Abstract
Despite substantial research in the past few decades, only slight progress has been made toward developing biocompatible, tissue-engineered scaffolds for heart valve leaflets that can withstand the dynamic pressure inside the heart. Recent progress on the development of hybrid scaffolds, which are composed of a thin metal mesh enclosed by multi-layered tissue, appear to be promising for heart valve engineering. This approach retains all the advantages of biological scaffolds while developing a strong extracellular matrix backbone to withstand dynamic loading. This study aims to test the inflammatory response of hybrid tissue-engineered leaflets based on characterizing the activation of macrophage cells cultured on the surfaces of the tissue construct. The results indicate that integration of biological layers around a metal mesh core—regardless of its type—may reduce the evoked inflammatory responses by THP-1 monocyte-like cells. This observation implies that masking a metal implant within a tissue construct prior to implantation can hide it from the immune system and may improve the implant’s biocompatibility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the early 1980s, scientists have been looking for ideal valve substitutes and engineered tissues to replace natural leaflets.7,23–25,27,34,38 However, despite substantial research in the past three decades, only slight progress has been made toward developing tissue-engineered scaffolds for heart valve leaflets. Most of the currently engineered tissue materials lack bioactive sites and are unable to coordinate the interaction between cells and scaffolds. As a result, superficial cells, particularly endothelial cells, cannot adhere firmly enough to the structure and are more easily lost to the blood flow. Therefore, the inflammatory cells and platelets aggregate and activate, which results in thrombosis and degradation.6,12 Additionally, engineered tissues that were previously developed and implanted in animals are either thicker, stiffer, and less pliable than native valves30,31 or exhibit size remodeling17 and partial degeneration with no interstitial tissue reconstitution.32 Other challenges involve an insufficiency or excess in composition and tenacity that makes the valve unable to withstand the pressure within the systematic circulation.37,14
We have recently developed a novel heart valve leaflet composed of a hybrid scaffold1 with a thin core of super elastic Nitinol mesh tightly enclosed within multi-layer biological tissue. This approach retains all the advantages of biological scaffolds while providing a strong extracellular matrix (ECM) backbone, which allows the valve to withstand the dynamic pressure loads inside the heart. Additionally, the high-resolution mesh pattern ensures the structural integrity of the surrounding tissue, which allows cells and ECM components on both sides of the mesh to actively interact with each other.
In the present study, we tested the inflammatory response of this leaflet in vitro by characterizing the activation of macrophage cells cultured on its surfaces, which was found to be well-correlated with post-implantation inflammation.20,22
Materials and Methods
Hybrid Leaflet Concept
We have developed tissue layers similar to a natural heart valve leaflet to create hybrid tissue-engineered leaflets, as previously described.1 The leaflet is composed of a thin metal mesh enclosed by layers of smooth muscle cells and fibroblast cells that are covered by an endothelial layer. We have currently used two types of metals, Nitinol and T316 Stainless Steel meshes, to test and compare the biocompatibility of the leaflet material.
The flat mesh of T316 Stainless Steel (Figs. 1a, 1c) is woven from 76 μm round wires, with a target size of 80 EPI × 80 PPIFootnote 1 (TWP Inc., Berkeley, CA). Nitinol meshes (Figs. 1b, 1d) were manufactured through acid etching of flat, superelastic, Nitinol sheets. The Nitinol meshes have a thickness of 76 μm etched with a network of holes of 240 μm diameter with a central distance of 320 μm. The base material was polished with a subsequent ultrasonic wash in ethanol and glow discharge for 40 s before autoclaving. Both meshes were cut into pieces with an area of 1 cm2 to be used for cell culture.
A cell pattern similar to a natural heart valve was selected to develop the hybrid leaflets. Three different cell types were isolated and used for the preliminary assay. Human aortic smooth muscle cells and human aortic adventitial fibroblast/myofibroblast cells were used to fulfill the role of valvular interstitial cells (VICs),10,11 and human umbilical vascular endothelial cells (all from Lonza Group, Allendale, NJ) were used to act as the valvular lining cells. The basal media for culturing cells contained DMEM (Dulbecco’s Modified Eagle Medium; Gibco, Carlsbad, CA), 10% fetal bovine serum (FBS, HyClone, Rockford, IL), 1% penicillin/streptomycin (Gibco, Carlsbad, CA) and 1% l-glutamine (Gibco, Carlsbad, CA), with appropriate growth factors added to the media for enhancement of growth and proliferation. The cultured cells were fed every 2–3 days, and split 1 to 3 at confluence. Cells were used at passages 3 to 5 for the experiment.
