Abstract
Electrical potentials in mechanically loaded bone have been implicated as signals in the bone remodeling cycle. Recently, interest has grown in exploiting this phenomenon to develop electrically active ceramics for implantation in hard tissue which may induce improved biological responses. Both polarized hydroxyapatite (HA), whose surface charge is not dependent on loading, and piezoelectric ceramics, which produce electrical potentials under stress, have been studied in order to determine the possible benefits of using electrically active bioceramics as implant materials. The polarization of HA has a positive influence on interfacial responses to the ceramic. In vivo studies of polarized HA have shown polarized samples to induce improvements in bone ingrowth. The majority of piezoelectric ceramics proposed for implant use contain barium titanate (BaTiO3). In vivo and in vitro investigations have indicated that such ceramics are biocompatible and, under appropriate mechanical loading, induce improved bone formation around implants. The mechanism by which electrical activity influences biological responses is yet to be clearly defined, but is likely to result from preferential adsorption of proteins and ions onto the polarized surface. Further investigation is warranted into the use of electrically active ceramics as the indications are that they have benefits over existing implant materials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The piezoelectric effect is a property of certain materials whereby an electrical potential is produced by the application of a mechanical stress. It was first discovered a century ago and the piezoelectric properties of bone were confirmed in the 1950s.15 The electrical potentials which occur in bone under mechanical loading are explained in terms of both the piezoelectric properties of the collagen in bone15 and by the movement of ionic fluids within the structure.18 These potentials have been linked to the mechanical adaptation of bone in response to loading,18,36 leading to the suggestion that the addition of an electrically active component to an implant material may improve healing and adaptation of the surrounding tissue.
In the last two decades, there have been many developments in the broad field of Bioceramics.3 More recently, interest has grown in using electrically active ceramics to improve biological responses to artificial implants and grafts.12,27 The current review aims to bring together the results of studies on polarized and piezoelectric bioceramics in order to establish the state of the art with respect to their use for implantation in bone. As the focus of this Special Issue of the journal is interfacial aspects, this review will concentrate specifically on the electrical properties of bioceramics and the biological response to this group of materials as opposed to the much broader field of biomaterials. Therefore, it begins with a summary of polarization effects in HA and piezoelectric ceramics. The following section introduces relevant aspects of the piezoelectric effect, bone biology, and the origins of piezoelectricity in bone.
Electrical Properties of Materials
The Piezoelectric Effect
Jacques and Pierre Curie first reported piezoelectricity in 1880 when investigating the effect of charge generation through applied force in crystals of Rochelle salt (sodium potassium tartrate), quartz, and tourmaline. Hankel proposed the now accepted term for this phenomenon, derived from the Greek ‘piezen’ (to press) and electricity; hence, piezoelectricity is the generation of electricity through applied pressure. This is the ‘direct’ piezoelectric effect, where a compressive or tensile force produces a potential difference across the opposite faces of the crystal (Figs. 1a and 1b). The ‘converse’ effect is also observed (Figs. 1c and 1d), such that a crystal will become strained in response to an applied electric field.
Illustration of piezoelectric behavior. The direct effect: application of (a) compressive or (b) tensile force generates charge on the opposing faces and a potential difference. The converse effect: an applied electric field either (c) equal or (d) opposite of the material’s polarity, causes the material to strain
The phenomenon of piezoelectricity is best described by considering an ionically bonded crystalline solid and the distribution of ions within an individual unit cell. If the distribution of ions is asymmetric, an electrical dipole is generated. When the dipole is mechanically strained, the movement of the positive and negative ions with respect to one another produces a net polarization—the ‘direct’ effect in Figs. 1a and 1b. Conversely, the application of an electric field causes ionic movement, since alignment of the dipole with the field direction is preferable, producing a change in dimension of the dipole and a strain in the material at the macroscopic level—the ‘converse’ effect in Figs. 1c and 1d.
Bone Biology
In order to understand the way in which a host bone responds to implanted materials and its piezoelectric behavior, it is important to take into account its structure and composition, the principal cell types present in bone and the way in which bone remodels and repairs itself.
Bone can be considered as a composite material with several levels of structural organization each of which comprise two main components—an inorganic mineral component, hydroxyapatite (HA), combined with an organic matrix of collagen. The inorganic phase can be described as a non-stoichiometric, poorly crystallized, highly defective form of mineral apatite, Ca10(PO4)6OH2, which contains small quantities of cations and complex anion groups such as Ca2+, PO4 3−, CO3 2−, in addition to even smaller quantities of Mg2+, Fe2+, F−, Cl−, Na+ and K+. Biological apatites therefore differ from naturally occurring mineral apatite in terms of their composition and crystallinity and, as a consequence, their mechanical properties.
On the macroscale, there are two forms of bone structure—compact and cancellous. Compact bone is a dense, solid continuous mass in which the structural elements can only be seen with the aid of a microscope. It forms the outer shell of adult bones. Cancellous bone (also known as trabecular or spongy bone) is a three-dimensional network of bony trabeculae which combine to give an overall ‘spongy’ appearance. It typically makes up the inner section of the bone and has an excellent blood supply. The relative quantities of each type of bone and the architecture vary for each bone in a manner which reflects its overall shape, position, and functional role.
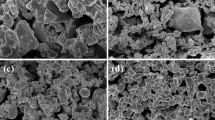
On the microstructural level, bone consists mainly of a number of irregular cylindrical units known as Haversian systems or osteons which run parallel to the long axis of the bone. A scanning electron micrograph of a polished transverse section is shown in Fig. 2. The diameter of the Haversian systems varies from 22 to 100 μm but each has a central canal which is surrounded by a series of concentric lamellae; these vary in number from 4 to 20. Within the lamellae are small pores or lacunae, approximately 10 μm in length connected to one another by small radiating channels, approximately 0.2 μm in diameter, known as canaliculi. The lacunae house the bone cells or osteocytes. Within each lamella, the collagen fibres have been shown to adopt a specific orientation but overall are oriented parallel to the long axis of the bone.49
Bone can be regarded therefore as a composite material on a number of levels. The main components are the mineral which accounts for in excess of 60% by weight, the organic collagen which accounts for over 20% by weight and liquids which make up the balance. Both the flexible collagen and the brittle mineral form continuous, highly orientated, networks throughout bone resulting in a unique combination of mechanical properties. The resultant composite material, in the form of cortical bone, has a modulus of elasticity in the order of 17–20 GPa, a tensile strength of 120–150 MPa, and compressive strength of 100–160 MPa. Bone can also have a strain to failure value of up to 4% depending on the rate of application of load. Developing a bone replacement material that can match this unusual combination of properties therefore presents an interesting challenge.
