Abstract
Aim
Attempted suicide is one of the most important public health problems among preventable causes of mortality in the general population. Identifying risk factors for the prevention of suicide is a major public health goal. The aim of this study was to determine the annual rate of attempted suicide, related risk factors, and interventions, among referrals to emergency departments in the Sanliurfa province of southeastern Turkey.
Subjects and methods
Data were obtained from all emergency departments in the province based on the ‘Suicide Attempt Registry’ standardized records for the calendar year 2010. Socio-demographic characteristics, aetiology, psychiatric history, psychiatric consultations, and interventions were examined. The groups were analysed with the chi-square test; the significance level was set at p < 0.05.
Results
The annual rate of suicide attempts was 55.39 in 100,000 for the calendar year 2010. The rate was 3.47 times higher among women than men, and in particular 4.15 times higher for the 15–24 year age group among women than in men with the highest incidence of suicide attempts. The majority of cases were referred in April and May. Medication or toxic agent ingestions comprised 90.3 % of cases. The main reason for attempts was family problems or domestic violence among women, and economic hardships among men, and rates of physical and mental problems were similar for both sexes. Only 8.8 % of cases were subsequently referred for psychiatric consultation. Among cases with a prior suicide attempt history, 44.6 % had a reported psychiatric disorder.
Conclusion
The results of this investigation show that strengthening of surveillance and emergency healthcare systems, enhancement of mental health literacy, and inter-sector collaboration for development of community empowerment programmes are of vital importance for prevention of attempted suicide. The low rate of psychiatric referrals for subsequent intervention represented a major gap in urgent mental health services in the region.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, the WHO has estimated that suicide rates have shown a 60 % rise worldwide with nearly one million deaths from suicides each year. Strikingly, low and middle-income developing countries have accounted for 84 % of suicides (WHO 2012). Suicide is a well-recognised public health challenge ranking as the second leading cause of death for the 15–19 years age group, and one of three leading causes of death in the most economically productive 15–44 year age range (Patton et al. 2009). Experts emphasize the importance of a diathesis-stress explanation in theoretical formulations of suicide across the lifespan with predisposing biological factors (e.g., serotonin imbalance), pre-morbid personality (e.g., perfectionism, impulsivity), cognitive vulnerability (e.g., impaired social problem-solving), and exposure to negative life events (including both early and current life adversities), and co-occurring psychiatric and physical disorders (Maris 2002; Evans et al. 2004; Patel et al. 2012).
The literature also emphasizes the importance of attempted suicide as a serious and preventable public health problem (Maris 2002; Daigle et al. 2011). The annual rates of reported suicide attempts range from 2.6 to 1,100 in 100,000 (Welch 2001). Risk factors for attempted suicide include depression, bipolar and substance use disorders, family history of suicide, exposure to traumatic life experiences, unemployment, homelessness, social isolation, physical illness (such as cancer), and pesticide exposures (Blumenthal 1988; Welch 2001). Lack of availability and acceptance of mental health services in the community, and inability to seek care due to stigma and fear of labelling also compound the picture.
It is essential to develop and test strategies for prevention of attempted suicide based on a systematic evaluation of risk factors, prevailing community attitudes, and available community and social resources. Key steps in designing a public health response to prevention of suicide attempts include: (1) defining and monitoring the extent of the problem by assessing characteristics of individual, place, and time; (2) searching for the causes of problems to define groups at risk; and (3) designing and testing solutions for better application of interventions that can prove effective. The aim of the present study was to determine the epidemiologic characteristics of suicide attempts in Sanliurfa, a southeastern province in Turkey, for development of preventive measures in the future.
