Abstract
Previous research including meta-analytic efforts supports the assumption that depression is able to predict dementia. The mechanisms of this association still remain to be revealed. Some possible explanations as, for example, the glucocorticoid cascade hypothesis assumes that there are underlying changes at the cortical level that drive the association. Therefore, gradual levels of depressive symptoms may also predict gradual change (decline) in cognitive performance. However, testing both of these predictions (depressive symptoms lead to dementia, and depressive symptoms lead to cognitive decline, respectively) with the same data has to our knowledge not been done in the previous literature. A sample of 562 participants aged 65 or older was examined four times over a period of 3 years. Study participants completed established measures of depression and cognitive functioning. Results based on Cox regression analysis showed that depressive symptoms were not able to predict the conversion to dementia during the following 3 years. Additionally, structural equation models as well as latent change score models did not support the assumption that depressive symptoms predict cognitive decline, measured as a continuous variable. We discuss several possibilities to explain these findings including the potential and possible limits of the glucocorticoid cascade hypothesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is a high comorbidity of depression and dementia, particularly with Alzheimer’s disease (AD; Forsell and Winblad 1998; Skoog 1993; Henderson 1990). However, the reasons for this comorbidity have not been fully revealed yet or remain controversial. One possibility is that depression and dementia appear at the same time, because they share common risk factors. Given the widely acknowledged assumption that both disorders have largely different etiologies and therefore deserve clear distinction at the diagnostic level (American Psychiatric Association 1995), it seems more likely that one disorder enhances the probability for the onset of the other. There are, however, inconsistent findings regarding this point. Some studies found an increased risk for older adults with depression to develop AD or major cognitive decline (Bassuk et al. 1998; Cui et al. 2007; Modrego and Ferrández 2004; Wilson et al. 2008; Irie et al. 2008; Saczynski et al. 2010; Van den Kommer et al. 2012), whereas others found an increased risk for people with AD to develop depression (Chen et al. 1999; Vinkers et al. 2004). There are also studies that did not find a longitudinal, but only a cross-sectional association between AD or severe memory decline and depression (Dufouil et al. 1996; Burke et al. 1988; Ganguli et al. 2006; Zimprich et al. 2003). It could be that a considerable portion of the observed inconsistency in the previous literature is due to the great diversity in how depression, AD, or severe cognitive decline were assessed or statistically analyzed. Moreover, some of the studies considered depression and AD as categorical variables, whereas others treated depression and cognitive decline as continuous variables.
To resolve the inconsistency, meta-analyses should be an appropriate mean, given that a considerable number of studies has been published on the subject. Indeed, there are two meta-analyses (Jorm 2001; Ownby et al. 2006) that came to a similar conclusion, i.e., individuals with depression revealed twice as high a risk to develop AD compared to individuals without depression. That is, meta-analytically it seems to be well established that depression comes with a significantly increased likelihood to develop dementia at a later point in time.
However, questions remain in terms of convincing explanations for this pathway. Various theoretical ideas to explain this linkage have been suggested. A prominent example is the glucocorticoid cascade hypothesis (Sapolsky et al. 1986). The central tenet of this approach is that glucocorticoids (GC) are released in reaction to stress (De Nicola et al. 2009) and during an episode of major depression (Gallagher et al. 2009). This effect may have an adaptive function (De Nicola et al. 2009), but prolonged exposure to a high level of GC may have detrimental effects on the hippocampus (Lupien et al. 1998). As a protective mechanism, the hippocampus is involved in a negative feedback loop. Thus, high levels of GC activate glucocorticoid receptors at the hippocampus which inhibit the release of more GC. This negative feedback is affected by aging (De Nicola et al. 2009). Therefore, higher concentrations in older adults do not lead to a sufficient inhibition of GC-release which in turn leads to even higher concentration of GC in the hippocampus and has adverse effects in terms of cognitive function. Thus, prolonged exposure to GC in the hippocampus during an episode of major depression in older adults may damage the hippocampus and thereby lead to memory malfunction.
The situation may be somewhat different, when depressive symptoms become the analytic target. For example, research on the association of cortisol levels and depressive symptoms has shown that this association is very likely not linear. Penninx et al. (2007) found that both very low and very high levels of cortisol are associated with more depressive symptoms. They argue that “low cortisol [is] (noncausally) accompanied with depression because of underlying frailty and high cortisol […] [is] a result of depression” (Penninx et al. 2007, p. 528). Bremmer et al. (2007) also reported a U-shaped association of cortisol level and the prevalence of major depression. These authors state that “this finding [i.e., high cortisol in combination with an episode of major depression is associated with low cognitive performance] might be in line with the glucocorticoid cascade hypothesis” (Bremmer et al. 2007, p. 484).
The GC cascade hypothesis also postulates a link of cortisol level and cognitive performance: as cortisol levels rise, cognitive performance should decrease. However, the relationship of cortisol levels and cognitive performance seems to follow an inverted-U-shape (see Lupien et al. 2007): both high and low cortisol levels are associated with low cognitive performance. Given that older people react stronger towards a testing situation (i.e., with higher cortisol levels) than younger participants (Kudielka et al. 2004; Lupien et al. 2007) one may argue that older people are in a state of relatively high cortisol level during the testing situation. This means that those individuals who have further enhanced cortisol levels (e.g., as a consequence of enhanced depressive symptoms) may show a decrease in cognitive performance as postulated by the GC cascade hypothesis. However, not all data is supportive of the GC cascade hypothesis. For example, Comijs et al. (2010) reported data showing that high cortisol levels were associated with low cognitive performance, but they were not predictive of cognitive decline over a period of 6 years. The authors argue, following the argumentation of Brunner et al. (2006) and Newcomer et al. (1999), that memory function recovers as soon as cortisol levels are back at a normal level. But this suggests that constantly high cortisol levels, which can be expected in depressed persons, should lead to cognitive decline.
