Abstract
Leptospirosis is a zoonotic infectious disease of global significance. Political, economic, demographic, ecologic, and other anthropogenically driven environmental changes have fueled the reemergence of this disease in industrialized and developing countries, and in both urban and rural settings. We argue that conventional disciplinary, even interdisciplinary, research methods are not sufficient to elucidate the complex mechanisms and causal relationships among the myriad factors responsible for infectious disease emergence. To address the significant gaps in the field of leptospirosis, an integrated research agenda is needed to guide successful public health remediation of the disease. Based on both working group analysis of literature and newly obtained information, we describe cross-disciplinary collaborative approaches that allow a novel approach to understand leptospirosis emergence with regard to mountain-to-sea ecosystems in Hawai‘i and other region-specific ecosystems. Leptospirosis research is a model for how complementary disciplines in the social, cultural, ecological, and biomedical sciences can optimally interact towards a higher understanding of emerging infectious diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The public health significance of leptospirosis, a globally important zoonotic infectious disease (Faine et al., 1999; Bharti et al., 2003), is remarkably neglected. Besides being vastly underreported (WHO, 2001), it is an important waterborne disease affecting hundreds of millions of people worldwide, most of whom cannot easily escape the conditions of exposure either in urban or rural environments. The transmission of leptospirosis occurs within an ecological context of humans coming into contact with water contaminated by urine from a wide variety of both wild and domesticated animals. For this reason, both from a research standpoint, and as a case example for exploring interdisciplinary methods, leptospirosis is particularly well-suited as a model system for the study of the causes of pathogen emergence—from the microbial to the ecosystem level.
Leptospirosis is characterized in its most extreme form as a fulminant hemorrhagic fever accompanied by jaundice, renal failure, and multiple organ failure (Bharti et al., 2003). Leptospirosis affects people living in urban slums and rural environments in developed and developing countries alike. Populations at risk exhibit a similarly disparate pattern—from urban residents (Fig. 1) to those living in rural areas (Fig. 2), to specific industrial occupations, to traditional wetland farming communities (Fig. 3) and adventure tourists (Vinetz et al., 1996; Sejvar et al., 2003). While much of the recent increase in reported cases of leptospirosis is due to increased vigilance, leptospirosis appears to be increasing around the world, both in endemic and epidemic settings (Sehgal, 2000). Although waterborne, leptospirosis is not transmitted by the fecal–oral route as are cholera, bacterial dysentery, and other diarrheal diseases (Bharti et al., 2003). Its transmission cycle (Fig. 4) often involves “spill-over” from wildlife to domestic species, coastal watershed contamination resulting in infection of marine mammals, and even “spill-back,” closing the wild-domestic–wild species loop (Daszak et al., 2000, 2001). As humans increase their urbanization and move themselves, along with domesticated animals and unwanted rodent companions, into new places, there are more opportunities for leptospirosis transmission.
The urban slum environment of the Belen district of Iquitos, Peru in the Amazon region. A, B: Typical houses in the Belen district, built on stilts to avoid flood waters when the river rises. C: The typical sanitation of the Belen Market area that attracts scavenger animals such as dogs and rats. D: A typical view of the Belen Market area where commerce goes on and rats are often seen underneath tables and in gutters. Rats are so abundant in the market areas that they are commonly seen during the day despite their being primarily nocturnal.
The rural village of Padrecocha outside of Iquitos, Peru. A: A quebrada (creek), strongly associated with leptospirosis transmission. B: A typical well in close association with activities of daily living. C: The pond of Padrecocha adjacent to the river. D: Flooding in the village during the high river season after heavy rains.
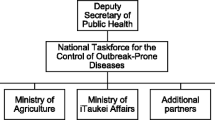
Transmission cycle of pathogenic Leptospira. Leptospira are transmitted between mammals—the natural maintenance hosts—to humans who are accidental hosts, through water. The transmission cycle is amplified when Leptospira spill-over from shedding wild or feral maintenance host populations produces chronic infections or outbreaks in domestic species (i.e., pigs, cattle, horses, dogs, cats) due either to weather-related phenomena such as flooding, or anthropogenic influences such as hydrologic alternations of watersheds.
Despite nearly a century of research on leptospirosis, major gaps exist in understanding central mechanisms in its transmission, pathogenesis, protective immunity, ecology (both of the microbes and mammalian reservoirs), and the taxonomic and genetic relationships among Leptospira species. Satisfactory diagnostic and environmental tests are lacking, as are studies that would lead to improved programs in disease prevention.
The theme of this article is that the spread of leptospirosis is anthropogenically driven and that a variety of human cultural factors combine with unique biological aspects of this disease to contribute to its increasing human impact. We describe leptospirosis as a transdisciplinary problem to be framed within biomedical, ecological, environmental, social, political, and cultural contexts. The overall goal of this socio-ecological systems approach to infectious disease emergence is to develop an integrated, interdisciplinary understanding of large-scale mechanisms and determinants of infectious disease emergence (Lewis, 2005). Starting with considerations in Hawai‘i, leptospirosis appeared to be ideal for examining how emerging infectious disease (EID) research in general might be advanced through an approach that transcended disciplinary boundaries: the transdisciplinary approach (Parkes et al., 2005). Hawai‘i’s mountain-to-sea ecosystems are associated with the highest rates of leptospirosis incidence in the U.S. In Hawai‘i, the term “ahupua‘a” is used to describe the watersheds within these ecosystems, which correspond to discrete mountain-to-sea watershed zones defined by distinct ridges extending from upland to the shore and seaward to the barrier reefs.
In this article, two major sub-themes emerge that demonstrate the need and opportunity for developing a more systematic, and ecosystem-based approach to leptospirosis transmission research. First, culturally important activities within the disease transmission model necessitate the inclusion of taro farmers as both a population at highest risk and as a community with which researchers could partner for participatory research and prevention programs. It also includes dissolving the perceived boundary between the terrestrial and marine environment compelled by the recent discovery of endangered Hawaiian monk seals threatened by leptospirosis.
