Abstract
Immunoassay is one of the most widely used biomedical diagnostic methods due to its sensitivity and specificity. Microfluidic lab-on-a-chip technology has the advantages of portability, integration, and automation. The combination of these two technologies leads to a pathway for point-of-care diagnostics using the unprocessed samples such as the whole blood. This article reviews the recent advancement and the major development in the microfluidic-based whole-blood immunoassays. After a survey of the recent studies on microfluidic whole-blood immunoassays, an in-depth review about the detection methods that can be miniaturized and integrated in the immunoassay chips is provided. Point-of-care diagnostics applications require developing a fully integrated, disposable, low-cost, and handheld microfluidic device for the whole-blood immunoassay. In this regard, some comments and suggestions for future research are given.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
On-site detection of pathogenic infection from the human body liquids such as the whole blood is highly desirable, particularly at the resource-limited settings, because of the increasing demand for early diagnostics and rapid testing results. In general, most whole-blood tests are being performed at hospitals, medical laboratories, outpatient clinics, and emergency rooms. However, in the developing countries and some low-resource settings, the long testing time, the high cost and the large sample consumption are not acceptable. In order to solve these problems, Point-of-Care (POC) diagnostic technologies must meet certain requirements including portability, cost effectiveness and ease of use (Huckle 2008). POC diagnostics should be able to analyze small volumes of body fluids, e.g., blood, saliva and urine; and minimize the number of assay steps, such as sample preparation and washing processes. In addition, the cost of POC diagnosis devices should be significantly low (Huckle 2006). To be used in resource-limited settings, environmental conditions, such as insufficient water, high or low temperatures, humidity, and poor power supply should also be considered (Petti et al. 2006).
Immunoassay is one of the most widely used biomedical diagnostic methods. It is based on the specific binding of an antibody to an antigen (Wild 2008). Over the past 50 years, immunoassay technology has played a particularly important role in the diagnosis of body fluids. In general, this technique has two formats: heterogeneous and homogeneous immunoassays. In heterogeneous immunoassays, the antibody or antigen is immobilized on a solid substrate, while homogeneous immunoassays take place in the solution phase. Heterogeneous immunoassays are popular because they are easy to design, but they require a step of separating antigen or antibody from the samples and need to immobilize the antibody or antigen on the solid surface. Homogeneous immunoassays can often be run without a separation step. The sample and the antigen can be carried out simply by mixing in the solution. Immunoassay is well known thanks to ELISA (enzyme-linked immunosorbent assay) developed over 20 years ago (Engvall and Perlman 1971; Van Weeman and Schuurs 1971). Figure 1 shows the different types of ELISA. Although ELISA is an excellent method, it requires the sophisticated climate-controlled laboratory and highly trained personnel. A conventional immunoassay test needs at least several hours to complete because it is a multistage, labor-intensive process. Automation of immunoassay test generally requires a complex and cumbersome robotic technique for fluid handling, which is very expensive and not a practical tool for point of care testing.
In recent years, the rapid development of microfluidics based on the lab-on-a-chip technology lights a pathway for POC diagnostics. Microfluidic devices allow integration of multiple liquid handling processes required in diagnostic assays, such as pumping, metering, sampling, dispensing, and sequential loading and washing. These lab-on-a-chip solutions have been recognized as an opportunity to bring portable, accurate, and sensitive diagnostic tests to the POC diagnostics in low-resource settings as well as in the developing world (Chin et al. 2007; Yager et al. 2006; Weigl et al. 2003; Singer et al. 2007). It provides a very promising way to miniaturize immunoassays with added benefits such as portability, improved reaction kinetics, minimal reagent consumption, automation, and parallel processing (Zimmermann et al. 2005; Cho et al. 2006; Parsa et al. 2008). In order to obtain the quantitative results of immunoassay, the immunoassay chips can combine microfluidics with optical, electrical, and mechanical sensors in an integrative format (Herr et al. 2007; Morozov et al. 2007; Yacoub-George et al. 2007; Stevens et al. 2008).
Conventional immunoassay requires extracted and purified antibodies or antigens. A key challenge in POC diagnostics is to perform the test using the unprocessed samples such as the whole blood. Blood is one of the most important body fluids for many diseases diagnostics. A rapid whole-blood immunoassay device with the capacity to detect a variety of selected analytes would be greatly beneficial for a wide spectrum of point-of-care or public health applications. This review examines the status and the major development in the microfluidic-based whole-blood immunoassays. The first half of this review focuses on the microfluidic whole-blood immunoassays, with emphasis of how to deal with the whole-blood samples in the microfluidic chips. The second half concentrates on the detection methods that can be miniaturized and integrated in the immunoassay chips. Finally, some suggestions for future research are provided.
2 Microfluidic whole-blood immunoassay
A conventional immunoassay requires a separation step to obtain the purified blood plasma for detection. Therefore, the conventional immunoassays are rarely carried out with whole blood. In most cases, this separation step is additional to the assay. The plasma separation is performed typically using a centrifuge. Before doing so, an anticoagulant must be used to prevent the coagulation of the fresh blood. The disadvantages are obvious: expensive and bulky centrifuge device, large sample requirement, and time consumption. Hirsch et al. (2003, 2005) first introduced a simple rapid immunoassay capable of detecting analyte without any sample preparation using gold nanoshells. This method successfully detected the immunoglobulins in serum and in whole blood. However, there are some limitations to realize this method in the POC diagnostics: the difficulty of fabricating the gold nanoshell immunoconjugates; large reagent and sample consumption (e.g., 4.444 mL of antibody-nanoshells, 3.75 mL of the whole blood, 1.25 mL of the lysis buffer working solution, and an additional 6.25 mL of 100 mM PBS are needed); non-portability (a spectrometer and tubes are involved in the immunoassay). To overcome these limitations, microfluidic technology has been tested in the whole-blood immunoassay.
2.1 Diffusion-based whole-blood microfluidic immunoassay
An exploitation of the diffusion-based whole-blood immunoassay in the microfluidic laminar flow channel was reported by Yager’s group (Weigl and Yager 1999; Hatch et al. 2001; Hawkins et al 2002). In their study, they described a novel microfluidic immunoassay based on the diffusivity differences––the competitive diffusion immunoassay (DIA). The DIA was performed in a simple “T-sensor” which consists of two inlets, one outlet and a main microchannel (Fig. 2). One inlet contained the antibody. The other contained both labelled antigen and sample antigen. In the microfluidic laminar flow channel, large particles such as blood cells could not diffuse significantly within the time. Small particles such as H+, Na+, and small molecules diffused rapidly between streams. Therefore, the labelled antigen and the sample antigen diffused into the fluid stream, it randomly encountered the antibody and binds at a characteristic rate. The antibody–antigen conjugates accumulated in the center of the channel where antigen and antibody interdiffused. The accumulation of fluorescence in the interdiffusion zone could be quantified with a digital camera and microscope. In their experiments, the phenytoin was be used as the analyte, a typical small drug molecule in the blood sample. Removal of cells from blood samples was not necessary in the homogeneous microfluidic immunoassay. The detection limit of the phenytoin was 0.43 nM in their experiments. Recently, Hosokawa et al. (2007) demonstrated a homogeneous microfluidic immunoassay based on the diffusion principle for detecting the C-reactive protein which was an important biomarker in the human blood. They made use of the Y-shaped channel to carry out the sandwich immunoassay. The anti-CRP, the blocking solution, CRP sample, B-anti-CRP, F-SA, and B-anti-SA were injected into the microchip sequentially. The reagents of F-SA and B-anti-SA were used to improve the LOD by employing dendritic amplification (DA) methods. They achieved 0.15 pM for CRP with 0.5-μL sample consumption. Tachi et al. (2009) realized a homogeneous immunoassay for detecting the theophylline in serum based on the competitive diffusion immunoassay. The sample and fluorescence-labeled theophylline were introduced through different inlets and combined in a microchannel where anti-theophylline antibody was added. The fluorescent signal was detected by fluorescence polarization spectroscopy, and the quantitative analysis of theophylline was obtained near the therapeutic range (10–20 mg/mL) in 65 s. The diffusion-based whole-blood microfluidic immunoassay offered some clear advantages over conventional immunoassays: direct analysis of blood samples, the small sample and small reagent volumes, and less analysis time. However, it needs precise systems to get the accurate measurement because diffusive transport at the early stage is in the non-equilibrium state which may cause the error detection signal.
Diffusion immunoassay in a T-sensor. a Schematic of a diffusion immunoassay (DIA) implemented in the T-sensor. Reagents are pumped separately through syringe pump and meet at the junction. At this point, under laminar flow conditions, reagents flow side by side and mix only by diffusion. b Photograph of a microfluidic device used for testing (Source: Hatch et al. 2001)
2.2 Surface/beads-immobilized whole-blood microfluidic immunoassay
In the immunoassays, the attachment of the primary antibody/antigen to a solid support is important. Usually, in microfluidic chips, the antibody/antigen probes are coated on the microchannel surface or onto the surface of microparticles which are immobilized in the certain area of the microfluidic chip. By using this technique, a homogeneous immunoassay can be implemented on the microfluidic chip. Therefore, the separation of the blood cells and the plasma is eliminated. The analytes in the blood can bind with the antibody/antigen directly. The remaining blood cells can be flushed using the buffer solution. This can reduce the complexity of the chip design and simplify the operating steps. Lim et al. (2003) described an on-chip electrochemical flow immunoassay system with a multichannel matrix column which was functionally coated with cation-exchange resin and used for separation of immuno-complexes after a competitive binding event (Fig. 3). Based on different isoelectric points, antibody–antigen complexes were separated from free Fc-conjugated IgG antibody (Fc-IgG) using the multichanneled matrix column. The immunocomplexes were detected by electrochemical method in the eluent. Histamine concentration in the 200–2000 ng/mL range was measured in whole blood within 2 min. Hofmann et al. (2002) reported a microchip-based flow confinement method for rapid delivery of small sample volumes to sensor surfaces. A sample flow was joined with a perpendicular makeup flow of water or sample medium. Under laminar flow conditions, the makeup flow confined the sample flow into a thin layer above the sensing area and increased its velocity. Using this method, a high-affinity immunoassay was carried out on the microfluidic chip. Rabbit IgG was immobilized onto a silicon nitride waveguide and Cy5-labeled anti-rabbit IgG was hydrodynamically pumped over the immobilized zone. The binding event was monitored by fluorescence detection method. This flow confinement method is most suited for detecting the low analyte concentration without filtration in the raw sample such as blood. Stern et al. (2010) showed a microfluidic purification chip which simultaneously captured multiple biomarkers from row blood sample. When the blood sample flowed through the chip, specific biomarkers were captured by the antibodies which were immobilized on the surface of the chip. After washing and UV irradiation, the complexes were released and flowed into the nanosensor chip where the complexes bound with the second antibodies (Fig. 4). They showed specific and quantitative detection of two model cancer antigens from a 10-mL sample of whole blood in less than 20 min. Homogeneous immunoassay is a single step immunoassay with relatively poorer sensitivity and specificity. In the process of the homogeneous immunoassay, the solution containing sample molecules continues to pass through the reaction region. It is difficult for some antibodies and antigens to react without the incubation. This will cause a lower sensitivity and may give the false positive signal.