In adults, continuous bone remodeling is necessary to maintain biomechanically and metabolically functioning tissue; it begins with the replacement of primary bone during infancy and continues throughout life.22 This continuous remodeling allows bone to adapt its shape and architecture to form an efficient load-bearing structure.56 Remodeling consists of a cycle of bone resorption and formation and may be triggered by dynamic mechanical loading56 or by hormonal responses to changes in calcium or phosphorus levels.47 Wolff’s law states that mechanical stress is responsible for determining the architecture of bone and that bone tissue is able to adapt its mass and three-dimensional structure to the prevailing demands of stress-bearing.41,58 Various theories exist as to the details of this mechanism, though a complete explanation is yet to be developed.14,35 It has been suggested that piezoelectric and streaming electrical potentials in bone may act as signals in mechanotransduction.8
The four principal types of bone cells (osteoclasts, osteoblasts, osteocytes, and bone-lining cells) are key to the remodeling process and to the healing of injured bone.22 Osteoclasts resorb the inorganic phase of the bone. Osteoblasts are the cells responsible for forming bone matrix. Active osteoblasts lay down bone matrix on the surface of trabeculae or Haversian systems via the synthesis of osteoid, which contains type I collagen and non-collagenous proteins. Osteoid is subsequently mineralized to form the inorganic phase of the bone. In addition to laying down osteoid, osteoblasts are thought to be implicated in the regulation of osteoclast activity.22 While some osteoblasts die through apoptosis, the remainder become osteocytes or bone-lining cells. Osteoblasts become osteocytes when they are trapped in the bone matrix. The lacunae in which osteocytes are housed are pores in the lamellar structure of the Haversian system and are visible in Fig. 2. Osteocytes have a role in regulating the bone remodeling cycle in addition to a sensory role contributing to mechanotransduction. However, their exact role remains controversial, as it is not clear how osteocytes actually sense mechanical loading and transduce it into a cellular signal.51 Bone-lining cells cover bone surfaces which are not being remodeled. It has been suggested that these cells are responsible for activating the remodeling cycle, acting in response to biochemical signals from osteocytes.35 Osteoblasts have also been shown to be sensitive to mechanical strain.28
The remodeling of bone after trauma or fracture follows a different pattern. Immediately after the damage is incurred, a reactive healing phase is triggered during which a blood clot forms and fibroblast cells form granulation tissue. Macrophages (white blood cells which ingest debris and foreign organisms) clear the debris in the fracture site and over a period of weeks chondrocytes form cartilage between the fracture surfaces. Osteoblasts form bone which replaces this cartilaginous callous during the reparative phase. The bone is then remodeled to regain its pre-fracture structure. Macrophages also mediate immune and inflammatory responses in the body through the release of cytokines (signalling proteins). The response of macrophages to biomaterials is critical to their biocompatibility. They influence osteoblast and osteoclast differentiation around fractures and implanted materials and have been shown to make up 60–80% of the cell population in interfacial tissues between an implanted ceramic and the host bone.52 It is therefore important to understand the response of these cells to electrically active biomaterials.
Piezoelectricity in Bone
Fukada and Yasuda were the first to measure and propose a mechanism for piezoelectricity in bone.15 They suggested that the piezoelectric effect occurs when shearing forces cause collagen fibres in the bone to slip past each other. It has been discussed in the section “The piezoelectric effect” that piezoelectric materials generally have some form of asymmetry, leading to the generation of an electrical dipole that reacts to an applied mechanical stress or an electric field. For bone the electrical dipole is thought to form as a result of asymmetric collagen molecules. Collagen fibres are oriented parallel to the long axis of the bone which form helices within the lamellae forming the Haversian systems, oriented at various angles. The overall orientation of the collagen is therefore in the direction of the bone axis and results in piezoelectric properties and the development of charge in response to the application of a mechanical load.16
Due to the symmetry of the collagen fibres only two piezoelectric constants, d14 and d25 (equal but opposite to d14), represent the piezoelectric effect in bone. These piezoelectric constants are an indication of the charge generated per unit force relative to the polarization direction. The first subscript of the dij-constant provides the electrical direction (electric field or dielectric displacement) and the second subscript relates to the mechanical deformation or stress. Fukada and Yasuda reported the highest value of d14 to be 6 × 10−9 c.g.s.e.s.u. (0.2 pCN−1),15 although a later study found values as high as 14 × 10−9 c.g.s.e.s.u. (0.7 pCN−1).32 These are much smaller than piezoelectric coefficients of piezoelectric ceramics such as barium titanate (BaTiO3) or lead zirconate titanate (PZT) which can be up to 600 pCN−1.
In addition to the piezoelectric effect, streaming potentials can also result in electrical activity in bone, which will now be described. It is generally accepted that the electromechanical properties of wet and dry bone are different and cannot be explained by a single mechanism: both streaming potentials and piezoelectricity are thought to occur in live bone.18 The extracellular matrix (ECM) is negatively charged due to the presence of proteins. It is deformed in mechanical loading, inducing a flow of positively charged fluid and therefore developing streaming potentials.7,14 The site of this mechanism within the bone is under debate, although the interstitial fluids are thought to move within bone canaliculi8 which have a very small diameter in the order of 0.2 µm. Streaming potentials are thought to be part of the mechanosensory mechanisms in bone by which mechanical forces influence bone remodeling.7,31
Previous biomaterial development has sought to mimic bone chemistry and structure.3 Interest is growing in a new generation of biomaterials which seek to influence healing by mimicking the electrical effects in bone; namely the creation of a negative or a positive charge on the surface of the biomaterial. Two methods have been employed to create a surface charge, namely:
-
(i)
to polarize an ionic biomaterial by application of an electric field at elevated temperature to displace cations and anions in opposite directions and
-
(ii)
to develop a piezoelectric biomaterial so that a charge is generated under the application of a mechanical stress.
The following sections review the mechanisms to polarize ionic biomaterials, such as hydroxyapatite (HA), and piezoelectric ceramics, such as barium titanate (BaTiO3), before discussing in vitro and in vivo work on polarized and piezoelectric materials for bone repair.
Polarized Hydroxyapatite (HA) Ceramics as Implant Materials
Hydroxyapatite (HA), Ca10(PO4)6(OH)2, has the ability to chemically interact with bone both in vitro and in vivo. 19,23 The material has been extensively researched as a possible bone substitute material3,19 and its biocompatibility is related to the fact that HA is a major component of bone. The structure of HA consists of a lattice of hydroxyl ions, (OH−), located at the center of Ca2+ triangles along the c-axis of a hexagonal unit cell.60 The OH− ions are aligned in columns parallel to the c-axis, along with Ca2+ and (PO4 3−) ions,33 as in Fig. 3. Since the aligned hydroxyl ions within the c-axis columns are thought to have an important role in ionic conduction,60 HA has been regarded as a one dimensional conductor.62 While HA is frequently considered in hexagonal form it can also exist in a monoclinic form30 and exhibit a non-centrosymmetric unit cell, leading to piezoelectric properties. Tofail et al. have presented piezoelectric stress coefficients for HA which were predicted using an interatomic potential method.55 Ultrasound measurement have also provided experimental evidence of piezoelectric nature of HA, although it was not possible to quantify the value to the piezoelectric coefficients.54
In the absence of any clear or significant piezoelectric behavior for HA materials, it is necessary to polarize the material to create a surface charge. There has been recent interest in the polarization of HA to generate a surface charge by the application of electric fields (kV/cm) at elevated temperature (>200 °C). The importance of the polarization temperature is thought to be due to the fact that the polarization of HA is related to the ordering of lattice OH− ions due to the reorientation of protons around O2−, which is activated at an elevated temperature (200–300 °C).27,61 The presence of surface charges as a result of polarization has been shown to have a significant effect on the crystallization of inorganic ions dissolved in vitro or in vivo and will be discussed in more detail in the next section.