METHODS: WORKING GROUP
A multidisciplinary leptospirosis working group was convened in March 2005. The working group held a leptospirosis mini-symposium with presentations ranging from clinical to ecological, including the application of complex systems thinking to understanding parasite (and pathogen) and host relationships as part of ecosystems. This was part of a larger meeting “Socio-ecological Systems and Emerging Infectious Diseases” held in Honolulu, hosted by the East–West Center and Asia-Pacific Institute for Tropical Medicine and Infectious Diseases and funded by the U.S. National Institutes of Health Roadmap initiative “Research Teams of the Future.” The aim of this meeting was to address interdisciplinary integration to solve problems in EIDs; this project’s purpose was to attempt to break down disciplinary boundaries by viewing disease emergence from the standpoint of the interaction of human and natural systems. An important catalytic factor in breaking down some of the disciplinary boundaries was the group’s impromptu walk to a nearby wetland taro field, as well as the meeting’s venue, Manoa Campus of the University of Hawai‘i, the site of a recent leptospirosis outbreak associated with a flood. This experience catalyzed the group’s adoption of a culturally based, ecological systems perspective as a way to broaden the research “lens” to meaningfully capture the dimensions of this EID. Despite substantial differences in training and research perspectives, the group rapidly found common ground by identifying several critical themes that took a social–ecological systems or biocomplexity view (Wilcox and Colwell, 2005). Incorporating the different perspectives of all the disciplines involved, an approach to transdisciplinary integration was developed.
This working group focused on identifying biomedical and socio-political factors that serve as barriers to understanding mechanisms of leptospirosis emergence, persistence and remediation. A systematic literature review was performed in preparation for the meeting. Medline searches since 1966 used the terms “Leptospira,” “leptospirosis,” “anthropogenic,” “epidemiology,” “social sciences,” “ecology,” “mammalian reservoir,” and “risk assessment.” In addition, the general literature on biocomplexity, social–ecological systems, and the application of complexity theory in ecology was reviewed prior to the meeting.
The working group visited model lo‘i (plots irrigated by the natural flow of water downhill in which wet taro is grown) at the Papa Lo‘i Kānewai at Kamakakūokalani at the Center for Hawaiian Studies at the University of Hawai‘i. Lo‘i were examined with regard to botanical contents and hydrology. The cultural staff at this site were interviewed with regard to cultural underpinnings of the lo‘i and political motivations and contexts of taro farming. These observations were combined with ethnographic interview data previously collected by working group members. Wetland taro farmers on the island of Kaua‘i were interviewed with regard to their understanding of the microbiology and epidemiology of leptospirosis, the possible effects of leptospirosis on health, and possible relationships between taro cultivation, encroachment of modern agricultural methods on traditional farming, and the transmission of leptospirosis.
RESULTS
Working Group Summary: Biology of Leptospira and Leptospirosis
Leptospirosis is caused by more than 250 varieties of spirochetes (one clade of bacteria characterized as having spiral shapes and characteristic winding motility) in the genus Leptospira. Mammals are the primary hosts for pathogenic Leptospira; thus the disease is a zoonosis. The organisms live attached to the brush border of proximal renal tubules and are chronically shed into the urine. Chronic shedding is the means of transmission to the environment where humans contract infection through mucosal or percutaneous exposure. Many human leptospirosis infections are due to Leptospira interrogans, one of seven pathogenic species of Leptospira that produce febrile illness with a wide range of manifestations and seriousness ranging from mild flu-like symptoms to syndromes including jaundice, renal failure, and pulmonary hemorrhage that are frequently fatal (Trevejo et al., 1998; Ko et al., 1999; Segura et al., 2005).
The genus Leptospira contains hundreds of serovars and genetic types that occupy different ecosystems, habitats, and mammalian reservoirs. Within the genus are highly pathogenic host-specific strains, and harmless free-living waterborne strains termed saprophytes. Strains of Leptospira are morphologically indistinguishable. Saprophytic leptospires can be differentiated from pathogenic leptospires by a variety of biochemical and nucleic acid tests, most precisely using DNA-based tools which continue to be developed (Ramadass et al., 1992; Faine et al., 1999). In contrast to pathogenic Leptospira, the free-living saprophytes inhabit highly diverse habitats, including some serovars that have managed to cross the saltwater boundary. Little is known about the genetics, pathology, and parasite/host adaptations of these nonpathogenic types, or about tolerance for saltwater of Leptospira that affect marine mammals.
Rats, mice, cattle, pigs, and dogs are the domestic species most commonly implicated in the transmission of leptospirosis. The organisms persist in proximal renal tubules; chronic excretion of organisms in the urine is the means of transmission to the environment. The incidence of leptospirosis is significantly higher in tropical compared to temperate regions, since warm temperatures prolong the persistence of the microorganism in the environment (Levett, 2001).
Most mammals can become infected with pathogenic Leptospira. Different leptospiral serovars are associated with one or more maintenance hosts, which serve as long-term reservoirs, although pathogenic Leptospira can clearly cross animal species both to cause disease and to result in transmission.
Specific serovars are classically linked to particular reservoir hosts (Table 1; Bolin, 2003). The relationship between maintenance host and serovar is characterized by efficient transmission, high seroprevalence (up to 50%), and chronic asymptomatic carriage. Recent evidence suggests that specific molecular interactions between leptospire and host occur to allow for such specific mammal-serovar pairing (Nally et al., 2005). Leptospires are primarily transmitted directly or indirectly via infected urine, although semen, placental fluids, and milk have been suggested as additional modes of transmission. Transplacental transmission has been documented.
International Epidemiological Problem of Understanding Leptospirosis: Lack of Reporting
Leptospirosis is the most globally widespread zoonosis (Bharti et al., 2003). The incidence of leptospirosis is significantly higher in tropical than temperate regions (Levett, 2001). Conditions such as high humidity, sunshine protection, and warm temperatures allow the bacteria to survive outside of hosts for months. Solid supports onto which leptospires can adhere (such as diatoms, agar granules, etc.) greatly facilitate long-term environmental persistence (Trueba et al., 2004; Matsunaga et al., 2005). Epidemics of leptospirosis are associated with unusually high rainfall and flooding in relationship to land use and land coverage changes associated with urbanization. In regions where the disease is epidemic, incidence is strongly seasonal. Peak transmission occurs during rainy seasons in tropical climates, particularly associated with monsoons or hurricanes, and summer in temperate climates; abundant water and warm temperatures combine to increase leptospire survival and distribution (Levett, 2001).
From 1974 until the cessation of national surveillance in 1995, leptospirosis was a “reportable infectious disease” to state and national epidemiologists. Statutory requirements for reporting leptospirosis was stopped because of the perceived low incidence of disease in the United States combined with the recognized lack of public health measures aimed at controlling zoonotic transmission. Given the epidemic potential of the disease (Rathinam et al., 1997; Trevejo et al., 1998; Ko et al., 1999), the high case fatality rate in the presence of severe disease (Ko et al., 1999; Smythe, 2001; Segura et al., 2005), its manifestations as a hemorrhagic fever mimicking feared bioterrorism diseases (Bharti et al., 2003; Segura et al., 2005), and its global impact, there is a clear need to reinstitute leptospirosis as a reportable disease both in the U.S. and internationally. Making leptospirosis a reportable disease will require public health systems to establish systematic diagnosis and implement measures to remediate environmental contributions to the spread of leptospirosis. These measures need to target zoonotic reservoirs and initiate and sustain sanitation efforts guided by microbiological environmental risk assessment and will depend on experts in the field being able to demonstrate the substantial economic and public health impact of leptospirosis.