Schematic diagram of the on-chip-type electrochemical flow immunoassay system (Source: Lim et al. 2003)
Schematic of chip operation. a Primary antibodies are bound with a photocleavable crosslinker to the chip. A valve directs fluid flow exiting the chip to either a waste receptacle or the nanosensor chip. b Whole blood is injected into the chip with the valve set to the waste compartment. Biomarkers bind their cognate antibodies. c Washing and UV irradiation follow blood flow. During UV exposure, the antibody–antigen complexes are released into solution. d The valve is set to the nanosensor reservoir. The complexes bind the secondary antibodies on the nanowire surfaces (Source: Stern et al. 2010)
The microbead-based immobilization also offers a large surface area and improves the performance of the whole-blood microfluidic immunoassay. Moorthy et al. (2004) developed a microfluidic platform for detecting botulinum neurotoxin directly from the whole blood by using the sandwich immunoassay. Process steps such as sample preparation, mixing and incubation with reagents were carried out on the device. A porous filter was incorporated for filtering the blood cells. Biotinylated antibody was immobilized on avidin–agarose gel beads which were fixed in the microchip. The whole blood with toxoid sample passed through the filter and transported to the agarose beads. After the washing and incubation steps, the second antibody was introduced to the agarose beads. The color change of the agarose beads was monitored to quantify the amount of the sample. Yang et al. (2008) presented a new microfluidic flow cytometer integrated with several functions such as viral sample purification and detection by utilizing a magnetic bead-based microfluidic immunoassay. Using the sandwich immunoassay technology, target viruses in whole blood could be captured and separated by the antibody-conjugated magnetic beads which were fixed in the microchannel via an applied magnetic field, followed by a second set of fluorescent labeled antibodies for identifying the surface antigen of the target viruses. The dengue virus sample with a concentration of 103 PFU/ml was detected successfully by the developed system. A handheld device based on the optomagnetic technology for the sensitive detection of cardiac troponin I (cTnI) in a finger-prick blood sample was presented by Dittmer et al. (2010). A compact plastic disposable with on-board dry reagents and superparamagnetic nanoparticles were used in this device. A blood cell separation filter was added at the sample inlet and a 100-μm connecting tape was used to enable rapid capillary filling of the chamber with the generated plasma. In the one-step assay, all reaction processes were precisely controlled using electromagnets positioned above and below the microfluidic chip. Nanoparticle labels (500 nm) bound to the sensor surface via a sandwich immunoassays were detected using the optical technique of frustrated total internal reflection (Fig. 5). A limit of detection of 0.03 ng/mL cTnI was obtained. The use of microbeads as the solid support has been getting much attention for the whole-blood microfluidic immunoassay applications. However, using the microbeads also has some shortcomings in the microfluidic devices. For example, the microbeads could easily adhere onto the microchannel surface that limits the motion of the microbeads. The microbeads could also block the microchannels, reducing the flow rate and causing some detection problems such as scattering light.
a Schematic of the optomagnetic analyzer consists of the top and bottom magnets and the detection optics. b Picture of a functional handheld reader. c Picture of an assembled disposable cartridge. d f-TIR image of four spots of 200 μm diameter with magnetic nanoparticles bound to the sensor surface via an immunoassay. e Magnets show the assay processes in the reaction chamber: analyte binding by antibody-functionalized nanoparticles (top and bottom magnets off), nanoparticles binding to the sensor surface and magnetic removal of free and weakly bound nanoparticles (Source: Dittmer et al. 2010)
2.3 Separation-based whole-blood microfluidic immunoassay
In general, whole-blood microfluidic immunoassays require carrying out multiple functions on the microfluidic chip. The plasma separation is a key step in the whole-blood microfluidic immunoassays. In the whole-blood, plasma contains many proteins and biomarkers and is the major analyte. In order to eliminate the interference and non-specific binding event, the blood cells need to be removed from whole-blood samples. Thorslund and Bergquist (2006) reported a microsystem for on-chip sample preparation that was able to remove blood cells from whole blood (Fig. 6). The device consisted of a lid and a bottom substrate, both fabricated by PDMS. A polymeric membrane filter of 13-mm diameter was incorporated into the lid before irreversible bonding. Forty parallel microchannels underneath the membrane filter collected the filtrate and leaded it into the collection microchannel. Using this membrane filter, they successfully separated human plasma from the whole blood. Testosterone concentrations were measured with testosterone radio immunoassay (RIA). A microfluidic flow-through membrane immunoassay with on-card dry reagent storage was introduced by Stevens et al. (2008). The disposable assay card design consisted of a chamber holding the assay membrane, three upstream fluid lines (sample line, conjugate pad line, and bubble venting line) connecting to syringe pumps, and a downstream waste line. The most important component of this chip is a laser-cut porous membrane which held the anti-PfHRP2 IgM molecules and a fibrous conjugate pad which contained an anhydrous analyte label. For a sandwich immunoassay, the PfHRP2, a water-soluble protein, was passed through the membrane and captured by anti-PfHRP2 IgM, followed by a buffer wash to remove unbound sample. The analyte label was released and passed through the membrane, followed by a buffer wash to remove unbound label. The immunocomplexes were formed and measured. The system could achieve a detection limit in the sub-nanomolar range within 9 min. When combined with the upstream blood separation, it shows the potential for quantitative, multianalyte analysis of human blood samples. Lenshof et al. (2009) reported an acoustophoresis-based separation chip that prepared diagnostic plasma from whole blood and linked it to the porous silicon sandwich antibody microarray chip (Järås et al. 2008) for prostate specific antigen (PSA) detection. In their microfluidic chip, the ultrasonic standing wave (USW) combined with the laminar flow formed a band of concentrated blood cells in the center of the channel. The plasma distributed toward the periphery. By providing a trifurcated channel outlet, the clean plasma was allowed to exit through the side outlet. This acoustic separator had the capacity to sequentially remove the enriched blood cells and yielded high quality plasma of low cellular content. After that, the plasma with the PSA was introduced to a porous silicon microarray chip where the capture antibody H117 was immobilized. After the incubation and the washing steps, the FITC-labeled 2E9 monoclonal mouse anti-PSA antibody was bound with the conjugates to generate the fluorescent signal. PSA was detected via fluorescence readout without any signal amplification. The detection limit is 0.19 ng/mL. By combining USW microfluidics and microarray chip, an all microchip-based PSA detection from whole blood was obtained in a lab-on-a-chip configuration.
Diagram of the microsystem device. a The structure of the device. b Photograph of the final device. (Source: Thorslund and Bergquist 2006)
With the use of the membrane in the microfluidic immunoassay chip, separating the plasma from the blood is simple. However, the leakage of the blood must be considered when assembling the membrane into the chip. Furthermore, it is difficult to provide the continuous plasma separation by this method because of the blocking of the membrane. The acoustophoresis-based methods are generally difficult to process high hematocrit levels such as whole blood. Recently, a principle called the bifurcation law (Zweifach–Fung effect) is used in the blood plasma separation. It describes that erythrocytes have a tendency to travel into small blood vessels which has the higher flow rate leaving very few cells flowing into the lower flow rate vessel (Fung 1973; Schmid-Schonbein et al. 1980; Yen and Fung 1978). Based on this principle, Yang et al. (2006a, b; 2007) reported a microfluidic device for continuous blood plasma separation. Under a pressure difference, the whole blood flowed through a low-flow-resistance primary channel with high-resistance branch channels at right angles. As the flow resistance is higher in the branches than that in the primary channel, the plasma was skimmed into the branches and the remaining whole blood is directed toward a waste outlet. Based on Yang’s previous study, Fan et al. (2008) reported an integrated blood barcode chip (IBBCs) to detect a large panel of protein biomarkers in the whole blood (Fig. 7). The IBBCs consisted of two major components. One was the plasma separation part which was redesigned from the Yang’s previous report to obtain the pure plasma continuously. Another component is the DEAL (DNA-encoded antibody library) barcodes which were oriented perpendicular to the microfluidic plasma-skimming channels. When the plasma was skimmed into the channels, the proteins of interest were captured by the DNA-antibody conjugates in the assay zone where the DEAL barcodes were placed. After 10 min, a mixture of biotin-labeled detection antibodies for the entire proteins and the fluorescence Cy5-streptavidin conjugates were injected sequentially to complete the sandwich immunoassay. All the barcode array slides were scanned using a microarray scanner. In the same group, the similar research was also reported by Qin et al. (2009).
