Abstract
Background
Several studies have demonstrated that prehabilitation helps reduce the incidence of postoperative complications. In this study, we investigated the safety and efficacy of enhanced prehabilitation (EP) in the hospital for patients with esophageal cancer.
Methods
We retrospectively reviewed the data of 48 consecutive patients who underwent radical esophagectomy with gastric tube reconstruction between September 2015 and June 2019. EP program had been introduced in August 2017. In the EP group, patients received the EP program during hospitalization 7 days before surgery in addition to conventional perioperative rehabilitation. The EP program consisted of aerobic exercise and muscle strength training in the morning and afternoon. Operative outcomes were compared between patients who received EP (EP group; 23 patients) and patients who did not receive EP (control group; 25 patients).
Results
The preoperative (EP group vs. control group, 492.9 ± 79.7 vs. 418.9 ± 71.8 m, p < 0.001) and postoperative (EP group vs. control group, 431.5 ± 80 vs. 378 ± 68.7 m, p < 0.001) 6-min walk distance was significantly higher in the EP group than in the control group. The respiratory complications rate was significantly lower in the EP group (4.3%) than in the control group (36%) (p = 0.007). The incidence of atelectasis was particularly significantly lower in the EP group (0%) than in the control group (24%) (p = 0.012).
Conclusions
EP was performed safely for patients before esophagectomy. EP improved the exercise tolerance of the patients before esophagectomy and might be useful in preventing respiratory complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Postoperative complications after radical esophagectomy lead to prolonged hospital stay and deterioration of physical strength and quality of life [1]. In particular, studies have reported that respiratory complications, including pneumonia, occurred at a rate of 15.4–38.1% after esophagectomy [2, 3], which in turn worsened the overall survival of patients after esophagectomy [4]. Deciding the perioperative counterplan for preventing such complications remains an important problem that we need to overcome.
We introduced perioperative rehabilitation and intervention with multidisciplinary support team step-by-step for preventing postoperative complications in patients who previously underwent esophagectomy [5]. Although perioperative rehabilitation prevented the progression and prolongation of pneumonia and shortened postoperative hospitalization, the incidence of pneumonia was not reduced by previous interventions including preoperative rehabilitation in the outpatient ward. In our previous rehabilitation program, the contents of preoperative training program were not clearly established; nonetheless, postoperative early ambulation and perioperative respiratory rehabilitation were enhanced. Simultaneously, patients were advised to perform self-training with walking and squat; however, their degree of achievement of the aim was not evaluated.
Prehabilitation is a preoperative exercise program aimed at increasing the perioperative functional reserve of an individual to enable him or her withstand the upcoming surgical stress and to accelerate the postoperative functional recovery [6]. Several studies have demonstrated that prehabilitation helps reduce the incidence of postoperative complications in patients undergoing lobectomy and upper abdominal surgery [7, 8]. For instance, Soares et al. reported that patients who received physical therapy with respiratory and global exercises before surgery showed better results in the 6-min walk distance (6MWD) test measuring exercise tolerance on the seventh postoperative day (POD) and also had lower incidence of postoperative pulmonary complications following upper abdominal surgery compared to control group. Other studies have examined the usefulness of prehabilitation in esophagectomy [9,10,11]. For example, Minnela et al. reported that functional outcomes in preoperative and postoperative 6MWD changes had improved in the prehabilitation group; however, there were no significant differences in postoperative complication rates and severity in comparing to the control group [9]. However, whether prehabilitation reduces postoperative morbidities in esophagectomy remains controversial [9, 11].
In previous studies, prehabilitation training was primarily performed under self-training at home during the outpatient period [9, 11]. However, it was difficult to confirm that patients accomplished self-training and to assess of the quality in of their home training. Moreover, periodic rehabilitation in the outpatient ward may be impractical when the patient’s home is distant from the hospital. For these reasons, we introduced enhanced prehabilitation (EP) during hospitalization in which the patients received intensive aerobic and muscle training exercise, in addition to conventional interventions, to improve exercise capacity and muscle strength begining 7 days before surgery for all patients scheduled for thoracic esophagectomy. The postoperative adverse effects of EP creating a load on cardiopulmonary function for patients scheduled for surgery was a concern. In this study, we investigated the safety and efficacy of EP for patients with esophageal cancer.