Need for Eco-epidemiological Modeling in Leptospirosis
Until recently, little consideration has been given to developing general “eco-epidemiological” or disease ecology models for understanding nonbiomedical factors leading to human disease causation. In the case of leptospirosis, the current level of analysis has been focused primarily on relating severe weather to leptospirosis outbreaks (Kupek et al., 2000). With regard to epidemic disease, rainfall and floods are known to trigger outbreaks, presumably through the mobilization of leptospires from soil into flowing waters (Correa, 1975; Murhekar et al., 1998; Trevejo et al., 1998; Ko et al., 1999; Sanders et al., 1999; Kupek et al., 2000). In the endemic setting, the disease is transmitted via contaminated ground waters during activities of daily living (Sehgal et al., 1999; Johnson et al., 2004). While flooding is often associated with poor environmental management, the quality of flood waters, i.e., proximity to animal pastures, modified landscape, natural water filtration processes, rate of water fluxes (so essential to wet taro farming), has enormous influence on disease incidence in the case of water-associated diseases.
New models of leptospirosis need to take into account the complex anthropogenic environmental factors that influence infectious disease emergence, the socio-political factors that determine how humans interact with their environments, and combine these with quantification of leptospires in the environment, i.e., surface waters. The lack of a rapid diagnostic test and accuracy in identifying leptospires in water samples has limited investigation into the environmental distribution of pathogenic Leptospira, although new molecular approaches to assess the quantity and species of pathogenic Leptospira in environmental water surface waters is currently under active development [Ganoza et al., unpublished data]. Polymerase chain reaction (PCR) methods, the recent completion of the L. interrogans DNA sequence and development of primer sets has dramatically improved the capacity to address these research areas. Yet, as we argue, improving on existing methods of clinical, epidemiological, and biomedical research per se, while necessary, will not be sufficient to understand what factors have specifically led to new foci of leptospirosis. For example, an outbreak of leptospirosis occurred in a new village (Los Delfines) outside the city of Iquitos, Peru, where governmental subsidies led to the creation of housing, pig farming, and new settlements to support people involved in deforestation activities to reclaim rainforest for human use. These activities took place without adequate provision for sanitation, led to environmental contamination by pig urine (as determined by quantification of leptospires along a gradient of a creek leading from the pig farm to the pond site of the leptospirosis outbreak [Cunningham et al., unpublished data]). Another example is the presence of Asian leptospires, Leptospira santarosai serovar Shermani, in cattle, pigs, and water buffalo in the Peruvian Amazon. We hypothesize that this leptospire was introduced in this region when water buffalo were given to peasants in exchange for rainforest land reclamation; the water buffalo originated from southeast Asia, where this leptospiral serovar is known to be present [Cunningham et al., unpublished data]. Understanding the root causes of these phenomena requires understanding social, cultural, and political imperatives.
Mechanisms of Environmental and Ecological Factors in Leptospiral Emergence and Persistence
Anthropogenically driven land use changes can produce ecological conditions that facilitate geographic expansion of pathogens via range extension or reemergence of hosts and vectors, increased host prevalence, host-jumping (spill-over and spill-back), and pathogen adaptation (Wilcox and Gubler, 2005). The eco-epidemiology of leptospirosis fits this model: association with proliferation of domestic and peridomestic host reservoir species (e.g., Rattus and Mus); jumping of pathogens from wild to domestic animal populations precipitating endemic cycles in the latter; and outbreaks and epidemics driven by maintenance-accidental host cycle amplification as seen commonly in vectorborne diseases (e.g., dengue, Rift Valley fever, West African schistosomaisis). Thus, the increased contact and ecological mixing of pest, domestic, feral, and wild animals accompanying rapid land use change can explain the apparent increasing incidence of human disease.
Many individual cases result from direct human contact with animals shedding leptospires. Yet the increased endemism and epidemic activity appears to involve group exposure resulting from continuous environmental contamination with the urine of chronically infected maintenance hosts. Contaminated water used for drinking or bathing, and exposure to contaminated surface water, particularly during the rainy season or following floods precipitated by storm events, appear to be the most frequent causes of the disease. Previous research linking increased rainfall and certain soil types with outbreaks of leptospirosis in domestic animals (Carroll and Campbell, 1987; Miller et al., 1991; Barwick et al., 1997, 1998; Ward, 2002) and the association of flooding with human outbreaks (Trevejo et al., 1998; Barcellos and Sabroza, 2000), including observation of a recent outbreak in Hawai‘i, has prompted the development of an hydro-ecological model linking catchment or watershed development and disease risk (Kaneshiro et al., 2005) [Wilcox et al., in preparation]. A next step for research is to test and refine this model using quantitative real time PCR techniques (Smythe et al., 2002) combined with sequencing of leptospiral 16S ribosomal RNA genes [Ganoza and Vinetz, in preparation].
Hawai‘i Illustrates the Practical Utility of Transdisciplinary Approaches to Understand Leptospirosis Endemicity
The reported annual incidence in the United States ranged from 0.02–0.04 cases per 100,000 persons from 1985–1994. Hawai‘i reports the highest annual occurrence rate in the United States. Between June 1998 and February 1999, this state reported 405 suspected cases of leptospirosis; 61 of those cases were confirmed. Case numbers varied markedly from island to island within the state. Incidence rates ranged from 2.3–40.2 cases per 100,000 persons, with the highest numbers of cases on Kaua‘i and Hawai‘i. These reported cases contrast starkly with the prevalence rates found under active surveillance. Using active surveillance measures, Hawai‘i researchers projected the state’s true local incidence at approximately 128 cases per 100,000 persons. Major risk factors identified in Hawai‘i include the use of water catchment systems, wild pig hunting, and the presence of skin wounds (Lewin, 1987; Katz et al., 2002).
Despite nearly a century of research aimed at controlling the disease, leptospirosis remains a significant public health problem in Hawai‘i, where taro farmers (usually residents with Hawaiian or part-Hawaiian ancestry or Asian-Pacific Islanders who have lived in Hawai‘i for generations, often adopting Hawaiian lifestyles and language, and identifying as “locals”) and people who enjoy recreational freshwater activities (resident populations, visitors, and tourists) are the highest risk groups. Although leptospirosis is not a particularly high priority U.S. public health concern, it is for segments of the population in Hawai‘i, particularly given recent sentiments regarding regaining closer relationships to traditional land use activities, particularly wet taro farming.