Design of an integrated blood barcode chip. a Plasma separating from a finger prick of blood. DEAL barcode arrays are patterned within the plasma-skimming channels for in situ protein measurements. b Schematics of DEAL barcode arrays. A, B, C indicate different DNA codes. The inset represents a barcode of protein biomarkers, which is read out using fluorescence detection. The green bar represents an alignment marker (Source: Fan et al. 2008)
2.4 Centrifugal-based whole-blood microfluidic immunoassay
The high-speed rotation on a compact disk generates a strong centrifugal force which can be utilized as a microfluidic pump. In recent years, the microfluidic compact disk (CD) becomes a promising platform for POC applications by integrating many functions such as sample/reagent transport, mixing, separation and detection. For whole-blood microfluidic immunoassay, the plasma-cell separation is a necessary and crucial step which can easily be realized by the centrifugal force on a microfluidic disk. Figure 8 shows a continuous blood flow in the separation structure on a microfluidic disk. First, the metering chamber was filled by capillary force with a droplet of human whole blood while the disk was stationary. The sample was metered under a moderate rotation frequency. Then, with a high rotation frequency, sedimentation was started through the drain channel into the decant chamber. Under the centrifugal force, the blood cells was separated and stored in the decant chamber. The purified plasma overflowed into a subsequent reservoir where it was available for further processing. The separation time of this continuous centrifugation was controlled by the flow resistance of the drain channel and the spinning frequency (Steigert et al. 2005). In Ducrée’s group (Ducrée et al. 2007; Grumann et al. 2005; Riegger et al. 2006; Steigert et al. 2006), they presented the novel centrifugal microfluidic platform enabling a fast colorimetric alcohol assay from a single droplet of whole blood and first time demonstrated the feasibility of color-multiplexed fluorescence immunoassays on such a platform. The core of their setup was a microstructured disk with a round mixing chamber rotating on a macroscopic drive unit. This centrifugal microfluidic platform is suitable for the whole-blood immunoassay, because it could accomplish sedimentation, batch-mode mixing, frequency-dependent online flow control, and optical read-out. By the centrifugal microfluidic technologies, Ko’s group (Cho et al. 2007; Lee et al. 2009) demonstrated a portable, disk-based, and fully automated microfluidic immunoassay system to test infectious diseases from whole blood (Fig. 9). The centrifugal microfluidic platform consisted of plasma separation channels and different chambers such as washing buffer storage chamber, stopping solution chamber, mixing chamber, waste chamber, and detection chamber. Before doing the sandwich immunoassay on the disk, HRP-conjugated detection antigen and polystyrene beads coated with capture antigen were preloaded in the mixing chamber. The blood plasma with the Anti-HBs was separated by the centrifugal force and transferred into the mixing chamber. After the incubation and washing step, the HBsAg and Anti-HBs were detected via the absorbance detection method. The detection limit of HBsAg and Anti-HBs were 0.51 ng/mL and 8.6 mIU/mL, respectively. Similar research was also reported by Pugia et al. (2005).
a Continuous flow scheme in the separation structure. b The photograph of the decant chamber after sedimentation (Source: Steigert et al. 2005)
a Disk design showing the detailed microfluidic layout and functions. b–g Schematic of the reaction principle of the ELISA on a disk (Source: Lee et al. 2009)
3 Detection in microfluidic immunoassays
For most immunoassays, the detection depends on the use of an analytical reagent that is associated with a detectable label. The commonly used labels include radioactive elements used in radioimmunoassay (RIA) (Yalow and Berson 1960; Nobel Prize home page accessed June 2005; Ekins 1960; Miles and Hales 1968); enzymes used in enzyme-linked immunoassay (EIA) (Engvall and Perlmann 1971; Van Weemen and Schuurs 1971; Ljungstrom et al. 1974; Engvall 1977; Uotila et al. 1981; Schuurs and Van Weemen 1980); particles such as latex, magnetic, gold, and silver used in bead-based immunoassay (Verpoorte 2003; Qiu et al. 2009; Christodoulides et al. 2002; Sato et al. 2000, 2001, 2002; Pereira et al. 2010a) and others. According to the label used, immunoassay detection methods can be classified as optical detection methods and non-optical detection methods. Some non-optical detection methods are uniquely available for microfluidic-based immunoassay. In the following, we will focus on the most common detection techniques used for microfluidic immunoassays in recent years.
3.1 Optical detection
3.1.1 Fluorescence detection
The most commonly observed form of optical detection is fluorescence, because of its high sensitivity and the ease of integrating a label. Fluorescence is the emission of certain wavelength of visible light from a substance by the absorption of an excitation light of different wavelength. Laser-induced fluorescence (LIF) has a high sensitivity and fast response. Figure 10 shows the basic principle of the of LIF method. A microscope focuses on the microchannel and connects to a charge coupled device (CCD) camera or photomultiplier tube. The excitation light is provided by a laser system. It passes through a beam splitter and is focused on the detection area. The fluorescence emission returns through the same beam splitter and is reflected towards the detection system. In recent years, the LIF method is widely applied to the microfluidic immunoassays. Kong et al. (2009) reported an integrated microfluidic system combining with microvalves and micropumps for the clenbuterol immunoassay via the LIF detection method. This system consists of an integrated microchip and a linear confocal LIF scanner. The microfluidic chip is composed of three layers: a fluidic channel layer, a PDMS membrane layer, and a pneumatic control layer (Fig. 11). The limit of detection of the clenbuterol was 0.088 ng/mL. Darain et al. (2009a, b) demonstrated a simple microfluidic immunoassay based on polystyrene (PS) substrate for the detection of horse IgG and myoglobin by using the fluorescence detection method. The detection limit of the horse IgG and myoglobin was 0.71 μg/mL and 16 ng/mL, respectively. Table 1 summarizes the applications of the fluorescence detection method in the microfluidic immunoassays. It should be noted that all parts of the fluorescence setup, such as the lens, the excitation source, and detection device, can be miniaturized. The entire device can be made portable. Herr and Anup (2007) and Herr and Singh (2007) developed a portable device for detection of potential biomarkers of periodontal disease in saliva. The microfluidic chip was integrated with miniaturized electronics, optical elements (such as diode lasers), fluid-handling components, and data acquisition software (Fig. 12). This device could perform rapid microfluidic chip-based immunoassays (<3–10 min) with low sample volume requirements and appreciable sensitivity (nM–pM).
a Layout of the integrated microfluidic device for clenbuterol immunoassay. b Photograph of the prototype microfluidic device. c Cross-sectional view of microvalves on chip. d Scheme of the optical configuration of the confocal LIF scanning system (Source: Kong et al. 2009)
Image of IMPOD with hardware components. Inset shows glass microdevice used in performing immunoassays (Source: Herr and Singh 2007)
Another type of the fluorescence detection used in microfluidic immunoassay applications is fluorescence polarization (FP) which detects the change in anisotropy caused by the slower rotation of a free label. FP gives a direct and nearly instantaneous measure of a tracer’s bound/free ratio, even in the presence of free tracer. Figure 13 illustrates the FP principle. A single-plane fluorescence polarization light can be generated by installing two polarizing filters in the light paths of both excitation and emission in a fluorescent system. The intensity of FP light is proportional to the size of the fluorescent molecules and inversely proportional to the rotating speed of the molecules. In the solution, the rotation of the small molecules is very rapid, but the larger molecules become slower. Therefore, in an immunoassay, the emission light of the fluorescent-labeled small molecules is depolarized when the molecules are excited. However, when the fluorescent-labeled small molecules are bound to the antigen/antibody, the emitted light of the conjugates is obviously less depolarized due to the larger mass. Difference between these states is dependent on the number of bound molecules and the binding constant or affinity constant (Kakehi et al. 2001). Yadavalli and Pishko (2004) demonstrated that fluorescence polarization can be used to reliably and accurately study binding events and detect analytes in microfluidic devices. A tetramethylrhodamine isothiocyanate (TRITC) labeled antibody was used to detect the polyaromatic hydrocarbon pyrene at 10–40 nmol. Tachi et al. (2009) reported a microfluidic FPIA system composed of a microfluidic chip, a laser, a CCD camera, and an optical microscope with two specially installed polarizers (one fixed and one rotatable). Using this system, they successfully carried out a quantitative analysis of theophylline in serum near the therapeutic range in 65 s.
a Illustration of a fluorescence polarization apparatus. b Principle of the assay of binding reaction using fluorescence polarization (Source: Kakehi et al. 2001)
3.1.2 Chemiluminescence detection
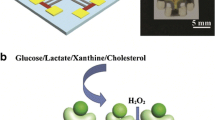
Chemiluminescence (CL) is another excellent optical detection method in microfluidic immunoassays. CL is the light produced by a chemical reaction. The CL intensity is directly proportional to the concentration of a limiting reactant involved in the CL reaction. As a principle of the CL, reactants A and B react with an excited intermediate to form a product and emit the light which can be detected and analyzed by an optical detection system (Fig. 14). The advantage of this technique is that the excitation light instrumentation is not required. Because of this advantage, the background interference can be eliminated. Yang et al. (2009) demonstrated a microfluidic chip integrated with pneumatic micropumps, micro-valves and vortex-type micromixers for C-reactive protein (CRP) measurement. The magnetic beads with CRP-specific DNA aptamers and bio-samples with CRP were placed in the reaction chamber. The target CRP was captured by the magnetic beads and the complex was attracted to the bottom of the microchannel using a magnet. After washing, the Anti-CRP antibody labeled with acridinium ester was added and interacted with the target CRP. Finally, a developer (H2O2) was added for CL. The CL light signal was measured by using a luminometer. The entire reaction time is less than 25 min and the detection limit of the CRP concentration was 0.0125 mg/L. Mello’s group (Wang et al. 2009, 2007) reported a microfluidic chip integrated with the thin-film organic photodiodes (OPDs) for antioxidant capacity screening (Fig. 15). The PDMS microchip comprised two inlets, mixing channel, a circular detection chamber and an outlet. The PO-CL reagent, dye, catalyst, hydrogen peroxide and sample were injected into the microchip and reacted at the detecting zone. In this study, the CL was based on hydrogen peroxide-induced oxidation of an aryl oxalate ester which resulted in the formation of an electronically excited intermediate. When the fluorophore was added, the energy transferred to the fluorophore with concomitant emission of light. However, during the reaction, antioxidants scavenged hydrogen peroxide and resulted in a decrease in CL emission. The OPDs detectors were applied to detect the CL signal for determining antioxidant capacity. The whole detection system can be portable and has wider applications for CL-based point-of-care diagnostic tests. Huang et al. (2009) reported a rapid and sensitive CL microfluidic immunoassay system based on super-paramagnetic microbeads for determination of alpha-fetoprotein (AFP). In their system, the microfluidic chip was fabricated by the CO2 laser. Super-paramagnetic microbeads coated with AFP antibody were immobilized in the reaction chamber by electromagnetism. After loading the sample and the HRP-labeled anti-AFP antibody, the sandwich immunoassay was carried out. Then, the Luminol and H2O2 were loaded into the reaction chamber to generate the CL signal. With this system they performed AFP analysis in 20 min and the detection limit is 0.23 ng/mL.
