Shea, and T. K. Woodruff. Multiple follicle culture supports primary follicle growth through paracrine-acting signals. Reproduction 145:19–32, 2013.
Irving-Rodgers, H. F., and R. J. Rodgers. Extracellular matrix of the developing ovarian follicle. Semin. Reprod. Med. 24:195–203, 2006.
Itoh, T., M. Kacchi, H. Abe, Y. Sendai, and H. Hoshi. Growth, antrum formation, and estradiol production of bovine preantral follicles cultured in a serum-free medium. Biol. Reprod. 67:1099–1105, 2002.
Jayasinghe, S. N. Cell electrospinning: a novel tool for functionalising fibres, scaffolds and membranes with living cells and other advanced materials for regenerative biology and medicine. Analyst 138:2215–2223, 2013.
Jewgenow, K. Impact of peptide growth factors on the culture of preantral follicles of domestic cats. Theriogenology 45:889–895, 1998.
Ji, L., J. J. de Pablo, and S. P. Palecek. Cryopreservation of adherent human embryonic stem cells. Biotechnol. Bioeng. 88:299–312, 2004.
Jiao, Z. X., and T. K. Woodruff. Follicle microenvironment-associated alterations in gene expression in the mouse oocyte and its polar body. Fertil. Steril. 99:1453–1459, 2013.
Jin, S. Y., L. Lei, A. Shikanov, L. D. Shea, and T. K. Woodruff. A novel two-step strategy for in vitro culture of early-stage ovarian follicles in the mouse. Fertil. Steril. 93:2633–2639, 2010.
Kreeger, P. K., J. W. Deck, T. K. Woodruff, and L. D. Shea. The in vitro regulation of ovarian follicle development using alginate-extracellular matrix gels. Biomaterials 27:714–723, 2006.
Kreeger, P. K., N. N. Fernandes, T. K. Woodruff, and L. D. Shea. Regulation of mouse follicle development by follicle-stimulating hormone in a three-dimensional in vitro culture system is dependent on follicle stage and dose. Biol. Reprod. 73:942–950, 2005.
Kreeger, P. K., T. K. Woodruff, and L. D. Shea. Murine granulosa cell morphology and function are regulated by a synthetic Arg-Gly-Asp matrix. Mol. Cell Endocrinol. 205:1–10, 2003.
Laronda, M. M., F. E. Duncan, J. E. Hornick, M. Xu, J. E. Pahnke, K. A. Whelan, L. D. Shea, and T. K. Woodruff. Alginate encapsulation supports the growth and differentiation of human primordial follicles within ovarian cortical tissue. J. Assist. Reprod. Genet. 31:1013–1028, 2014.
Lee, K. Y., and D. J. Mooney. Hydrogels for tissue engineering. Chem. Rev. 101:1869–1879, 2001.
Lenie, S., R. Cortvrindt, U. Eichenlaub-Ritter, and J. Smitz. Continuous exposure to bisphenol A during in vitro follicular development induces meiotic abnormalities. Mutat. Res. 651:71–81, 2008.
Mainigi, M. A., T. Ord, and R. M. Schultz. Meiotic and developmental competence in mice are compromised following follicle development in vitro using an alginate-based culture system. Biol. Reprod. 85:269–276, 2011.
Makanji, Y., D. Tagler, J. Pahnke, L. D. Shea, and T. K. Woodruff. Hypoxia-mediated carbohydrate metabolism and transport promote early-stage murine follicle growth and survival. Am. J. Physiol. Endocrinol. Metab. 306:893–903, 2014.
Merz, C., S. Saller, L. Kunz, J. Xu, R. R. Yeoman, A. Y. Ting, M. S. Lawson, R. L. Stouffer, J. D. Hennebold, F. Pau, G. A. Dissen, S. R. Ojeda, M. B. Zelinski, and A. Mayerhofer. Expression of the beta-2 adrenergic receptor (ADRB-2) in human and monkey ovarian follicles: a marker of growing follicles? J. Ovarian Res. 7:8, 2015.