Hawai‘i’s relatively high incidence of leptospirosis may be related to several factors, including its tropical climate, relatively high rainfall, and abundance of nonnative small mammal reservoir species with a lack of natural predators or competitors keeping them in check. Details of the mechanisms and dynamics of transmission, however, have imprecisely been determined, in particular the specific animals that result in human infection, and the role of anthropogenic influences on the environment in promoting transfer of pathogenic leptospires from infected animals to people. As is a general feature of environment-related diseases, the complex role of sociological and economic determinants leading to human infection by pathogenic Leptospira is poorly understood. One focus here is to describe the methodological approach that has developed, centered on Hawai‘i’s traditional “catchment” (watershed) basins, ahupua‘a, that conveniently represent distinct “model” socio-ecological systems (Kaneshiro et al., 2005), as well as the resulting insights applicable to research and understanding leptospirosis emergence in general.
Perspective on Leptospirosis Research in Hawai‘i
Leptospirosis has been studied in Hawai‘i for close to a century, beginning with initial discovery of the disease in the region (Katz et al., 2002), and, ultimately, studies of human disease and mammalian reservoirs of transmission including field sampling and pathogen isolation studies. The introduction of molecular methods to study environmental water sources and mammalian reservoirs of leptospiral transmission are adding an important dimension to this work, though as yet has only been used preliminarily in Hawai‘i. However, even with such laboratory technology advances, the problem has remained defined by classic epidemiology primarily relying on serology to identify human cases (Effler et al., 2002).
Although not described in such terms, two recent historically oriented studies demonstrated how leptospirosis in Hawai‘i has long been associated with specific social and ecological circumstances, dating to the first report of the disease in sugar cane workers in 1907. The combination of introduced Rattus species serving as effective reservoirs, irrigation water, and cuts and abrasions resulting from handling sugar cane, appear to have been responsible for the close association and emergence of leptospirosis in Hawai‘i. With the decline of plantation agriculture, leptospirosis primarily has become associated with taro farming and freshwater recreation (Middleton et al., 2001; Katz et al., 2002). The working group identified several key issues suggesting a renewed, and more ecologically and culturally oriented, research and prevention program was needed in Hawai‘i:
-
The perception that Leptospira contamination of streams and other freshwater environments has increased to a level making streams and other freshwater bodies unswimable—something middle-aged people growing up in Hawai‘i recall never having imagined decades ago.
-
The State Department of Health’s frequent posting of warning signage at specific streamside sites, after an outbreak possibly (but not known to be) due to exposure to contaminated water in the particular stream, may convey accurate risk exposure information—which many locals have come to ignore but may negatively impact Hawai‘i’s tourism industry.
-
The lack of public health infrastructure, including diagnostic and environmental detection methods—either for efficient diagnosis or environmental detection—to forensically link the two based on serological or molecular genetic tests.
-
The difficulty of confirming sites of leptospiral transmission or to determine the mammalian sources of contamination, pathway, and contributing environmental, hence, ecological, factors—such information would be essential as a basis for targeting sources, transmission pathways, or environmental factors to prevent disease.
-
The mammals suspected to be animal sources for leptospirosis transmission are also a major concern of scientists and wildlife conservationists attempting to protect Hawai‘i’s endangered plants and animals.
-
Many native Hawaiians have come to believe that leptospirosis poses a significant risk to their most sacred and historically economically important activity other than fishing: taro cultivation.
Framing Leptospirosis in a Social–Ecological Context
Leptospirosis in Hawai‘i is far more than a public health problem. Its emergence, and control, is inextricably tied to Hawai‘i’s cultural, historic, and contemporary aspects of environmental and natural resources management. Both in pre-European contact and contemporary Hawai‘i since the cultural renaissance of the 1970s, the geographically distinct mountain-to-sea ecosystem units characteristic of the Hawaiian Islands, called ahupua‘a, represent a common cultural context for environmental management activities (Kaneshiro et al., 2005). Besides an historic cultural significance that continues to be recognized by many Hawaiians, most of Hawai‘i’s towns and communities bear the names of the ahupua‘a in which they reside. Also, in a number of rural communities, native Hawaiians and groups of mixed ethnic (Pacific Islander, Asian, and European) descent cultivate wetland taro and are involved in cultural and ecological restoration activities centered on the ahupua‘a and associated values. Most notably these focus on restoring and maintaining what might best be described as a sustainable social–ecological system (Kaneshiro et al., 2005).
As a first step toward developing the project, ethnographic interview methods were used to explore community concerns and perceptions regarding leptospirosis as a foundation of the participatory research program (Appendix 1). The information gathered not only was helpful in confirming the community’s concerns, but also turned out to be remarkably helpful in framing our research, including generating a general disease ecology model toward understanding leptospirosis incidence. Taro farmers are an important part of this project, not only because they are considered to be at high risk for acquiring leptospirosis, but also because of their in-depth experience and close interaction with the biological and ecological factors thought to be related to the disease’s ecology.
Local Perceptions and Explanatory Model for Leptospirosis Transmission
Few people in communities understand the detailed microbiology regarding the etiology of leptospirosis. However, our interviews demonstrate that many did understand, in a loose sense, the association of leptospirosis with stagnant water and waters subject to contamination with the leptospirosis disease agent in proximity to domestic animals (cattle, pigs, dogs) and rodents, particularly rats. In general, leptospirosis is considered to be more of a threat to mainlanders and children (i.e., those with less previous exposure) than to taro farmers who have been around it and are more likely to develop resistance. The clinical symptoms of leptospirosis were understood to be similar to a flu-like illness. In contrast to other ailments commonly known to affect native Hawaiians, no traditional home remedies were generally considered to be useful for treating leptospirosis, suggesting that the recognition of leptospirosis, or even the presence of the disease, may be historically recent among native Hawaiians. In fact, because the mammalians species believed to be the major leptospiral reservoir hosts were introduced into Hawai‘i by Westerners, and the disease was first recognized in Hawai‘i in sugar cane workers, leptospirosis may not have been present in pre-contact Hawai‘i.