Schematic of the experimental set-up for on-chip antioxidant capacity screening (Source: Wang et al. 2009)
3.1.3 Thermal lens microscope
Thermal lens microscope (TLM) is a very sensitive detection method. Compared with the fluorescence detection method, the detection limit can reach zeptomole to yoctomole levels under the perfect conditions (Uchiyama et al. 2000). It is good at detecting the nonfluorescent samples. Microfluidic immunoassay needs very high sensitive detector to analyze the very small volume of the analyte. Therefore, TLM is a powerful tool for the microfluidic immunoassay. TLM is implemented by using a laser microscope. Two coaxial laser beams are introduced into a liquid sample under an optical microscope. The wavelength of the excitation beam is selected to coincide with an absorption band of the analyte. The wavelength of the probe beam is chosen so that the sample solution has no absorption (Fig. 16). The temperature of the analyte in the confocal region increases because the heat is yielded by absorbing the excitation beam. For most solutions, the refractive index (RI) decreases with the high temperature. According to the proportional relationship among the laser intensity, the temperature distribution and the RI distribution, the RI distribution becomes a nearly Gaussian distribution because the laser intensity profile is nearly a Gaussian distribution. This phenomenon forms a concave lens and is called “thermal lens effect.” The degree of the thermal lens which is measured by the probe beam is proportional to the number of analyte molecules in the confocal region (Kitamori et al. 2004). For example, Henares et al. (2007) reported a multiple micro ELISA system to simultaneously determine human, goat, and chicken IgGs by combining a capillary-assembled microchip and TLM detection method. The microchip had a PDMS plate with the lattice microchannel network. The plugged capillaries, the valving capillaries and the immuno-reaction capillaries were embedded into the microchannel network to form a flow controlling and immune reaction system. A Peltier device was used to open or close the valve. The thermal lens detector focused on the region of the immuno-reaction capillaries to detect the IgGs. The detection limits of 0.1 ng/mL IgGs (human, goat, chicken) were obtained in 30 min. Ihara et al. (2010) developed a novel detection system that combined the merits of open-sandwich enzyme-linked immunoadsorbent assay, a microfluidic sensor chip system and a sensitive thermal lens microscope. In their study, OS-ELISA was performed in a microfluidic channel in which polystyrene microbeads were packed using an automated ELISA system. The microfluidic channel with a dam structure was used for retaining the microbeads (Fig. 17). A small amount of the BGP, a biomarker for bone metabolism, was quantified by utilizing the thermal lens microscope. In a short analysis time (12 min), detection limits of the total BGP-C concentrations in bovine and human serum samples were 17 and 10 nM, respectively.
The micro-ELISA system. a A glass chip integrated with microfluidic channels was used for the OS-ELISA reaction. b–e Polystyrene beads with immobilized MBP-VL were introduced and stored between a dam structure and the three-way junction. Extra beads were flushed away. The reagents were introduced into the microchip to form an immuno-complex on the beads. After washing, the substrates were applied, and dye molecules produced by the enzyme reaction were detected by a TLM downstream of the dam structure. The microbeads after each assay were flushed by an inversed flow (Source: Ihara et al. 2010)
3.1.4 Surface plasmon resonance
Another detection strategy that widely used in optical microfluidic immunoassay is Surface Plasmon Resonance (SPR). A landmark article involved in the SPR was published by Kretschmann in (1971). The “Kretschmann structure” lays a solid foundation for the SPR sensor. The operation principle and experimental configurations of SPR immunosensors have been described in several review articles (Shankaran et al. 2007; Luppa et al. 2001; Cooper 2002; Karlsson 2004; Mullett et al. 2000). Briefly, when a polarized light hits a prism covered with a thin film of metal at a specific (resonance) angle, SPR occurs. SPR effect is sensitive to the binding of analyte because the increase in mass causes a proportional increase in the refractive index at the interface between a thin metal film and an ambient medium. For an immunoassay, before an antigen binding to an immobilized antibody, the refractive index of the prism is constant. After the binding event, the refractive index was changed. In this way, it is possible to monitor the biomolecular interaction information on the metal film. Therefore, SPR provides a non-invasive, label-free approach for detecting the concentration of analytes, kinetics, and affinity in real time. Figure 18 shows the scheme of a typical experimental configuration for SPR instrumentation. The transduction surface is usually a thin gold-film (50–100 nm) on a glass slide, optically coupled to a glass prism through a refractive index matching oil. Because of several advantages including high sensitivity, specificity and rapid response time, a great variety of SPR-based immunosensors have been developed since its introduction in the 1990s. Recently, Estmer Nilsson et al. (2010) introduced a new approach using SPR for accurate quantification of influenza virus. Recombinant HA proteins (A/H1N1, A/H3N2 and B respectively) were immobilized on the dextran matrix of a sensor chip. By using a microfluidic system for reagents handling, a binding event occurred on the sensor surface. A change in SPR response was detected. In their study, the calibration curve range was 0.5–10 μg/mL and the limit of detection was estimated as <0.5 μg/mL for all three analytes. Lee et al. (2007) developed a microfluidic system integrated with 2-D SPR phase imaging system for microarray immunoassays. In this study, the microfluidic device was composed of an arrayed sample/reagent delivering module and a micro-temperature control module. Using this system, the interaction of anti-rabbit IgG and IgG was successfully detected. A detection limit of 10−4 mg/mL for IgG was obtained. Liu and DafuCui (2010) developed a compact microfluidic-based biosensor flow cell for SPR imaging immunoassay. This biosensor flow cell consisted of a “hard” plastic substrate (PMMA) coated with a SiO2 thin film which was used as an adhesion intermediate layer and a “soft” PDMS microfluidic layer which adhered to the SPR array chip. An immunoassay was successfully carried out on the microchip and the limits of detection of sulfamethoxazole and sulfamethazine were obtained as 3.5 and 0.6 ng/mL, respectively. Krishnamoorthy et al. (2009, 2010) used a surface Plasmon resonance imaging (iSPR) label-free biosensor to detect surface binding events in a microchip which used electrokinetic flow focusing to selectively deliver samples over an array (Fig. 19). By combining the electroosmotic flow (EOF) for sample transport and the electrokinetic focusing (EKF) for sample guiding, an advantage of this approach was the ability to direct a single analyte to a specific ligand location in the microarray which could facilitate analysis parallelization. The SPR signal was changed and measured during sample focusing. In their study, they successfully analyzed the binding kinetics and affinity during the biomolecular interaction. In addition, Many commercial SPR systems have been introduced by different companies with various options and resolutions; BIAcore (Uppsala, Sweden), Nippon Laser Electronics (Hokkaido, Japan), Affinity sensors (Franklin, MA), IBIS technologies (Enschede, The Netherlands), Texas Instruments (Dallas, TX), Moritex (Japan), Aviv (Lakewood, NJ), etc. (Shankaran and Miura 2007). SPR detection is a highly sensitive, labeling-free and real-time response detection method. However, the structure of the SPR device is complex, and a layer of metal (such as gold) must be deposited on the microchip. In addition, when doing the immunoassay, the impact of the change of the temperature must be considered. Because the refractive index of the solution is sensitive to the change of the temperature, the accuracy of the detection may be reduced.
a Microarray of gold iSPR sensing islands. b glass-PDMS microfluidic chip. c The iSPR interface module with chip fixture with integrated platinum electrodes. d Electrical circuit (Source: Krishnamoorthy et al. 2010)
3.1.5 Absorbance detection
UV/visible absorption spectroscopy is a general optic technique. When a beam of light passes through the sample, the light absorption occurs because of the atoms or molecules taking away the energy from the light. It means that the transmission of light is reduced when passing through a sample. In general, the absorbance of a sample is directly proportional to the optical path length of the sample holder and the concentration of the sample. Absorbance detection is used in macroscale analytical chemistry and laboratory diagnostics because of its simplicity and acceptable sensitivity. However, in the microscale, the absorbance of a sample is constant. If the optical path length is shortened greatly, the concentration of the sample must be high enough to be detected. The short optical path length limits the applications of this method because of micron- or nano-sized channel. Laiwattanapaisal et al. (2009) performed an immunoassay on a portable microfluidic device to measure urinary albumin by monitoring the absorbance changes. For increasing the sensitivity of absorbance detection in a microfluidic chip, the PDMS chip was composed of two layers. The upper layer was a 2-mm thick PDMS containing the channel structure. A modified flow cell made from a polystyrene cuvette with a 1-cm path length, and a total volume of 90 μL was incorporated into the lower, 6-mm thick PDMS layer. The optical path length was increased significantly in this way. With their proposed system, a calibration curve which was linear up to 10 mg/L, with a detection limit of 0.81 mg/L was obtained. Lee et al. (2009) developed a portable, disk-based, and fully automated enzyme-linked immuno-sorbent assay (ELISA) system to test infectious diseases from whole blood. In their study, a portable analyzer is equipped with an optical detection module to measure the absorbances at 450 and 630 nm to conduct the absorbance detection. Two photodiodes and the corresponding LEDs (450 and 630 nm) were used. The measured signal was amplified by a trans-impedance amplifier and digitized by an analog-to-digital converter. The limit of detection of Anti-HBs tests is 8.6 mIU/mL.
3.2 Non-optical detection
3.2.1 Electrochemical detection
Electrochemistry-based methods have played a major role in the microfluidic immunoassays. The electrochemical detection can be used to measure the concentration of the analyte by converting the analyte’s chemical signal into the electrical signal via the electrodes. According to the principle of the electrochemical detection method, there are three basic categories of the electrochemical techniques: amperometry, potentiometry and conductometry.
Amperometric detects the current signal generated by the redox reaction on the electrode. A three-electrode amperometric electrochemical concept is shown in Fig. 20. The detecting sensor is composed of three electrodes (working electrode, reference electrode and auxiliary electrode). A polarizable electrode is used for the working electrode on which an electrochemical reaction takes place. The reference electrode is a potential standard to supply a constant potential for introducing the electrochemical reaction on the working electrode. When a certain potential is applied to the working and the reference electrode, the redox reaction occurs. The reaction generates the current and can be measured between the working electrode and the auxiliary electrode. The current is proportional to the concentration of the analyte (Bard and Faulkner 2001). Amperometric approach is a simple technique. Miniaturization and integration can be easily achieved by creating a three-electrode system in the microfluidic chip. Recently, Yoo et al. (2009) demonstrated a microfluidic chip-based electrochemical immunoassay for rapid and quantitative detection of urinary hippuric acid (HA) in human urine (Fig. 21). In their study, all the complicated HA detection processes were integrated on a single microfluidic system. The metal three-electrode layer was patterned and deposited by chemical etching process on a glass slide. A PDMS microfluidic channel was bonded on this glass. It had a polybead reserving chamber (PRC) which was used to store beads coated with anti-HA antibody, a detection chamber, and a dam which was used to prevent bead spillover. For the electrochemical immunoassay, antigens (HA and Fc-Lys-HA) were injected into the microfluidic channel and competitively bound with the antibody (anti-HA) coated on the beads. After the reaction, the unbound antigens passed through the dam and entered into the detection chamber. The unbound Fc-Lys-HA caused the redox reaction on the electrode and the change of the current which was correlated with the HA concentration that was measured. They could detect the HA concentration in the range of 0–40 mg/mL. Table 2 summarizes the applications of the amperometric detection approach in the microfluidic immunoassays in recent years.