The most common technique used for the polarization is to take sintered HA material and place it between two platinum electrodes21,27,61 which are used to apply an electric field. This whole arrangement is then heated to the desired polarization temperature (typically greater than 200 °C) and a dc electric field of ~1–10 kV/cm is applied for 1 h. The simultaneous application of a high electric field and heat can lead to polarization of the material via ordering of lattice OH− ions due to the reorientation of protons around O2− (compare Figs. 4a and 4b) or ionic conduction due to the migration of OH− or H+ ions in the OH− columnar channels (Fig. 4c).40 The sample is then cooled while maintaining the applied electric field40,53 to produce a polarized HA material. Based on the potential polarization mechanisms described above, the existence of lattice OH− ions is essential for polarization of HA. This has led to polarized HA being sintered in the presence of water vapor to restrict the dehydration of OH− ions. In air, partial dehydration of the OH− ions leaves vacancies within the structure which predominantly determines the conductivity.9
(a) Schematic of OH− ions in HA with no applied electric field. (b) Reorientation of protons under the application of an electric field. (c) Ionic conduction in the OH− columnar channels under the application of an electric field. Reprinted with permission from Nakamura et al.37 Copyright 2001, American Institute of Physics
While the piezoelectric materials, such as barium titanate or bone, develop a charge under the application of a force and can be characterized in terms of piezoelectric coefficients, polarized HA is neither piezoelectric nor ferroelectric. Polarized HA merely has surfaces with a net positive and negative charge and it is necessary to use thermally stimulated depolarization current (TSDC) to characterize the degree of polarization. TSDC simply involves heating a polarized sample under short-circuit conditions in the absence of an electric field and measuring the corresponding depolarization current as a function of temperature. Figure 5 shows typical TSDC curves for HA polarized at various temperatures showing the measured depolarization current density as the HA material is heated. The peak in depolarization current roughly corresponds to the temperature at which the sample was polarized. In addition to peak depolarization current and temperature, it is also possible to calculate the total charge stored in the material from the TSDC data. Takeda et al. recorded remnant polarization in HA of 3600 μC compared with 65 μC for poled ferroelectric BaTiO3.53 Nakamura et al. noted that even though the current density recorded for HA during TSDC measurements was approximately one-twelfth that of BaTiO3, the stored charge in HA was almost twice as large.40 It is this stored charge in HA that is of importance both in vitro and in vivo to the growth of bone cells and bone tissue on synthetic HA.
TSDC spectra of HA ceramics polarized at 1 kV cm−1 for 1 h at 250–400 °C. Reprinted with permission from Nakamura et al.37 Copyright 2001, American Institute of Physics
Piezoelectric Ceramics as Implant Materials
Investigations of piezoelectric ceramics for implantation have focused for the most part on materials containing barium titanate (BaTiO3), a ferroelectric ceramic. Ferroelectrics represent a valuable subgroup of piezoelectric materials, characterized by the presence of a spontaneous polarization in the unstrained state and the capability to reorientate in the direction of polarization. Ferroelectricity corresponds to certain crystal structures, of which the perovskite configuration is the most technologically significant.
As with bone, the origin of piezoelectric behavior in ferroelectric materials originates from the formation of an electrical dipole due to an asymmetric distribution of ions. At high temperatures, the model perovskite BaTiO3 structure has a simple cubic unit cell (Fig. 6a), with large cations (Ba2+) at the corner sites, a smaller cation (Ti4+) in the body center and face centered oxygen ions (O2−). This symmetrical unit cell has no electric dipole and is neither ferroelectric nor piezoelectric. Below a critical temperature referred to as the Curie point, T c, the symmetrical cubic structure transforms to a asymmetrical structure, typically tetragonal or rhombohedral. Associated with this transformation is a spontaneous polarization, which results from the relative shift of ions with respect to the unit cell. The displacement of the ions is restricted to specific crystal directions, allowing polarization toward one of the six faces in the tetragonal cell, or toward one of the eight corners for the rhombohedral phase. Figures 6b and 6c show the net polarization of the unit cell due to its lack of symmetry and the resulting electrical dipole that is responsible for piezoelectric behavior.
Regions in a ferroelectric material such as BaTiO3 where the unit cells have equal polarization directions are known as domains. After sintering a ferroelectric ceramic and cooling below the Curie temperature (T c), domains will form in a notionally random arrangement, such that there is no net polarization in the bulk material. To align the domains in a single direction and make the material piezoelectric, it is necessary to ‘pole’ the material. Figure 7 shows a simple schematic of the poling process. The initial material consists of randomly orientated domains (Fig. 7a). The material is heated to an elevated temperature (normally below the T c) to facilitate domain motion, and a high electric field (typically ~2 kV/mm) applied to orientate domains (Fig. 7b) in a single direction. The material is then cooled to ambient while the electric field is still applied. On removal of the electric field at ambient temperatures, although some domains may change orientation (Fig. 7c), the material retains a net polarization producing a poled ferroelectric ceramic with piezoelectric behavior.
Poling of a ferroelectric ceramic. (a) After sintering the ceramic has a notionally random arrangement of domains. (b) Application of an electric field at elevated temperature causes domains to align with the field. (c) Once cooled to room temperature the field is removed and a remnant polarization and strain is observed
In Vitro and In Vivo Responses to Electrically Active Ceramics
In an early review examining the importance of surface charge species on cell behavior at the biomaterial interface, Davies concluded that surface charge has a profound effect on biological responses.9 It was concluded that surface charges affect the adsorption of proteins onto the material surface and subsequently affect cell migration and morphology. Cells may also be influenced by the release of charge carrier species at the surface and the biological response is dependent on the nature of those charge carriers in addition to their charge sign. These conclusions were based on studies of cells cultured on charged polymer surfaces. The following sections now discuss studies relating to in vitro and in vivo responses to polarized hydroxyapatite and piezoelectric ceramics.
Responses to Polarized Hydroxyapatite
Early work on polarized HA bioceramics investigated the influence of the induced surfaces charges on calcium phosphate deposition and on cellular responses. This in vitro testing is reviewed in the following sections, along with in vivo studies of biological responses to polarized HA. Where relevant, studies involving other electrically active materials are included.
In Vitro Testing
Yamashita et al. examined the bioactivity of polarized HA using immersion studies. They found bone-like crystal growth, which appeared to be accelerated on the negative surfaces of polarized HA immersed in simulated body fluid (SBF).61 Decreased crystal growth was observed on the positive surface. A more recent study agreed with these findings for HA immersed in “stable” SBF solution in which no precipitates were allowed to form.63 Deposition of CaP on positive surfaces did occur, however, when “unstable” soaking solutions were used. In these solutions, the pH or ionic concentrations were altered to allow the nucleation of CaP in the solution. This suggests that the results observed in this type of study are highly dependent on the exact condition of the test environment.