The perception of risk of leptospirosis was commonly considered to be increased now compared to “when we were kids” and people considered this to be connected to changes in environment—coffee farming, diversion of water, less rain, more invasive species (e.g., apple snails, Job’s tears, wild grass). Leptospirosis was considered to be a new occupational hazard and fact of life for taro farmers, a plight thought to be the result of external (i.e., nonnative Hawaiian) influences such as the importation of Western culture into Hawai‘i. Many felt that medical professionals (physicians and nurses) were not well informed on how to recognize leptospirosis, or on health education efforts required to protect people from contracting infection. Importantly, the new introduction of the fear of leptospirosis was considered to be a major problem because it keeps people away from cultural and healthful pursuits, i.e., traditional Hawaiian activities.
A common view expressed by taro farmers was that alterations in the environment are linked with ecological changes affecting conditions for wet taro farming. This included the perception that a healthy lo‘i has cool flowing water, is ecologically diverse (includes a variety of helpful plants and invertebrates besides taro) and helps channel rainfall, all to the benefit of a reduction of leptospirosis risk. Ecologists also recognize these characteristics necessary for a healthy ecosystem.
Issues of water rights as a collective good and community political power were prominently considered in relation to leptospirosis as well. It was commonly felt that water should not be diverted to plantations and that contaminated water outflows from farms with cattle should be monitored as critical measures in the control and prevention of leptospirosis. In contrast, while scientists view feral pigs as “rototillers of the forest” and disseminators of leptospires, the community members viewed pigs in a different context. As the centerpiece of a Hawaiian lū‘au (feast), kālua pig (pig cooked in an imu, underground earth oven) is viewed by native Hawaiian community members as valuable. Thus, there is an important disconnect between pigs as a known major reservoir of leptospirosis transmission and traditional views of pigs as part of a human–environment interaction. However, both scientists and local community members agree that leptospirosis is an indicator of poor ecological health. The traditional Hawaiian land division and natural resource management unit, the ahupua‘a, has served as a common organizational theme and reference. Assessing local knowledge and risk perception among taro farmers is a first step toward developing community participatory approaches to Leptospirosis control in ahupua‘a.
Land–Ocean Connections in Leptospirosis Transmission
Leptospirosis has been reported in three seal species that live along the Pacific coast of North America. The disease was first described in California sea lions (Zalophus californianus) along the California and Oregon coasts in 1970 (Vedros et al., 1971) during a major epizootic. Most descriptions of leptospirosis in pinnipeds are of Leptospira interrogans serovar Pomona. The antibody to serovar Pomona was associated with abortion, prematurity, and stillbirth (Smith et al., 1974a,b) on San Miguel Island. In Northern fur seals, the same agent was suggested to be responsible for a syndrome characterized by multiple hemorrhagic lesions in perinatal seals (Smith et al., 1974a,b). More recently, serovar Pomona has been responsible for three sea lion epizootics along the central California coast, characterized by a high prevalence (33%) of renal disease leading to death in over 70% of affected animals. A 1996 survey of 225 California sea lions found 38% of the animals to be positive, with the highest seroprevalence rates among subadult males (Colagross-Schouten et al., 1998). Positive titers to leptospiral serovars Bratislava, Hardjo, Icterohaemorrhagica, and Pomona were identified in monk seals at French Frigate Shoals, Kure Atoll, and Laysan in the Northwestern Hawaiian Islands (Aguirre et al., in press). Leptospirosis has not been documented in phocids until recently. High titers have been found in apparently healthy elephant seals (Gulland, 1999). The recent accounts of infection with renal disease due to serovar Grippotyphosa in both wild and captive Pacific harbor seals undergoing rehabilitation in close proximity with elephant seals and California sea lions (Stamper et al., 1998; Stevens et al., 1999) adds to the need to screen broadly across the serovars of this organism. However, as monk seals expand their numbers within the main Hawaiian Islands, the risk of getting the infection may increase. Recently, the first case of a monk seal dying of probable leptospirosis was documented. The potential risk of humans acquiring the disease from pinnipeds is evident. During the course of a 5-year study, three researchers became ill after exposure to California sea lions (Zalophus californianus) that were infected with Leptospira interrogans serovar Pomona (Vedros et al., 1971; Smith et al., 1974a,b).
The effects of ecological variables on the evolution of transmissibility and virulence, including the role of inter-serovar interaction at the “community” level (competition and genetic exchange) and at the “host level” (within host pathogen “ecology”) in relation to host immune response are unknown. The apparently clear-cut difference in infection response of maintenance hosts, which rarely exhibit the disease, and accidental hosts including naive wildlife (seals), domestic animals, and humans ranging from sub-clinical to fatal (Aguirre, 2000; Leighton and Kuiken, 2001; Meites et al., 2004; Aguirre et al., in press) suggests that substantial genetic variation in pathogen virulence exists. Infection or exposure rates have been found to be relatively high in maintenance and accidental hosts, including accidental wildlife hosts such as endangered Hawaiian monk seals. Also, multiple Leptospira serovars have been shown to exist within and among host species. The correlation between natural and anthropogenic environmental variables and variation in rates of disease incidence as well as the mechanisms underlying these associations need to be investigated further.
DISCUSSION: INTEGRATING OUR FINDINGSINTO A NEW RESEARCH AGENDA FORTRANSDISCIPLINARY RESEARCH INLEPTOSPIROSIS
Major gaps persist in understanding general principles and precise mechanisms of infectious disease emergence and reemergence. We suggest that these gaps persist because of “silo” effects that separate social sciences, ecological sciences, and mechanistic biomedical sciences into noninteracting disciplines. Bridging these gaps allows a higher understanding of complex processes affecting human health to begin to emerge. What emerged from our working group was an assessment of which disciplines were necessary to encompass the critical areas needed to effectively address mechanisms of leptospirosis emergence and reemergence (Table 2). We identified research needs and opportunities presented by leptospirosis and we expect that the outcome of this approach will be new scientific ideas and novel approaches and methods for EID research and their application to control and prevention.
This research agenda will include:
-
How do modern changes in Hawaiian watersheds affect leptospirosis transmission?
-
How has human alteration of the environment led to introduction of new leptospiral strains in relation to domesticated animals or peridomestic rodents?
-
How can environmental water sources be assessed for risk of leptospirosis transmission? How can such information be used for remediation?
-
How do introduced domesticated animals lead not only to environmental alterations but also to the introduction of new pathogens?
-
How do cultural imperatives have an impact on both disease understanding and approaches to amelioration of disease transmission?
-
How can anthropogenic effects on the environment lead to cross-species introduction of leptospires, such as the potential for the spread of leptospires from domesticated or human habitation-associated leptospires to marine mammals, or vice-versa?
