Abstract
The assessment of functional coronary lesion severity using intracoronary hemodynamic parameters like the pressure-derived fractional flow reserve and the flow-derived coronary flow reserve are known to rely critically on the establishment of maximal hyperemia. We evaluated a hyperemia-free index, basal pressure drop coefficient (bCDP), that combines pressure and velocity for simultaneous assessment of the status of both epicardial and microvascular circulations. In 23 pigs, simultaneous measurements of distal coronary arterial pressure and flow were performed using a dual-sensor tipped guidewire in the settings of both normal and abnormal microcirculation with the presence of epicardial lesions of area stenosis (AS) < 50% and AS > 50%. The bCDP, a parameter based on fundamental fluid dynamics principles, was calculated as the transtenotic pressure-drop divided by the dynamic pressure in the distal vessel, measured under baseline (without hyperemia) conditions. The group mean values of bCDP for normal (84 ± 18) and abnormal (124.5 ± 15.6) microcirculation were significantly different. Similarly, the mean values of bCDP from AS < 50% (72.5 ± 16.1) and AS > 50% (136 ± 17.2) were also significantly different (p < 0.05). The bCDP could significantly distinguish between lesions of AS < 50% to AS > 50% under normal microcirculation (52.1 vs. 85.8; p < 0.05) and abnormal microcirculation (84.9 vs. 172; p < 0.05). Further, the bCDP correlated linearly and significantly with the hyperemic parameters FFR (r = 0.42, p < 0.05) and CDP (r = 0.50, p < 0.05). The bCDP is a promising clinical diagnostic parameter that can independently assess the severity of epicardial stenosis and microvascular impairment. We believe that it has an immediate appeal for detection of coronary artery disease if validated clinically.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Assessment of functional coronary lesion severity, using sensor-equipped guidewires, has emerged as a standard diagnostic modality to provide objective evidence of myocardial ischemia during cardiac catheterization.20,36 Coronary diagnostic indices, fractional flow reserve (FFR; pressure derived), and coronary flow reserve (CFR; flow derived) showed a high agreement with non-invasive stress testing.10,11 The FFR is an established invasive clinical parameter used for assessing the physiological significance of epicardial disease. The FFR is defined as the ratio of pressures distal and proximal to a stenosis measured at maximal hyperemia. Based on extensive clinical trials, a cut-off value of 0.75–0.8 for FFR was shown to indicate the hemodynamic significance of coronary stenosis.28,29,32 Some limitations of FFR include the assumption of zero central venous pressure, and its dependence on achieving maximal hyperemia. Failure to achieve peak hyperemia may result in not achieving minimal constant microvascular resistance, leading to underestimation of pressure drop and overestimation of FFR across a stenosis.26 The CFR, defined as the ratio of flow at hyperemia to flow at rest, was found to have excellent agreement with noninvasive stress testing at a cut-off value of 2.0.11 An abnormal CFR (<2.0) corresponded to reversible myocardial perfusion defects with high sensitivity and specificity.11 It should be noted that CFR can provide the combined effect of epicardial stenosis and microvascular dysfunction, but cannot delineate between the two.
Because these indices, FFR and CFR, are based on either intracoronary pressure or flow, they do not differentiate between the hemodynamic status of the epicardial stenosis (normal microcirculation) and microvasculature (abnormal microcirculation).8,35 To overcome these issues, parameters based on simultaneous measurements of pressure drop and velocity were proposed. However, these parameters were defined for detection of either epicardial stenosis, namely, hyperemic stenosis resistance index (HSR; ratio of pressure drop across the stenosis to the distal velocity during hyperemia),21 or for detection of microvascular dysfunction, namely, hyperemic microvascular resistance index (HMR; ratio of mean distal pressure and velocity during hyperemia).31
Recently, for simultaneous detection of epicardial stenosis and microvascular dysfunction using a single diagnostic parameter, we introduced the functional index, the pressure drop coefficient CDP, the ratio of trans-stenotic pressure drop, Δp, to distal dynamic pressure, [½ × blood density × APV 2], where average peak flow velocity (APV) is measured under maximal hyperemia.33 The pressure drop coefficient (CDP), combining pressure and flow velocity information, was previously shown by our group to delineate between epicardial stenosis and microvascular dysfunction, in in vitro,23,33 and in vivo animal studies.1,14,15,23–25,33 Further, in a recent clinical trial16 CDP has been evaluated in a target patient population to distinguish between stenosis severities.