Ohgaki et al. studied in vitro biological responses to polarized HA using osteoblasts.42 While no increase in cell numbers was noted on the charged surfaces in comparison with unpolarized HA controls at 24 h after seeding, larger cell populations were found on negatively charged HA surfaces 48 h after seeding. As no error bars were included for the data, it is not possible to assess the significance of the trends shown. Ohgaki et al. also examined cell responses to positively charged HA and reported reduced cell attachment to the positive surface compared to the neutral surface.42 The mechanism proposed by the authors for the reaction between charged surfaces and the in vitro biological environment is illustrated in Figs. 8a–8c, showing how the exchange of ions and proteins on the surfaces may affect cell attachment. This model includes a mechanism for reduced cell attachment on positively charged surfaces. The work of Jeong et al. concurs with these results, finding greater number of cells on negatively charged HA surfaces compared to neutral surfaces 3 to 4 days after seeding.23
Schematic drawing of the interaction between the polarized charge and environmental materials contributing to cell adhesion. (a) On the neutral material, inorganic ions, amino acids and proteins float and attach to the HA. (b) On the negative material cations, particularly calcium, are selectively adsorbed and form a bone-like apatite layer. This apatite layer encourages the adsorption of proteins and the attachment of cells. (c) On the positive material, anions and negatively charged species are selectively adsorbed and discourage cell attachment
A different trend was, however, observed by Kizuki et al., who found increased osteoblast-like (MC3T3-E1) cell numbers on positively charged HA compared to a negatively charged HA surface two days after seeding.25 Fewer cells were counted on the negative surface than the neutral surface at both time points. Morphologically, the cells were described as being “flattened” on the negative surface.
Although their study examined the attachment of rat marrow stromal cells to charged titanium, rather than to a bioceramic, Qiu et al. contribute to the discussion on cellular responses to charged surfaces.46 In this paper, it is suggested that an increase in substrate surface potential increases the electrical field in the double layer, modifying the local environment in the vicinity of the cell membrane and affecting the intra- or extracellular ion concentrations, altering cell development. This is in general agreement with the mechanisms proposed by Ohgaki et al.,42 though the specific exchange of ions would be influenced by the composition of the implant material.33 A later study on titanium also furthers the understanding of cellular interactions with charged surfaces, highlighting the role of hyaluronan, an extracellular matrix component, in cell adhesion.13 The hyaluronan gives the cell a negative surface charge and has been shown to mediate the first contact between osteoblasts and metal surfaces. The authors link an observed increase in osteoblast adhesion on positive titanium surfaces (zeta potential +7.7 mV) to the negative charge of the hyaluronan.
Improved attachment of osteoblast-like cells to negatively charged HA surfaces has also been reported by Dekhtyar et al. 10 In this study, ten times more cells attached to the charged material than to the electrically neutral surface, with a 1.6 times increase in cell proliferation on the negatively charged HA. More recently, Bodhak et al. have reported increased human foetal osteoblast cell adhesion on negatively polarized HA surfaces and decreased cell attachment on positive surfaces in vitro. 5 This study concurs with Ohgaki et al. in attributing modifications in cell behavior to the differential binding of proteins and inorganic ions to the charged surfaces. However, it was also shown that increasing the surface potential through polarizing the HA led to a decrease in hydrophobicity on the surface. This increase in wettability may account for some of the differences in cell behavior and CaP nucleation on polarized HA surfaces.
Most recently, Nakamura et al. found an increased rate of osteoblast-like (MC3T3-E1) cell migration on polarized HA when compared to non-polarized HA.38 In contrast with some earlier studies, the improvement occurred on both positive and negative surfaces. The increase in migration corresponded to an increased elongation of migrating cells and a change in the pattern of actin filaments within the cytoskeleton.
Although the mechanisms of action proposed by Ohgaki et al.42 appear to have merit and are in general agreement with earlier theory, they are not borne out by the later experimental results. Differences in experimental protocols are likely be the origin of some of the variations in responses seen in these studies. As a range of cell types is used in the studies, differences in phenotype, including for the wide range of cell lines considered “osteoblast-like”,4 may reasonably be expected to cause variation in experimental results. For further discussion on the importance of experimental methods in biomaterials testing, the reader is referred to a recent guide to the biological performance of materials.24 In addition, the surface roughness and topology of the ceramics used in the various experiments are unlikely to be identical. Any one of these factors could influence the biological response and mask or override any effect resulting from polarization.21 It is clear that the polarization of HA does have an influence on biological responses and, in some cases, this influence can be a positive one.
Investigations of polarized HA ceramics have continued in recent years, examining in vivo responses using a range of animal models. The following section summarizes and compares the results of these studies.
In Vivo Testing
Itoh et al. observed enhanced osteoblast activity on both the positive and negative surfaces of polarized HA plates implanted in calvarial bones of rats.21 This was coupled with a decrease in osteoclast activity. The authors attributed the increase in bone formation on the negative surfaces to the accumulation of Ca2+ ions on the surfaces. On the positive surfaces, the observed differences were attributed to the adhesion of molecules such as fibronectin, osteocalcin, and bone morphogenetic proteins (BMPs), improving osteoblast migration.
These results are supported by data obtained by Nakamura et al. from the examination of polarized HA samples implanted in canine femora.39 The surface charge on polarized HA was shown to influence protein adsorption onto the HA surface in vivo. Specifically, increased amounts of fibrin were found on both positive and negative surfaces when compared to neutral surfaces. The authors conclude that the −COOH groups of the fibrin were electrostatically attracted to the positively charged HA surfaces. Calcium ions were attracted to the negatively charged HA surfaces, resulting in the presence of a positively charged ion layer, which subsequently encouraged fibrin adsorption. This increased fibrin layer resulted in improved osteoconduction on both positively and negatively charged HA surfaces through an increase in platelet adhesion and activation. This mechanism is illustrated in Figs. 9a and 9b for negatively and positively charged surfaces, respectively.
A further study reported the results of implanting HA-coated titanium in canine femora for 8 days. It was found that, while all HA coatings bonded with newly formed bone, polarized HA coatings formed stronger bonds than non-polarized coatings, as measured by the force required to pull the implant out of the bone. This effect was more evident for negatively charged coatings than for positively charged coatings.26
Significant improvement has been found in bone ingrowth into polarized samples of porous HA/β-tricalcium phosphate.37 Samples of the polarized material measuring 5.8 mm × 2.8 mm × 1 mm were implanted into femoral diaphyses of rabbits. Two weeks after surgery, bone ingrowth was observed in 90% of the pores in the ceramics. In contrast, in non-polarized samples the majority of pores were filled with fibrous tissue. No link was observed between the polarization axis of the porous HA and the direction of bone growth.
Similarly, Wang et al. investigated bone ingrowth in polarized porous HA samples.57 Their results were in agreement with previous in vivo studies, finding increased bone ingrowth into polarized HA samples with interconnected pores. In this study, new bone growth was found in the center of plugs of porous polarized HA (6 mm diameter, 5 mm length) implanted into rabbit femoral condyle. The increased growth was observed throughout the samples and was not associated with a particular charge (positive or negative). In the non-polarized HA, fibrous tissue had formed instead of bone.