These considerations have practical political, cultural, economic, and public health importance. For example, recent political efforts have been made for U.S. federal recognition of the special status of native Hawaiian’s rights and identity. Such efforts are exemplified by the increase in taro farming by native Hawaiians who seek increased connection with their cultural past. There is a clear relationship between wet taro farming and leptospirosis, yet we found strong feelings in local communities where taro farming is common that leptospirosis primarily affects nonnative Hawaiians. Modern watersheds have altered water flow patterns through lo‘i in which wet taro is grown, with the potential for increased leptospirosis transmission (Kaneshiro et al., 2005). Further, nonnative animals are present, bringing new infectious agents to contaminate the watershed. Similarly, leptospirosis is a major concern for tourists in Hawai‘i who are strongly warned by posted signs along rural streams and watersheds about the risk for leptospirosis. This situation certainly has a negative economic impact, suggesting that forces between scientists, public health officials, and businesses could be joined to address ways to assess the potential for leptospirosis transmission in rural water sources and ameliorate the conditions that lead to transmission.
Effective assessment of environmental surface waters, the most common source of leptospirosis transmission to humans, has not previously been done but new developments make such an approach feasible [Ganoza and Vinetz, unpublished data]. Such assessment would have substantial public health and sanitation importance and could be practically applied, for example, to remediation of Leptospira-contaminated streams in Hawai‘i, preventing leptospirosis after severe flooding, or interrupting outbreaks. One major impediment to such investigations is the difficulty of isolating fastidious pathogenic Leptospira from surface water sources in the presence of more rapidly growing saprophytic leptospires. Traditional methods of identifying Leptospira in environmental water and soil sources including culture and direct animal inoculation are time-consuming and laborious, and also run the risk of missing the bacteria altogether.
The need for transdisciplinary approaches to the study of leptospirosis is certainly not unique to Hawai‘i. In Peru, farmers are given domesticated livestock as an incentive for clearing tropical rain forest, including pigs, cattle, and imported Asian water buffalo. These animals not only are vectors for transmitting leptospires to the environment, but activities that lead to land clearance inevitably will lead to other unanticipated consequences, such as facilitating tropical viral emergence and reemergence, as has occurred with sylvatic yellow fever, alphaviruses, arenaviruses, etc. (Weaver et al., 2000; Moncayo et al., 2001; Travassos da Rosa et al., 2001; Bryant et al., 2003). Transdisciplinary approaches, incorporating the diverse disciplines and approaches outlined here specifically in reference to leptospirosis, should have broad applicability to understanding the mechanisms by which infectious diseases emerge and reemerge. At the same time, such approaches will point to strategies of control and remediation that will only become more important with increased globalization, urbanization, and anthropogenically driven environmental stress.
References
Aguirre AA (2000) Health assessment and disease status studies of the Hawaiian monk seal. NOAA NMFS Administrative Report U.S. Department of Commerce, NOAA, NMFS, Honolulu, Hawaii
Aguirre AA, Keefe TJ, Reif JS, Kashinsky L, Saliki JT, Stott JL, et al. (2005) Serological epidemiology of Hawaiian monk seals: the role of infectious disease monitoring in conservation. Journal of Wildlife Diseases (in press)
Barcellos C, Sabroza PC (2000) Socio-environmental determinants of the leptospirosis outbreak of 1996 in western Rio de Janeiro: a geographical approach. International Journal of Environmental Health Research 10:301–313
Barwick R, Mohammed H, McDonough P, White M (1997) Risk factors associated with the likelihood of leptospiral seropositivity in horses in the state of New York. American Journal of Veterinary Research 58:1097–1103
Barwick R, Mohammed H, McDonough P, White M (1998) Epidemiological features of equine Leptospira interrogans of human significance. Preventive Veterinary Medicine 36:153–165
Bernard HR (1995) Research Methods in Anthropology: Qualitative and Quantitative Approaches, Walnut Creek, CA: Alta Mira Press
Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. (2003) Leptospirosis: a zoonotic disease of global importance. Lancet Infectious Diseases 3:757–771
Bolin CA (2003) Leptospirosis. In: Fowler ME, Miller RE (editors), Zoo and Wild Animal Medicine St. Louis: Saunders, pp 699–702
Bryant J, Wang H, Cabezas C, Ramirez G, Watts D, Russell K, et al. (2003) Enzootic transmission of yellow fever virus in Peru. Emerging Infectious Diseases 9:926–933
Carroll AG, Campbell R (1987). Reproductive and leptospiral studies in beef cattle in central Queensland. Australian Veterinary Journal 64:1–5
Colagross-Schouten A, Mazet J, Chechowitz M, Gulland F, Hietala S (1998) The prevalence of Leptospira pomona in California sea lions (Zalophus californianus) along the California Coast, 1996. San Diego: IAAM
Correa MO (1975) Human leptospirosis in Brazil. International Journal of Zoonoses 2:1–9
Daszak P, Cunningham AA, Hyatt AD (2000) Emerging infectious diseases of wildlife—threats to biodiversity and human health. Science 287:443 –449
Daszak P, Cunningham AA, Hyatt AD (2001) Anthropogenic environmental change and the emergence of infectious diseases in wildlife. Acta Tropica 78:103–116
Davis A, Wagner JR (2003) Who knows? On the importance of identifying “experts” when researching local ecological knowledge. Human Ecology 31:463–489
Effler PV, Bogard AK, Domen HY, Katz AR, Higa HY, Sasaki DM (2002. Evaluation of eight rapid screening tests for acute leptospirosis in Hawaii. Journal of Clinical Microbiology 40:1464 –1469
Faine S, Adler B, Bolin C, Perolat P (1999) Leptospira and Leptospirosis, 2nd ed., Melbourne: Medisci
Gulland FMD (1999) Leptospirosis in marine mammals. In: Zoo & Wild Animal Medicine Current Therapy 4, Fowler ME, Miller RE (editors), Philadelphia: Saunders, pp 469–471