Nevertheless, the GC cascade hypothesis is not the only theoretical explanation linking depressive disorders to the onset of dementia. For example, Byers and Yaffe (2011) argue that vascular disease might play a role in this linkage. This “vascular depression hypothesis” (Alexopoulos et al. 1997) states that cerebrovascular disease can be a predisposition for, a cause of, or a perpetuating factor for depressive disorders in later life. Following this argumentation, depression could either lead to vascular disease, which in turn can lead to the onset of dementia, or it could be a mediator linking vascular disease to the onset of dementia.
Another explanation for the high comorbidity of depression and dementia is that depression could be a prodromal state of dementia. This would suggest that neurobiological changes in the preclinical stage of dementia, such as the loss of noradrenergic neurons, give rise to the development of depressive symptoms. This explanation suggests that the causal pathway as compared with the GC hypothesis may actually be reversed: Dementia (or to be more precise: pre-clinical dementia) may increase the risk of the onset of depression. However, there are also problems with this view. For example, early-life depression (occurring before the age of 60) has also been found to be a risk factor for dementia (e.g., Geerlings et al. 2008; Dotson et al. 2010; for a review, see Byers and Yaffe 2011), and a meta-analysis showed that length of interval since diagnosis of depression was positively related to the increased risk to develop dementia (Ownby et al. 2006). Such evidence is opposed to the view of depression being a prodrome of dementia.
Taken together, fully convincing models to explain the linkage between depression and dementia do still not exist, although it seems likely that, as Byers and Yaffe (2011) put it, the “underlying pathway linking depression to dementia is multifactorial, and the proposed mechanisms are probably not mutually exclusive” (p. 329). This study aims to add a missing link to the existing empirical evidence, which may also contribute to a more differentiated understanding of the frequently (but not always) found depression–dementia pathway. Particularly, we focus on depressive symptoms instead of a clinical diagnosis of depression and on both a clinical diagnosis of dementia and continuous cognitive decline. There is some evidence suggesting that there is a linear relationship between the number of depressive symptoms and the incidence of dementia. For example, Wilson et al. (2002) reported that for each additional depressive symptom the risk for the onset of dementia increased by 20 %. This effect was also found among participants with relatively mild depressive symptomatology, i.e., participants who would not have met the criteria for the diagnosis of an episode of major or minor depression. Similarly, Saczynski et al. (2010) reported that both depression as a dichotomous variable and number of depressive symptoms can predict conversion to dementia. Again, the heightened risk to convert to dementia could also be found when taking a continuous measure of depression. Therefore, by using established clinical criteria for the diagnosis of dementia, our first research goal is to replicate the emerging evidence that depressive symptoms can predict the incidence of dementia.
Another question is whether such a risk constellation can also be observed, when taking continuous variables to indicate cognitive decline into account. It is clear that going for such continuous variables is not completely comparable to a yes–no case definition approach, because cognitive decline is not equivalent to the development of dementia. Notably as one of the rare studies in this context, Zimprich et al. (2003) did not find a significant longitudinal association of depressive symptoms and cognitive decline in their community-dwelling sample. Therefore, our second research goal was to impose another empirical test on the question, whether depressive symptoms are able to predict continuous cognitive decline over time.
Testing both predictions in the same sample has the advantage that sample characteristics and the measurement instruments are being held constant.
Method
Study design and sample
The sample consisted of participants who were recruited during a hospital stay in the internal medicine wards of three general hospitals in the city of Munich, Germany. The inclusion criteria were age between 65 and 85 years and residence in the greater Munich area. The age limit of 85 years was introduced since otherwise a very high attrition rate due to mortality would be expected in this prospective study, designed to run over several years. The major reason why this specific sample suits the research questions of this study particularly well is that the sample was expected to have a relatively high incidence rate of dementia across the rather short observation period of 3 years. Exclusion criteria were very severe physical illnesses which according to a physician’s rating would prove lethal within a year or in which complications were to be expected due to participation in the study; previously extant dementia; residence in a nursing home; the need for nursing care according to the criteria of the German long-term care insurance planFootnote 1; blindness or deafness; insufficient German language skill; planned discharge within 48 h. All in all, 2,741 patients fulfilled the inclusion criteria, 1,515 (55.3 %), however, exhibited one or more reasons for exclusion. Of the 1,226 patients available who did not meet any exclusion criteria, 809 (66.0 %) agreed to participate in the study.
The study protocol was approved by the institutional review board of the faculty of medicine at the Technical University of Munich and written informed consent was obtained from the participants. Participants were examined five times by trained physicians and psychologists. The first examination took place during the hospital stay (between April 1999 and March 2001), the first follow-up examination approximately 3 months after discharge from the hospital (M = 14.7 weeks; SD = 10.1). Thereafter, three additional measurement occasions took place, i.e., 1, 2, and 3 years after the second examination, respectively. We will exclude in this study the originally first measurement point, because procedures differed slightly between the sessions in the hospital and sessions at participants’ homes. That is, our study starts with the first follow-up 3 months after discharge (t1), followed by another three measurement points (t2–t4). Of the 809 participants in the baseline assessment, 562 (69.5 %) participated at t1. Reasons for dropout were: conversion to dementia before t1; severe physical illness; death of participant; participant refused to participate. Drop-outs were compared to the remaining participants on those study variables that were assessed at the baseline assessment (results shown below after introduction of measures).