Achieving hyperemia8,26 is critical to the physiological assessment of functional lesion severity using the currently existing diagnostic parameters. Failure to achieve peak hyperemia can occur in situations where either the patient is unresponsive to adenosine, influenced by disease states (patients with microvascular dysfunction, e.g., diabetics, asthma, hypotension, and bradycardia) or has been on drugs or caffeine which inhibit the effect of adenosine.13,27,30,34 Thus, in an effort to further simplify physiologic testing and reduce the procedure cost and time involved with hyperemia, there has been an increasing trend lately in evaluating diagnostic parameters for detecting epicardial stenosis under basal conditions (without hyperemia). Three hyperemia-free physiologic indices of epicardial lesion severity have recently been introduced: basal fractional flow reserve (bFFR),12 basal stenosis resistance (bSR)34 and instantaneous wave-free ratio (iFR).30 However, similar to their hyperemic counterparts, the above parameters also cannot simultaneously assess the degree of epicardial stenosis and microvascular dysfunctions.
Thus, considering the previously documented utility of hyperemic CDP in pre-clinical1,14,15,23–25,33 and clinical16 trials, we hypothesized that the pressure drop coefficient determined during baseline (hyperemia-free) conditions (bCDP) can also simultaneously assess the degree of epicardial stenosis and microvascular dysfunctions. Consequently, we report herein in vivo data from animal experiments comparing the group mean values of bCDP under epicardial stenosis in the presence and absence of microvascular obstruction, and also compared them between the groups of AS < 50% and AS > 50%. We also report the correlations of bCDP with current hyperemic indices (FFR and CDP).
Methods
Animal Preparation
The preclinical study protocol was approved by the Institutional Animal Care and Use Committee at the University of Cincinnati and at Cincinnati Children’s Hospital Medical Center. The in vivo study was performed on 23 Yorkshire pigs (46 ± 3 kg), a group of 12 pigs with normal microcirculation and a group of 11 pigs with abnormal coronary microcirculation. The animals were fasted for 24 h before the procedure and were premedicated with intramuscular ketamine (20 mg/kg) or telazol (2–7 mg/kg), atropine (0.4 mg/kg), xylazine (2 mg/kg) and buprenorphine (0.005 mg/kg). General anesthesia was maintained with 2% of isoflurane and endotracheal oxygen supply as per the surgical procedural standards. Heart rate, oxygen saturation and end-tidal CO2 level were monitored every 15 min, and ventilator changes were made as needed to maintain these values in the normal range. The baseline characteristics of weight, heart rate, % oxygen saturation and end-tidal CO2 level are shown in Table 1. In a closed chest pig heart model, an arterial sheath was placed by surgical cut-down in the carotid artery followed by the insertion of a 6 French (Fr) guide catheter, which was advanced under fluoroscopic guidance to the left main coronary ostium. An intravenous dose of heparin (300 U/kg) was injected immediately. Angiographic images were used to select a segment of the left anterior descending (LAD) artery with no significant side branches.
Anatomical Measurements
After engaging the guide catheter at the coronary ostium, the native vessel lumen area was measured by motorized pullback (1 mm/s) of a 2 Fr In-Vision Gold intravascular ultrasound (IVUS) catheter (Volcano Corp., Rancho Cordova, California). Before IVUS measurements, a bolus dosage (0.1–1.0 µg/kg/min) of intracoronary nitroglycerin was injected to eliminate spasm that can be caused by insertion of the IVUS catheter. Based on the IVUS and angiographic images, a portion of the LAD was selected for creating epicardial flow obstruction which was induced by inflating a Voyager coronary angioplasty balloon (Guidant Corp., Indianapolis, Indiana), with the outer diameter determined from the inflation pressure table provided by the manufacturer. Sample balloons were tested for the variation of diameter with respect to recommended inflation pressure within an in vitro flow-loop system pressurized to the physiologic pressure. The influence of the physiologic pressure on the balloon diameter is expected to have negligible influence since inflation pressure within the balloon was maintained at a much higher pressure (at least 3 times the physiologic pressure). The balloon was mounted on the dual sensor-tipped guidewire used for pressure and flow measurements. The configuration of sensor-tipped guidewires and balloon placement is summarized in Fig. 1. The value of %AS for each in vivo trial was based on the measured value of vessel diameter by IVUS. An appropriate balloon size was then selected based on the vessel diameter and inflated to obtain %AS values in the range of both <50 and >50%.19,33 The range of %AS achieved in this study for AS < 50% was from 4 to 48% and for AS > 50% was from 50 to 88%.