a Schematic diagram of the microfluidic immunoassay system. b The chamber holding the polybeads. c A photograph of the immunoassay microchip (Source: Yoo et al. 2009)
Using the micromachining technology, the electrodes are easily miniaturized. The sizes of the electrodes are commonly on the order of micrometer and the nanometer sizes have also been achieved. Therefore, the electrochemical detection approach can be integrated into the microfluidic immunoassay systems where the compactness and the portability are important. Chen and Lindner (2009) reported a passive pump-driven microfluidic system integrated with microfabricated electrodes as electrochemical sensors to detect the analyte of the hexacyanoferrate (II) (Fig. 22). The detection limit is smaller than 3 × 10−1 M. Liu et al. (2009a) developed a handheld system for detection of urinary proteins. Their system was composed of a control circuit, an electromagnetic valve, an air compressor, and a microfluidic chip which was integrated with a microfluidic control module and a micro-electrochemical module. The microfluidic control module consisted of a two-way, spiral-shape micropump which could transport the urine samples to the sensing regions. The electrochemical sensing module had three sensing electrodes. The detection limits of the lysozyme and albumin measurement were experimentally found to be 0.1 ppm.
a Photograph of a glass slide with three electrochemical cells. b Schematic representation of the reference (ER), interdigitated working (Ew), and counter electrodes (EA) (Source: Chen and Lindner 2009)
Potentiometry is used to determine the analytical concentration by detecting the electrical potential of an electrode. It consists of an ion-selective electrode and a reference electrode. The voltage difference between the ion-selective electrode and the reference electrode is measured as the signal. The relationship between the ion-selective electrode potential and the ion concentration of the analyte is expressed by the Nernst equation. The potential is proportional to the logarithm of the ion activity. Therefore, the ion-selective electrode must use ion-selective membranes to achieve charge separation between the sample and the electrode surface. Chumbimuni-Torres et al. (2006) demonstrated for the first time a polymer-membrane-based potentiometric method for nanoparticle-based protein detection. A silver ion-selective electrode (ISE) was used as an effective transducer for sandwich immunoassays. The target mouse IgG antigen was captured by the primary anti-mouse IgG antibody-modified gold substrate. The immunocomplex captured the gold nanoparticles labelled the secondary anti-mouse IgG antibody. After that, the catalytic deposition of silver on the conjugated Au nanoparticles was carried out to enhance the mouse IgG signal. The precipitated silver was oxidatively dissolved with hydrogen peroxide to yield electrolyte backgrounds for the potentiometric detection of the released silver ions with the ISE. They obtained a detection limit of around 12.5 pmol of IgG in the 50 μL sample.
Conductometric detection approach depends on the difference of the electrical conductivity between the background solution and the analyte. Conductometric detection is performed in two modes either with or without direct contact of the sensing electrodes with the background solution and the sample components. In general, the detection limit of this approach can reach 10−6–10−8 mol/L. The structure of the conductometric detection is simple: only a pair of electrodes is necessary. This simple structure facilitates miniaturization and integration. Detection based on the conductometry has been used in immunoassay systems for food-borne pathogens (with the detection limits of the Salmonella, E.coli O157:H7, and E.coli biosensors being 8.39 ± 0.6, 7.9 ± 0.3, and 7.59 ± 0.3 CFU/mL, respectively) (Muhammad-Tahir and Alocilja 2003), hepatitis B surface antigen (the detection limit of HBsAg is 0.01 ng/mL.) (Liu et al. 2009b), interleukin-6 (the detection limit is 5 pg/mL.) (Liang et al. 2009), and Escherichia coli (the detection limit is 0.5 CFU/mL) (Hnaiein et al. 2008).
Amperometric detection method has some advantages including simple, low background noise. It is the most popular electrochemical detection method in the microfluidic immunoassay system. However, it is not the universal method. It requires that the analyte has the electrochemical activity; otherwise some additional substances which have the electrochemical activity must be introduced to the immunoassay system for the indirect detection. Potentiometric detection method has the specificity because it uses the ion-selective membrane to achieve charge separation. However, the selective membrane is hard to integrate into the microfluidic system, which greatly limits the application of this method in the microfluidic immunoassay. Conductometric detection method is a universal detection method. However, it lacks the specificity. According to the principle, the conductivity between the background solution and the analyte must be sufficiently different. If there are two kinds of the analytes which have the similar conductivity, then this method cannot distinguish them.
Impedimetric detection method is the similar to the Amperometric or conductometric detection method. Usually, it uses either the two-electrode or the three-electrode concept. The difference between them is that the AC is used in the impedimetric detection. Compared with the amperometric or conductometric detection method, the electrolysis of the electrode can be eliminated by using the AC. In a microfluidic immunoassay, with the antibody–antigen interaction, the variation of the impedance can be easily measured by an impedimetric analyzer. However, like the conductometric detection method, the sensitivity depends on the difference of the impedance between the background and the analyte. Madhukar Varshney and Steve Tung et al. (Varshney et al. 2007) demonstrated a microfluidic flow cell integrated a label-free impedance biosensor for the direct detection of Escherichia coli O157:H7 in food samples. Magnetic nanoparticle-antibody conjugates (MNAC) were embedded in the microfluidic flow cell to capture the bacterial cells. The microelectrodes were coated on the microfluidic chip to form the impedance biosensor. The impedance changes were recorded by an impedance analyzer during the immune reaction. In their study, 1.6 × 102 cells could be concentrated from a sample volume of 5 mL, with a detection limit of 8.4 × 104 cfu/mL. In Lin’s group (Yeh et al. 2009; Kuei-Ling et al. 2009), they developed a new, simple and sensitive immunoassay that used the impedance variation caused by silver nanoparticles (AgNPs) coated with an antibody. In their study, the electro-microchip was composed of the two parallel gold electrodes and an immuno-reaction well. The first antibodies were immobilized on the glass slides and the test antigen, the washing buffer, the PBT and the silver-conjugated second antibodies were introduced into the microchip sequentially. The AgNPs made short circuit between two electrodes and decreased the impedance. The variation of the impedance was measured during the immune reaction. The antigen detection limit is 10 ng/mL.
3.2.2 Quartz crystal microbalance
When applied the electrical field on the quartz crystal, it produces the mechanical deformation. Conversely, when applied the mechanical stress on the quartz crystal, it generates the electrical field. This phenomenon is called “piezoelectric effect.” The quartz crystal microbalance (QCM), also called “micro weighing instrument” is a sensitive mass microbalance based on the piezoelectric effect for measuring the change of the mass on a surface and works well without using any label. The detection limit of this method is up to 10−13 g (Mecea 2005). Michalzik et al. (2005) and Rabe et al. (2000) demonstrated a miniaturized system for the determination of protein A by integrating a QCM sensor and a PDMS-based microfluidic cell. In their study, the AT-cut quartz with the gold electrodes was used to form the quartz resonator. The PDMS flow cell was bonded to the quartz surface. The protein A was immobilized on the gold electrode. The anti-protein was introduced into the flow cell and bound with the protein A. The frequency shift was monitored by a frequency and the measured values were recorded online with software. The detection limit for protein A is 1 mg/mL. Recently, Frisk et al. (2008) reported a novel microsystem which absorbed airborne narcotics molecules and performed a liquid assay using an integrated quartz crystal microbalance (QCM). In this study, the microsystem consisted of four parts. A quartz crystal fixed to a silicon chip and covered by a protective polymer cap by using double-sided vertically conductive adhesive foil (VCAF). The silicon chip gave rigid support to all device parts and supplied microchannels for transport of buffer liquid. It defined a robust air–liquid interface where airborne molecules could become absorbed into the liquid. The anisotropically conductive property of the foil (VCAF) provided electrical connection between the silicon chip and the QCM, and electrical isolation to the rest of the system. The polymer cap gave protection to the QCM from external influences without making any mechanical contact to it. The quartz crystal was a shear mode electromechanical oscillator, with the resonance frequency dependent on the mass of the material attached to its surface (Fig. 23). The microsystem was based on a QCM with a competitive immunoassay. They successfully measured 100–200 ng of narcotics samples with a sensitivity ranging from 6 to 20 ng Hz−1. In the immunoassay, the QCM has been used for detecting the different analytes including C-reactive protein (the detection limit is 0.13 ng/mL) (Kim et al. 2009), prostate specific antigen (the detection limit is 0.29 ng/mL) (Uludag and Tothill 2010). The QCM is a label-free detection method which has a potential to be widely used in the microfluidic immunoassays. It offers some advantages including high sensitivity, real-time readout, and low cost. In addition, the QCM not only can detect the mass changes of the analyte but also can provide the structure information of the analyte. However, one of the biggest challenges for the development of QCM immunosensor devices is how to coat the analyte on the detection surface evenly; otherwise it is hard to obtain the accurate result and the repeatability.
a Schematic cross-sectional (top) and top view (down) of the microsystem. b Exploded to scale view of the designed four-component system: the silicon substrate, the VCAF, the quartz crystal, and the protective polymer cap. c Front and backside pictures of two devices. The QCM crystal is visible through the polymer backside cover (Source: Frisk et al. 2008)
4 Summary
The whole-blood microfluidic immunoassay plays an important role in POC medical diagnostics because of the possibilities for miniaturization, integration, and automation. With the development of the microfabrication technology, the new materials, the surface modification methods, the antigen/antibody immobilization methods, and the detection approaches, better microfluidic immunoassay chip technology can be developed in the near future. In general, the applications of the whole-blood microfluidic immunoassay require that the device must be inexpensive, fast, and sensitive. In the future, the devices need to decrease the size and integrate multiple functions. The on-chip detection strategies are especially important because the detection volume or area is very small in the microfluidic immunoassay. To achieve these goals, research is required in the following fields:
-
Surface modification and immobilization: A most crucial problem is the reagents nonspecific adsorption or nonspecific binding, especially in the whole-blood environment where the blood consists of multiple biological components. While trying to increase the sensitivity of the signal detector, the efforts could be destroyed by the nonspecific adsorption which can create a background noise (and even false positive) that determines the detection limit for an immunoassay. So far, blocking buffers have been used to stop the nonspecific adsorption or binding. However, to some extent, it also can stop the specific binding, and decreases the detection limit. Unstable immobilization of antigen or antibody is another problem that also directly affects the detection limit. In a microfluidic immunoassay chip, the antibody/antigen usually is mobilized on the surface of the channel or the substrate such as glass and microbeads. The binding constants values are different with the use of different materials. Improved surface chemistry is needed to solve these problems.