There are evident contradictions in the results found in some of the in vivo and in vitro investigations of biological responses to polarized HA. Specifically, early indications of decreased cell activity on positive surfaces observed in vitro 42 are contested by later studies, both in vitro and in vivo. It is the more recent in vitro work, predicting improved outcomes on both positive and negative surfaces of polarized HA, which corresponds most closely with cellular responses as observed in animal models.
The mechanism proposed by Nakamura et al. 39 (as in Fig. 9) provides an explanation for improving biological responses to both positive and negative surfaces of polarized HA. It appears to concur with the conclusions of Davies9 but is yet to be comprehensively proven.
Current in vitro methods vary greatly in terms of the cell types tested, use of serum and other procedural aspects. They do not replicate the complexity of the chemical, mechanical, electrical, and biological in vivo environment. In particular, cell culture studies do not take into account the presence of blood at the implant site. Certain proteins, blood cells, and particularly macrophages are all present in vivo after implantation59 but are usually absent during in vitro studies for practical reasons. In vitro studies serve as a useful first step in biological testing, reducing the need for animal studies. However, the discrepancies that become evident when the available literature is reviewed and discussed highlight the need for care in the interpretation of in vitro results.
The body of work relating to in vivo studies shows polarized HA to have clear and consistent benefits over electrically inert HA in terms of bone ingrowth and healing in vivo. Both positive and negative surfaces have been shown to induce improved biological responses and some progress has been made toward the identification of the process by which these responses are modified. As much of this work has been carried out by researchers at a single institution, corroboration of the results would be desirable. Further studies are needed to substantiate the evidence of the beneficial in vivo behavior of polarized HA.
Responses to Piezoelectric Ceramics
While polarized HA retains a surface charge which is independent of loading, piezoelectric materials produce electrical signals when exposed to cyclical loading. In this way, they may be used to mimic the stress-generated potentials occurring in bone. The response to a range of materials, including pure ceramics, multiphase ceramics, and ceramic-polymer composites, with piezoelectric properties, has been the subject of a number of studies, both in vivo and in vitro.
In Vitro Studies
In a study of CaP formation on BaTiO3, samples of the ceramic were immersed in SBF for 30 days.20 CaP was found to form preferentially on the negative surfaces of the poled samples. The authors suggest that this demonstrates an increased capacity for bone development on negative surfaces. Although the piezoelectric properties of the material are not given, the poling conditions used (poling in a silicon oil bath whilst cooling from 160 to 25 °C over 2 h with an applied field of 5 kV cm−1) were suitable for inducing a piezoelectric coefficient in the ceramic. A related study by the same group immersed BaTiO3 in Modified Eagle’s Medium (MEM).23 Preferential growth of CaP crystals was observed on the negative surface when compared to the positive surface. The authors suggest that Ca2+ ions adsorb more rapidly on the negative surface and act as nuclei for the formation of CaP. In addition, a similar study evaluated CaP formation on BaTiO3 thin films immersed in MEM.23 A thicker, more homogeneous layer of CaP formed on the negatively poled surface of BaTiO3 compared to an unpoled BaTiO3 surface. Positively poled films were not tested. In addition, the response of L929 mouse fibroblast cells to BaTiO3 thin film materials was investigated. The cells were found to attach (tested 3 h after seeding) and proliferate (tested 3 days after seeding) on the material surface, showing a preference for the negatively charged areas.
The in vitro biocompatibility of BaTiO3-containing piezoelectric polymer films has been examined.2 The adhesion of human osteoblastic cells to poly(vinylidene-trifluoroethylene)/barium titanate (P(VDF-TrFE)-BaTiO3) composites was found to be improved compared to that on a non-piezoelectric polymer control (e-PTFE). Interestingly, the cell adhesion to the e-PTFE was low (around 25% of the seeded cells) with adherence on the piezoelectric material around 70–80%. This study examined both poled and unpoled materials without detecting significant differences (Beloti 2008, personal communication). The d33 of the material was 25–30 pCN−1 and the remnant polarization was 33 μcm−2, though the values cited for remnant polarization do not concur with the polarization-field hysteresis loop given in the same paper.17 The proliferation of cells on P(VDF-TrFE)-BaTiO3 composites was examined up to 10 days after seeding.2 Subsequently, cultures were tested for alkaline phosphatase (ALP) production and matrix mineralization up to 21 days of incubation. The composite was found to encourage an increase in cell numbers, ALP and matrix mineralization when compared to results for the commercially available material. The authors conclude that the piezoelectric film had better in vitro biocompatibility than e-PTFE.
The use of hydroxyapatite-barium titanate (HABT) composites for bone graft was first suggested by Feng et al.12 whose work is discussed in more detail later in this review. The exact composition of the ceramics is not stated. The biocompatibility of the HABT material was investigated by the culture of L929 mouse fibroblast cells in medium in which samples of the ceramic had been soaked.11 This “leaching test” did not detect any cytotoxic effect caused by the composites.
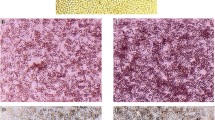
Recently, an in vitro study of osteoblast-like cell behaviors on poled and unpoled HABT ceramics indicated increased cell attachment on both the negative and positive surfaces of the poled material. The composites tested contained 90% BaTiO3 by volume. Cell numbers were, however, similar on poled and unpoled HABT after longer periods in culture. Osteoblast-like cells were shown to proliferate in intimate contact with the material, thus HABT was shown to be biocompatible in vitro.1
This was in agreement with the earlier work of Li et al., who also found ceramics containing up to 20% BaTiO3 by volume to be biocompatible.29 In this study, the doping of titania ceramics with BaTiO3 to produce TiO2/BaTiO3 composites was shown to increase the proliferation of osteoblasts on the material surface. The ceramics used in this study were poled and subjected to mechanical pressure to induce a piezoelectric response. Data is not given for poled samples in the absence of loading and piezoelectric coefficients for the material are not given. The study does, however, add to the evidence of the benefits of using piezoelectric materials in bone as cell numbers were found to be higher on the poled ceramics compared to unpoled samples of the same material up to 6 days after seeding.
Most of the work carried out on piezoelectric materials in vitro has taken place in the absence of mechanical loading. Any differences between cell responses to poled and unpoled materials observed in such studies must therefore be the result of the remnant surface charge in the material and not specifically as a result of the piezoelectricity of the material. However, the majority of these studies focus on the biocompatibility of the materials tested rather than the influence of their electrical state. Ceramics containing BaTiO3 have repeatedly been shown to be biocompatible in vitro. Significantly, where loading was applied to a piezoelectric material, an improvement in biological response was observed.
The earliest in vivo studies on piezoelectric ceramics predate these in vitro studies. This work is reviewed in the following section, along with the more recent investigations of piezoelectric ceramics and composites.