Materials and method
In this descriptive surveillance record-based study, an analysis was conducted of the Sanliurfa Provincial Health Directorate of Mental Health emergency services under the auspices of the Ministry of Health. The ‘Emergency Service Suicide Attempt Registry’ record forms were obtained from 11 provincial and one private hospital in the calendar year 2010. The data included characteristics of individual, place, and time, for each reported suicide attempt. Population information was obtained from the residence address-based registry of the Turkish Statistical Institute. Suicide attempts are reported to the registry by each hospital on a monthly basis. The registry record form was developed by the Ministry of Health Directorate and includes data on demographic and social characteristics of each individual, reasons for the suicide attempt, history of previous attempts, personal and family history of psychiatric disorders, and medical interventions. The study was carried out with the approval and cooperation of the Ministry of Health Provincial Directorate. Following the analysis of the forms, feedback meetings were held with all emergency service chiefs and the Ministry of Health Provincial Directorate Mental Health Department staff to plan registry-based studies. Data entry and analyses were carried out with SPSS 11.5 using the chi-square test and the t-test.
Results
Table 1 shows a total of 693 suicide attempt cases for the provincial population of 1,251,076 for the calendar year 2010. Of the total suicide attempters, 77.6 % were women, and 64.1 % were individuals in the 15–24 years age group; 53.7 % were single and 86.7 % were living in the city centre. Among individuals in this age group, 45.3, and 22.1 %, had primary and high school education, respectively.
Table 2 shows the incidence of suicide attempts according to sex and age groups. The total incidence of suicide attempts was 79.36 in 100,000 for women, and 22.83 in 100,000 for men. The combined incidence for both sexes was 55.39 in 100,000. Incidence among women had increased by 3.47-fold compared to men. There was also a 4.15-fold increase in the 15–24 year age group, compared to other age groups.
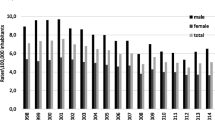
When the distribution of suicide attempts across calendar months were analysed, it was seen that 17.5 % of attempts took place in May, and 10.2 % of attempts took place in April; the figures for other months ranged from 3.4 to 9.4 % (Fig. 1). According to the distribution of days on which suicide was attempted, Monday was the most frequent, at 16.7 %, while the incidence of attempts on other days ranged between 12.3 and 14.9 %.
When methods of suicide attempt were examined, 90.3 % of the cases involved ingestions of medication or toxic substances. The remainder included exsanguinations (2.5 %), hanging (1.4 %), jumping from a height (0.6 %), use of a firearm (0.3 %), jumping under a moving vehicle (0.3 %), drowning (0.1 %), burning (0.1 %) and gassing (0.1 %). In 3.8 % of cases, the method remained unknown.
As seen in Table 3, 14.6 % of patients had a previous suicide history, 18.3 % had a psychiatric history, and 18.0 % of the patients had received psychiatric treatment in 6-months prior to the event.In the analysis of the 101 cases with a previous history of suicide attempt, 44.6 % had a history of psychiatric disorder, whereas this rate was 12.7 % for cases with no history of a previous suicide attempt. There was a statistically significant relationship between suicide attempt and a previous history of psychiatric disorder (Chi-square = 61.18; df = 4; p = 0.001). As noted in Fig. 2, 8.8 % of patients received psychiatric consultation. A statistically significant relation between psychiatric consultation request and a previous history of suicide attempt was found with 26.2 % of cases with a previous history of suicide attempt being referred to psychiatry clinics (Chi-square = 15.47; p = 0.001).
The most frequent reasons for suicide attempts were conflict within the family (27.8 %) followed by physical or mental disorder (20.3 %), although endorsement of conflict within family was higher for women than men (29.7 vs. 21.3 %); likewise a higher proportion of women endorsed domestic violence as a cause than men (8.9 vs. 3.9 %; Table 4).
Discussion
The annual rate of attempted suicide based on the Emergency Service records in the Sanliurfa province was 55.39 in 100,000. A review of the literature on field studies of parasuicide that comprise suicide attempts in the general population report annual rates ranging from 2.6 to 1,100 in 100,000 (Welch 2001). The data collection on suicide attempt behaviours however remain poor and an accurate estimation of the true incidence is therefore highly likely to be biased due to various religious norms and cultural beliefs as well as socio-political or economic constraints. Nonetheless, several countries have established national prevention strategies that focus on individuals in known high-risk groups, and strategies aimed at prevention in the general population (Daigle et al. 2011; Hawton et al. 2012; Patel et al. 2012; Philips et al. 2012).