-
Sample extraction: Owing to the complexity and the low amount of analytes in the whole-blood, plasma extraction steps are often required in the microfluidic immunoassay such as removing the blood cells. Micro/nanoparticles and magnetic beads have been widely used in the whole-blood immunoassay. With a high surface area and ease of manipulation, these beads are expected to provide a promising method for the homogenous immunoassay without separation the whole blood. For heterogeneous immunoassay, currently, the commercial membrane filters are used in the microfluidic device to separate the plasma from the whole blood. There are other physical methods that can be used to realize the separation. Further study is required to find simple, on-chip methods to increase the efficiency of the separation.
-
Transporting liquids: This is a key step in the whole-blood microfluidic immunoassay device. The immunoassay involves multiple steps of loading different reagents and washing processes. In microfluidic immunoassay, the liquid is typically introduced by pressure-, electrokinetic-, or capillary- driven flow. In this review, most of the cases utilize the pressure-driven flow, which is generated by a syringe pump producing positive/negative pressure to push/pull the liquid. However, using the pressure-driven flow, it is difficult to integrate the bulking pumps, tubing and valves in a POC device. In some devices, electrokinetic flow is used to transport liquids and control the on-chip fluidic processes, because of the ease of automation and no moving parts (Hu et al. 2005, 2007; Xiang et al. 2006; Gao et al. 2005a, b). Centrifugal-based microfluidic chips are a good choice for POC immunoassay applications.
-
Detection: In general, the detection system in the POC microfluidic immunoassay devices must have high sensitivity, high response time, and miniature size. Currently, the detection systems for the whole-blood microfluidic immunoassay are usually bulky and expensive. It will be very difficult to integrate the detection system into a portable device if the detection system requires microscope, power supply, laser, and pump.
Optical detection still is the most powerful technique for analysis in microfluidic immunoassays. Speaking in general, fluorescence detection method is the most popular optical method for quantifying analyte in the microfluidic immunoassays systems. It has high sensitivity (the detection limit is from 10−9 mol/L to 10−13 mol/L), high response time and high selectivity due to fluorescent labeling techniques. The key to get the high qualitative fluorescent signal is to minimize the background light as much as possible. Therefore, material selection and sample purification are very important. Profiting from the laser diode and the miniaturized CCD sensor, fluorescence detection method can be easily integrated and miniaturized into a portable microfluidic immunoassay device. Recently, LEDs (Seo and Lee 2003, 2004; Chediak et al. 2004; Pais et al. 2008) as an excitation light and COMS image sensors (Schmidt et al. 2007) are used for fluorescence detection to decrease the cost. They may be developed into a cost-effective way of detection in the microfluidic immunoassay. The CL detection method is generally acknowledged to be a highly sensitive method which can be comparable to the FIA method. The biggest benefit of this technique is that the excitation component, beam splitter, and filter are not required. Compared with the FIA, CL detection method is much easier to integrate and miniaturize. Just a detector fixed at the reactor cell in the microchannel can accomplished the detection. Therefore, the design of the reactor cell in the microchannel is crucial to the whole system. On the one hand, the analyte and the antibody/antigen require highly efficient mixing and full reaction in the reactor cell. On the other hand, the reaction system may influence the quantification of the detection, such as reaction accompanied by gas production. SPR detection method is growing rapidly, mostly because it is a free labelng and real-time response detection method, and the background noise is virtually eliminated. SPR detection method is feasible for miniaturization and portability (Chinowsky et al. 2007a, b; Fu et al. 2007; Feltis et al. 2008). However, the structure of the SPR device is complex, and a layer of metal (such as gold) must be deposited on the disposable microchip, thus increasing cost. Thermal lens microscopy (TLM) is a kind of very sensitive photothermal conversion detection technique. It is a promising method for detecting analysis in liquids. The detection limit was demonstrated to be as low as the 0.1 nM level (close to the sub-single molecule range) (Tokeshi et al. 2001). However, TLM has a low selectivity so that it cannot distinguish the changes of the temperature and light intensity caused by different analytes. Therefore, it is hard to be applied in the complicated detection. Besides, Integrating and miniaturizing the TLM method into a microfluidic immunoassay is a big challenge.
Nonoptical detection is another important branch of detection methods for the microfluidic immunoassay, especially the electrochemical detection method. Since the electrochemical detection method was firstly combined with the microfluidic immunoassay technique in 1998, it has been developed and applied rapidly in the microfluidic immunoassay system due to the speed, portability and low cost. Because the structure of electrochemical methods is simple, the electrochemical-based microfluidic immunoassay system can be much easily miniaturized and integrated by the micromachining technology. However, the major disadvantage of this method is the interference caused by the components such as the electronic circuits, the electrodes and the microchip. In the liquid environment, because of the electrolysis, the bubbles are easily generated and will influence the result. The electrochemical detection depends on detecting the change of the current or the voltage. Therefore, compared with other detection methods, the background noise of the electronic circuits impacts the detection limit greatly in the electrochemical detection method. The QCM is a potential detection method in the microfluidic immunoassays due to its high sensitivity, the real-time readout, and the low cost. However, how to coat the analyte on the detection surface evenly is a big challenge.
For POC applications, the final goal is to develop a fully integrated, disposable, low-cost, and handheld microfluidic device for the whole-blood immunoassay. Although many existing whole-blood microfluidic immunoassay technologies have the potential, most of them are operated by well-trained technicians and require additional off-chip supporting units, such as fluid controlling systems, power and detection systems etc.. Significant advancement in this area is still required, and much more study remains to be done.
References
Bard J, Faulkner LR (2001) Electrochemical methods: fundamentals and applications, 2nd edn. Wiley, New York
Berti F, Marrazza G et al (2009) Microfluidic-based electrochemical genosensor coupled to magnetic beads for hybridization detection. Talanta 77:971–978
Chediak JA, Luo Z, Seo J, Cheung N, Lee LP, Sands TD (2004) Heterogeneous integration of CdS filters with GaN LEDs for fluorescence detection microsystems. Sens Actuator A Phys 111:1–7
Chen I-J, Lindner E (2009) Lab-on-chip flow injection analysis system without an external pump and valves and integrated with an in line electrochemical detector. Anal Chem 81:9955–9960
Chikkaveeraiah B, Rusling J et al (2009) A microfluidic electrochemical device for high sensitivity biosensing: detection of nanomolar hydrogen peroxide. Electrochem Commun 11:819–822
Chin CD, Linder V, Sia SK (2007) Lab-on-a-chip devices for global health: past studies and future opportunities. Lab Chip 7:41–57
Chinowsky TM, Grow MS, Johnston KS, Nelson K, Edwards T, Fu E, Yager P (2007a) Compact, high performance surface plasmon resonance imaging system. Biosens Bioelectron 22:2208–2215
Chinowsky TM, Soelberg SD, Baker P, Swanson NR, Kauffman P, Mactutis A, Grow MS, Atmar R, Yee SS, Furlong CE (2007b) Portable 24-analyte surface plasmon resonance instruments for rapid, versatile biodetection. Biosens Bioelectron 22:2268–2275
Cho JH, Han SM, Paek EH, Cho IH, Paek SH (2006) Plastic ELISA-on-a-chip based on sequential cross-flow chromatography. Anal Chem 78:793–800
Cho Y-K, Ko C et al (2007) One-step pathogen specific DNA extraction from whole blood on a centrifugal microfluidic device. Lab Chip 7:565–573
Christodoulides N, Tran M, Floriano PN, Rodriguez M, Goodey A, Ali M, Neikirk D, McDevitt JT (2002) A microchip-based multianalyte assay system for the assessment of cardiac risk. Anal Chem 74(13):3030–3036
Chumbimuni-Torres K, Bakker E et al (2006) Potentiometric biosensing of proteins with ultrasensitive ion-selective microelectrodes and nanoparticle labels. J Am Chem Soc 128:13676–13677
Cooper MA (2002) Optical biosensors in drug discovery. Nat Rev 1:515–528
Darain F, Tjin S et al (2009a) Antibody immobilization on to polystyrene substrate––on-chip immunoassay for horse IgG based on fluorescence. Biomed Microdevices 11:653–661
Darain F, Tjin S et al (2009b) On-chip detection of myoglobin based on fluorescence. Biosens Bioelectron 24:1744–1750
Dittmer WU, Martens MFWC et al (2010) Rapid, high sensitivity, point-of-care test for cardiac troponin based onoptomagnetic biosensor. Clin Chim Acta 411:868–873
Ducrée J, Zengerle R et al (2007) The centrifugal microfluidic bio-disk platform. J Micromech Microeng 17:S103–S115
Ekins RP (1960) The estimation of thyroxine in human plasma by an electrophoretic technique. Clin Chim Acta 5:453–459
Engvall E (1977) Quantitative enzyme immunoassay (ELISA) in microbiology. Med Biol 55:193–200