Nagashima, J., D. E. Wildt, A. J. Travis, and N. Songsasen. Follicular size and stage and gonadotropin concentration affect alginate-encapsulated in vitro growth and survival of pre- and early antral dog follicles. Reprod. Fertil. Dev. 2015. doi:10.1071/RD15004.
Ouwerx, C., N. Velings, M. M. Mestdagh, and M. A. V. Axelos. Physico-chemical properties and rheology of alginate gel beads formed with various divalent cations. Polym. Gel Netw. 6:393–408, 1998.
Pangas, S. A., H. Saudye, L. D. Shea, and T. K. Woodruff. Novel approach for the three-dimensional culture of granulosa cell-oocyte complexes. Tissue Eng. 9:1013–1021, 2003.
Park, K. E., Y. Y. Kim, S. Y. Ku, S. M. Baek, Y. Huh, Y. J. Kim, S. H. Kim, Y. M. Choi, and S. Y. Moon. Effects of alginate hydrogels on in vitro maturation outcome of mouse preantral follicles. Tissue Eng. Regen. Med. 9:170–174, 2012.
Peretz, J., Z. R. Craig, and J. A. Flaws. Bisphenol A inhibits follicle growth and induces atresia in cultured mouse antral follicles independently of the genomic estrogenic pathway. Biol. Reprod. 87:63, 2012.
Pessoa, A. F. C., R. M. P. Rocha, I. R. Brito, G. M. Silva, R. N. Chaves, D. M. Magalhães-Padilha, C. C. Campello, A. P. R. Rodrigues, D. C. S. Nunes-Pinheiro, and J. R. Figueiredo. Effect of morphological integrity, period, and type of culture system on the in vitro development of isolated caprine preantral follicles. Theriogenology 82:312–317, 2014.
Picton, H. M., and R. G. Gosden. In vitro growth of human primordial follicles from frozen-banked ovarian tissue. Mol. Cell. Endocrinol. 166:27–35, 2000.
Rodrigues, J. K., P. A. Navarro, M. B. Zelinski, R. L. Stouffer, and J. Xu. Direct actions of androgens on the survival, growth and secretion of steroids and anti-Müllerian hormone by individual macaque follicles during three-dimensional culture. Hum. Reprod. 30:664–674, 2015.
Rossetto, R., M. V. A. Saraiva, M. P. Bernuci, G. M. Silva, I. R. Brito, A. M. C. V. Alves, D. M. Magalhães-Padilha, S. N. Báo, C. C. Campello, A. P. R. Rodrigues, and J. R. Figueiredo. Impact of insulin concentration and mode of FSH addition on the in vitro survival and development of isolated bovine preantral follicles. Theriogenology 86:1137–1145, 2016.
Rowley, J. A., G. Madlambayan, and D. J. Mooney. Alginate hydrogels as synthetic extracellular matrix materials. Biomaterials 20:45–53, 1999.
Rowley, J. A., and D. J. Mooney. Alginate type and RGD density control myoblast phenotype. J. Biomed. Mater. Res. 60:217–223, 2002.
Roy, S. K., and G. S. Greenwald. Methods of separation and in vitro culture of pre-antral follicles from mammalian ovaries. Hum. Reprod. Update 2:236–245, 1996.
Roy, S. K., and G. S. Greenwald. In vitro effects of follicle-stimulating hormone, luteinizing hormone and prolactine on follicular deoxyribonucleic acid synthesis in the hamster. Endocrinology 122:952–958, 1998.
Roy, S. K., and B. J. Treacy. Isolation and long-term culture of human preantral follicles. Fertil. Steril. 59:783–790, 1993.
Ruoslahti, E. RGD and other recognition sequences for integrins. Annu. Rev. Cell Dev. Biol. 12:697–715, 1996.