Individual characteristics of attempted suicide
Number of findings is highlighted by Sanliurfa study. First, the attempted suicide rate was 3.47 fold more common among women than in men; this finding supports previous research findings that women are a priority risk group for suicide attempts (Devrimci-Ozguven and Sayıl 2003; Zhang et al. 2005; Borges et al. 2010). This is not surprising given that social and economic disadvantages experienced by many women in both high-income developed, as well as low- and middle-income developing countries, along with reported higher rates of anxiety and depression among women compared to men, are common knowledge (Maselko and Patel 2008). In the southeastern Anatolia Region today there is still a prevailing feudal-like ideology that assigns a central role to the male. Such a predominant tribal leadership system emphasizes male head of households and blood ties, over choice and gender equality; this is also reflected in a persistent disparity in the poor literacy and educational level of girls and women in the region. Consanguineous marriages (50–63.6 %) and adolescent marriages (45–98.5 %) are common and gender inequality is an insurmountable problem, although improving over the past decade (Okten 2009). In particular, for the age group of 15–49 years, and for women in general, attention to mental illness and evaluations of prior histories of suicide attempts needs to be an integral part of health screening. At the present time, such counselling services are primarily the responsibility of family physicians with limited mental health training. Therefore, the promotion of gender equality needs to be taken into consideration when designing preventive strategies that will seek to integrate mental health and counselling services within primary healthcare.
Second, the age group with the highest incidence of suicide attempts among both women and men was the 15–24 year age group, consistent with results of other field studies (Welch 2001; Maris 2002; Bridge et al. 2006; Borges et al. 2010; Patel et al. 2012). The clustering of suicide attempts within this 15–24 year age group may have different explanations, such as the negative effects of social change in society, or the challenging life conditions facing youth (Evans et al. 2004). Geller et al. (2001) reported that the adolescent period is more risky in the context of depressive and other emotional disorders. Due to the fact that physical disorders are less likely in the adolescent period, referral to the hospital is less likely, and therefore in-school health services such as mental health screening programmes and educational programmes to increase the awareness of suicide can be useful.
Third, the present study underscores that the most common contributors to suicide attempts include a combination of social problems such as interpersonal, family, and financial difficulties, again as also reported in previous field studies (Welch 2001). Such adversities are often first to emerge among families in conflict, and in the present study had a higher ranking than physical or mental disorders as a reported cause. In the Sanliurfa province in southeastern Turkey with well-recognized gender disparities, women reported conflict in the family as their top reason for suicide attempts; in fact, when the conflict in the family is combined with domestic violence these two causes represent 38.6 % of suicide attempts among women. Women reported economic problems as their least common reason for suicide attempts (1.1 %). In contrast, men endorsed economic problems at a higher ranking (8.4 %) than domestic violence (3.9 %).
Fourth, the suicide attempt rate among single persons was highest for both sexes in this study. There is strong empirical support for this prevailing idea that being single, or divorced, may serve as a risk factor for attempted suicide (Welch 2001; Maris 2002; Borges et al. 2010). Low socio-economic status, including low levels of education, has also been examined as a risk factor for attempted suicide (Welch 2001; Hawton et al. 2003; O’Loughlin and Sherwood 2005; Zhang et al. 2005). This could be explained by the absence of limited education, problem-solving skills, lack of awareness of psychosocial problems, and poor living conditions. Another risk factor is living in an urban area. Urban residents have long been considered as more vulnerable to mental problems than rural ones (Maselko and Patel 2008); however, there is additional data suggesting that socio-demographic factors are better predictors than location of residence (Judd et al. 2002). Therefore, the integration of mental health services within both general and primary healthcare services provided in the urban and rural settings based on the socio-demographic characteristics of population is a matter of great importance.
Fifth, co-existing mental illness, prior history of suicide attempts, insufficient psychiatric treatment, and even types of antidepressants used, are known risk factors in individuals who attempt suicide. In this study, 18.3 % of patients had a prior psychiatric history, and 4.8 % of case families had previous mental illness; 14.6 % of patients had a history of previous suicide attempts. These findings are compatible with those reported by other studies (Welch 2001; Maselko and Patel 2008; Ono et al. 2008; Borges et al. 2010; Mandour 2012; Patel et al. 2012). It has been well reported that incidence of suicide among patients with psychiatric disorders is increased by up to 5–40 times, each completed suicide case corresponds to 6–25 repeated suicide attempts (Maris 2002; Yamada et al. 2007). In a prospective follow-up study by Christiansen and Jensen (2007), the risk of repetition of suicide attempts in patients with a prior history of suicide attempt was increased 37.34 %, and mortality was increased four-fold, compared to other groups.