Measures
Cognitive functioning
To assess cognitive functioning we used the Mini Mental State Examination (MMSE; Folstein et al. 1975), the syndrome short test (Syndrom-Kurz Test, SKT; Erzigkeit 2001), and the Clinical Dementia Rating Scale (CDR; Hughes et al. 1982). The MMSE consists of 30 items and tests memory performance, executive functioning, and orientation. The range is from 0 (worst performance) to 30 (perfect performance). Internal consistency across the four measurement occasions of the present study ranged from α = .67 (t1) to α = .86 (t4). The SKT is a brief instrument that tests memory performance and attention. It consists of nine subtests (three tests for memory performance and six tests for attention). For each of the nine subtests a score of zero means best performance and a score of three indicates worst performance. The subtest scores are summed up, i.e., the range is from 0 (best performance) to 27 (worst performance). Internal consistency in this study ranged from α = .79 (t1) to α = .86 (t4). After each session the severity of cognitive impairment was rated on the CDR based on all available information. Possible CDR scores are 0 (no cognitive impairment), 0.5 (very mild dementia), 1 (mild dementia), 2 (moderate dementia), and 3 (severe dementia).
Depressive symptoms
Depressive symptoms were assessed using the 15-item version of the Geriatric Depression Scale (GDS; Sheikh and Yesavage 1986) and the short scale mood/activation (Kurzskala Stimmung/Aktivierung, KUSTA; Binz and Wendt 1986). The range for the GDS is from 0 (no depressive symptoms) to 15 (high depressive symptoms). Internal consistency ranged from α = .73 (t1) to α = .76 (t4). The KUSTA consists of three items and participants were instructed to rate their current mood and activation on a seven-point Likert scale. The range therefore is from 0 (high depressive symptoms) to 21 (no depressive symptoms). Internal consistency ranged from α = .61 (t1) to α = .69 (t3).
The data was transformed so that high scores indicate good cognitive performance (MMSE and SKT) and high depressive symptoms (GDS and KUSTA), respectively. Table 1 gives an overview of the descriptive statistics of the sample.
Additional measures
Additional data was collected, including participants’ gender, age, and years of education. 59.6 % of the participants were female. On average, participants were 75.7 years old at t1 (SD = 5.51), and had 9.57 years of education (SD = 2.85). Finally, the severity of physical illness was assessed using the Charlson Comorbidity Index (Charlson et al. 1987). This score indicates the number of comorbid diseases weighted by the severity of the disease; the mean score in our sample was 1.64 (SD = 1.41).
Drop-out analysis
Drop-outs between baseline assessment and t1 were younger, had higher comorbidity scores, and lower MMSE scores at the baseline assessment (all ts > 2.17, all ps < .05) than the remaining participants. Selective drop-out of depressed participants would not be unexpected, as depression has been found to be linked to higher comorbidity, mortality, as well as more and longer hospital stays (Prina et al. 2012); however, KUSTA scores at baseline assessment did not differ between drop-outs and the remaining sample (t(804) = 1.18, p = .238).
Data transformation and data analysis
Regarding our first research question, participants were classified as demented if their CDR score at the respective measurement occasion was greater than 0.5 (Hughes et al. 1982). We then conducted a Cox regression survival analysis with time-to-event (demented vs. not demented) as dependent variable. In a first step, we entered age, gender, years of education, and comorbidity into the regression. In a second step, we entered the GDS score at t1. Time-to-event was calculated as time from t1 assessment to the last assessment in the study (in days) for those participants whose CDR scores were not greater than 0.5 at any measurement occasion. For the other participants, time-to event was defined as follows: If the first time the CDR score was greater than 0.5 at the nth measurement occasion, time-to event was calculated as time from t1 to t(n − 1) plus half the time interval between t(n − 1) and tn. If, for example, a participant’s CDR score was greater than 0.5 at t3 (and less than or equal 0.5 at t1 and t2), time-to-event was calculated as (time in days between t1 and t2) + (time in days between t2 and t3)/2. This was done because the exact day of the onset of dementia is unknown. Therefore, the best approximation is that it happened halfway between measurement occasions.