Sadeghnia, S., M. M. Akhondi, G. Hossein, S. Mobini, L. Hosseini, M. M. Naderi, S. B. Boroujeni, A. Sarvari, B. Behzadi, and A. Shirazi. Development of sheep primordial follicles encapsulated in alginate or in ovarian tissue in fresh and vitrified samples. Cryobiology 72:100–105, 2016.
Sadr, S. Z., B. Ebrahimi, M. Shahhoseini, R. Fatehi, and R. Favaedi. Mouse preantral follicle development in two-dimensional and three-dimensional culture systems after ovarian tissue vitrification. Eur. J. Obstet. Gynecol. Reprod. Biol. 194:206–211, 2015.
Sandvig, I., K. Karstensen, A. M. Rokstad, F. L. Aachmann, K. Formo, A. Sandvig, G. Skjåk-Bræk, and B. L. Strand. RGD-peptide modified alginate by a chemoenzymatic strategy for tissue engineering applications. J. Biomed. Mater. Res. A. 103:896–906, 2015.
Serra, M., C. Correia, R. Malpique, C. Brito, J. Jensen, P. Bjorquist, M. J. Carrondo, and P. M. Alves. Microencapsulation technology: a powerful tool for integrating expansion and cryopreservation of human embryonic stem cells. PLoS ONE 6:e23212, 2011.
Sharma, G. T., P. K. Dubey, and S. K. Meur. Survival and developmental competence of buffalo preantral follicles using three-dimensional collagen gel culture system. Anim. Reprod. Sci. 114:115–124, 2009.
Shaw, J. M., S. L. Cox, A. O. Trounson, and G. Jenkin. Evaluation of the long-term function of cryopreserved ovarian grafts in the mouse, implications for human applications. Mol. Cell. Endocrinol. 161:103–110, 2000.
Shikanov, A., M. Xu, T. K. Woodruff and L. D. Shea. A method for ovarian follicle encapsulation and culture in a proteolytically degradable 3 dimensional system. J. Vis. Exp. 49, 2011.
Shikanov, A., M. Xu, T. K. Woodruff, and L. D. Shea. Interpenetrating fibrin-alginate matrices for in vitro ovarian follicle development. Biomaterials 30:5476–5485, 2009.
Silva, G. M., R. Rossetto, R. N. Chaves, A. B. G. Duarte, V. R. Araújo, C. Feltrin, M. P. Bernuci, J. A. Anselmo-Franci, M. Xu, T. K. Woodruff, C. C. Campello, and J. R. Figueiredo. In vitro development of secondary follicles from pre-pubertal and adult goats cultured in two-dimensional or three-dimensional systems. Zygote 23:475–484, 2015.
Singelyn, J. M., P. Sundaramurthy, T. D. Johnson, P. J. Schup-Magoffin, D. P. Hu, D. M. Faulk, J. Wang, K. M. Mayle, K. Bartels, M. Salvatore, A. M. Kinsey, A. N. Demaria, N. Dib, and K. L. Christman. Catheter-deliverable hydrogel derived from decellularized ventricular extracellular matrix increases endogenous cardiomyocytes and preserves cardiac function post-myocardial infarction. J. Am. Coll. Cardiol. 59:751–763, 2012.
Skory, R. M., Y. Xu, L. D. Shea, and T. K. Woodruff. Engineering the ovarain cylce unsing in vitro follicle culture. Hum. Reprod. 30:1386–1395, 2015.
Songsasen, N., P. Comizzoli, J. Nagashima, M. Fujihara, and D. E. Wildt. The domestic dog and cat as models for understanding the regulation of ovarian follicle development in vitro. Reprod. Domest. Anim. 47:13–18, 2012.
Songsasen, N., C. Guzy, and D. E. Wildt. Alginate-fibrin gel matrix promotes in vitro growth of dog secondary follicles. Reprod. Fertil. Dev. 24:173, 2011.
Songsasen, N., T. K. Woodruff, and D. E. Wildt. In vitro growth and steroidogenesis of dog follicles as influenced by the physical and hormonal microenvironment. Reproduction 142:113–122, 2011.