Time and methods of suicide attempts
First, the findings of the present study show that the incidence of suicide attempts increased in April and May across the calendar year. In the southeastern Anatolia region, in particular April–June is a time for agricultural pesticide application in cotton fields. A literature review reveals a statistically significant correlation between the prevalence of pesticide use and suicide attempt (Pine et al. 1995; Chowdhury et al. 2010; Parrón et al. 2011). It is therefore important to investigate the relation between suicidal behaviour and pesticide use and to identify the relevant risk groups. When the data were analysed further, most of the attempted suicides were seen to have occurred on Monday. In other studies, Mondays were also reported to be the most common day for suicide attempts, a situation explained by the ‘Monday effect’ for suicide. A foundation for this has been hypothesized to be the transition from weekend to the working week—that ‘Monday-morning feeling’ (Johnson et al. 2005). It is not possible to explain the reason for this in the present study, as the majority of women were housewives, nevertheless further research needs to elucidate this finding.
Second, most of the suicide attempts were done with ingestion of medications or toxic agents. This finding is compatible with prior literature (Christiansen and Jensen 2007; Mandour 2012). One important population strategy to reduce suicides is the modification of the local environment to decrease general access to toxic agents as prevailing method for suicide attempt. This approach (so-called means restriction) is reported to be one of the intervention measures with the strongest empirical support.
Psychiatric consultation in emergency departments
A major finding of the present study is the very low proportion, less than 1 in 10 of persons who attempted suicide who were referred for psychiatric consultations through the emergency services. Relatively low rate of psychiatric referral and consultation is reported in the literature in the management of suicide attempts (Runeson and Wasserman 1994). In the present study in southeastern Turkey, the rate of psychiatric referral was strikingly poor. This also reflects the additional paucity of psychiatric services with particularly low representation of psychiatric caregivers regionally. Despite an attempt made by the Ministry of Health to institute mandatory assignment of graduating specialists to address regional disparities the situation of psychiatric care in the region remains limited. However, the period following a suicide attempt represents an important window of opportunity in the immediate aftermath of an incident to provide urgent care that includes access to mental health services that will enable longer-term interventions, and most importantly, prevent a repeat occurrence. Despite these difficulties, it was encouraging to note a higher rate of referral (more than 1 in 4) among those with prior history of suicide attempt. This provides hope that improvement is possible with greater awareness. Therefore systematic and institutional steps are also needed to increase awareness among emergency staff and encourage them to refer individuals for appropriate mental health services.
Limitations
The present study should be considered in the light of a number of limitations. First, the results are not indicative of the overall public health situation for attempted suicides in Turkey. Second, the study concerned hospital-based emergency services in Sanliurfa province and could underestimate the rate of suicide attempts within the province. Stigma and fear due to religious and cultural beliefs may prevent especially non-serious cases from reaching emergency services. Similarly hospital managers may not have reported some cases to the directorate for similar reasons, although such reporting is mandated by the Ministry of Health. The low literacy and educational level of women and working conditions in the fields may also have affected access to emergency healthcare services. The majority of population in the region are seasonal migratory farmworkers. They are characterized by lower education, larger household size, larger number of children per family, greater poverty, and greater likelihood of environmental exposures to pesticides (Simsek et al. 2012). Finally, additional limitation was the cross-sectional nature of the design of the study examining risk factors, not causality. Nonetheless, despite all these limitations, the study represents a systematic evaluation of emergency surveillance data regarding suicide attempts, collected using standardized forms with cooperation of the Ministry of Health. It is likely that a majority of the cases of attempted suicides in the province were accounted for. The study is also a unique effort for a disparate region in Turkey and represents the largest such evaluation of suicide attempts, to date, in the country. A strong endorsement of the validity of the results of the present is study is that it is highly consistent with prior studies, including the question as to the day of the week when the suicide attempts peaked, but further research is needed to address as to why this is true in Sanliurfa.