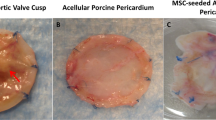
The tissue engineered constructs were cultured, as described in our previous publication.1 Briefly, a collagen gel mixture composed of bovine type I collagen was neutralized using proper amounts of NaOH. After combining the mixture with smooth muscle cells to form the first layer, collagen constructs were formulated by casting collagen solution in circular molds. The cells in the next layers were then plated around these collagen scaffolds at 1 week intervals to achieve a phenotype similar to a natural heart valve in vivo.1 Figures 2a and 2b show the engineered hybrid tissue after 3 months of cell culture for both the Stainless Steel and Nitinol mesh scaffolds, respectively.
Immunogenicity Assay
The immune responses of THP-1 cells (ATCC, Manassas, VA) to the leaflet constructs were tested in vitro. It has been shown that these cells, which are of human origin and well-characterized, mimic human monocyte behavior and are frequently used in biocompatibility assays.5,13,16,19,40,41 We cultured the THP-1 monocyte-like cells at 0.5–7 × 105 cells/mL in RPMI 1640 with 10% FBS, 50 μmol L−1 of β-mercaptoethanol (Gibco, Carlsbad, CA), 100 units mL−1 penicillin, 100 μg L−1 streptomycin and 2 mmol L−1 glutamine. These monocytes were seeded at a density of 150,000 cells/cm2 over the tissue samples and incubated at 37 °C overnight. THP-1 cells were added to the surface of the fully formed hybrid tissues, which were comprised of all three cell layers (i.e., smooth muscle, fibroblasts and endothelial cells). Additionally, THP-1 cells were added to the bare metal meshes (i.e., Stainless Steel and Nitinol) to test and compare the inflammatory responses evoked onto the isolated metal mesh. We also compared the biocompatibility of the fully formed hybrid leaflet with glutaraldehyde-treated bovine pericardial tissue, which is widely used in bioprosthetic heart valve leaflets. To do so, THP1 cells were added to the surface of the bovine pericardial leaflets (Neovasc, Inc, Richmond, BC, Canada).
The THP-1 cell line can be differentiated to macrophages by factors such as phorbol 12-myristate 13-acetate (PMA).36 PMA is not particularly relevant in an in vivo environment, therefore, it was only used to differentiate THP-1 monocytes into macrophage cells in vitro. Different conditions based on the presence or absence of PMA—as a positive control—were considered. The activation of THP-1 cells was determined using ELISA (Enzyme-Linked Immunosorbent Assay) for quantifying the secretion level of tumor necrosis factor-α (TNF-α) by immune cells, in response to the biomaterials. The experimental procedure is schematically shown in Fig. 3. Two constructs made of cells from different sources were considered for each condition, while the sample removal in ELISA was performed three times for each construct.
Schematic representation of the experimental procedure used for the biocompatibility assay. The experimental groups and the conditions considered for both immunogenicity assay and cell tracker probe are shown. There were two constructs for each condition, and the sample removal in ELISA was performed three times per construct
THP-1 cells were seeded for 24 h, and the cell culture supernatant was removed and analyzed by ELISA (R&D Systems, Minneapolis, MN), according to the manufacturer’s instructions. In some instances, as indicated, 50 ng/mL PMA (Sigma, St. Louis, MO) was added 1 h after the addition of THP-1 cells to enhance the differentiation of the cells into macrophage cells (Fig. 3).
Cell-Tracker Experiment
Activation and adhesion of the monocytes were visually verified using a cell-tracker dye experiment (Invitrogen, Carlsbad, CA) that stained the THP-1 cells before adding them to different experimental groups. These cell tracker reagents can be loaded into cells by adding the reagent to the culture media and then washing the cells briefly with fresh medium prior to analysis. THP-1 cells were harvested by centrifuging the supernatant with subsequent aspiration. The dye was added to the THP-1 cells with fresh, pre-warmed media that was incubated for 30 min at 37 °C. Finally, the dye-contained medium was replaced, and the cells were washed with PBS.