In order to address our second research question, a structural equation model (SEM) approach was used in the first step. For each measurement occasion, GDS scores and KUSTA scores were used as manifest indicators for the latent depressive symptoms factor. Also, for each measurement occasion, MMSE and SKT scores were used as manifest indicators for the latent cognitive performance factor (in the following called “cognition”). The weights of MMSE scores and GDS scores, respectively, were fixed to one across all measurement occasions in order to scale the latent factors (Schumacker and Lomax 2010). In the second step, we used a latent change model (LCM) Type II approach (Steyer et al. 1997). That is, for each measurement occasion GDS scores and KUSTA scores were used as manifest indicators for the latent depressive symptoms factor. The latent cognitive performance factors were modeled as follows: There were four latent factors, the first of which can be interpreted as the true state of cognitive performance at t1 (in the following called “cognition baseline”). The other three factors (in the following called “cognition change”) can be interpreted as latent change compared to the previous measurement occasion (i.e., the latent change in cognitive performance from t1 to t2, from t2 to t3, and from t3 to t4, respectively; see Steyer et al. 1997). MMSE and SKT scores at t1 were used as indicators for the latent cognition baseline factor only; MMSE and SKT scores at t2 were used as indicators for the latent cognition baseline factor and the first cognition change factor; MMSE and SKT scores at t3 were used as indicators for the latent cognition baseline factor and the first two cognition change factors; and MMSE and SKT scores at t4 were used as indicators for all four latent factors. All latent cognition factors, thus, can be interpreted as latent change compared to the previous measurement occasion (see Steyer et al. 1997). Again, the regression weights of GDS scores were fixed to one across all measurement occasions in order to scale the latent depressive symptoms factor. Additionally, the regression weight of MMSE at t1 on the cognition baseline factor was fixed to one, as were the regression weights of the other MMSE scores on the respective cognition change factors (Schumacker and Lomax 2010). For both models, the latent measurement errors for the four SKT scores were allowed to co-vary, as were the latent measurement errors for the four KUSTA scores. The level of factorial invariance across time (Meredith 1993) was assessed following recommendations by Dimitrov (2010).
Analyses were conducted using SPSS Version 20 for Windows and Mplus Version 5 for Windows (Muthén and Muthén 2007).
Results
Predicting dementia as a function of depressive symptoms
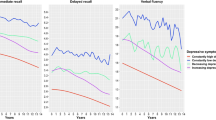
In the course of the study, a total of 84 participants converted to dementia across the 3-year observation period. Another 16 participants who were classified as demented at t1 were not included in the analysis. In a first step, age, gender, years of education, and the Charlson Comorbidity Index were entered as covariates into a Cox regression analysis with time-to-event (demented vs. not demented) as dependent variable. The overall model was significant, χ2(4) = 32.86, p < .001. In a second step, GDS score at t1 was entered into the regression. The overall fit increased, but this increase failed to reach significance, χ 2diff (1) = 1.89, p = .170. Also, the regression weight for GDS score was not significant, b = .06, Wald(1) = 1.98, p = .160. The Hazard Ratio for GDS score was 1.06 (95 % CI: [0.98; 1.15]). Of the covariates, only the regression weight for age became significant, b = .04, Wald(1) = 28.10, p < .001; the regression weights for the covariates gender, years of education and comorbidity did not reach significance (all ps > .255). Figure 1 depicts the cumulated hazard for the onset of dementia as a function of time and depressive symptoms.Footnote 2 Although Fig. 1, based on a median split of the depressive symptom score, suggests that there seems to be some truth in the depressive symptoms—dementia pathway, we were not able to confirm a statistically meaningful linkage between depressive symptoms and the prospective occurrence of dementia in our data after adjustment for confounders.
Testing temporal relationships among depressive symptoms and continuous cognitive decline
A crucial issue when applying structural equation models to longitudinal data is to assess whether the assumption of factorial invariance across time is tenable. According to Meredith (1993), there are different levels of factorial invariance. Configural invariance means that the number of latent factors remains constant across time. This assumption is clearly met in this analysis, as there was one latent cognition factor and one latent depressive symptoms factor at each measurement occasion. Weak factorial invariance means that the factor loadings of the manifest indicators remain constant across measurement occasions. Strong factorial invariance can be assessed by further constraining the intercepts of the manifest indicators to be equal across time. Under strict factorial invariance, the residual variances of the manifest indicators have to be equal across time as well. In order to determine the level of factorial invariance in the data, measurement models were built as described above for the SEM. The eight latent factors (four cognition factors and four depressive symptom factors) were allowed to co-vary. This model served as baseline measurement model under the assumption of configural invariance.
The assumption of weak factorial invariance was tested by constraining the loadings of the indicators to be equal across time. This was accomplished by constraining the regression weights of the SKT scores to be equal across time, and by constraining the regression weights of the KUSTA scores to be equal across time.Footnote 3 To test the assumption of strong factorial invariance, the intercepts of the four MMSE scores and the four GDS scores were constrained to be zero, the intercepts of SKT and KUSTA scores, respectively, were constrained to be equal across time, and the means of the latent cognition and latent depressive symptom factors were explicitly estimated (see Dimitrov 2010). Finally, to test the assumption of strict factorial invariance, the residual variances of the MMSE scores were constrained to be equal across time, as were the residual variances of the four SKT scores, the four GDS scores, and the four KUSTA scores, respectively. Because these models are nested models, Chi-square difference scores can be used for model comparisons. As can be seen from Table 2, model fit did not statistically differ between the baseline model and the model under the assumption of weak factorial invariance (χ2(6) = 11.73, p = .068) and between the model under the assumption of weak factorial invariance and the model under the assumption of strong factorial invariance (χ2(6) = 5.97, p = .427). However, the model under the assumption of strict factorial invariance fitted significantly worse than the model under the assumption of strong factorial invariance (χ2(12) = 72.95, p < .001). The other fit indices in Table 2 also favor the model under the assumption of strong factorial invariance. Therefore, the model that we used to test our hypothesis that depressive symptoms predict cognitive performance was built under the assumption of strong but not strict factorial invariance.