Conclusions
The present study highlights a number of risk factors for attempted suicide that includes: younger age, female gender, being single, co-existing physical or mental disorder, as well as reported conflict within the family, domestic suicide and economic hardship. The low rate of implementation of psychiatric referral measures highlighted by this study reflects a profound disparity as recognized by World Health Organization in the Mental Health and Gap Action Programme (mhGAP) (WHO 2010). This disapirty between what is urgently needed and what is available to reduce the burden of suicide attempts in Sanliurfa is still very considerable.
There is an urgent need for development of simple evaluation tools in the context of primary care by practitioners for assessing and monitoring suicide risk factors and orienting patients for appropriate mental health services (Perogamvros et al. 2010). This approach needs to be linked to an integrated public health effort to educate primary and emergency care staff to better define important target groups for psychiatric emergency outreach. Such a linkage is particularly salient in Turkey with an important network of provincial primary care services that traditionally lacked a mental health component (Ministry of Health 2006). Studies also suggest that suicidal individuals referred to psychiatric services following such an evaluation do not necessarily always follow up and receive the planned treatment (Nordentoft 2007). Therefore emergency and primary care public health facilities need to adopt a more assertive approach to psychiatric care of suicide attempters. Additional recommended public health and medical educational approaches include: (1) enhanced surveillance systems to gather and analyse data for identification and monitoring of risk groups; (2) intersectorial approaches to reduce gender inequality and family conflict; (3) undergraduate medical education and in-service training for primary healthcare and emergency department staff to provide better mental health screening and management attempted skills especially targeting the 15–49 year age group; and (4) community empowerment programmes in peer education and development of mental health leadership. All these domains are likely to be of vital importance for prevention and intervention measures in attempted suicide.
References
Blumenthal SJ (1988) Suicide: a guide to risk factors, assessment, and treatment of suicidal patterns. Med Clin North Am 72(4):937–971
Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, Andrade LH, Angermeyer MC, Beautrais A, Bromet E, Bruffaerts R, de Girolamo G, Florescu S, Gureje O, Hu C, Karam EG, Kovess-Masfety V, Lee S, Levinson D, Medina-Mora ME, Ormel J, Posada-Villa J, Sagar R, Tomov T, Uda H, Williams DR, Kessler RC (2010) Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization world mental health surveys. J Clin Psychiatry 71(12):1617–1628
Bridge JA, Goldstein TR, Brent DA (2006) Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry 47(3–4):372–394
Chowdhury AN, Banerjee S, Brahma A, Das S, Sarker P, Biswas MK, Sanyal D, Hazra A (2010) A prospective study of suicidal behaviour in Sundarban Delta, West Bengal, India. Natl Med J India 23(4):201–205
Christiansen E, Jensen BF (2007) Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysis. Aust NZ J Psychiatry 41(3):257–265
Daigle MS, Pouliot L, Chagnon F, Greenfield B, Mishara B (2011) Suicide attempts: prevention of repetition. Can J Psychiatry 56(10):621–629
Devrimci-Ozguven H, Sayıl I (2003) Suicide attempts in Turkey: results of the WHO-EURO multicentre study on suicidal behaviour. Can J Psychiatry 48(5):324–329
Evans E, Hawton K, Rodham K (2004) Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clin Psychol Rev 24(8):957–979
Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL (2001) Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry 158(1):125–127
Hawton K, Harriss L, Hall S, Simkin S, Bale E, Bond A (2003) Deliberate self-harm in Oxford, 1990–2000: a time of change in patient characteristics. Psychol Med 33(6):987–995
Hawton K, Saunders KE, O'Connor RC (2012) Self-harm and suicide in adolescents. Lancet 379(9834):2373–2382