In Vivo Studies
The first study examining the possibility of using piezoelectric BaTiO3 as a bone implant material was carried out in 1980.45 Ceramic samples with porous surfaces and a voltage coefficient (g33) of approximately 9 × 10−3 mVN−1 were implanted into canine femora (specifically, into the cortex of the femoral midshaft). The g33 coefficient is a measure of electric field generated per unit stress. Subjects were sacrificed at 16 and 86 days. Analysis of explanted femora showed larger voltages were produced under compression in samples implanted for the longer period. This was attributed to an increase in osseointegration and therefore improved load transfer to the implants over the course of the experiment.
A subsequent study compared bone responses to poled and unpoled barium titanate ceramics.44 The implantation method was the same as that used in the previous experiment. Subjective assessment of bone ingrowth at the bone–implant interface showed no differences between poled and unpoled samples. In addition, bone–implant interface strengths also showed no difference between the two groups. The authors concluded that the geometry of the holes drilled to house the implants may have restricted loading of the samples, leading to an absence of stress generated voltages in the piezoelectric implants.
Similar problems were encountered in a later study,48 which assessed the biological response to lead-based piezoceramics (Pb(Ti,Zr)O3) with a voltage coefficient (g33) of 11 × 10−3 mVN−1 in avian subjects. No difference was found when comparing poled and unpoled samples. As with the Park et al. study,43 the authors state that experimental design is likely to have led to insufficient loading on the implants to produce a piezoelectric signal. In this case, the piezoelectric signal was limited by the low body weight of the test subjects and the properties of the piezoelectric material. It is concluded that, given the lack of piezoelectric response in the materials, the absence of influence on bone response in these studies is not surprising. Although the poled materials must have retained some remnant surface charge resulting from poling, it is possible that this charge was of a smaller magnitude than that of charged materials found by other studies to exert an influence on biological responses. Neither the piezoelectric coefficient nor the remnant polarization of this material was given.
A later study in a small animal model used an implantation method previously shown to ensure loading of implants.34 In this study, bone responses to chemically identical piezoelectric and neutral polyvinlyidene fluoride (PVDF) films with a piezoelectric charge coefficient of 17 pCN−1 were investigated. Films were implanted in the interosseous membrane of the anterior tibia of rats. Histological analysis of explanted materials showed improved osteogenesis on the piezoelectric films from 7 days to 6 weeks. An increased periosteal response was also noted in the first week. The authors speculate that this periosteal response indicates an increase in production in bone cells in response to the piezoelectric signal, resulting in improved osteogenesis. In agreement with earlier work, increased ossification was found on piezoelectric films made from PLLA in a rabbit model.50
A further study showing an improved biological response to piezoelectric materials was carried out by Feng et al. 12 As with the earlier studies,44,45 BaTiO3-containing ceramics were implanted in canine subjects. In this case, the piezoelectric material was in the form of a hydroxyapatite-barium titanate (HABT) composite. The exact composition and properties of the material are not given. The piezoelectric coefficient was given as 6 pCN−1, though in an earlier paper11 it was reported as 60 pCN−1. The values given for the permittivity of the materials used are also inconsistent, with the relative permittivity of the composites (4864) much higher than that of the BaTiO3 used to manufacture them (1700). This is contrary to the parallel and series equations for the permittivity of a composite, given that reported values of relative permittivity of HA vary between 452 and 57.43 Histological analysis showed improved bone tissue growth on HABT samples compared to HA controls. Bone growth was also found to be direction dependent, being aligned with the direction of poling. The authors claim that these results demonstrate a link between osteogenesis and stress generated potentials in the piezoelectric materials. However, the possible effects of residual surface charge are not considered in this analysis and loading of samples is not quantified.
In vivo responses to P(VDF-TrFE)-BaTiO3 composites, studied previously in vitro,2 were examined.17 Membranes containing 10% BaTiO3 were implanted into rabbit tibiae and the animals were sacrificed 21 days postoperatively. Although bone growth and vascularization indicated the biocompatibility of the material, the authors make no comment on the influence of the remnant polarization or stress-generated potentials in the material on bone growth.
More recently, responses to PVDF polymers were analyzed after the materials were implanted in rats.6 The polymer was in the form of tubes with negatively charged inner surfaces. Bone was found to grow preferentially on the inner surfaces of the tubes. In this study, the authors question whether remnant surface charge, rather than a stress generated potential difference, could be responsible for improved biological responses. The hydrostatic piezoelectric coefficient (d3h) was 2.5 pCN−1. This work is supported by an earlier study on piezoelectric polymers which investigated the promotion of ossification by piezoelectric PLLA films implanted on the periosteum of rabbit tibiae. Newly formed osteoid was detected at 1 week, maturing over 6 to 8 weeks following insertion. Significantly more new bone was formed on the piezoelectric polymers compared to electrically inert films.50
In general, in those studies, both in vitro and in vivo, in which piezoelectric ceramic implants were deemed by the authors to have been appropriately mechanically loaded, improved biological responses were observed. In those studies where implants were not loaded, piezoelectric implants did not perform better than electrically inert controls. It is therefore reasonable to conclude that the piezoelectric nature of the poled and mechanically loaded materials contributed to the improvement of biological responses. In addition, the lack of improvement in unloaded materials suggests that remnant polarization, along with the resulting remnant surface charge, is not sufficiently strong in materials tested to date to induce the improved in vivo biological response seen for poled HA. However, the choice of control materials and lack of non-loaded controls in some studies means that any influence from remnant polarization cannot be considered separately to that of stress-generated potentials. No single study has effectively isolated the influence of surface charge from that of the piezoelectric effect for a particular material.
A uniform study comparing both hydroxyapatite and a piezoelectric ceramic, polarized and non-polarized, would be the most effective way of discerning if the electrical potentials generated in piezoelectric materials have more or less advantage than the static surface charges on poled HA. This would allow the development of a more comprehensive understanding of how the body responds to implanted charged and piezoelectric materials. In general, it appears that there is sufficient evidence, particularly from the in vivo studies, to justify the continued investigation of piezoelectric materials for orthopaedic applications.
Conclusions
A substantial number of investigations have been carried out into the use of piezoelectric and charged ceramics for use as bone implant materials. Polarized HA has been shown to alter biological responses both in vitro and in vivo when compared to non-polarized HA. There are strong indications from in vivo results that polarization can improve bone ingrowth into HA bioceramics.
A range of piezoelectric bioceramics has been shown to be biocompatible. Improved bone ingrowth has also been shown around these materials in cases in which the material was appropriately loaded. Barium titanate-based materials have been the focus of a number of studies which have indicated their potential benefits as implant materials.
The mechanisms by which charges and piezoelectric properties affect responses at the biological interface have been discussed. No single mode of action has been identified to date, although the preferential adsorption of proteins, ions, and other molecules onto surfaces of differing electrical states is probable. Consequently, it can be assumed that responses are related to particular materials rather than to specific electrical states. For example, a positive surface charge on BaTiO3 may induce a different response to a positive charge on HA.
The evidence from the various studies reported in the literature is difficult to compare directly as the compositions of the materials, the charges they retain, the cell types used in vitro and the animal models used in vivo vary. Direct comparisons are therefore impossible to make. However, the indications from the diverse studies are that charged HA and piezoelectric composites based on BaTiO3 have the potential to enhance biological responses at the interface with cells. As such they may have a useful role to play as bone substitute materials in the clinical context in the future.