Figure 2 depicts the SEM tested and Table 3 shows the standardized regression coefficients for the manifest indicators of the latent variables. The overall Chi-square test reveals that there was not a good fit for the specified model assuming that depressive symptoms lead to lowered cognitive functioning. Considering the relatively large sample size this test might, however, be too liberal (Schumacker and Lomax 2010). Therefore, with large sample sizes, using other fit indices such as the Root Mean Square Error of Approximation (RMSEA) and the Comparative Fit Index (CFI) is more appropriate. These fit parameters indicated that the model provides a good fit for the data. Although the lagged coefficients for the latent cognition factors were high (ranging from .88 to .95), the residual variances of these factors were statistically significantly greater than 0 (all ps < .001). This means that cognitive performance is rather stable across time, but it is not perfectly predicted by cognitive performance at the preceding measurement occasion. However, the predicted regression weights from the latent depressive symptoms factor to the latent cognition factor were all not significant (all ps > .083; Fig. 2). When these three regression weights were fixed to zero, model fit did not change significantly, χ 2diff (3) = 5.48, p = .140. Thus, our SEM approach did not support a meaningful relationship between depressive symptoms and cognitive performance.
Going further, we additionally tested a LCM as depicted in Fig. 3; Table 4 shows the standardized regression coefficients for the manifest indicators of the latent variables.Footnote 4 The overall Chi-square test shows that there was not an adequate model fit, while other fit indices reveal an acceptable overall model fit. However, the regression weights from the latent depressive symptoms factors to the latent cognition change factors were all not significant (all ps > .118). When these three regression weights were fixed to zero, model fit did not change significantly, χ 2diff (3) = 3.60, p = .308. Thus, the LCM analysis again confirmed that depressive symptoms cannot predict cognitive decline.
Discussion
Overall, our results convergently show that depressive symptoms were not able to predict a person’s risk to develop dementia across a 3-year observational interval. We did not anticipate this result, as prior research has shown, that depressive symptoms are associated with greater incidence of dementia (Wilson et al. 2002; Saczynski et al. 2010). These diverging findings could be the result of measurement instruments and applying different diagnostic criteria, length of the observation period, statistical power due to different numbers of dementia cases, or low reliability of the effect. As to the first possibility, measurement instruments and diagnoses of dementia cases were not identical across previous studies. Whereas both, Wilson et al. (2002) and Saczynski et al. (2010) used the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977), the present results are based on the GDS. Additionally, while Wilson et al. used a 10-item short version of the CES-D and calculated the effect for every one-point increase in the CES-D scale, Saczynski et al. used the 60-item version and calculated the effect for every 10-point increase in this scale. Furthermore, Wilson et al. (2002) based the diagnosis of dementia on the criteria for probable or possible AD according to the criteria of the National Institute of Neurologic and Communicative Disorders and Stroke and the AD and Related Disorders Association (NINCDS/ADRDA; McKhann et al. 1984); Saczynski et al. relied on the criteria of the DSM-IV (American Psychiatric Association 1995). One might argue that, as the criterion in this study was less stringent, this might have lead to a number of false positive diagnoses in our sample. Although we cannot exclude this possibility, we argue that this was not the main reason why our results differed from the results obtained by the other two studies, as using a more strict criterion did not change the results (see also Footnote 2).
Concerning the second possibility, the length of the observation period in this study (3 years) was shorter than the length in the Wilson et al. study (up to 7 years) or the length in the Saczynski et al. study (up to 17 years). One could argue that the interval in this study was simply not long enough to detect the effect of depressive symptoms on the incidence of dementia. This is especially true when considering the finding by Ownby et al. (2006) that the effect of depression on the incidence of dementia increases as the interval between the diagnosis of depression and the onset of dementia increases.
Additionally, the shorter interval in this study also came with a lower number of dementia cases (84 cases) compared to the Wilson et al. and Saczynski et al. studies (108 and 164, respectively), and in turn with decreased statistical power. However, the effect sizes in these two studies were substantial (Hazard Ratios 1.19 and 1.41, respectively). If a similarly large effect had been present in our sample, statistical power would have been sufficient to detect it.
One final reason to explain the diverging results might be that the mechanism that is driving the increased risk for persons with depression (as a dichotomous variable) to develop dementia cannot be observed when using depressive symptoms (as continuous variable). This interpretation receives some support from the inconsistent results regarding the predictive validity of depressive symptoms for the incidence of dementia. In line with our results, Becker et al. (2009) did not find a longitudinal association of depressive symptoms and conversion to dementia either. Therefore, whereas the longitudinal association of depression and dementia has been established meta-analytically, the association of depressive symptoms and incidence of dementia is less well established. Our second main result that depressive symptoms cannot predict cognitive performance (as a continuous variable) or cognitive decline is also in line with the interpretation that the mechanism responsible for the depression-dementia association (Jorm 2001; Ownby et al. 2006) does not work for the continuous variable depressive symptoms. This finding is also consistent with data reported by Zimprich et al. (2003) who also did not find a longitudinal association of depressive symptoms and continuous cognitive performance decrements.
Taken together, our findings are contrary to the predictions made by GC cascade hypothesis (Sapolsky et al. 1986), which would predict that heightened number of depressive symptoms should lead to an increased incidence of dementia and predict cognitive decline. None of these effects were observed in our data. We cannot exclude, however, the possibility that accumulating depressive symptoms lead to increased cortisol levels as assumed by the GC cascade hypothesis, because we did not measure cortisol levels. Thus, there are two possibilities to discuss our findings in light of the GC cascade hypothesis. First, the GC cascade mechanism can explain the depression-dementia link, but depressive symptoms do not increase cortisol levels. However, prior research suggests that high number of depressive symptoms (measured as a continuous variable) lead to high cortisol levels (Penninx et al. 2007). The second possibility is that the GC cascade mechanism is not the causal factor underlying the depression-dementia link. This argumentation is also in line with results reported by Comijs et al. (2010) who found that cortisol levels could not predict cognitive decline.