Sun, J., and X. Li. Growth and antrum formation of bovine primary follicles in long-term culture in vitro. Reprod. Biol. 13:221–228, 2013.
Tagler, D., Y. Makanji, N. R. Anderson, T. K. Woodruff, and L. D. Shea. Supplemented αMEM/F12-based medium enables the survival and growth of primary ovarian follicles encapsulated in alginate hydrogels. Biotechnol. Bioeng. 110:3258–3268, 2012.
Tagler, D., Y. Makanji, T. Tu, B. P. Bernabé, R. Lee, J. Zhu, E. Kniazeva, J. E. Hornick, T. K. Woodruff, and L. D. Shea. Promoting extracellular matrix remodeling via ascorbic acid enhances the survival of primary ovarian follicles encapsulated in alginate hydrogels. Biotechnol. Bioeng. 111:1417–1429, 2014.
Tagler, D., T. Tu, R. M. Smith, N. R. Anderson, C. M. Tingen, T. K. Woodruff, and L. D. Shea. Embryonic fibroblasts enable the culture of primary ovarian follicles within alginate hydrogels. Tissue Eng. A 18:1229–1238, 2012.
Tambe, S. S., and T. D. Nandedkar. Steroidogenesis in sheep ovarian antral follicles in culture: time course study and supplementation with a precursor. Steroids 58:379–383, 1993.
Telfer, E. E., and M. B. Zelinski. Ovarian Follicle Culture: Advances and Challenges for Human and Non-human Primates. Fertil. Steril. 99:1523–1533, 2013.
Ting, A. Y., J. Xu, and R. L. Stouffer. Differential effects of estrogen and progesterone on development of primate secondary follicles in a steroid-depleted milieu in vitro. Hum. Reprod. 30:1907–1917, 2015.
Ting, A. Y., R. R. Yeoman, J. R. Campos, M. S. Lawson, S. F. Mullen, G. M. Fahy, and M. B. Zelinski. Morphological and functional preservation of pre-antral follicles after vitrification of macaque ovarian tissue in a closed system. Hum. Reprod. 28:1267–1279, 2013.
Ting, A. Y., R. R. Yeoman, M. S. Lawson, and M. B. Zelinski. In vitro development of secondary follicles from cryopreserved rhesus macaque ovarian tissue after slow-rate freeze or vitrification. Hum. Reprod. 26:2461–2472, 2011.
Ting, A. Y., R. R. Yeoman, M. S. Lawson, and M. B. Zelinski. Synthetic polymers improve vitrification outcomes of macaque ovarian tissue as assessed by histological integrity and the in vitro development of secondary follicles. Cryobiology 65:1–11, 2012.
Tingen, C. M., S. E. Kiesewetter, J. Jozefik, C. Thomas, D. Tagler, L. Shea, and T. K. Woodruff. A macrophage and theca cell-enriched stromal cell population influences growth and survival of immature murine follicles in vitro. Reproduction 141:809–820, 2011.
Townsend-Nicholson, A., and S. N. Jayasinghe. Cell electrospinning: a unique biotechnique for encapsulating living organisms for generating active biological microthreads/scaffolds. Biomacromolecules 7:3364–3369, 2006.
Vanacker, J., A. Camboni, C. Dath, A. Van Langendonckt, M. M. Dolmans, J. Donnez, and C. A. Amorim. Enzymatic isolation of human primordial and primary ovarian follicles with Liberase DH: protocol for application in a clinical setting. Fertil. Steril. 96:379–383, 2011.
Vanacker, J., M. M. Dolmans, V. Luyckx, J. Donnez, and C. A. Amorim. First transplantation of isolated murine follicles in alginate. Regen. Med. 9:609–619, 2014.