Functional Measurements
In the first group of 12 pigs (normal microcirculation group with epicardial stenosis only), the phasic distal coronary pressure (p d) and APV were measured simultaneously with a dual sensor-tipped guidewire (Combowire, Volcano Therapeutics) as shown in Fig. 1. The mean proximal aortic pressure (p a) was continuously recorded at the tip of the guide catheter. The hemodynamic measurements were performed at both the baseline flow and at the maximal hyperemic flow (after injecting 10 mg intracoronary papaverine). Typically, we waited 30 s after Papaverine injection for three consecutive sets of similar hyperemic readings, for a specific stenotic condition. These measurements were recorded simultaneously using the ComboMap System (Volcano Corp.). The hemodynamic measurements of pressure and velocity were sampled every 5 ms, and peak systolic, diastolic and average pressures and velocities were calculated automatically by the workstation based on the time-period of a cardiac cycle. After the hyperemia measurement the balloon was deflated and the pig was rested for about 3–5 min (washout period) allowing the pressure and flow to return to normal. The data acquisition procedure described above was then repeated again after varying the balloon diameter to simulate various degrees of epicardial stenoses. The average number of inflations performed in each pig ranged from 5 to 7.
In the other group of 11 pigs (abnormal microcirculation [elevated microvascular resistance] group having concomitant epicardial stenosis), the diseased microcirculation was simulated by microvasculature disruption via an injection of ~12000 microspheres of 90 µm in diameter (Polysciences, Inc., Warrington, Pennsylvania). The severity of epicardial stenosis was again varied by inflating the balloon as discussed above. Distal pressure and flow (to obtain FFR, CFR, CDP and bCDP) were recorded both under basal and hyperemic conditions, as explained earlier for normal microvasculature. As reported in a previous study6 data with average proximal pressure (p a) values less than 48 mmHg were not included in the analysis.
The hemodynamic data under baseline conditions was acquired in both normal and abnormal microcirculation conditions. But in some scenarios the hyperemia was ambiguous following basal reading and for those basal data points the corresponding hyperemic data was not acquired. Owing to this the number of basal data points (N = 556) is more than the number of hyperemic data points (N = 329).
Calculation of Indices
The bCDP, developed from fundamental fluid dynamics principles,2,16 is defined as the ratio of trans-stenotic pressure drop and distal dynamic pressure (0.5 × ρ × APV 2) measured at baseline (without hyperemia) conditions where blood density ρ does not change significantly, as reported in several past studies,16 and thus can be assumed constant having a value of 1.05 g/cm3.
Comparison of the Equivalent Balloon Stenosis and Physiological Stenosis
The study of hemodynamics in an animal model simulating coronary stenosis has been limited due to the lack of a safe, accurate, and reliable technique for creating an artificial stenosis. Creating artificial stenosis using occluders in an open-chest procedure has often caused myocardial infarction (MI) or severe injury to the vessel resulting in high failure rates. To minimize these issues, closed-chest procedures with internal balloon obstruction as discussed above are often used to create an artificial stenosis. In a recent numerical study,17 using a Design of Experiments (DOE) based optimization approach, a relationship to predict the balloon obstruction equivalent to that of a physiological stenosis has been developed. The pressure drop in a balloon obstruction was evaluated and compared with that in a physiological stenosis. It was observed that the flow characteristics in balloon obstruction are more viscous dominated, whereas those in physiological stenosis were momentum dominated. Balloon radius was iteratively varied using a DOE based optimization method to obtain a pressure drop equal to that of a physiological stenosis at mean hyperemic flow rates. A linear relation was thus obtained to predict equivalent balloon obstruction for a physiological stenosis (Fig. 2). For a 15 mm balloon length, the equivalent balloon area stenoses of 31, 48 and 65% AS were observed to have pressure drops similar to those of physiological stenoses of 64, 80 and 90% AS, respectively. Thus, the mean %AS of balloon obstruction (50%) as noted in the results section is equivalent to ~80% physiological stenosis, which falls into clinically categorized intermediate area stenosis. It should be noted that the intermediate stenosis represents a clinically important scenario from the diagnostic viewpoint.34
Comparison of equivalent balloon stenosis and physiological stenosis17
Statistical Analysis
The main effect of both the disease condition (normal and abnormal microcirculation) and %AS (AS < 50% and AS > 50%) on the bCDP was assessed based on a two-way repeated-measure mixed-model ANOVA using SAS (v 9.0; Cary, NC). Pig was considered as the random factor, and a compound symmetry covariance structure was assumed between the repeated measures. The categorical (cell) means of various %AS levels under each of the diseased conditions was analyzed using one-way ANOVA. All functional measurements and hemodynamic parameters are represented as mean ± SE. The degree of agreement between the hemodynamic parameters, bCDP and CDP, was assessed using Bland–Altman plot (Medcalc version 10.2.0.0, Mariakerke, Belgium). A value of p < 0.05 was considered statistically significant.