Methods
Patients
We retrospectively reviewed the data of 48 consecutive patients with esophageal squamous cell carcinoma who underwent radical esophagectomy with gastric tube reconstruction at the Department of Surgery, Iwate Medical University Hospital, between September 2015 and June 2019. The practice of EP was initiated in August 2017. Operative outcomes were compared between patients who received EP (EP group; from August 2017 to June 2019) and patients who did not receive EP (control group; from September 2015 to July 2017). Table 1 shows the clinical characteristics of the patients. The tumor location was classified according to the Japanese Classification of Esophageal Cancer, 11th edition [12]. Clinical and pathological stage was determined according to the classification of the Union for International Cancer Control, 8th edition [13]. Neoadjuvant chemotherapy was administered to patients with stage II/III squamous cell carcinoma as previously reported [14].
Thoracoscopic esophagectomy was performed in the prone position [15]. For all patients, the reconstruction conduit was a gastric tube pulled through the posterior mediastinum or retrosternal route with cervical esophagogastrostomy [16]. Perioperative management and nutritional treatment approaches have been described previously [5, 17]. In this study series, all the patients did not receive enteral nutrition after surgery instead they received Ringer’s acetate and amino acid solution via peripheral intravenous catheters [17].
Enhanced prehabilitation
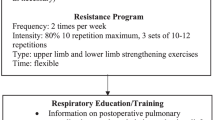
For the patients in the control group, inspiratory muscle training (IMT) with incentive spirometry was started in the outpatient department approximately 1 month before for the planned surgery (Fig. 1). The IMT consisted of four to five sets of ten deep inspirations per day. The patients were advised to commence self-training with walking for 20 min and performing 20 sets of squats 10 times per day. They were admitted to the hospital 3 days before surgery. The patients in this group did not receive planned training between admission and operative day. After surgery, on POD 1, they began early mobilization with ambulation, respiratory training, and training for chewing and swallowing. All patients stayed in the intensive care unit until POD 4. When they were moved to the surgical ward on POD 4, they were able to walk freely in the hospital. The patients practiced exercise in the rehabilitation room twice a day, morning and afternoon after POD 5; the training consisted of cycling ergometer for 20–30 min, IMT with incentive spirometry, and walking training, with two sessions each per day.
In the EP group, patients received the EP program during hospitalization 7 days before surgery in addition to conventional perioperative rehabilitation in the outpatient department approximately 1 month before for the planned surgery similar to that in the control group (Fig. 1). The EP program consisted of aerobic exercise and muscle strength training in the morning and afternoon. The aerobic exercise training consisted of cycling ergometer for 20–30 min twice per day at 60–70% of maximum heart rate. The muscle strength training for lower limbs consisted of 20 sets of squats each performed 10–15 times at a frequency of twice per day. Patients in both groups received all exercise training under the supervision of a physiotherapist in the hospital. On the contrary, in the outpatient department training, the implementation status of self-trained prehabilitation and the degree of achievement of the aim were not regularly evaluated in both groups. Postoperative rehabilitation program in the EP group was similar to that in the control group. During rehabilitation training, patient’s heart rate, blood pressure, oxygen saturation, and onset of new arrhythmia were monitored. Rehabilitation training was terminated when tachycardia (> 180 beats per minute), bradycardia (< 40 beats per minute), systolic arterial pressure decreased to < 80 mmHg or increased to > 40 mmHg from the resting period, or < 90% oxygen desaturation was observed. Patients were also monitored for new onset of chest pain, respiratory discomfort, and physical pain.
Outcome measures
The 6MWD, bilateral handgrip, and knee extensor muscle strength were measured on admission (only in the EP group), preoperatively (1 day before surgery), and postoperatively (scheduled before the patients left the hospital, approximately POD 10–15). Postoperative morbidity and mortality rates and postoperative hospital stay were compared between the two groups. The 6MWD was measured using the 6MWD test according to the guidelines of the American Thoracic Society [18]. Handgrip and knee extensor muscle strength were assessed using a digital dynamometer. Postoperative complications were defined according to classifications of the Esophagectomy Complications Consensus Group [1]. Atelectasis included all cases confirmed by X-rays that were examined routinely twice per day on PODs 1–4, and once on POD5 and 7. Atelectasis was diagnosed by loss of volume of lobe or lobar segment including sign such as displacement of the interlobar fissure, increase in the hemidiaphragm and mediastinal shift, and silhouette sign [19]. If pleural effusion was identified, differential diagnosis of pleural effusion and atelectasis was made via ultrasonography. Complication grades were defined according to the Clavien–Dindo classification [20].