Engvall E, Perlman P (1971) Enzyme-linked immunosorbent assay (ELISA): quantitative assay of immunoglobulin G. Immunochemistry 8(9):871–874
Engvall E, Perlmann P (1971) Enzyme-linked immunosorbent assay (ELISA): quantitative assay of immunoglobulin G. Immunochemistry 8:871–874
Estmer Nilsson C et al (2010) A novel assay for influenza virus quantification using surface plasmon resonance. Vaccine 28:759–766
Fan R, Heath J et al (2008) Integrated barcode chips for rapid, multiplexed analysis of proteins in microliter quantities of blood. Nat Biotechnol 26:1373–1378
Feltis B, Sexton B, Glenn F, Best M, Wilkins M, Davis T (2008) A hand-held surface plasmon resonance biosensor for the detection of ricin and other biological agents. Biosens Bioelectron 23:1131–1136
Frisk T, Stemme G et al (2008) An integrated QCM-based narcotics sensing microsystem. Lab Chip 8:1648–1657
Fu E, Chinowsky T, Nelson K, Johnston K, Edwards T, Helton K, Grow M, Miller J, Yager P (2007) SPR imaging-based salivary diagnostics system for the detection of small molecule analytes. Ann N Y Acad Sci 1098:335–344
Fung YC (1973) Stochastic flow in capillary blood vessels. Microvasc Res 5:34–48
Gao Y, Hu G, Lin F, Li D (2005a) An electrokinetically-controlled immunoassay for simultaneous detection of multiple microbial antigens. Biomed Microdevices 7(4):301–312
Gao Y, Lin F, Hu G, Li D (2005b) Development of a novel electrokinetically driven microfluidic immunoassay for the detection of Helicobacter pylori. Anal Chim Acta 543:109–116
Godino N, del Campo FJ et al (2010) Construction and characterisation of a modular microfluidic system: coupling magnetic capture and electrochemical detection. Microfluid Nanofluid 8:393–402
Grumann M, Geipel A, Riegger L, Zengerle R, Ducre′e J (2005) Batch-mode mixing on centrifugal microfluidic platforms. Lab Chip 5:560–565
Hashimoto M, Kaji H, Kemppinen ME, Nishizawa M (2008) Localized immobilization of proteins onto microstructures within a preassembled microfluidic device. Sens Actuator B Chem 128(2):545–551
Hatch AE, Kamholz KR, Hawkins MS, Munson EA, Schilling B, Weigl H, Yager P (2001) A rapid diffusion immunoassay in a T-sensor. Nat Biotechnol 19:461–465
Hawkins KR, Yager P et al (2002) Diffusion immunoassay for protein analytes. 2nd annual international IEEE-EMBS special topic conference on microtechnologies in medicine & biology, pp 535–540
Henares TG, Funano S-i, Terabe S, Mizutani F, Sekizawa R, Hisamoto H (2007) Multiple enzyme linked immunosorbent assay system on a capillary-assembled microchip integrating valving and immunoreactions functions. Anal Chim Acta 589(2):173–179
Herr AE, Anup K (2007) Microfluidic immunoassays as rapid saliva-based clinical diagnostics. PNAS 104:5268–5273
Herr AE, Singh AK (2007) Integrated microfluidic platform for oral diagnostics. Ann NY Acad Sci 1098:362–374
Herr AE, Hatch AV, Throckmorton DJ, Tran HM, Brennan JS, Giannobile WV, Singh AK (2007) Microfluidic immunoassays as rapid saliva-based clinical diagnostics. Proc Natl Acad Sci USA 104(13):5268–5273
Hirsch LR, Jackson JB, Lee A, Halas NJ, West JL (2003) A whole blood immunoassay using gold nanoshells. Anal Chem 75:2377–2381
Hirsch LR, Halas NJ, West JL (2005) Whole-blood immunoassay facilitated by gold nanoshell-conjugate antibodies. Methods Mol Biol 303:101–112
Hnaiein M, Jaffrezic-Renault N et al (2008) A conductometric immunosensor based on functionalized magnetite nanoparticles for E. coli detection. Electrochem Commun 10:1152–1154
Hofmann O, Voirin G, Niedermann P, Manz A (2002) Three-dimensional microfluidic confinement for efficient sample delivery to biosensor surfaces: application to immunoassays on planar optical waveguides. Anal Chem 74:5243–5250
Hosokawa K, Omata M, Sato K, Maeda M (2006) Power-free sequential injection for microchip immunoassay toward point-of-care testing. Lab Chip 6(2):236–241
Hosokawa K, Omata M, Maeda M (2007) Immunoassay on a power-free microchip with laminar flow-assisted dendritic amplification. Anal Chem 79:6000–6004
Hu G, Gao Y, Sherman P, Li D (2005) A microfluidic chip for heterogeneous immunoassay using electrokinetical control. Microfluid Nanofluid 1:346–355
Hu G, Gao Y, Li D (2007) Modeling micropatterned antigen–antibody binding kinetics in a microfluidic chip. Biosens Bioelectron 22:1403–1409
Huang H, Pu X et al (2009) Rapid analysis of alpha-fetoprotein by chemiluminescence microfluidic immunoassay system based on super-paramagnetic microbeads. Biomed Microdevices 11:213–216
Huckle D (2006) Point-of-care diagnostics: will the hurdles be overcome this time? Expert Rev Med Device 3:421–426
Huckle D (2008) Point-of-care diagnostics: an advancing sector with nontechnical issues. Expert Rev Mol Diagn 8:679–688
Ihara M, Ueda H et al (2010) Micro OS-ELISA: rapid noncompetitive detection of a small biomarker peptide by open-sandwich enzyme-linked immunosorbent assay (OS-ELISA) integrated into microfluidic device. Lab Chip 10:92–100
Järås K, Tajudin AA, Ressine A, Soukka T, Marko-Varga G, Bjartell A, Malm J, Laurell T, Lilja H (2008) ENSAM: europium nanoparticles for signal enhancement of antibody microarrays on nanoporous silicon. J Proteome Res 7:1308–1314
Kagebayashi C, Yamaguchi I, Akinaga A, Kitano H, Yokoyama K, Satomura M, Kurosawa T, Watanabe M, Kawabata T, Chang W, Li C, Bousse L, Wada HG, Satomura S (2009) Automated immunoassay system for AFP-L3% using on-chip electrokinetic reaction and separation by affinity electrophoresis. Anal Biochem 388(2):306–311
Kakehi K, Oda Y et al (2001) Fluorescence polarization: analysis of carbohydrate–protein interaction. Anal Biochem 297(2):111–116
Karlsson R (2004) SPR for molecular interaction analysis: a review of emerging application areas. J Mol Recognit 17:151–161
Kim N, Kim D-K, Cho Y-J (2009) Development of indirect-competitive quartz crystal microbalance immunosensor for C-reactive protein. Sens Actuator B 143:444–448
Kitamori T, Tokeshi M, Hibara A, Sato K (2004) Peer reviewed: thermal lens microscopy and microchip chemistry. Anal Chem 76(3):52A–60A
Kong J, Lin B et al (2009) Integrated microfluidic immunoassay for the rapid determination of clenbuterol. Lab Chip 9:1541–1547
Kretschmann E (1971) The determination of the optical constants of metals by excitation of surface plasmons. Z Phys 241:313
Krishnamoorthy G, Carlen ET, Kohlheyer D, Schasfoort RBM, van den Berg A (2009) Integrated electrokinetic sample focusing and surface plasmon resonance imaging system for measuring biomolecular interactions. Anal Chem 81:1957–1963
Krishnamoorthy G et al (2010) Electrokinetic lab-on-a-biochip for multi-ligand/multi-analyte biosensing. Anal Chem 82:4145–4150
Kuei-Ling S, Lin Y-C, Chen W-T et al (2009) An immunoassay using an electro-microchip, nanogold probe and silver enhancement. Microfluid Nanofluid 6:93–98
Laiwattanapaisal W, Songjaroen T, Maturos T, Lomas T, Sappat A, Tuantranont A (2009) On-chip immunoassay for determination of urinary albumin. Sensors 9:10066–10079
Lee K-H, Yuan-Deng S, Chen S-J, Tseng F-G, Lee G-B (2007) Microfluidic systems integrated with two-dimensional surface plasmon resonance phase imaging systems for microarray immunoassay. Biosens Bioelectron 23(4):466–472
Lee B, Ko C et al (2009) A fully automated immunoassay from whole blood on a disc. Lab Chip 9:1548–1555
Lenshof A, Laurell T et al (2009) Acoustic whole blood plasmapheresis chip for prostate specific antigen microarray diagnostics. Anal Chem 81:6030–6037
Liang K-Z, Liu Z-X et al (2009) Conductometric immunoassay for interleukin-6 in human serum based on organic/inorganic hybrid membrane functionalized interface. Bioprocess Biosyst Eng 32:353–359
Lim T-K, Ohta H, Matsunaga T (2003) Microfabricated on-chip-type electrochemical flow immunoassay system for the detection of histamine released in whole blood samples. Anal Chem 75:3316–3321
Liu C, DafuCui H (2010) A hard–soft microfluidic-based biosensor flow cell for SPR imaging application. Biosens Bioelectron 26(1):255–261
Liu C-Yu, Lee G-B et al (2009a) Integrated microfluidic system for electrochemical sensing of urinary proteins. Biomed Microdevices 11:201–211
Liu H, Zhong Z et al (2009b) Enhanced conductometric immunoassay for hepatitis B surface antigen using double-codified nanogold particles as labels. Biochem Eng J 45:107–112
Ljungstrom I, Engvall E, Ruitenberg EJ (1974) Proceedings: ELISA, enzyme-linked immunosorbent assay—a new technique for serodiagnosis of trichinosis. Parasitology 69:xxiv
Luppa PB, Sokoll LJ, Chan DW (2001) Immunosensors—principles and applications to clinical chemistry. Clin Chim Acta 314:1–26
Meagher RJ, Hatch AV, Renzi RF, Singh AK (2008) An integrated microfluidic platform for sensitive and rapid detection of biological toxins. Lab Chip 8(12):2046–2053
Mecea VM (2005) From quartz crystal microbalance to fundamental principles of mass measurements. Anal Lett 38:753–767
Michalzik M, Wilke R, Buttgenbach S (2005) Miniaturized QCM-based flow system for immunosensor application in liquid. Sens Actuator B Chem 111–112(11):410–415
Miles LEM, Hales CN (1968) Labelled antibodies and immunological assay systems. Nature 219:186–189
Moorthy J, Mensing GA, Kim D, Mohanty S, Eddington DT, Tepp WH, Johnson EA, Beebe DJ (2004) Microfluidic tectonics platform: a colorimetric, disposable botulinum toxin enzyme-linked immunosorbent assay system. Electrophoresis 25:1705
Morozov VN, Groves S, Turell MJ, Bailey C (2007) Three minutes-long electrophoretically assisted zeptomolar microfluidic immunoassay with magnetic-beads detection. J Am Chem Soc 129:12628–12629
Muhammad-Tahir Z, Alocilja E (2003) A conductometric biosensor for biosecurity. Biosens Bioelectron 18:813–819
Mullett WM, Lai EPC, Yeung JM (2000) Surface plasmon resonance-based immunoassays. Methods 22:77–91
Nobel Prize home page. http://nobelprize.org/nobel_prizes/medicine/laureates/1977/. Accessed June 2005
Pais A, Banerjee A, Klotzkin D, Papautsky I (2008) High-sensitivity, disposable lab on-a-chip with thin-film organic electronics for fluorescence detection. Lab Chip 8:794–800