Results
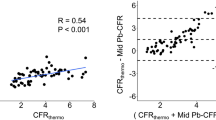
A total of 556 simultaneous pressure-flow readings were recorded in 23 pigs (106 readings with epicardial stenosis and 450 readings with concomitant epicardial and microvascular obstruction). The bCDP was calculated from the recorded pressure-flow data. The bCDP when correlated with FFR (Fig. 3) had an r-value of 0.42 (moderate correlation) but with p < 0.05 (statistically significant). The moderate correlation between bCDP and FFR can be due to the fact that FFR is only a pressure-based parameter, whereas bCDP is a combined measure of pressure and flow.
The statistical hemodynamic data for all the 23 pigs under baseline conditions is discussed below. The mean native LAD diameter was 3.01 ± 0.11 mm. The mean %AS of balloon obstruction was 50 ± 1% which is equivalent to ~80% physiological stenosis (Fig. 2). The mean value of proximal aortic pressure (p a), distal pressure (p d) and average peak flow velocity (APV) of blood were 66.4 ± 0.6, 53.7 ± 0.7 mmHg and 18.3 ± 0.3 cm/s, respectively.
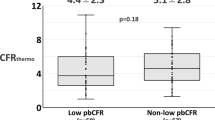
The main effect of the disease condition (normal and abnormal microcirculation) is shown in Fig. 4. Main effects are the differences in means over levels of one factor (for e.g., disease condition), collapsed over levels of the other factor (for e.g., %AS). The mean values of bCDP from normal (84 ± 18) and abnormal (124.5 ± 15.6) microcirculation were significantly different (p < 0.05), as shown in Fig. 4. Similarly, the main effects for mean values of bCDP from AS < 50% (72.5 ± 16.1) and AS > 50% (136 ± 17.2) were also significantly different (p < 0.05), as shown in Fig. 5. The conclusions were based on significance of p-values, even if there is some overlap in the error bars.4,22
Further, it should also be noted that the interaction between the two main effects in the two-way repeated measures mixed model ANOVA was not significant (p > 0.05). Thus, a one-way ANOVA was used to quantify the categorical means of various %AS levels under each of the diseased conditions. The bCDP significantly increased from lesions of AS < 50% to AS > 50% (52.1 vs. 85.8; p < 0.05) with normal microcirculation, as shown in Fig. 6. Similarly, bCDP value was also statistically significant in the abnormal microcirculation group for both AS < 50% and AS > 50% (84.9 vs. 172; p < 0.05) as shown in Fig. 7.
To study the effect of hyperemia on CDP, we correlated CDP measured under hyperemic conditions with bCDP measured without hyperemia (Fig. 8). It can be seen that there is a moderate correlation (r = 0.50) between CDP measured at hyperemia and baseline conditions (without hyperemia) with statistically significant p value (p < 0.05). The moderate correlation between bCDP and CDP is most likely caused by the wider range of bCDP and CDP values and the large sample size in this study that encompasses data from all possible disease conditions of normal to abnormal microcirculation and stenosis severities ranging from AS < 50% and AS > 50%.
Additionally, the agreement between the basal and hyperemic CDP was also assessed using a Bland–Altman analysis (Fig. 9). The mean differences between bCDP (measured without hyperemia) and the CDP (measured under hyperemia) was −86.1 ± 12.4 (95% limit of agreement = −110.5 to −61.7). The Bland–Altman analysis revealed neither trend nor bias between differences for the functional parameter, bCDP. Thus, indicating that bCDP is an independent parameter that can be used under clinical setting.
In the future, extending this analysis, we also plan to test the reproducibility and diagnostic accuracy of bCDP measured under basal conditions in a clinical trial.
Discussion
In this study, we sought to test the hyperemia-free diagnostic parameter, bCDP, in the presence of normal and elevated microvascular resistance (abnormal microcirculation). We hypothesized that the diagnostic parameter bCDP, calculated under basal conditions can distinguish between severity of area stenosis (AS) under normal and abnormal microcirculation. To test this hypothesis, we evaluated the main effects of mean values for bCDP under: (i) normal and abnormal microcirculation, and (ii) AS < 50% and AS > 50%. We also compared the sub-groups of AS < 50% and AS > 50% under both normal and abnormal microcirculation groups, respectively. Confirming our hypothesis, the mean values of the bCDP for normal and abnormal microcirculation changed significantly. The bCDP was also able to distinguish stenosis severities (AS < 50% and AS > 50%) under normal and abnormal microcirculation, respectively.