Statistical analysis
Statistical analyses were performed using SPSS software (version 23.0; IBM-SPSS, Inc., Armonk, NY, USA). Between-group differences in patient characteristics and outcomes were assessed using the chi-squared test, Student’s t test, or Mann–Whitney U test. The p values for multiple comparisons of correlated data in the 6MWD of the EP group were adjusted for multiplicity using the Tukey–Kramer test. p < 0.05 was considered to statistically significant.
Results
The clinical characteristics of the patients are shown in Table 1. There were no significant between-group differences in age, sex, body mass index, tumor location, clinical and pathological stage, preoperative treatment, the American Society of Anesthesiologists performance status, comorbidities, respiratory function, and surgical procedures (Table 1). Although 16 patients (69.6%) had comorbidities in the EP group, there were no exercise-related adverse events during perioperative rehabilitations. All patients in the EP group were able to accomplish a planned program.
Table 2 shows the functional outcomes in the EP group. The preoperative (EP group vs. control group, 492.9 ± 79.7 vs. 418.9 ± 71.8 m, p < 0.001) and postoperative (EP group vs. control group, 431.5 ± 80 vs. 378 ± 68.7 m, p < 0.001) 6MWD was significantly higher in the EP group than in the control group. The rate of change between preoperative and postoperative 6MWD was not significantly different between the two groups. No significant differences were also found in the handgrip or knee extensor muscle strength before and after surgery between the two groups.
The mean 6MWD values in both groups are shown in Fig. 2. There was a significant increase in the 6MWD after EP (492.9 ± 79.7 m) compared to that at admission (448.8 ± 81.5 m; p < 0.000). Although the value of 6MWD decreased significantly after surgery (431.5 ± 80 m) comparing to that before surgery (492.9 ± 79.7 m; p < 0.000), the same level was maintained as that recorded at admission (p = 0.941).
Details of postoperative morbidities are presented in Table 3. The overall complication rates in the EP and control groups were 34.8% and 44%, respectively (Table 3). Although between-group difference was not observed in overall morbidity rates, the rate of respiratory complications was significantly lower in the EP group (4.3%) than in the control group (36%) (p = 0.007). In particular, the incidence of atelectasis was significantly lower in the EP group (0%) than in the control group (24%) (p = 0.012). We did not perform preventive mini-tracheostomy for all patients. Among the six patients with atelectasis in the control group two developed pneumonia; one underwent tracheostomy and the other underwent mini-tracheostomy via cricothyrotomy. No patients underwent tracheostomy or mini-tracheostomy in the EP group. The operative mortality rate was zero in both groups.
Results of postoperative blood tests conducted after surgery and at postoperative month (POM) 3 and POM 6 are shown in Table 4. Regarding total protein, the value at POM 6 was significantly higher in the EP group than in the control group (6.9 vs. 6.6 g/dL, p = 0.028). Postoperative maximum values of total bilirubin (0.8 vs. 1.2 mg/dL, p = 0.013) and blood urea nitrogen (BUN; 19.7 vs. 22 mg/dL, p = 0.044) on POD 7 were significantly lower in the EP group than in the control group. In terms of body weight loss after surgery, there was no significant difference in rate of weight loss at discharge, postoperative 3 month, and postoperative 6 month compared with body weight at operation in both groups. No significant differences between the two groups were observed in the length of hospital stay after surgery (Table 4).
Discussion
Several studies have demonstrated that intensive preoperative physical therapy performed for short periods reduced the incidence of postoperative morbidities or the length of hospital stay in patients undergoing esophagectomy and lobectomy [11, 21]. However, there is insufficient knowledge regarding the appropriate training period, the training content, and the intensity of training for prehabilitation.