Scanning Electron Microscopy (SEM)
The ultra-structural features of cell adhesion and spreading were visualized at various magnifications ranging from 10 to 1000×, using a low-voltage, high-resolution SEM (Quanta 3D FEG Electron Microscope, FEI, Hillsboro, OR) at 10 kV. Hybrid tissue groups as well as bare metal groups were used for SEM analysis. To prime the constructs, the tissue samples were dehydrated in ascending concentrations of ethanol (30–100%), followed by critical-point drying in CO2. Then, all of the samples were mounted on carbon stubs, and sputtered using a 4 nm coating of gold (VCR Group, San Francisco, CA).
Statistical Analysis
Quantitative data from the immunogenicity assay were reported as mean ± SD. The R software package for Windows (Lucent Technologies Inc., Costa Mesa, CA) was used for statistical analysis. The unpaired Student’s t test was performed. A p value of less than 0.05 was considered statistically significant.
Results
After culturing the third layer (i.e., the endothelium) around the hybrid leaflets, the mesh was completely concealed by formation of a smooth, confluent surface that lined the construct. The collagen scaffold shrinkage stopped after the tissue was fully formed at the end of 8 weeks of producing sufficient ECM components. The endothelial layer seemed to be participating in the remodeling activities of the tissue and was strongly attached to the inner two layers.1
Four different conditions were considered: (1) the addition of THP-1 cells with PMA, (2) the addition of THP-1 cells without PMA, (3) groups without THP-1 cells or PMA to see whether the cells in the construct secrete any cytokines by themselves, and finally (4) groups without THP-1 cells but with PMA addition. The results of the ELISA for the levels of monocyte activation in all the experimental groups are shown in Fig. 4.
Secretion of human TNF-α was measured in different experimental groups using ELISA. The groups contained: hybrid tissue with Nitinol core, hybrid tissue with Stainless Steel core, Nitinol mesh alone, Stainless Steel mesh alone, fixed pericardial sheets and cell culture media as the control group. The tests were performed in four different conditions: (1) THP-1 cells were added to the groups without addition of PMA, (2) THP-1 cells were added to the groups along with addition of PMA at proper time step, (3) groups with no THP-1 cells addition but with PMA, and finally (4) a condition with no added THP-1 cells and no PMA
Groups Containing Nitinol Mesh
We found that the level of TNF-α secretion was significantly lower in the hybrid tissue constructs with a Nitinol core when compared to bare Nitinol mesh (p < 0.05; Table 1). Furthermore, it was observed that the addition of PMA significantly increases the inflammatory responses in both the bare Nitinol mesh (p < 0.05; Table 1) and the hybrid tissue construct with Nitinol core groups (p < 0.05; Table 1). No TNF-α secretion was found in the absence of THP-1 cells without PMA, while the response with PMA was negligible. This indicated that the source of TNF-α secretion was merely due to differentiated THP-1 cells and not due to the cells in the tissue portion. The results of the Cell Tracker probe showed adhesion of THP-1 cells on the metal/tissue surfaces. After the addition of PMA, the fluorescent images showed that the THP-1 cells attached to the Nitinol mesh with a higher rate of attachment (Figs. 5a, 5b). The amount of the cells that attached to the same area at the top of the mesh was almost 9 and 23 cells, without and with PMA, respectively, which demonstrated a nearly 2.5 fold increase in the rate of attachment (p < 0.05; data were extracted from 6 images per condition). The images of the same probe for the hybrid tissues with the Nitinol mesh core were taken under normal light microscopy (Figs. 6a, 6b). The average amount of attached cells was almost 13 and 7 cells, with and without PMA, respectively (p < 0.05). The thick tissue (~0.6 mm) around the mesh did not allow the fluorescent light to effectively penetrate through. Therefore, it was not possible to take clear fluorescent images for those groups. To address this issue and clearly image the surface of the tissue, SEM was performed for all the hybrid tissue constructs to test whether the THP-1 monocytes were firmly attached to the surface (Fig. 7). It can be observed in Figs. 7a and 7b that the THP-1 cells were attached and embedded onto the surfaces of the hybrid tissue leaflets.