Current Hyperemic Diagnostic Indices
Conventional methods of stenosis evaluation in the cardiac catheterization laboratory involve the assessment of pressure-derived FFR and flow-derived CFR. As explained in the Introduction, FFR and CFR might fail to accurately assess the functional severity of epicardial stenosis in the presence of concomitant microvascular disease. Therefore, hyperemic CDP33 (ratio of pressure drop [Δp] to distal dynamic pressure, [½ × fluid density × velocity 2]) a parameter that combines pressure and flow, has been defined for the simultaneous detection of epicardial stenosis and concomitant microvascular dysfunction. The advantages of CDP over other parameters is that (a) it allows the use of a non-dimensional form of the pressure drop that is developed from fundamental fluid dynamic principles2; (b) it includes both the momentum change and viscous related pressure losses2; and (c) it has a higher resolving power for separating normal and diseased conditions of epicardial conditions and microvasculature simultaneously because of square of velocity term in denominator.1
In a previous animal study,1 the hyperemic CDP correlated significantly (r = 0.72, p < 0.05) when both the pressure-derived FFR and flow-based CFR are combined. More importantly hyperemic CDP was also shown to simultaneously assess and distinguish between epicardial stenosis and microvascular dysfunction.1 Recently, in a clinical study consisting of a group of 27 patients,16 hyperemic CDP was also found to have a significant linear correlation (r = 0.61, p < 0.05) when correlated simultaneously with FFR and CFR.
Interest in Hyperemia-Free Parameters
Hyperemic indices might not always lead to the best possible diagnosis. Failure to achieve peak hyperemia can occur in situations where either the patient is unresponsive to adenosine, influenced by disease states (patients with microvascular dysfunction, e.g., diabetic patients, asthma, hypotension and bradycardia) or has been on drugs or caffeine which inhibit the effect of adenosine. Furthermore, there is an ongoing debate on the dosage of vasodilator drugs and the site of administration, intracoronary vs. intravenous,3,5,7,9,18 for achieving maximal hyperemia. Consequently, current parameters like FFR,26 which are critically dependent upon the minimal microvascular resistance might be affected and could result in a possible mis-interpretation of stenosis severity. Due to this, there has been a recent interest in assessing the applicability of basal parameters for the detection of epicardial stenosis. Hyperemia-free indices like bFFR (bFFR; ratio of pressure’s distal and proximal to a stenosis during baseline conditions),12 which is the basal counterpart of the FFR measured at hyperemia, basal stenosis resistance (bSR; ratio of pressure drop across the stenosis to the distal velocity during baseline conditions),34 the basal counterpart of HSR, and instantaneous wave-free ratio (iFR; ratio of distal to proximal translesional pressure during a finite period in diastole [the wave-free period])30 have been introduced.
In a recent clinical study,12 the bFFR was shown to have a significant correlation with hyperemic FFR. However, it was also reported that the diagnostic accuracy of bFFR was not significant enough to justify its use over the hyperemic FFR. The other hyperemia-free novel index, iFR, is even easier than FFR to measure and is based on the assumption that mean resting myocardial resistance is equivalent to the mean hyperemic resistance over the complete cardiac cycle. The bSR has been shown to have similar diagnostic accuracy to FFR for identifying ischemia on myocardial perfusion imaging,34 but it has not been clinically adopted. These diagnostic parameters based on baseline hemodynamic measurements are not validated in extensive multi-center clinical trials unlike the clinically adopted hyperemic hemodynamic measurements (e.g., FFR). Currently, evidence on diagnostic accuracy of the basal hemodynamic parameters, including bSR, bFFR, iFR and bCDP, is encouraging, but limited. We believe that the basal parameters must be evaluated rigorously to determine their true diagnostic accuracy to be adopted clinically. Further, it should be noted that these parameters need to be tested for the delineation of epicardial disease and concomitant microvascular disease.
Basal CDP (bCDP)
Based on the above and considering the previous validation of hyperemic CDP, we proposed and tested the diagnostic ability of a basal CDP (bCDP). Similar to hyperemic CDP, bCDP was also found to distinguish between normal microcirculation (epicardial stenosis only) and abnormal microcirculation (concomitant epicardial stenosis). Analogously, bCDP could also distinguish between stenosis severities (AS < 50% and AS > 50%) under normal and abnormal microcirculation. It should also be noted that the correlation between bCDP and CDP in this animal study (r = 0.50, p < 0.05) and our recent clinical trial16 (r = 0.78, p < 0.05) were also similar. Similarly, the Bland–Altman analysis in the clinical and animal studies, between differences of bCDP and CDP, revealed neither trend nor bias for the bCDP. Thus, indicating that bCDP is an independent parameter that can be used under clinical setting.
Theoretically, the values of bCDP range from zero to infinity. The square of the flow in the denominator of bCDP magnifies its value and provides an increased resolving power for bCDP. This allows improved delineation of the status of epicardial vessel and microcirculation simultaneously. Further, it should be noted that, in the presence of microvascular dysfunction, pressure drop and blood flow are affected in the same direction. In such scenarios, as mentioned previously, diagnostic indices based on either pressure or flow alone can be affected significantly. The bCDP, however, being a diagnostic parameter based on both pressure and flow information, is expected to be unaffected and show a similar trend (Figs. 3 and 8). Further extensive human studies are needed to identify the cut-off values of bCDP to delineate between different combinations of epicardial and microvascular diseases.