As reported in the introduction, the association between cortisol levels and cognitive performance follows an inverted-U-shape, i.e., both low and high cortisol levels are associated with low cognitive performance (Lupien et al. 2007). So far we have only elaborated on the right end of this inverted-U (association of high cortisol level and low cognitive performance). As high numbers of depressive symptoms are related to both low and high cortisol levels (Penninx et al. 2007) the possibility remains that those participants who had a relatively high number of depressive symptoms and high cortisol levels did have increased risk to develop dementia, and those participants who had a relatively high number of depressive symptoms but low cortisol levels did not have this elevated risk. Such an explanation would be partially consistent with the GC cascade hypothesis by explaining the depression–dementia link for those participants with depression and elevated cortisol levels only. The other group (depression plus low cortisol levels) would then either be subject to a different mechanism (e.g., cerebrovascular disease, cf. Alexopoulos et al. 1997) or not show an elevated risk to develop dementia. On the other hand, as low cortisol levels are also associated with low cognitive performance, one could also expect this group to show an elevated risk to develop dementia. However, it is not possible to answer the question whether this was the case in our sample as cortisol levels were not assessed.
The major strength of this study is the multifaceted statistical approach taken to test the study hypotheses. As our results are supported by a typically epidemiologic approach (Cox regression) and by two psychometric approaches (SEM and LCM) we are confident about the validity of our results. Furthermore, the fit indices were in an acceptable (LCM) to very good (SEM) range which further increases the credibility of our results.
Nevertheless, the present study comes with a number of limitations. In our study, no clinically established diagnosis of depression was available. Therefore, a direct comparison with the results reported in the two meta-analyses (Jorm 2001; Ownby et al. 2006) is not possible. Another limitation can be seen with regard to the assessment of cognitive performance. Although the MMSE is widely used for assessment of mild cognitive impairment and dementia, it is not very sensitive to gradual changes in cognitive performance (Zimprich et al. 2003). Therefore, one might argue that we could not capture small gradual changes in cognitive performance of the non-demented participants. However, we modeled cognitive performance at the latent level by means of the MMSE and the SKT and therefore this problem may have been reduced at least to some extent. One should also note that the overall model fit of the LCM indicates that there was sufficient variance in the cognitive change variables. This does of course not rule out the possibility that we might have obtained different results, when using cognitive tests that are more sensitive to gradual changes such as the digit symbol test. Going further, our observation period of 3 years may have been simply not long enough to see the effect of depressive symptoms on cognitive performance. As discussed above the measurement intervals reported by Wilson et al. (2002) and Saczynski et al. (2010) were longer than 3 years. One could argue that number of depressive symptoms is only predictive for the incidence of dementia in a longer time span (Ownby et al. 2006). Whether this association is also true for depressive symptoms (as a continuous variable) is a question that needs to be addressed by future research. In addition to a rather short observation period, the length between the measurement occasions differed slightly between participants in our sample. If timing of the measurement occasions would be correlated with our study variables, this could likely have confounded our results. However, interval length between the measurement occasions was not correlated with age, comorbidity, GDS score at t1 or MMSE score at t1, all |r|s < .08, all ps > .081. It, thus, seems unlikely that this could have biased our results.
Also, our sample of participants originally recruited in internal medicine wards of general hospitals may have possessed particular features, which may have had some impact on the depressive symptoms–cognitive performance linkage. For example, our sample may have been somewhat more unhealthy than the general population and this may have overshadowed the depressive symptoms–cognitive performance pathway. Depressive symptoms, which were assessed 3 months after discharge from the hospital, could reflect prior and current health problems.Footnote 5 We cannot be certain that this pattern of results can also be found in a more representative sample. Regarding the role of education, more than 60 % of our participants had only the most basic education in the German educational system. Only 10 % of our sample had a college degree. Therefore, level of education in our sample was not unusually high, but rather in an expected range for an urban population. Also, drop-out analyses support the notion that the remaining sample from baseline to t1 was not less depressed as compared to drop-outs. Additionally, our data did not allow to test the glucocorticoid cascade hypothesis or related neurobiological ideas directly, that is, further research able to shed more light on the mechanisms involved should consider to include behavioral measures as well the assessment of neurochemical correlates.
Future research is clearly needed to better understand the depression–cognitive impairment pathway, resolve remaining inconsistencies, and to shed more light on the mechanisms that underlie the interplay between depression, cognitive impairment and dementia.
Notes
In the year 1995 Germany introduced a statutory long-term care insurance. People who are persistently dependent on the assistance of caregivers are eligible for benefits from this insurance. These participants were excluded from this study as people in need for nursing are often diagnosed with dementia and have lower life expectancies. Because this study was planned as a longitudinal study to investigate the precursors of and risk factors for dementia (see Bickel et al. 2006), this exclusion criterion seemed justifiable.
We used CDR > .5 as cut-off because we did not expect many participants to develop moderate to severe dementia (CDR > 1) within this short measurement interval. Nevertheless, we repeated the analyses using a more strict criterion (classifying only participants with a CDR score of 2 or 3 as demented). The results obtained in this analysis did not change, the regression coefficient for the GDS score remained insignificant.
Please note that the regression weights of MMSE scores and GDS scores have already been fixed to be one in the configural invariance model.