Johnson MAS, Smith H, Joseph P, Gilman RH, Bautista CT, Campos KC, et al. (2004) Environmental exposure and leptospirosis, Peru. Emerging Infectious Diseases. 10:1016–1022
Kaneshiro KY, Chinn P, Duin KN, Hood AP, Maly K, Wilcox BA (2005) Hawaii’s mountain-to-sea ecosystems: social-ecological microcosms for sustainability science and practice. EcoHealth 2 (DOI: 10.1007/s10393-005-8779-z, this issue)
Katz AR, Ansdell VE, Effler PV, Middleton CR, Sasaki DM (2002) Leptospirosis in Hawai’i, 1974–1998: epidemiologic analysis of 353 laboratory-confirmed cases. American Journal of Tropical Medicine and Hygeine 66:61–70
Ko AI, Galvao Reis M, Ribeiro Dourado CM, Johnson WD Jr, Riley LW (1999) Urban epidemic of severe leptospirosis in Brazil. Salvador Leptospirosis Study Group. Lancet 354:820–825
Kupek E, de Sousa Santos Faversani MC, de Souza Philippi JM (2000) The relationship between rainfall and human leptospirosis in Florianopolis, Brazil, 1991–1996. Brazilian Journal of Infectious Diseases 4:131–134
Leighton FA, Kuiken T (2001) Leptospirosis. In: Williams ES, Barker IK (editors), Infectious Diseases of Wild Mammals Ames, IA: Iowa State University Press, pp 498–502
Levett PN (2001) Leptospirosis. Clinical Microbiological Reviews 14:296–326
Lewin JC (1987). Leptospirosis in Hawai’i. Hawai’i Medical Journal 46:330
Lewis ND (2005) Is the social-ecological framework useful in understanding infectious diseases? The case of HIV/AIDS. EcoHealth 2 (DOI: 10.1007/s10393-005-8477-x, this issue)
Matsunaga J, Sanchez Y, Xu X, Haake DA (2005) Osmolarity, a key environmental signal controlling expression of leptospiral proteins LigA and LigB and the extracellular release of LigA. Infection and Immunity 73:70 –78
Meites E, Jay MT, Deresinski S, Shieh W-J, Zaki SR, Tomkins L, et al. (2004) Reemerging Leptospirosis, California. Emerging Infectious Diseases 10:406–412
Middleton CR, Ansdell VE, Sasaki DM (2001) Of mice and mongooses: a history of leptospirosis research in Hawaii. Hawaii Medical Journal 60:179–186
Miller D, Wilson M, Beran G (1991) Relationships between prevalence of Leptospira interrogans in cattle, and regional climactic, and seasonal factors. American Journal of Veterinary Research 52:1766–1768
Moncayo AC, Hice CL, Watts DM, Travassos de Rosa AP, Guzman H, Russell KL, et al. (2001) Allpahuayo virus: a newly recognized arenavirus (Arenaviridae) from arboreal rice rats (Oecomys bicolor and Oecomys paricola) in northeastern Peru. Virology 284:277–286
Murhekar MV, Sugunan AP, Vijayachari P, Sharma S, Sehgal SC (1998) Risk factors in the transmission of leptospiral infection. Indian Journal of Medical Research 107:218–223
Nally JE, Chow E, Fishbein MC, Blanco DR, Lovett MA (2005) Changes in lipopolysaccharide O antigen distinguish acute versus chronic Leptospira interrogans infections. Infection and Immunity 73:3251–3260
O’Fallon LR, Dearry A (2002) Community-based participatory research as a tool to advance environmental health sciences. Environmental Health Perspectives 110:155–159
Parkes M, Beinin L, Breilh J, Hsu L, Lebel J, McDonald M, et al. (2005) All hands on deck: A transdisciplinary, social-ecological systems-based approach to emerging infectious disease. EcoHealth 2 (DOI: 10.1007/s10393-005-8387-y, this issue)
Ramadass P, Jarvis BD, Corner RJ, Penny D, Marshall RB (1992) Genetic characterization of pathogenic Leptospira species by DNA hybridization. International Journal of Systematic Bacteriology 42:215–219
Rathinam SR, Rathnam S, Selvaraj S, Dean D, Rozik RA, Namperumalsamy P (1997) Uveitis associated with an epidemic outbreak of leptospirosis. American Journal of Ophthalmology 124:71–79
Sanders EJ, Rigau-Perez JG, Smits HL, Deseda CC, Vorndam VA, Aye T, et al. (1999) Increase of leptospirosis in dengue-negative patients after a hurricane in Puerto Rico in 1996. American Journal of Tropical Medicine and Hygiene 61:399–404
Segura E, Ganoza C, Campos K, Ricaldi JN, Torres S, Silva H, et al. (2005) Clinical spectrum of pulmonary involvement in leptospirosis in an endemic region, with quantification of leptospiral burden. Clinical Infectious Diseases 40:343–351
Sehgal SC (2000) Leptospirosis on the horizon. National Medical Journal of India 13:228–230
Sehgal SC, Vijayachari P, Murhekar MV, Sugunan AP, Sharma S, Singh SS (1999) Leptospiral infection among primitive tribes of Andaman and Nicobar Islands. Epidemiology and Infection 122:423–428
Sejvar J, Bancroft E, Winthrop K, Bettinger J, Bajani M, Bragg S, et al. (2003) Leptospirosis in Eco-Challenge athletes, Malaysian Borneo, 2000. Emerging Infectious Diseases 9:702–707
Smith AW, Brown RJ, Skilling DE (1974a) Naturally occurring leptospirosis in northern fur seals. Journal of Wildlife Diseases 13:144–148
Smith AW, Brown RJ, Skilling DE, DeLong RL (1974b) Leptospira pomona and reproductive failure in California sea lions. Journal of the American Veterinary Medical Association 165:996–998
Smythe LD (2001) Leptospirosis worldwide, 1999. Weekly Epidemiological Record 76:109–116
Smythe LD, Smith IL, Smith GA, Dohnt MF, Symonds ML, Barnett LJ, et al. (2002) A quantitative PCR (TaqMan) assay for pathogenic Leptospira spp. BMC Infectious Diseases 2:13–19
Stamper M, Gulland F, Spraker T (1998) Leptospirosis in rehabilitated Pacific harbor seals from California. Journal of Wildlife Diseases 34:407–410
Stevens E, Lipscomb TP, Gulland FMD (1999) An additional case of leptospirosis in a harbor seal. Journal of Wildlife Diseases 35:150
Travassos da Rosa AP, Turell MJ, Watts DM, Powers AM, Vasconcelos PF, Jones JW, et al. (2001) Trocara virus: a newly recognized alphavirus (Togaviridae) isolated from mosquitoes in the Amazon Basin. American Journal of Tropical Medicine and Hygiene 64:93–97
Trevejo RT, Rigau-Pérez JG, Ashford DA, McClure EM, Jarquín-González C, Amador JJ (1998) Epidemic leptospirosis associated with pulmonary hemorrhage-Nicaragua, 1995. Journal of Infectious Diseases 178:1457–1463
Trueba G, Zapata S, Madrid K, Cullen P, Haake D (2004) Cell aggregation: a mechanism of pathogenic Leptospira to survive in fresh water. International Microbiology 7:35–40
Vedros NA, Smith AW, Schonweld J (1971) Leptospirosis epizootic among California sea lions. Science 172:1250–1251
Vinetz JM, Glass GE, Flexner CE, Mueller P, Kaslow DC (1996) Sporadic urban leptospirosis. Annals of Internal Medicine 125:794–798
Ward M (2002) Seasonality of canine leptospirosis in the United States and Canada and its association with rainfall. Preventive Veterinary Medicine 56:203–213