Thus, we believe that bCDP incorporates all the advantages of the hyperemic CDP and in addition, can be measured under hyperemic-free conditions for the assessment of coronary artery disease. Further, due to the higher resolving power and combination of both the pressure and flow, bCDP might prove to be better parameter for clinical application in comparison to the existing hyperemia-free indices like bFFR,12 bSR34 and iFR.30
Limitations
Flow Measurements
The epicardial arterial obstruction was induced internally by inflating the angioplasty-balloon. Errors in flow measurement could occur if the downstream placement of the Doppler flow sensor relative to the angioplasty-balloon33 was inaccurate. While placing the sensor downstream to the balloon, arterial branches were avoided between the sensor and the balloon. At the same time, sufficient distance between the two was maintained in order to avoid downstream instabilities in flow measurement. Moreover, the position of the Doppler sensor was manipulated (to avoid noise) until an optimal and stable blood velocity signal was obtained distal to the lesion.
Balloon Obstruction
This study assumes a single blockage with a focal lesion in the LAD artery created by an angioplasty balloon. The degree of stenosis created by a balloon catheter is somewhat hemodynamically different from focal lesions found in humans. The balloon obstruction leads to a slightly increased pressure drop across the stenosis, due to additional flow resistance and viscous losses caused by the balloon shaft. However, the values of the diagnostic parameters obtained by internal balloon obstruction area expected to follow a similar trend when compared with an external stenotic resistance (as is the case for patients in the catheterization laboratory), if the resistances of the balloon shaft and internal balloon obstruction are combined. It should also be noted that the mean balloon obstruction in this study was at 50%, which effectively corresponds to ~80% of physiological stenosis (Fig. 2).
Collateral Flow
In humans, the effect of collateral flow might play an important role in the reperfusion of the vascular bed that is originally perfused by the stenosed artery. However, pig hearts are not known to have significant coronary collaterals. Hence, the effect of collateral flow could not be studied in this porcine model study.
Microvascular Disease Model
The method of disrupting microcirculation by injecting microspheres may represent only a certain variant of structural microvascular diseases. Though we injected the same size and amount of microspheres in the group of pigs with abnormal microcirculation, these microspheres might affect different arterioles and capillaries of the heart, creating variable levels of microcirculations and microvascular resistances.
Conclusion
The hyperemia-free index, bCDP, was able to significantly distinguish between normal and abnormal microcirculation. In addition, the bCDP was able to distinguish between stenosis severities (AS < 50% and AS > 50%) under normal and abnormal microcirculation, respectively. Further, bCDP correlated significantly with the current hyperemic parameters FFR and CDP. Therefore, we conclude that the hyperemia-free index, bCDP, if clinically validated, holds the potential for routine diagnostic applications in detecting coronary artery disease in the cardiac catheterization laboratory.
References
Banerjee, R. K., K. D. Ashtekar, M. A. Effat, T. A. Helmy, E. Kim, E. W. Schneeberger, R. A. Sinha, W. M. Gottliebson, and L. H. Back. Concurrent assessment of epicardial coronary artery stenosis and microvascular dysfunction using diagnostic endpoints derived from fundamental fluid dynamics principles. J. Invasive Cardiol. 21:511–517, 2009.
Banerjee, R. K., A. Sinha Roy, L. H. Back, M. R. Back, S. F. Khoury, and R. W. Millard. Characterizing momentum change and viscous loss of a hemodynamic endpoint in assessment of coronary lesions. J. Biomech. 40:652–662, 2007.
Cubero, J. M., L. S. D. de la Llera, P. C. García, M. V. Gil-Ortega, J. B. Mazuecos, and A. Sanchez-Gonzalez. A comparative study between intravenous and intracoronary administration of high doses adenosine for fractional flow reserve measurements, in the “fame” era. J. Am. Coll. Cardiol. 59:E1465–E1465, 2012.
Cumming, G., F. Fidler, and D. L. Vaux. Error bars in experimental biology. J. Cell Biol. 177:7–11, 2007.
De Bruyne, B., N. H. J. Pijls, E. Barbato, J. Bartunek, J.-W. Bech, W. Wijns, and G. R. Heyndrickx. Intracoronary and intravenous adenosine 5′-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation 107:1877–1883, 2003.
Fearon, W. F., L. B. Balsam, H. M. O. Farouque, R. C. Robbins, P. J. Fitzgerald, P. G. Yock, and A. C. Yeung. Novel index for invasively assessing the coronary microcirculation. Circulation 107:3129–3132, 2003.