Please note that this model was built under the assumption of strict factorial invariance for the latent depressive symptoms factor. Here, too, the level of factorial invariance across time was determined using the approach described above. Assessing factorial invariance for the cognition change factors was not appropriate given the different approach with which they were modeled. Therefore, factorial invariance was only determined for the latent depressive symptoms factor. The results of this analysis mirror the results for the SEM approach with one exception: the model under the assumption of strict factorial invariance did not fit significantly worse than the model under the assumption of strong factorial invariance, χdiff 2(6) = 8.58, p = .199. Therefore, the model used for the LCM approach was tested under the assumption of strict factorial invariance for the latent depressive symptoms factor.
We thank an anonymous reviewer for this important observation.
References
Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M (1997) The ‘vascular depression’ hypothesis. Arch Gen Psychiatry 54(10):915–922
American Psychiatric Association (1995) Diagnostic and statistical manual of mental disorders: DSM-IV, international version with ICD-10 codes, Washington, DC
Bassuk SS, Berkman LF, Wypij D (1998) Depressive symptomatology and incident cognitive decline in an elderly community sample. Arch Gen Psychiatry 55(12):1073–1081
Becker JT, Chang Y-F, Lopez O, Dew MA, Sweet RA, Barnes D, Yaffe K, Young J, Kuller L, Reynolds CF III (2009) Depressed mood is not a risk factor for incident dementia in a community-based cohort. Am J Geriatr Psychiatry 17(8):653–663
Bickel H, Mösch E, Seigerschmidt E, Siemen M, Förstl H (2006) Prevalence and persistence of mild cognitive impairment among elderly patients in general hospitals. Dement Geriatr Cogn Disord 7:242–250
Binz U, Wendt G (1986) KUSTA. Kurz-Skala Stimmung/Aktivierung. Manual 2. Revidierte und erweiterte Auflage (Short scale mood/activation. Second edition). Beltz, Weinheim, Germany
Bremmer MA, Deeg DJH, Beekman ATF, Penninx BWJH, Lips P, Hoogendijk WJG (2007) Major depression in late life is associated with both hypo- and hypercortisolemia. Biol Psychiatry 62(5):479–486
Brunner R, Schaefer D, Hess K, Parzer P, Resch F, Schwab S (2006) Effect of high-dose cortisol on memory functions. In: Yehuda R (ed) Psychobiology of posttraumatic stress disorders: a decade of progress. Blackwell Publishing, Malden, pp 434–437
Burke WJ, Rubin EH, Morris JC, Berg L (1988) Symptoms of “depression” in dementia of the Alzheimer type. Alz Dis Assoc Dis 2:356–362
Byers AL, Yaffe K (2011) Depression and risk of developing dementia. Nat Rev Neurol 7:323–331
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Chen P, Ganguli M, Mulsant BH, DeKosky ST (1999) The temporal relationship between depressive symptoms and dementia: a community-based prospective study. Arch Gen Psychiatry 56(3):261–266
Comijs HC, Gerritsen L, Penninx BWJH, Bremmer MA, Deeg DJH, Geerlings MI (2010) The association between serum cortisol and cognitive decline in older persons. Am J Geriatr Psychiatry 18(1):42–50
Cui X, Lyness JM, Tu X, King DA, Caine ED (2007) Does depression precede or follow executive dysfunction? Outcomes in older primary care patients. Am J Psychiatry 164(8):1221–1228
De Nicola AF, Pietranera L, Beauquis J, Ferrini MG, Saravia FE (2009) Steroid protection in aging and age-associated diseases. Exp Gerontol 44:34–40
Dimitrov DM (2010) Testing for factorial invariance in the context of construct validation. Meas Eval Couns Dev 43(2):121–149
Dotson VM, Beydoun MA, Zonderman AB (2010) Recurrent depressive symptoms and the incidence of dementia and mild cognitive impairment. Neurology 75(1):27–34
Dufouil C, Fuhrer R, Dartigues J-F, Alpérovitch A (1996) Longitudinal analysis of the association between depressive symptomatology and cognitive deterioration. Am J Epidemiol 144:634–641
Erzigkeit H (2001) Kurztest zur Erfassung von Gedächtnis- und Aufmerksamkeitsstörungen: SKT; Form A; Form B; Form C; Form D; Form E. (Syndrom Short Test) Geromed, Erlangen, Germany
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Forsell Y, Winblad B (1998) Major depression in a population of demented and nondemented older people: prevalence and correlates. J Am Geriatr Soc 46(1):27–30
Gallagher P, Reid KS, Ferrier IN (2009) Neuropsychological functioning in health and mood disorder: modulation by glucocorticoids and their receptors. Psychoneuroendocrinology 34(Suppl 1):196–207
Ganguli M, Du Y, Dodge HH, Ratcliff GG, Chang C-Ch (2006) Depressive symptoms and cognitive decline in late life. A prospective epidemiological study. Arch Gen Psychiatry 63(2):153–160
Geerlings MI, den Heijer T, Koudstaal PJ, Hofman A, Breteler MMB (2008) History of depression, depressive symptoms, and medial temporal lobe atrophy and the risk of Alzheimer disease. Neurology 70(15):1258–1264
Henderson AS (1990) Co-occurence of affective and cognitive symptoms: the epidemiologial evidence. Dementia 1:119–123
Hughes C, Berg L, Danziger W, Coben L, Martin R (1982) A new clinical scale for the staging of dementia. Brit J Psychiatry 140(6):566–572