Weaver SC, Salas RA, de Manzione N, Fulhorst CF, Duno G, Utrera A, et al. (2000) Guanarito virus (Arenaviridae) isolates from endemic and outlying localities in Venezuela: sequence comparisons among and within strains isolated from Venezuelan hemorrhagic fever patients and rodents. Virology 266:189–195
WHO (2001) Weekly Epidemiological Record 76:109–116
Wilcox BA, Colwell RR (2005) Emerging and reemerging infectious diseases: biocomplexity as an interdisciplinary paradigm. EcoHealth 2 (DOI: 10.1007/s10393-005-8961-3, this issue)
Wilcox BA, Gubler DJ (2005) Disease ecology and the global emergence of zoonotic pathogens. Journal of Environmental Health & Preventive Medicine 10:263–272
Acknowledgments
This work was supported by a conference grant from the U.S. Public Health Service, R13TW007300—NIH Roadmap initiative “Research Teams of the Future” (Principal Investigator, B.A.W.) and, in part, by U.S. Public Health Service grants R01TW005860, “Leptospirosis Transmission in the Peruvian Amazon,” and D43TW007120, “Endemic Infectious Diseases of the Peruvian Amazon” (Principal Investigator, J.M.V.). We thank Dr. Christian Ganoza for the photographs in Figures 1 and 2; and Kenneth Kaneshiro and Mike Kido for the photographs in Figure 3. We also are grateful to Kenneth Kaneshiro for his support of our field work in Hawai‘i through the University of Hawai‘i EPSCoR grant (NSF EPS-0237065). We thank Shannon Bennett, Yuko Chiba, Kristin Duin, Andrew Hood, Alan Tice, George Watt, Mayee Wong, and many other people participating in the Honolulu meeting for assistance with developing many of the ideas expressed in the article. Finally, we express Mahalo to the staff at Papa Lo‘i Kānewai at Kamakakuokalani, Center for Hawaiian Studies, University of Hawai’i for providing a tour of the lo‘i and sharing their knowledge of taro farming and cultivation with our group.
Author information
Authors and Affiliations
Corresponding author
APPENDIX 1: HAWAIIAN TARO FARMERS’ PERCEPTIONS RELATED TO LEPTOSPIROSIS TRANSMISSION
APPENDIX 1: HAWAIIAN TARO FARMERS’ PERCEPTIONS RELATED TO LEPTOSPIROSIS TRANSMISSION
Taro farmers responded to questions about the environmental and exposure risk factors associated with leptospirosis [L. Gollin, unpublished data]. Responses are part of a larger questionnaire and preliminary study and participatory research project on leptospirosis with wetland taro farmer communities on the island of Kaua‘i. Twenty-nine people either completed surveys (14), were interviewed at home or in their taro patches (15), or both (1). Length of interviews ranged from ½ to 2 hours.
I. Major Environmental Causes of Leptospirosis
Questions Asked
What are the main reasons for leptospirosis? Explain anything you know about what causes it and where it comes from, i.e., tell us what you know about the land, water, soil, animals, insects/bugs, plants, or anything else you can think of related to leptospirosis.
Response
Most farmers said that stagnant (low or no flow) water and runoff after a heavy rain, water contamination from animals, from cattle, rats, and pigs urinating in the water are the main causes of leptospirosis. Specific factors responsible for pathogen transmission mentioned (frequency factor was mentioned): stagnant/dirty water (28%); cattle (20%); rats and mice (19%); pigs (18%); cats and dogs (9%); other (4%); plants (2%).
Quotes
“When the river is dry and low, stay away.” “Stagnant water leads to lepto. Doctors say you get it from rats.” “Baloney. Nobody got it growing up! It’s from the cattle upriver.”
II. Relationship to Ecological Health of Wetland Taro Patches
Questions Asked
Describe a “healthy” lo‘i/taro pond (i.e., the water, ditches, soil, plants/weeds, animals, birds, insects, or anything else that you can think of) and, is a healthy lo‘i/taro pond more or less likely to have leptospirosis? Why or why not?
Response
Most said that cool, flowing water is most important for a healthy taro pond and that a healthy lo‘i is less likely to have leptospirosis. Only two people said a healthy lo‘i is not necessarily going to have less lepto; five were not sure.
Quotes
“Weeds keep the taro water cool.” “Fish, frogs, toads, ducks ...if you have a lot living in it, it’s not toxic. Smell the soil. Bad soil smells like methane gas and sulfur.” “If you keep your banks clean, free of weeds (there’s no place for the rats to live). It’s good for the lo‘i and there is less lepto.”
III. Preventive Measures
Question Asked
Do you do anything to keep from getting lepto or to help your family avoid leptospirosis? How do you help children to keep them from getting sick with lepto?
Response
The main preventive measures from most to least favored were to not go in the taro pond or swimming with an open cut, wear protective gear such as boots, gloves, or eye protection; avoid drinking the water from the taro pond, especially from the irrigation ditches; staying out of the water after a hard rain or flood; and washing immediately with soap after exposure to water in the taro patch. Five farmers said they do nothing to avoid getting leptospirosis. A few farmers noted that cuts from apple snails on the taro and handling certain weeds such a rice grass (Paspalum orbiculare) lead to leptospirosis. Children, in particular, should not drink from, or wade in, the irrigation ditch. However, a few farmers said that children should swim often to build up resistance to lepto.
Quotes
“We were born and raised in this valley. We built up a resistance drinking water from the stream. When we go hunting we don’t bring water...just drink from the fresh flowing streams.” “I now know not to wash my face in the ditch. I don’t thinks it’s in the lo‘i, it’s in the ditch from the cattle.” “When we were kids, if we had a cut we’d go to the ocean to dry the cut. Ocean water has iodine. Maybe that also protects people from lepto...we used to swim every day after work [and we didn’t get it]...Also, you’re less likely to get it if your immune system is strong.”
Rights and permissions
About this article
Cite this article
Vinetz, J.M., Wilcox, B.A., Aguirre, A. et al. Beyond Disciplinary Boundaries: Leptospirosis as a Model of Incorporating Transdisciplinary Approaches to Understand Infectious Disease Emergence. EcoHealth 2, 291–306 (2005). https://doi.org/10.1007/s10393-005-8638-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10393-005-8638-y