Vanacker, J., V. Luyckx, C. Amorim, M. M. Dolmans, A. Van Langendonckt, J. Donnez, and A. Camboni. Should we isolate human preantral follicles before or after cryopreservation of ovarian tissue? Fertil. Steril. 99:1363–1368, 2013.
Vanacker, J., V. Luyckx, M. M. Dolmans, A. Des Rieux, J. Jaeger, A. Van Langendonckt, J. Donnez, and C. A. Amorim. Transplantation of an alginate-matrigel matrix containing isolated ovarian cells: first step in developing a biodegradable scaffold to transplant isolated preantral follicles and ovarian cells. Biomaterials 33:6079–6085, 2012.
Vegetti, W., and F. Alagna. FSH and folliculogenesis: from physiology to ovarian stimulation. Reprod. Biomed. 12:684–694, 2006.
Vilela, J. M. V., E. C. R. Leonel, L. D’Oliveira, R. E. G. Paiva, A. L. Miranda-Vilela, C. A. Amorim, A. Pic-Taylor, and C. M. Lucci. Culture of domestic cat ovarian tissue in vitro and in the chick embryo chorioallantoic membrane. Theriogenology 86:1774–1781, 2016.
Viswanath, A., J. Vanacker, L. Germain, J. G. Leprince, A. Diogenes, K. M. Shakesheff, L. J. White and A. des Rieux. Extracellular matrix-derived hydrogels for dental stem cell delivery. J. Biomed. Mater. Res. A. 105: 319-328, 2017.
Wang, R. M., and K. L. Christman. Decellularized myocardial matrix hydrogels: In basic research and preclinical studies. Adv. Drug Deliv. Rev. 96:77–82, 2016.
Wang, T., J. Yan, C. Lu, X. Xia, T. Yin, X. Zhi, X. Zhu, T. Ding, W. Hu, H. Guo, R. Li, L. Yan, and J. Qiao. Human single follicle growth in vitro from cryopreserved ovarian tissue after slow freezing or vitrification. Hum. Reprod. 31:763–773, 2016.
Wang, T. R., L. Y. Yan, J. Yan, C. L. Lu, X. Xia, T. L. Yin, X. H. Zhu, J. M. Gao, T. Ding, W. H. Hu, H. Y. Guo, R. Li, and J. Qiao. Basic fibroblast growth factor promotes the development of human ovarian early follicles during growth in vitro. Hum. Reprod. 29:568–576, 2014.
West, E. R., L. D. Shea, and T. K. Woodruff. Engineering the follicle microenvironment. Semin. Reprod. Med. 25:287–299, 2007.
West, E. R., M. Xu, T. K. Woodruff, and L. D. Shea. Physical properties of alginate hydrogels and their effects on in vitro follicle development. Biomaterials 28:4439–4448, 2007.
West-Farrell, E. R., M. Xu, M. A. Gomberg, Y. H. Chow, T. K. Woodruff, and L. D. Shea. The mouse follicle microenvironment regulates antrum formation and steroid production: alterations in gene expression profiles. Biol. Reprod. 80:432–439, 2009.
Xiao, S., F. E. Duncan, L. Bai, C. T. Nguyen, L. D. Shea, and T. K. Woodruff. Size-specific follicle selection improves mouse oocyte reproductive outcomes. Reproduction 150:183–192, 2015.
Xu, M., A. Banc, T. K. Woodruff, and L. D. Shea. Secondary follicle growth and oocyte maturation by culture in alginate hydrogel following cryopreservation of the ovary or individual follicles. Biotechnol. Bioeng. 103:378–386, 2009.
Xu, M., S. L. Barrett, E. West-Farrell, L. A. Kondapalli, S. E. Kiesewetter, L. D. Shea, and T. K. Woodruff. In vitro grown human ovarian follicles from cancer patients support oocyte growth. Hum. Reprod. 24:2531–2540, 2009.