Irie F, Masaki KH, Petrovitch H, Abbott RD, Ross GW, Taaffe DR, Launer LJ, White LR (2008) Apolipoporotein E ε4 allele genotype and the effect of depressive symptoms on the risk of dementia in men. The Honolulu-Asia Aging Study. Arch Gen Psychiatry 65(8):906–912
Jorm AF (2001) History of depression as a risk factor for dementia: an updated review. Aust NZ J Psychiatry 35(6):776–781
Kudielka BM, Buske-Kirschbaum A, Hellhammer DH, Kirschbaum C (2004) HPA axis responses to laboratory psychosocial stress in healthy elderly adults, younger adults, and children: impact of age and gender. Psychoneuroendocrinology 29(1):83–98
Lupien SJ, de Leon M, de Santi S, Convit A, Tarshish C, Nair NPV, Thakur M, McEwen BS, Hauger RL, Meaney MJ (1998) Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat Neurosci 1(1):69–73
Lupien SJ, Maheu F, Tu M, Fiocco A, Schramek TE (2007) The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition. Brain Cogn 65(3):209–237
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan E (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS/ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34:939–944
Meredith W (1993) Measurement invariance, factor analysis and factorial invariance. Psychometrika 58(4):525–543
Modrego PJ, Ferrández J (2004) Depression in patients with mild cognitive impairment increases the risk of developing dementia of Alzheimer type. Arch Neurol 61(8):1290–1293
Muthén LK, Muthén BO (2007) Mplus user’s guide, 5th edn. Muthén & Muthén, Los Angeles, CA
Newcomer JW, Selke G, Melson AK, Hershey T, Craft S, Richards K, Alderson AL (1999) Decreased memory performance in healthy humans induced by stress-level cortisol treatment. Arch Gen Psychiatry 56(6):527–533
Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D (2006) Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry 63(5):530–538
Penninx BWJH, Beekman ATF, Bandinelli S, Corsi AM, Bremmer M, Hoogendijk WJ, Guralnik JM, Ferrucci L (2007) Late-life depressive symptoms are associated with both hyperactivity and hypoactivity of the hypothalamo-pituitary-adrenal axis. Am J Geriatr Psychiatry 15(6):522–529
Prina A, Deeg D, Brayne C, Beekman A, Huisman M (2012) The association between depressive symptoms and non-psychiatric hospitalisation in older adults. Plos ONE 7(4). doi:10.1371/journal.pone.0034821
Radloff LS (1977) The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Saczynski JS, Beiser A, Seshadri S, Auerbach S, Wolf PA, Au R (2010) Depressive symptoms and risk of dementia. The Framingham Heart Study. Neurology 75:35–41
Sapolsky RM, Krey LC, McEwen BS (1986) The neuroendocrinology of stress and aging: the glucocorticoid cascade hypothesis. Endocr Rev 7:284–301
Schumacker RE, Lomax RG (2010) A beginner’s guide to structural equation modeling. Routledge, New York
Sheikh JI, Yesavage JA (1986) Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 5(1–2):165–173
Skoog I (1993) The prevalence of psychotic, depressive and anxiety syndromes in demented and non-demented 85-year-olds. Int J Geriatr Psychiatry 8(3):247–253
Steyer R, Eid M, Schwenkmezger P (1997) Modeling true intraindividual change: true change as a latent variable. Method Psychol Res 2(1):21–33
Van den Kommer TN, Commijs HC, Aartsen MJ, Huisman, M, Deeg DJ, Beekman AT (2012) Depression and cognition: how do they interrelate in old age? Am J Geriatr Psychiatry (e-published)
Vinkers DJ, Gussekloo J, Stek ML, Westendorp RGJ, van der Mast RC (2004) Temporal relation between depression and cognitive impairment in old age: prospective population based study. Brit Med J 329:881–884
Wilson RS, Barnes LL, de Leon CFM, Aggerwal NT, Schneider JS, Bach J, Pilat J, Beckett LA, Arnold SE, Evans DA, Bennett DA (2002) Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology 59(364):370
Wilson RS, Arnold SE, Beck TL, Bienias JL, Bennett DA (2008) Change in depressive symptoms during the prodromal phase of Alzheimer disease. Arch Gen Psychiatry 65(4):439–446
Zimprich D, Martin M, Kliegel M (2003) Subjective cognitive complaints, memory performance, and depressive affect in old age: a change-oriented approach. Int J Aging Hum Dev 57(4):339–366
Acknowledgments
This study was supported by Dr. Willmar Schwabe Arzneimittel, Karlsruhe, Germany. We are indebted to the hospital medical directors Prof. Dr. A. Schömig, Prof. Dr. M. Classen (Klinikum rechts der Isar, Fakultät für Medizin der Technischen Universität München), Prof. Dr. R. Heinrich (Städtisches Krankenhaus München-Neuperlach), Prof. Dr. K. Helmke, Prof. Dr. K.D. Hepp, Prof. Dr. W. Schepp (Städtisches Krankenhaus München-Bogenhausen) and their staff, whose cooperation made the investigation possible.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: D. J. H. Deeg.
Rights and permissions
About this article
Cite this article
Neubauer, A.B., Wahl, HW. & Bickel, H. Depressive symptoms as predictor of dementia versus continuous cognitive decline: a 3-year prospective study. Eur J Ageing 10, 37–48 (2013). https://doi.org/10.1007/s10433-012-0246-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10433-012-0246-4