Johnson H, Brock A, Griffiths C, Rooney C (2005) Mortality from suicide and drug-related poisoning by day of week in England and Wales, 1993–2002. Health Stat Q 27:13–16
Judd F, Murray G, Fraser C, Humphreys J, Hodgins G, Jackson H (2002) The mental health of rural Australians: developing a framework for strategic research. Aust J Rural Health 10(6):296–301
Mandour RA (2012) Antidepressants medications and the relative risk of suicide attempt. Toxicol Int 19(1):42–46
Maris RW (2002) Suicide. Lancet 360:319–326
Maselko J, Patel V (2008) Why women attempt suicide: the role of mental illness and social disadvantage in a community cohort study in India. J Epidemiol Community Health 62(9):817–822
Ministry of Health (2006) National mental health policy for the Republic of Turkey. Ministry of Health, Ankara, Turkey, pp 191
Nordentoft M (2007) Prevention of suicide and attempted suicide in Denmark: epidemiological studies of suicide and intervention studies in selected risk groups. Dan Med Bull 54(4):306–369
Okten S (2009) Gender and power: the system of gender in southeastern Anatolia. J Int Soc Res 2(8):302–312
O’Loughlin S, Sherwood J (2005) A 20-year review of trends in deliberate self-harm in a British town, 1981–2000. Soc Psychiatry Psychiatr Epidemiol 40(6):446–453
Ono Y, Kawakami N, Nakane Y, Nakamura Y, Tachimori H, Iwata N, Uda H, Nakane H, Watanabe M, Naganuma Y, Furukawa TA, Hata Y, Kobayashi M, Miyake Y, Tajima M, Takeshima T, Kikkawa T (2008) Prevalence of and risk factors for suicide-related outcomes in the World Health Organization world mental health surveys Japan. Psychiatry Clin Neurosci 62(4):442–449
Parrón T, Requena M, Hernández AF, Alarcón R (2011) Association between environmental exposure to pesticides and neurodegenerative diseases. Toxicol Appl Pharmacol 256:379–385
Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, Suraweera W, Jha P, Million Death Study Collaborators (2012) Suicide mortality in India: a nationally representative survey. Lancet 379(9834):2343–2351
Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, Vos T, Ferguson J, Mathers CD (2009) Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 374:881–892
Perogamvros L, Chauvet I, Rubovszky G (2010) When should a patient in suicidal crisis be referred to the emergency ward (in French)? Rev Med Suisse 6(259):1555–1557
Pine DS, Trautman PD, Shaffer D, Cohen L, Davies M, Stanley M, Parsons B (1995) Seasonal rhythm of platelet [3H] Imipramine binding in adolescents who attempted suicide. Am J Psychiatry 152(6):923–925
Runeson B, Wasserman D (1994) Management of suicide attempters: what are the routines and the costs? Acta Psychiatr Scand 90(3):222–228
Simsek Z, Koruk I, Doni NY (2012) An operational study on implementation of mobile primary healthcare services for seasonal migratory farm workers, Turkey. Matern Child Health J16(9):1906–1912
Welch SS (2001) A review of the literature on the epidemiology of parasuicide in the general population. Psychiatr Serv 52(3):368–375
World Health Organization (2010) mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings. WHO, Geneva, 107 pp
World Health Organization (2012) Public health action for the prevention of suicide: a framework. WHO, Geneva
Yamada T, Kawanishi C, Hasegawa H, Sato R, Konishi A, Kato D, Furuno T, Kishida I, Odawara T, Sugiyama M, Hirayasu Y (2007) Psychiatric assessment of suicide attempters in Japan: a pilot study at a critical emergency unit in an urban area. BMC Psychiatry 7(7):64–70
Zhang J, McKeown RE, Hussey JR, Thompson SJ, Woods JR (2005) Gender differences in risk factors for attempted suicide among young adults: findings from the Third National Health and Nutrition Examination Survey. Ann Epidemiol 15(2):167–174
Acknowledgements
The authors thank the Şanlıurfa Health Directorate, Mental Health Division, for giving permission to analyse suicide surveillance data, and the D43 TW005807 Fogarty/NIH ICOHRTA grant from Children’s Hospital Boston (KM).
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simsek, Z., Demir, C., Er, G. et al. Evaluation of attempted suicide in emergency departments in Sanliurfa province, southeastern Turkey. J Public Health 21, 325–331 (2013). https://doi.org/10.1007/s10389-013-0558-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-013-0558-7