Park SW, Yang SS et al (2009) An electrochemical immunosensing lab-on-a-chip integrated with latch mechanism for hand operation. J Micromech Microeng 19:025024
Parsa H, Chin CD, Mongkolwisetwara P, Lee BW, Wang JJ, Sia SK (2008) Effect of volume- and time-based constraints on capture of analytes in microfluidic heterogeneous immunoassays. Lab Chip 8:2062–2070
Pereira SV et al (2010a) Integrated microfluidic magnetic immunosensor for quantification of human serum IgG antibodies to Helicobacter pylori. J Chromatogr B Anal Technol Biomed Life Sci 878(2):253–257
Pereira S, Raba J, Messina G (2010b) IgG anti-gliadin determination with an immunological microfluidic system applied to the automated diagnostic of the celiac disease. Anal Bioanal Chem 396:2921–2927
Petti CA, Polage CR, Quinn TC, Ronald AR, Sande MA (2006) Laboratory medicine in Africa: a barrier to effective health care. Clin Infect Dis 42:377–382
Pugia M, Schulman L et al (2005) Microfluidic tool box as technology platform for hand-held diagnostics. Clin Chem 51(10):1923–1932
Qin L, Vermesh O, Shi Q, Heath J (2009) Self-powered microfluidic chips for multiplexed protein assays from whole blood. Lab Chip 9:2016–2020
Qiu X, Thompson JA, Chen Z et al (2009) Finger-actuated, self-contained immunoassay cassettes. Biomed Microdevices 11(6):1175–1186
Rabe J, Buttgenbach S, Zimmermann B, Hauptmann P (2000) Design, manufacturing, and characterization of high-frequency thicknessshear mode resonators. In: Proceedings of the IEEE/EIA international frequency control symposium, pp 106–112
Reichmuth DS, Wang SK, Barrett LM, Throckmorton DJ, Einfeld W, Singha AK (2008) Rapid microchip-based electrophoretic immunoassays for the detection of swine influenza virus. Lab Chip 8(8):1319–1324
Riegger L, Ducr′ee J et al (2006) Read-out concepts for multiplexed bead-based fluorescence immunoassays on centrifugal microfluidic platforms. Sens Actuator A 126:455–462
Sato K, Tokeshi M, Odake T, Kimura H, Ooi T, Nakao M, Kitamori T (2000) Integration of an immunosorbent assay system: analysis of secretory human immunoglobulin A on polystyrene beads in a microchip. Anal Chem 72(6):1144–1147
Sato K, Tokeshi M, Kimura H, Kitamori T (2001) Determination of carcinoembryonic antigen in human sera by integrated bead-bed immunoasay in a microchip for cancer diagnosis. Anal Chem 73(6):1213–1218
Sato K, Yamanaka M, Takahashi H, Tokeshi M, Kimura H, Kitamori T (2002) Microchip-based immunoassay system with branching multichannels for simultaneous determination of interferon-gamma. Electrophoresis 23(5):734–739
Schmid-Schonbein GW, Skalak R, Usami S, Chien S (1980) Cell distribution in capillary networks. Microvasc Res 19:18–44
Schmidt O, Bassler M, Kiesel P, Knollenberg C, Johnson N (2007) Fluorescence spectrometer-on-a-fluidic-chip. Lab Chip 7:626–629
Schuurs AHWM, van Weemen BK (1980) Enzyme-immunoassay: a powerful analytical tool. J Immunoassay 1:229–249
Seo J, Lee LP (2003) Fluorescence amplification by self-aligned integrated microfluidic optical systems. IEEE transducers 2003, solid-state sensors, actuators and microsystems, pp 1136–1139
Seo J, Lee LP (2004) Disposable integrated microfluidics with self-aligned planar microlenses. Sens Actuator B Chem 99:615–622
Shankaran D, Miura N (2007) Trends in interfacial design for surface plasmon resonance based immunoassays. J Phys D Appl Phys 40:7187–7200
Shankaran DR, Gobi KV, Miura N (2007) Recent advancements in surface plasmon resonance immunosensors for detection of small molecules of biomedical, food and environmental interest. Sens Actuator B 12:158–177
Singer PA, Taylor AD, Daar AS, Upshur RE, Singh JA, Lavery JV (2007) Grand challenges in global health: the ethical, social and cultural program. PLoS Med 4(9):e265
Steigert J, Ducr′ee J et al (2005) Integrated sample preparation, reaction, and detection on a high-frequency centrifugal microfluidic platform. JALA 10(5):331–341
Steigert J, Ducr′ee J et al (2006) Fully integrated whole blood testing by real-time absorption measurement on a centrifugal platform. Lab Chip 6:1040–1044
Stern E, Fahmy T et al (2010) Label-free biomarker detection from whole blood. Nat Nanotechnol 5:138–142
Stevens DY, Petri CR, Osborn JL, Spicar-Mihalic P, McKenzie KG, Yager P (2008) Enabling a microfluidic immunoassay for the developing world by integration of on-card dry reagent storage. Lab Chip 8:2038–2045
Tachi T, Baba Y et al (2009) Microchip-based homogeneous immunoassay using fluorescence polarization spectroscopy. Lab Chip 9:966–971
Thorslund S, Bergquist J (2006) A hybrid poly (dimethylsiloxane) microsystem for on-chip whole blood filtration optimized for steroid screening. Biomed Microdevices 8:73–79
Tokeshi M, Uchida M, Hibara A, Sawada T, Kitamori T (2001) Determination of subyoctomole amounts of nonfluorescent molecules using a thermal lens microscope: subsingle-molecule determination. Anal Chem 73(9):2112–2116
Uchiyama K et al (2000) Thermal lens microscope. Jpn J Appl Phys 39:5316–5322
Uludag Y, Tothill I (2010) Development of a sensitive detection method of cancer biomarkers in human serum (75%) using a quartz crystal microbalance sensor and nanoparticles amplification system. Talanta 82:277–282
Uotila M, Ruoslathi E, Envall E (1981) Two-site sandwich enzyme immunoassay with monoclonal antibodies to human alphafetoprotein. J Immunol Methods 42:11–15
Van Weeman BK, Schuurs A (1971) Immunoassay using antigen-enzyme conjugates. FEBS Lett 15(3):232–236
Van Weemen BK, Schuurs AHWM (1971) Immunoassay using antigenenzyme conjugates. FEBS Lett 15:232–236
Varshney M, Tung S et al (2007) A label-free, microfluidics and interdigitated array microelectrode-based impedance biosensor in combination with nanoparticles immunoseparation for detection of Escherichia coli O157:H7 in food samples. Sens Actuator B 128:99–107
Verpoorte E (2003) Beads and chips: new recipes for analysis. Lab Chip 3(4):60N–68N
Wang X, Donal D, Bradley C et al (2007) Integrated thin-film polymer/fullerene photodetectors for on-chipmicrofluidic chemiluminescence detection. Lab Chip 7:58–63
Wang H, Liu B et al (2008) Microfluidic immunosensor based on stable antibody-patterned surface in PMMA microchip. Electrochem Commun 10:447–450
Wang X, de Mello AJ et al (2009) Thin-film organic photodiodes for integrated on-chip chemiluminescencedetection––application to antioxidant capacity screening. Sens Actuator B 140:643–648
Wang H, Liu B et al (2010) Microfluidic chip-based aptasensor for amplified electrochemical detection of human thrombin. Electrochem Commun 12:258–261
Weigl BH, Yager P (1999) Microfluidic diffusion-based separation and detection. Science 283:346–347
Weigl BH, Bardell RL, Cabrera CR (2003) Lab-on-a-chip for drug development. Adv Drug Deliv Rev 55:349–377
Wild D (2008) The immunoassay handbook. 3rd edn. Elsevier, Oxford
Wolf M, Juncker D et al (2004) Simultaneous detection of C-reactive protein and other cardiac markers in human plasma using micromosaic immunoassays and self-regulating microfluidic networks. Biosens Bioelectron 19(10):1193–1202
Xiang Q, Hu G, Gao Y, Li D (2006) Miniaturized immunoassay microfluidic system with electrokinetic control. Biosens Bioelectron 21:2006–2009
Yacoub-George E, Hell W, Meixner L, Wenninger F, Bock K, Lindner P, Wolf H, Kloth T, Feller KA (2007) Automated 10-channel capillary chip immunodetector for biological agents detection. Biosens Bioelectron 22:1368–1375
Yadavalli VK, Pishko MV (2004) Biosensing in microfluidic channels using fluorescence polarization. Anal Chim Acta 507(1):123–128
Yager P, Edwards T, Fu E, Helton K, Nelson K et al (2006) Microfluidic diagnostic technologies for global public health. Nat Insight 442:412–418
Yalow RS, Berson SA (1960) Immunoassay of endogenous plasma insulin in man. Clin Invest 39(7):1157–1175
Yang S, Ji B, Ündar A, Zahn J (2006a) Microfluidic devices for continuous blood plasma separation and analysis during pediatric cardiopulmonary bypass procedures. ASAIO J 52:698–704
Yang S, Undar A, Zahn JD (2006b) A microfluidic device for continuous, real time blood plasma separation. Lab Chip 6:871–880
Yang S, Undar A, Zahn J (2007) Continuous cytometric bead processing within a microfluidic device for bead based sensing platforms. Lab Chip 7:588–595
Yang S-Y, Lee G-B et al (2008) Micro flow cytometry utilizing a magnetic bead-based immunoassay for rapid virus detection. Biosens Bioelectron 24:855–862
Yang Y-N, Lee G-B et al (2009) An integrated microfluidic system for C-reactive protein measurement. Biosens Bioelectron 24:3091–3096
Yeh C-H, Lin Y-C et al (2009) Development of an immunoassay based on impedance measurements utilizing an antibody-nanosilver probe, silver enhancement, and electro-microchip. Sens Actuator B 139:387–393
Yen RT, Fung YC (1978) Effect of velocity distribution on red cell distribution in capillary blood vessels. Am J Physiol 235(2):H251–H257
Yoo S, Lee S-H et al (2009) Microfluidic chip-based electrochemical immunoassay for hippuric acid. Analyst 134:2462–2467
Zhang S, Su M et al (2009) MCE enzyme immunoassay for carcinoembryonic antigen and alphafetoprotein using electrochemical detection. Electrophoresis 30:3427–3435
Zimmermann M, Delamarche E, Wolf M, Hunziker P (2005) Modeling and optimization of high-sensitivity, low-volume microfluidic-based surface immunoassays. Biomed Microdevices 7:99–110
Acknowledgments
The authors wish to thank the financial support extended by the Canada Research Chair program and the Natural Sciences and Engineering Research Council (NSERC) of Canada through a research grant to D. Li.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, H., Weng, X. & Li, D. Microfluidic whole-blood immunoassays. Microfluid Nanofluid 10, 941–964 (2011). https://doi.org/10.1007/s10404-010-0718-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10404-010-0718-9