Groups Containing Stainless Steel Mesh
Activation of the monocytes, denoted by secretion of TNF-α, was significantly lower in tissue constructs with a Stainless Steel mesh core, compared to the bare Stainless Steel mesh (p < 0.05; Table 1). A significantly higher response was observed in the presence of PMA in both groups (p < 0.05; Table 1). It was also found that the level of monocyte activation in the bare Stainless Steel mesh groups and hybrid tissue constructs with Stainless Steel groups was almost 2-fold and 1.3-fold higher, respectively, compared to the similar Nitinol groups. Without the addition of THP-1 cells the same (p ~ 0.24) response was observed with or without the addition of PMA. The fluorescent images of the Cell Tracker probe confirmed that the groups, in the presence of PMA, have more THP-1 cells attached to the Stainless Steel mesh (28 cells, Fig. 5d) compared to those without PMA (19 cells, Fig. 5c). These quantitative data confirmed that the rate of activation is higher for these groups compared to those with a Nitinol core because the microscope field-of-view and the surface area of the meshes are the same in both situations. The same results were achieved from the Cell Tracker probe experiment, as observed in Figs. 6c and 6d. Here, the average amount of attached cells was almost 21 and 9 cells, with and without PMA, respectively (p < 0.05).
Groups Containing Glutaraldehyde-treated Bovine Pericardial Tissue
The result of the ELISA for this group showed a comparable (p ~ 0.32) level of TNF-α secretion compared to the hybrid tissue constructs with a Nitinol core. However, this immunogenic response was found to be significantly lower compared to the other experimental groups (Table 1).
Discussion
The ideal heart valve substitute should be a tissue-engineered valve durable enough to remain functional in the heart during the lifetime of the patient. Evoking an immune response on the surface of the constructs may lead to immature degradation of the tissue engineered construct and ultimately immune rejection. Therefore, the leaflets should be biocompatible and non-thrombogenic, with a regenerative capacity to eventually become part of the body.23 This study aimed to assess the immunogenicity of an engineered heart valve leaflet we recently developed.1 To reduce the unfavorable effect of scaffold components on biocompatibility, we cultured hybrid tissues using biological matrix components (bovine type I collagen in this study). Due to the ability of collagen to accommodate cellular ingrowth without cytotoxic degradation products, they are considered biocompatible for in vivo applications.21 As a result, we expect that the combined use of bovine collagen and human cells do not have any adverse immunological effect on cell–cell or cell–ECM interaction/signaling.
Several factors such as surface roughness and porosity, chemical reactions at the surface, corrosion properties of the material, and the toxicity of the metal may affect biocompatibility of the implants.18 With regards to the immune reactions to bare metal meshes without surface modifications, we found that the THP-1 monocytes secrete less TNF-α in response to Nitinol vs. Stainless Steel (Figs. 4, 5). Our results also confirmed the superior biocompatibility of Nitinol compared to Stainless Steel, which is in good agreement with previous studies.26,35 Enclosing the Nitinol and Stainless Steel meshes within the tissue profoundly reduced the activation of macrophage cells that seeded over the surface of the tissue. This can be considered a major improvement in the biocompatibility of metal scaffolds, as the adhesive proteins of the collagen scaffold in the hybrid construct mask the mesh to the monocytes. The results not only indicate that the hybrid leaflets with a Nitinol core provoke less of an immune response, but also show that these constructs evoke a similar (p ~ 0.32) immunologic response to processed bovine pericardial tissue membranes, which are frequently used in bioprosthetic heart valves and are well-known for their superior biocompatibility15 (Fig. 4). The addition of PMA to all the experimental groups increased the level of TNF-α secretion. In the absence of THP-1 cells, we found a trace level of TNF-α only in the hybrid constructs with a Stainless Steel mesh core while the rest of the constructs did not secrete a significant amount of TNF-α. This confirms that the main source of TNF-α is due to the THP-1 cells rather than the cultured cells.
Attachment of the THP-1 cells to the meshes and surface of the hybrid tissues are shown in Figs. 5 and 6, respectively. This attachment is an indication of differentiation of these cells to macrophages since adhesion is a phenotypic characteristic of macrophage cells and not monocytes. These monocytes attached to the mesh and the surface of the tissue even without addition of PMA (Figs. 5a/5c and 6a/6c). SEM was used to assess whether the monocytes were embedded into the endothelial surface of the tissue constructs (Fig. 7). This phenomenon is equivalent to the migration and chemotaxis of the differentiated monocytes in vivo.