References
Baxter, F. R., I. G. Turner, C. R. Bowen, J. P. Gittings, and J. B. Chaudhuri. An in vitro study of electrically active hydroxyapatite-barium titanate ceramics using Saos-2 cells. J. Mater. Sci. Mater. Med. 20(8):1697–1708, 2009.
Beloti, M. M., P. T. de Oliveira, R. Gimenes, M. A. Zaghete, M. J. Bertolini, and A. L. Rosa. In vitro biocompatibility of a novel membrane of the composite poly(vinylidene-trifluoroethylene)/barium titanate. J. Biomed. Mater. Res. 79A(2):282–288, 2006.
Best, S., A. Porter, E. Thian, and J. Huang. Bioceramics: past, present and for the future. J. Eur. Ceram. Soc. 28(7):1319–1327, 2008.
Black, J. Biological Performance of Materials: Fundamentals of Biocompatibility. Boca Raton: CRC Taylor & Francis, 2006.
Bodhak, S., S. Bose, and A. Bandyopadhyay. Electrically polarized HAp-coated Ti: in vitro bone cell–material interactions. Acta Biomater. 2009. doi:10.1016/j.actbio.2009.08.008.
Callegeri, B., and W. D. Belangero. Analysis of the interface formed among the poli (viniilidene) fluoride (piezoelectric and non piezoelectric) and the bone tissue of rats. Acta Orthop. Bras. 12(3):160–166, 2004.
Cowin, S. C., and M. L. Moss. Mechanosensory mechanisms in bone. In: Bone Mechanics Handbook, edited by S. C. Cowin. Boca Raton: CRC Press, 2001.
Cowin, S., S. Weinbaum, and Y. Zeng. A case for bone canaliculi as the anatomical site of strain generated potentials. J. Biomech. 28(11):1281–1297, 1995.
Davies, J. E. The importance and measurement of surface charge species in cell behaviour at the biomaterial interface. In: Surface Characterisation of Biomaterials, edited by R. D. Ratner. Amsterdam: Elsevier, 1988.
Dekhtyar, Y., N. Polyaka, and R. Sammons. Electrically charged hydroxyapatite enhances immobilization and proliferation of osteoblasts. 14th Nordic-Baltic Conference on Biomedical Engineering and Medical Physics, Vol. 20. Berlin, Heidelberg: Springer, 2008.
Feng, H. An investigation on the ceramic composite of the biological piezoelectric implants. In: Polymers and Biomaterials. Amsterdam: Elsevier, 1991.
Feng, J., H. P. Yuan, and X. D. Zhang. Promotion of osteogenesis by a piezoelectric biological ceramic. Biomaterials 18(21):1531–1534, 1997.
Finke, B., F. Luethen, K. Schroeder, P. D. Mueller, C. Bergemann, M. Frant, A. Ohl, and B. J. Nebe. The effect of positively charged plasma polymerization on initial osteoblastic focal adhesion on titanium surfaces. Biomaterials 28(30):4521–4534, 2007.
Frost, H. M. A. 2003 update of bone physiology and Wolff’s Law for clinicians. Angle Orthod. 74(1):3–15, 2004.
Fukada, E., and I. Yasuda. On the piezoelectric effect of bone. J. Phys. Soc. Jpn. 12(10):1158–1162, 1957.
Fukada, E., and I. Yasuda. Piezoelectric effects in collagen. Jpn. J. Appl. Phys. 3(2):117–121, 1964.
Gimenes, R., and M. A. Zaghete. Composites PVDF-TrFE/BT used as bioactive membranes for enhancing bone regeneration. Smart Structures and Materials 2004: Electroactive Polymer Actuators and Devices, San Diego, USA, 2004.
Hastings, G. W., and F. A. Mahmud. The electromechanical properties of fluid-filled bone: a new dimension. J. Mater. Sci. Mater. Med. 2(2):118–124, 1991.
Hench, L. L. Bioceramics. J. Am. Ceram. Soc. 81:1705–1728, 1998.
Hwang, K. S., J. E. Song, J. W. Jo, H. S. Yang, Y. J. Park, J. L. Ong, and H. R. Rawls. Effect of poling conditions on growth of calcium phosphate crystal in ferroelectric BaTiO3 ceramics. J. Mater. Sci. Mater. Med. 13(1):133–138, 2002.
Itoh, S., S. Nakamura, M. Nakamura, K. Shinomiya, and K. Yamashita. Enhanced bone ingrowth into hydroxyapatite with interconnected pores by Electrical Polarization. Biomaterials 27(32):5572–5579, 2006.
Jee, W. S. S. Integrated bone tissue physiology: anatomy and physiology. In: Bone Mechanics Handbook, edited by S. C. Cowin. Boca Raton: CRC Press, 2001.
Jeong, J. H., I. J. Kwak, H. I. Kim, J. L. Ong, H. R. Rawls, and Y. J. Park. The 81st General Session of the International Association for Dental Research. Goteberg, Sweden, 2003.
Kieswetter, K., Z. Schwartz, T. W. Hummert, D. L. Cochran, J. Simpson, D. D. Dean, and B. D. Boyan. Surface roughness modulates the local production of growth factors and cytokines by osteoblast-like MG-63 cells. J. Biomed. Mater. Res. 32(1):55–63, 1996.
Kizuki, T., M. Ohgaki, M. Katsura, S. Nakamura, K. Hashimoto, Y. Toda, S. Udagawa, and K. Yamashita. Effect of bone-like layer growth from culture medium on adherence of osteoblast-like cells. Biomaterials 24(6):941–947, 2003.
Kobayashi, T., S. Itoh, S. Nakamura, M. Nakamura, K. Shinomiya, and K. Yamashita. Enhanced bone bonding of hydroxyapatite-coated titanium implants by electrical polarization. J. Biomed. Mater. Res. 82A(1):145–151, 2007.
Kobayashi, T., S. Nakamura, and K. Yamashita. Enhanced osteobonding by negative surface charges of electrically polarized hydroxyapatite. J. Biomed. Mater. Res. 57(4):477–484, 2001.
Li, J., D. Liu, H. Z. Ke, R. L. Duncan, and C. H. Turner. The P2X7 nucleotide receptor mediates skeletal mechanotransduction. J. Biol. Chem. 280(52):42952–42959, 2005.
Li, Z., Y. Qu, X. Zhang, and B. Yang. Bioactive nano-titania ceramics with biomechanical compatibility prepared by doping with piezoelectric BaTiO3. Acta Biomater. 5(6):2189–2195, 2009.
Ma, G. B., and X. Y. Liu. Hydroxyapatite: Hexagonal or monoclinic? Cryst. Growth Des. 9(7):2991–2994, 2009.
Macginitie, L., G. D. Stanely, W. A. Beiber, and D. D. Wu. Bone streaming potentials and currents depend on anatomical structure and loading orientation. J. Biomech. 30(11–12):1133–1139, 1997.