Heusch, G. Adenosine and maximum coronary vasodilation in humans: myth and misconceptions in the assessment of coronary reserve. Basic Res. Cardiol. 105:1–5, 2010.
Hoffman, J. I. Problems of coronary flow reserve. Ann. Biomed. Eng. 28:884–896, 2000.
Jeremias, A., R. J. Whitbourn, S. D. Filardo, P. J. Fitzgerald, D. J. Cohen, E. M. Tuzcu, W. D. Anderson, A. A. Abizaid, G. S. Mintz, A. C. Yeung, et al. Adequacy of intracoronary vs. intravenous adenosine-induced maximal coronary hyperemia for fractional flow reserve measurements. Am. Heart J. 140:651–657, 2000.
Kern, M. J. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation 101:1344–1351, 2000.
Kern, M. J., A. Lerman, J. W. Bech, B. De Bruyne, E. Eeckhout, W. F. Fearon, S. T. Higano, M. J. Lim, M. Meuwissen, J. J. Piek, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation 114:1321–1341, 2006.
Kim, J. S., H. D. Lee, Y. K. Suh, J. H. Kim, K. J. Chun, Y. H. Park, J. Kim, D. C. Han, and C. B. Sohn. Prediction of fractional flow reserve without hyperemic induction based on resting baseline Pd/Pa. Korean Circ. J. 43:309–315, 2013.
Kleiman, N. S. Bringing it all together: integration of physiology with anatomy during cardiac catheterization. J. Am. Coll. Cardiol. 58:1219–1221, 2011.
Kolli, K. K., R. K. Banerjee, S. V. Peelukhana, M. A. Effat, M. A. Leesar, I. Arif, E. W. Schneeberger, P. Succop, W. M. Gottliebson, and T. A. Helmy. Effect of changes in contractility on pressure drop coefficient and fractional flow reserve in a porcine model. J Invasive Cardiol. 24:6–12, 2012.
Kolli, K. K., R. K. Banerjee, S. V. Peelukhana, T. A. Helmy, M. A. Leesar, I. Arif, E. W. Schneeberger, D. Hand, P. Succop, W. M. Gottliebson, and M. A. Effat. Influence of heart rate on fractional flow reserve, pressure drop coefficient, and lesion flow coefficient for epicardial coronary stenosis in a porcine model. Am. J. Physiol. Heart Circ. Physiol. 300:H382–H387, 2011.
Kolli, K. K., T. A. Helmy, S. V. Peelukhana, I. Arif, M. A. Leesar, L. H. Back, R. K. Banerjee, and M. A. Effat. Functional diagnosis of coronary stenoses using pressure drop coefficient: a pilot study in humans. Catheter. Cardiovasc. Interv. 83:377–385, 2014.
Kolli, K. K., A. K. Paul, L. H. Back, M. A. Effat, and R. K. Banerjee. Optimization of balloon obstruction for simulating equivalent pressure drop in physiological stenoses. Biorheology 50:257–268, 2013.
Leone, A. M., I. Porto, A. R. De Caterina, E. Basile, A. Aurelio, A. Gardi, D. Russo, D. Laezza, G. Niccoli, F. Burzotta, et al. Maximal hyperemia in the assessment of fractional flow reserve: intracoronary adenosine vs. intracoronary sodium nitroprusside vs. intravenous adenosine: The NASCI (Nitroprussiato vs. Adenosina nelle Stenosi Coronariche Intermedie) Study. JACC Cardiovasc. Interv. 5:402–408, 2012.
MacCarthy, P., A. Berger, G. Manoharan, J. Bartunek, E. Barbato, W. Wijns, G. R. Heyndrickx, N. H. Pijls, and B. De Bruyne. Pressure-derived measurement of coronary flow reserve. J. Am. Coll. Cardiol. 45:216–220, 2005.
Members, W. C., S. C. Smith, T. E. Feldman, J. W. Hirshfeld, A. K. Jacobs, M. J. Kern, S. B. King, D. A. Morrison, W. W. O’Neill, H. V. Schaff, et al. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention—Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). Circulation 113:156–175, 2006.
Meuwissen, M., M. Siebes, S. A. Chamuleau, B. L. van Eck-Smit, K. T. Koch, R. J. de Winter, J. G. Tijssen, J. A. Spaan, and J. J. Piek. Hyperemic stenosis resistance index for evaluation of functional coronary lesion severity. Circulation 106:441–446, 2002.
Payton, M. E., M. H. Greenstone, and N. Schenker. Overlapping confidence intervals or standard error intervals: what do they mean in terms of statistical significance? J. Insect Sci. 3:34, 2003.
Peelukhana, S. V., L. H. Back, and R. K. Banerjee. Influence of coronary collateral flow on coronary diagnostic parameters: an in vitro study. J. Biomech. 42:2753–2759, 2009.