Our results indicate that integration of biological layers around a Nitinol mesh core minimizes the evoked inflammatory response. In other words, establishing this environment in vitro somehow masked the immunogenic reactions of the metal scaffolds while creating the hybrid tissue leaflet. Therefore, enclosing the thin metal mesh within a soft tissue shell not only results in a biocompatible surface but also does not interfere with the overall elasticity and durability of the mesh.1
Cell Masking Improves Biocompatibility of Metal Implants
Immediately upon embedding a metal implant inside the body, an inflammatory process is initiated that eventually encapsulates the implant with granulation tissue. The inflammatory reaction results in the migration of polymorphonuclear granulocytes and, soon after, monocytes to the site of implant. Monocytes differentiate into macrophages, which create a confining fibrous capsule around the implant.2 It is thought that the prolonged activation of macrophage cells near the implant site is critical to the long term response of implanted devices.3 Our results suggest that prior enclosing of a metal implant within tissue constructs effectively masks it from the immune system and may reduce the inflammatory response by converting the implants to biologically inactive or inert materials.
Based on the properties of the implanted material, the surrounding cells may form scar material or regenerate new natural tissue. Because the implanted metals would be covered by migratory local cells, the response of the neighboring tissues is the most important aspect of biocompatibility.39 When the implant is completely inert or biocompatible, the body provokes a normal healing process. By growing tissue around a metal mesh in vitro, we mimicked the ideal in vivo implantation situation by pre-formation of granulation tissue. This observation implies that masking metal implants within a tissue construct prior to implantation can effectively hide it from the immune system and improve the implant’s biocompatibility. We expect that prior growing of an autologous tissue construct around an implant guarantees masking the implant and minimizes the formation of additional adverse granulation tissue in vivo.
Whether or Not to Cross-link?
For in vivo implantation, the bovine collagen-based tissues may need to be cross-linked in some manner. The reason for cross-linking treatments is to tailor the mechanical and degradation properties of collagen implants since these biological scaffolds are mechanically fragile and degrade quickly. However, the cross-linking procedure is a potential cause of calcification and degeneration.28 Cross-linking does not stabilize valvular glycosaminoglycans (GAGs), which play important roles in regulating the mechanical behavior of the native cuspal tissue during dynamic motion of the leaflet.29 As a result, the current bioprosthetic heart valves are associated with immune reaction and progressive deterioration that limit their durability.4,33 Here, the hybrid scaffold concept retains the advantages of using biological scaffolds while maintaining a stronger ECM backbone. Moreover, we have shown that after culturing the third layer (i.e., endothelial layer), the tissue completely formed after 8 weeks such that no further degradation or shrinkage was observed; the cells and ECM components on both sides of the mesh interacted with each other.1 As a result, we expect that the hybrid scaffold can be used as an alternative to cross-linked tissues. These hybrid valve leaflets possess a smooth, confluent surface that comprises of endothelial cells. The biological portion of the scaffold does not demonstrate any shrinkage after the tissue matures and produces enough ECM components. This behavior decreases the risk of potential thrombosis after in vivo implantation.
Limitations
The source of the cell lines used in this study cannot exactly emulate the role of VICs.8,9 However, it would have been extremely difficult to extract and culture the patients’ valvular cells for in vivo applications. Therefore, we used vascular cells that are easily obtainable from the peripheral vasculature and can be used for future therapeutic applications.
We have not yet tested for potential thrombosis, which is an important factor to consider in developing any type of heart valve. It is anticipated that the hybrid tissue will also reduce the secretion of other pro-inflammatory cytokines. However, further studies are required to determine whether or not the hybrid tissue material will in fact induce macrophage cells to undergo polarization toward a pro-healing phenotype. In addition to the assessment of the inflammatory responses discussed here, the blood compatibility of the hybrid composites in this study should be tested in the future.
Notes
EPI: end per inch; PPI: pick per inch.
References
Alavi, S. H., and A. Kheradvar. Metal mesh scaffold for tissue engineering of membranes. Tissue Eng. Part C Methods 18:293–301, 2011.
Anderson, J. M. Inflammatory response to implants. ASAIO J. 34:101, 1988.
Anderson, J. M., A. Rodriguez, and D. T. Chang. Foreign body reaction to biomaterials. Semin. Immunol. 20:86–100, 2008.
Apte, S. S., A. Paul, S. Prakash, and D. Shum-Tim. Current developments in the tissue engineering of autologous heart valves: moving towards clinical use. Futur. Cardiol. 7:77–97, 2011.
Auwerx, J. The human leukemia cell line, THP-1: a multifacetted model for the study of monocyte-macrophage differentiation. Cell. Mol. Life Sci. 47:22–31, 1991.