Xu, J., M. P. Bernuci, M. S. Lawson, R. R. Yeoman, T. E. Fisher, M. B. Zelinski, and R. L. Stouffer. Survival, growth, and maturation of secondary follicles from prepubertal, young, and older adult rhesus monkeys during encapsulated three-dimensional culture: effects of gonadotropins and insulin. Reproduction 140:685–697, 2010.
Xu, M., A. T. Fazleabas, A. Shikanov, E. Jackson, S. L. Barrett, J. Hirshfeld-Cytron, S. E. Kiesewetter, L. D. Shea, and T. K. Woodruff. In vitro oocyte maturation and preantral follicle culture from the luteal-phase baboon ovary produce mature oocytes. Biol. Reprod. 84:689–697, 2011.
Xu, J., J. D. Hennebold and D. B. Seifer. Direct vitamin D3 actions on rhesus macaque follicles in three-dimensional culture: assessment of follicle survival, growth, steroid, and antimüllerian hormone production. Fertil. Steril. 106:1815-1820.e1, 2016.
Xu, M., P. K. Kreeger, L. D. Shea, and T. K. Woodruff. Tissue-engineered follicles produce live, fertile offspring. Tissue Eng. 12:2739–2746, 2006.
Xu, J., M. S. Lawson, R. R. Yeoman, T. A. Molskness, A. Y. Ting, R. L. Stouffer, and M. B. Zelinski. Fibrin promotes development and function of macaque primary follicles during encapsulated three-dimensional culture. Hum. Reprod. 28:2187–2200, 2013.
Xu, J., M. S. Lawson, R. R. Yeoman, K. Y. Pau, S. L. Barrett, M. B. Zelinski, and R. L. Stouffer. Secondary follicle growth and oocyte maturation during encapsulated three-dimensional culture in rhesus monkeys: effects of gonadotrophins, oxygen and fetuin. Hum. Reprod. 26:1061–1072, 2011.
Xu, J., W. K. McGee, C. V. Bishop, B. S. Park, J. L. Cameron, M. B. Zelinski, and R. L. Stouffer. Exposure of female macaques to western-style diet with or without chronic T in vivo alters secondary follicle function during encapsulated 3-dimensional culture. Endocrinology 156:1133–1142, 2015.
Xu, M., E. West, L. S. Shea, and T. K. Woodruff. Identification of a stage-specific permissive in vitro culture environment for follicle growth and oocyte development. Biol. Reprod. 75:916–923, 2006.
Xu, M., E. R. West-Farrell, R. L. Stouffer, L. D. Shea, T. K. Woodruff, and M. B. Zelinski. Encapsulated three-dimensional culture supports development of nonhuman primate secondary follicles. Biol. Reprod. 81:587–594, 2009.
Yamamoto, K., T. Otoi, N. Koyama, N. Horikita, S. Tachikawa, and T. Miyano. Development to live young from bovine small oocytes after growth, maturation and fertilization in vitro. Theriogenology 52:81–89, 1999.
Yin, H., S. G. Kristensen, H. Jiang, A. Rasmussen, and C. Y. Andersen. Survival and growth of isolated pre-antral follicles from human ovarian medulla tissue during long-term 3D culture. Hum. Reprod. 31:1531–1539, 2016.
Zhou, H., M. A. Malik, A. Arab, M. T. Hill, and A. Shikanov. Hydrogel based 3-dimensional (3D) system for toxicity and high-throughput (HTP) analysis for cultured murine ovarian follicles. PLoS ONE 10:e0140205, 2015.
Acknowledgments
J. Vanacker is an FRS-FNRS postdoctoral researcher and C.A. Amorim is an FRS-FNRS research associate. The authors thank Mira Hryniuk, BA, for reviewing the English language of the manuscript.
Conflict of Interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Associate Editor Debra T. Auguste oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Vanacker, J., Amorim, C.A. Alginate: A Versatile Biomaterial to Encapsulate Isolated Ovarian Follicles. Ann Biomed Eng 45, 1633–1649 (2017). https://doi.org/10.1007/s10439-017-1816-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-017-1816-6