Maeda, H., K. Tsuda, and E. Fukada. The dependence on temperature and hydration of piezoelectric, dielectric and elastic constants of bone. Jpn. J. Appl. Phys. 15(12):2333–2336, 1976.
Mahabole, M. P., R. C. Aiyer, C. V. Ramakrishna, B. Sreedhar, and R. S. Khairnar. Synthesis, characterization and gas sensing property of hydroxyapatite ceramic. Bull. Mater. Sci. 28(6):535–545, 2005.
Marino, A., J. Rosson, E. Gonzalez, L. Jones, S. Rogers, and E. Fukada. Quasi-static charge interactions in bone. J. Electrostatics. 21(2–3):347–360, 1988.
Martin, R. B. Toward a unifying theory of bone remodeling. Bone 26(1):1–6, 2000.
McElhaney, J. H. The charge distribution on the human femur due to load. J. Bone. Jt. Surg. 49A:1561–1571, 1967.
Nakamura, S., T. Kobayashi, M. Nakamura, S. Itoh, and K. Yamashita. Electrostatic surface charge acceleration of bone ingrowth of porous hydroxyapatite/beta-tricalcium phosphate ceramics. J. Biomed. Mater. Res. 2009. doi:10.1016/j.actbio.2009.08.008.
Nakamura, M., A. Nagai, Y. Tanaka, Y. Sekijima, and K. Yamashita. Polarized hydroxyapatite promotes spread and motility of osteoblastic cells. J. Biomed. Mater. Res. 2009. doi:10.1002/jbm.a.32404.
Nakamura, M., Y. Sekijima, S. Nakamura, T. Kobayashi, K. Niwa, and K. Yamashita. Role of blood coagulation components as intermediators of high osteoconductivity of electrically polarized hydroxyapatite. J. Biomed. Mater. Res. 79A(3):627–634, 2006.
Nakamura, S., H. Takeda, and K. Yamashita. Proton transport polarization and depolarization of hydroxyapatite ceramics. J. Appl. Phys. 89(10):5386–5392, 2001.
Nijweide, P. J., E. H. Burger, J. K. Nulend, and A. Van der Plas. The osteocyte. In: Principles of Bone Biology, edited by J. Bilezikian, Z. Raiz, and T. J. Martin. London: Academic Press, 1996.
Ohgaki, M., T. Kizuki, M. Katsura, and K. Yamashita. Manipulation of selective cell adhesion and growth by surface charges of electrically polarized hydroxyapatite. J. Biomed. Mater. Res. 57(3):366–373, 2001.
Parek, B., M. Joshi, and A. Vaidya. Characterization and inhibitive study of gel-grown hydroxyapatite crystals at physiological temperature. J. Cryst. Growth 310(7–9):1749–1753, 2008.
Park, J. B., B. J. Kelly, G. H. Kenner, A. F. von Recum, M. F. Grether, and W. W. Coffeen. Piezoelectric ceramic implants: in vivo results. J. Biomed. Mater. Res. 15(1):103–110, 1981.
Park, J. B., A. F. von Recum, G. H. Kenner, B. J. Kelly, W. W. Coffeen, and M. F. Grether. Piezoelectric ceramic implants: a feasibility study. J. Biomed. Mater. Res. 14(3):269–277, 1980.
Qiu, K., X. J. Zhao, C. X. Wan, C. S. Zhao, and Y. W. Chen. Effect of strontium ions on the growth of ROS17/2.8 cells on porous calcium polyphosphate scaffolds. Biomaterials 27(8):1277–1286, 2006.
Raisz, L. G. Physiology and pathophysiology of bone remodeling. Clin. Chem. 45(8 Pt 2):1353–1358, 1999.
Schumacher, D., U. Gross, and V. Strunz. Does piezoceramic influence avian bone formation in the early postoperative phase? Biomaterials 4(3):215–217, 1983.
Seeley, R. R., T. D. Stephens, and P. Tate. Anatomy and Physiology. Boston: McGraw Hill, 2003.
Shimono, T., S. Matsunaga, E. Fukada, T. Hattori, and Y. Shikinami. The effects of piezoelectric poly-L-lactic acid films in promoting ossification in vivo. In Vivo 10(5):471–476, 1996.
Sikavitsas, V. I., J. S. Temenoff, and A. G. Mikos. Biomaterials and bone mechanotransduction. Biomaterials 22(19):2581–2593, 2001.
Silva, C. C., A. F. L. Almeida, R. S. de Oliveira, A. G. Pinheiro, J. C. Góes, and A. S. B. Sombra. Dielectric permittivity and loss of hydroxyapatite screen-printed thick films. J. Mater. Sci. 38(18):3713–3720, 2003.
Takeda, H., S. Nakamura, K. Yamada, T. Tsuchiya, and K. Yamashita. Dielectric properties of poled hydroxyapatite ceramics. Key Eng. Mater. 181–182:35–40, 2000.
Tofail, S. A. M., D. Haverty, F. Cox, J. Erhart, P. Hána, and V. Ryzhenko. Direct and ultrasonic measurements of macroscopic piezoelectricity in sintered hydroxyapatite. J. Appl. Phys. 105(6), 2009.
Tofail, S. A. M., D. Haverty, K. T. Stanton, and J. B. McMonagle. Structural order and dielectric behaviour of hydroxyapatite. Ferroelectrics 319:117–123, 2005.
Turner, C. H. Three rules for bone adaptation to mechanical stimuli. Bone 23(5):399–407, 1998.
Wang, W., S. Itoh, Y. Tanaka, A. Nagai, and K. Yamashita. Comparison of enhancement of bone ingrowth into hydroxyapatite ceramics with highly and poorly interconnected pores by electrical polarization. Acta Biomater. 5(8):3132–3140, 2009.
Wolff, J. D. Der gesetz der transformation der knochen. Berlin: A. Hirschwald, 1892.
Xia, Z., and J. T. Triffitt. A review on macrophage responses to biomaterials. Biomed. Mater. 1(1):R1–R9, 2006.
Yamashita, K., K. Kitagaki, and T. Umegaki. Thermal instability and proton conductivity of ceramic hydroxyapatite at high temperatures. J. Am. Ceram. Soc. 78(5):1191–1197, 1995.
Yamashita, K., N. Oikawa, and T. Umegaki. Acceleration and deceleration of bone-like crystal growth on ceramic hydroxyapatite by electric poling. Chem. Mater. 8(12):2697–2700, 1996.
Yamashita, K., H. Owada, T. Umegaki, T. Kanazawa, and T. Futagami. Ionic conduction in apatite solid solutions. Solid State Ionics 28–30(1):660–663, 1988.
Zhu, P., Y. Masuda, and K. Koumoto. The effect of surface charge on hydroxyapatite nucleation. Biomaterials 25(17):3915–3921, 2004.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Michael S. Detamore oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Baxter, F.R., Bowen, C.R., Turner, I.G. et al. Electrically Active Bioceramics: A Review of Interfacial Responses. Ann Biomed Eng 38, 2079–2092 (2010). https://doi.org/10.1007/s10439-010-9977-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-010-9977-6