Boontheekul, T., and D. J. Mooney. Protein-based signaling systems in tissue engineering. Curr. Opin. Biotechnol. 14:559–565, 2003.
Breuer, C. K., B. A. Mettler, T. Anthony, V. L. Sales, F. J. Schoen, and J. E. Mayer. Application of tissue-engineering principles toward the development of a semilunar heart valve substitute. Tissue Eng. 10:1725–1736, 2004.
Butcher, J. T., and R. M. Nerem. Porcine aortic valve interstitial cells in three-dimensional culture: comparison of phenotype with aortic smooth muscle cells. J. Heart Valve Dis. 13:478–486, 2004.
Butcher, J. T., A. M. Penrod, A. J. García, and R. M. Nerem. Unique morphology and focal adhesion development of valvular endothelial cells in static and fluid flow environments. Arterioscler. Thromb. Vasc. Biol. 24:1429–1434, 2004.
Chester, A. H., and P. M. Taylor. Molecular and functional characteristics of heart-valve interstitial cells. Philos. Trans. R. Soc. B: Biol. Sci. 362:1437–1443, 2007.
Filip, D., A. Radu, and M. Simionescu. Interstitial cells of the heart valves possess characteristics similar to smooth muscle cells. Circ. Res. 59:310–320, 1986.
Flanagan, T. C., and A. Pandit. Living artificial heart valve alternatives: a review. Eur. Cell Mater. 6:28–45, 2003.
Frankenberger, M., A. Pforte, T. Sternsdorf, B. Passlick, P. Baeuerle, and H. Ziegler-Heitbrock. Constitutive nuclear NF-kappa B in cells of the monocyte lineage. Biochem. J. 304:87, 1994.
Grande-Allen, K., and J. Liao. The heterogeneous biomechanics and mechanobiology of the mitral valve: implications for tissue engineering. Curr. Cardiol. Rep. 13:113–120.
Hammermeister, K. E., G. K. Sethi, W. G. Henderson, C. Oprian, T. Kim, and S. Rahimtoola. A comparison of outcomes in men 11 years after heart-valve replacement with a mechanical valve or bioprosthesis. N. Engl. J. Med. 328:1289–1296, 1993.
Heil, T., K. Volkmann, J. Wataha, and P. Lockwood. Human peripheral blood monocytes versus THP-1 monocytes for in vitro biocompatibility testing of dental material components. J. Oral Rehabil. 29:401–407, 2002.
Hoerstrup, S. P., R. Sodian, S. Daebritz, J. Wang, E. A. Bacha, D. P. Martin, A. M. Moran, K. J. Guleserian, J. S. Sperling, S. Kaushal, J. P. Vacanti, F. J. Schoen, and J. E. Mayer, Jr. Functional living trileaflet heart valves grown in vitro. Circulation 102(III):44–49, 2000.
Klinger, A., D. Steinberg, D. Kohavi, and M. Sela. Mechanism of adsorption of human albumin to titanium in vitro. J. Biomed. Mater. Res. 36:387–392, 1997.
Lee, S., F. Brennan, J. Jacobs, R. Urban, D. Ragasa, and T. Glant. Human monocyte/macrophage response to cobalt-chromium corrosion products and titanium particles in patients with total joint replacements. J. Orthop. Res. 15:40–49, 1997.
Liu, W. F., M. Ma, K. M. Bratlie, T. T. Dang, R. Langer, and D. G. Anderson. Real-time in vivo detection of biomaterial-induced reactive oxygen species. Biomaterials 32:1796–1801, 2011.
Lynn, A., I. Yannas, and W. Bonfield. Antigenicity and immunogenicity of collagen. J. Biomed. Mater. Res. B Appl. Biomater. 71:343–354, 2004.
Ma, M., W. F. Liu, P. S. Hill, K. M. Bratlie, D. J. Siegwart, J. Chin, M. Park, J. Guerreiro, and D. G. Anderson. Development of cationic polymer coatings to regulate foreign‐body responses. Adv. Mater. 2011.
Mendelson, K., and F. Schoen. Heart valve tissue engineering: concepts, approaches, progress, and challenges. Ann. Biomed. Eng. 34:1799–1819, 2006.
Rabkin, E., and F. J. Schoen. Cardiovascular tissue engineering. Cardiovasc. Pathol. 11:305–317, 2002.
Rabkin-Aikawa, E., J. E. Mayer, Jr., and F. J. Schoen. Heart valve regeneration. Adv. Biochem. Eng. Biotechnol. 94:141–179, 2005.