Peelukhana, S. V., R. K. Banerjee, K. K. Kolli, M. A. Effat, T. A. Helmy, M. A. Leesar, E. W. Schneeberger, P. Succop, W. Gottliebson, and I. Arif. Effect of heart rate on hemodynamic endpoints under concomitant microvascular disease in a porcine model. Am. J. Physiol. Heart Circ. Physiol. 302:H1563–H1573, 2012.
Peelukhana, S. V., K. K. Kolli, M. A. Leesar, M. A. Effat, T. A. Helmy, I. Arif, E. W. Schneeberger, P. Succop, and R. K. Banerjee. Effect of myocardial contractility on hemodynamic end points under concomitant microvascular disease in a porcine model. Heart Vessels 29:97–109, 2014.
Pijls, N. H., M. J. Kern, P. G. Yock, and B. De Bruyne. Practice and potential pitfalls of coronary pressure measurement. Catheter. Cardiovasc. Interv. 49:1–16, 2000.
Pijls, N. H., and P. A. Tonino. The crux of maximum hyperemia: the last remaining barrier for routine use of fractional flow reserve. JACC Cardiovasc. Interv. 4:1093–1095, 2011.
Pijls, N. H., B. Van Gelder, P. Van der Voort, K. Peels, F. A. Bracke, H. J. Bonnier, and M. I. el Gamal. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 92:3183–3193, 1995.
Pijls, N. H., P. van Schaardenburgh, G. Manoharan, E. Boersma, J. W. Bech, M. van’t Veer, F. Bar, J. Hoorntje, J. Koolen, W. Wijns, and B. de Bruyne. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J. Am. Coll. Cardiol. 49:2105–2111, 2007.
Sen, S., J. Escaned, I. S. Malik, G. W. Mikhail, R. A. Foale, R. Mila, J. Tarkin, R. Petraco, C. Broyd, R. Jabbour, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) Study. J. Am. Coll. Cardiol. 59:1392–1402, 2012.
Siebes, M., B. J. Verhoeff, M. Meuwissen, R. J. de Winter, J. A. Spaan, and J. J. Piek. Single-wire pressure and flow velocity measurement to quantify coronary stenosis hemodynamics and effects of percutaneous interventions. Circulation 109:756–762, 2004.
Silber, S., P. Albertsson, F. F. Aviles, P. G. Camici, A. Colombo, C. Hamm, E. Jorgensen, J. Marco, J. E. Nordrehaug, W. Ruzyllo, et al. Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur. Heart J. 26:804–847, 2005.
Sinha Roy, A., M. R. Back, S. F. Khoury, E. W. Schneeberger, L. H. Back, V. V. Velury, R. W. Millard, and R. K. Banerjee. Functional and anatomical diagnosis of coronary artery stenoses. J. Surg. Res. 150:24–33, 2008.
van de Hoef, T. P., F. Nolte, P. Damman, R. Delewi, M. Bax, S. A. J. Chamuleau, M. Voskuil, M. Siebes, J. G. P. Tijssen, J. A. E. Spaan, et al. Diagnostic accuracy of combined intracoronary pressure and flow velocity information during baseline conditions: adenosine-free assessment of functional coronary lesion severity. Circ. Cardiovasc. Interv. 5:508–514, 2012.
van de Hoef, T. P., F. Nolte, M. C. Rolandi, J. J. Piek, J. P. van den Wijngaard, J. A. Spaan, and M. Siebes. Coronary pressure-flow relations as basis for the understanding of coronary physiology. J. Mol. Cell. Cardiol. 52:786–793, 2012.
Wijns, W., and P. H. Kolh. Experience with revascularization procedures does matter: low volume means worse outcome. Eur. Heart J. 31:1954–1957, 2010.
Acknowledgments
The authors are grateful to Dr. Mahesh Krishnamoorthy, Dr. Subhashish Das Gupta, Marwan Al-Rjoub and Bhaskar Konala of Transport in Engineering and Medicine Laboratory at University of Cincinnati for their assistance during the experiments. This study is supported by Grant-In-Aid of Great Rivers Affiliate, National-Scientific Development Grant of American Heart Association (Grant reference #s: 0755236B and 0335270N) and a Department of Veteran Affairs Merit Review Grant (I01CX000342).
Disclosure
The authors report no financial relationships or conflicts of interest regarding the content herein.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Dan Elson oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Kolli, K.K., Effat, M.A., Peelukhana, S.V. et al. Hyperemia-Free Delineation of Epicardial and Microvascular Impairments Using a Basal Index. Ann Biomed Eng 42, 1681–1690 (2014). https://doi.org/10.1007/s10439-014-1020-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-014-1020-x