Ryhänen, J. Biocompatibility evaluation of nickel-titanium shape memory metal alloy. Oulun yliopisto, 1999.
Sacks, M. S., F. J. Schoen, and J. E. Mayer. Bioengineering challenges for heart valve tissue engineering. Annu. Rev. Biomed. Eng. 11:289–313, 2009.
Schoen, F. J., and R. J. Levy. Tissue heart valves: current challenges and future research perspectives. J. Biomed. Mater. Res. 47:439–465, 1999.
Shah, S. R., and N. R. Vyavahare. The effect of glycosaminoglycan stabilization on tissue buckling in bioprosthetic heart valves. Biomaterials 29:1645–1653, 2008.
Shinoka, T., C. K. Breuer, R. E. Tanel, G. Zund, T. Miura, P. X. Ma, R. Langer, J. P. Vacanti, and J. E. Mayer, Jr. Tissue engineering heart valves: valve leaflet replacement study in a lamb model. Ann. Thorac. Surg. 60:S513–S516, 1995.
Shinoka, T., P. X. Ma, D. Shum-Tim, C. K. Breuer, R. A. Cusick, G. Zund, R. Langer, J. P. Vacanti, and J. E. Mayer, Jr. Tissue-engineered heart valves. Autologous valve leaflet replacement study in a lamb model. Circulation 94:164–168, 1996.
Steinhoff, G., U. Stock, N. Karim, H. Mertsching, A. Timke, R. R. Meliss, K. Pethig, A. Haverich, and A. Bader. Tissue engineering of pulmonary heart valves on allogenic acellular matrix conduits: in vivo restoration of valve tissue. Circulation 102(III):50–55, 2000.
Stephens, E. H., N. de Jonge, M. P. McNeill, C. A. Durst, and K. J. Grande-Allen. Age-related changes in material behavior of porcine mitral and aortic valves and correlation to matrix composition. Tissue Eng. Part A 16:867–878, 2009.
Syedain, Z. H., and R. T. Tranquillo. Controlled cyclic stretch bioreactor for tissue-engineered heart valves. Biomaterials 30:4078–4084, 2009.
Thierry, B., M. Tabrizian, C. Trepanier, O. Savadogo, and L. H. Yahia. Effect of surface treatment and sterilization processes on the corrosion behavior of NiTi shape memory alloy. J. Biomed. Mater. Res. 51:685–693, 2000.
Tsuchiya, S., Y. Kobayashi, Y. Goto, H. Okumura, S. Nakae, T. Konno, and K. Tada. Induction of maturation in cultured human monocytic leukemia cells by a phorbol diester. Cancer Res. 42:1530, 1982.
van Geemen, D., P. Riem Vis, S. Soekhradj-Soechit, J. Sluijter, M. de Liefde-van Beest, J. Kluin, and C. Bouten. Decreased mechanical properties of heart valve tissue constructs cultured in platelet lysate as compared to fetal bovine serum. Tissue Eng. Part C Methods 7:607–617, 2011.
Vesely, I. Heart valve tissue engineering. Circ. Res. 97:743–755, 2005.
Vince, D. G., J. A. Hunt, and D. F. Williams. Quantitative assessment of the tissue response to implanted biomaterials. Biomaterials 12:731–736, 1991.
Wataha, J., P. Lockwood, M. Marek, and M. Ghazi. Ability of Ni-containing biomedical alloys to activate monocytes and endothelial cells in vitro. J. Biomed. Mater. Res. 45:251–257, 1999.
Wataha, J. C., S. Ratanasathien, C. T. Hanks, and Z. Sun. In vitro IL-1 [beta] and TNF-[alpha] release from THP-1 monocytes in response to metal ions. Dent. Mater. 12:322–327, 1996.
Acknowledgments
This work is partially supported by a Coulter Translational Research Award (CTRA) by the Wallace H. Coulter Foundation and a seed grant from the Edwards Lifesciences Center for Advanced Cardiovascular Technology at UC Irvine that was provided to Dr. Kheradvar.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Jane Grande-Allen oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Alavi, S.H., Liu, W.F. & Kheradvar, A. Inflammatory Response Assessment of a Hybrid Tissue-Engineered Heart Valve Leaflet. Ann Biomed Eng 41, 316–326 (2013). https://doi.org/10.1007/s10439-012-0664-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-012-0664-7