The primary purpose of EP training was to achieve improvements in exercise tolerance and muscle strength through cardiopulmonary functional training by aerobic and resistance exercise. Inoue et al. reported that preoperative physical training, such as muscle strength exercise and biking on ergometer, in addition to respiratory rehabilitation reduced the occurrence of postoperative pulmonary complications although the preoperative rehabilitation did not improve the respiratory function [11]. Furthermore, previous studies have reported that high maximum oxygen uptake (VO2 max), an index of endurance and exercise tolerance, was a predictor of low postoperative complications after surgery in patients with esophageal and lung cancer [22, 23]. These results might suggest that improvement in VO2 max on prehabilitation training could reduce the postoperative respiratory complications.
Many patients with esophageal cancer are elderly and undernourished. Further, some patients had comorbidities such as heart disease and musculoskeletal disease, for whom the safety of intensive rehabilitation training was a concern. Although in the EP group 6 patients (26.1%) were aged > 70 years and 16 (69.6%) had comorbidities, including as heart, pulmonary, cerebrovascular, and/or orthopedic diseases, there were no serious adverse events in any patient. In the postoperative hematologic examination, there was no deterioration in the findings between the time of surgery and at 6-month follow-ups in the EP group compared to those in the control group (Table 4).
In this study, we observed that appropriate exercise training can be performed safely under the supervision of professional physical therapist in our hospital. In contrast, it might be difficult to ensure the safety of the patients’ self-training in the outpatient setting. EP program would facilitate at-home training without hospitalization with some ingenuity. However, in terms of guaranteeing the quality of training and accurate evaluation of the outcomes, training in the hospital under the supervision of a physical therapist was found to be more favorable.
This study primarily aimed to investigate the safety of the EP. In this process, improvement of 6MWD and reduction in respiratory complications, especially atelectasis in the EP group, were also confirmed. In this study, we evaluated exercise tolerance using the 6MWD test. This test has been used to measure exercise tolerance and to determine the correlation with postoperative morbidities [24, 25]. In addition, the 6MWD value correlates with VO2 max [24, 25]. In the EP group, the 6MWD value increased significantly after EP training during the preoperative period (Fig. 2). Considering that there was no significant difference in the rate of change between preoperative and postoperative 6MWD values between the two groups, and that the postoperative 6MWD value decreased to the level observed at admission in the EP group, it is noteworthy that patients were able to achieve the maximum possible improvement before surgery. Preoperative reservation of tolerance via EP training may enable patients to better withstand surgical stress [9]. Although several studies have reported that prehabilitation training could improve exercise tolerance of patients, it is uncertain whether it translates into a reduction in postoperative complications [9, 26]. In a previous study, patients received home-based training program in the outpatient setting [9]. Interestingly, in the present study, the rate of respiratory complications, especially atelectasis, was significantly lower in the EP group than in the control group (Table 3). Licker et al. reported that preoperative enhanced cardiorespiratory fitness training under experienced physical therapists for patients with lung cancer significantly improved VO2 max and reduced postoperative atelectasis in the study group (12.2%) as compared with those in the control group (36.4%, p < 0.001) [27]. These results might suggest that quality-assured prehabilitation-induced improvement in cardiorespiratory fitness enables patients to better withstand respiratory muscular weakness and facilitates lung re-expansion postoperatively [27]. Improvement in VO2 max due to EP training improved the efficacy of oxygenation in ventilation, resulting in reduced perioperative respiratory muscle fatigue. Reduction in respiratory muscle fatigue is advantageous for postoperative lung expansion and self-expectoration and might contribute to the prevention of atelectasis. Further examination is required to determine the effectiveness of EP.
Studies have reported an association between preoperative sarcopenia and postoperative complications and prognosis [28, 29]. In recent years, several patients had received preoperative chemotherapy or chemoradiotherapy; therefore, frailty could have been further accelerated before surgery [30]. If sarcopenia of the patients can be improved before surgery, it may help reduce the occurrence of postoperative complications. Although the 6MWD value increased significantly during the preoperative period by EP training, muscle strength was not improved in terms of grip strength and knee extension in our study. This may have been caused by the less-intensive exercise or that more time may be required to increase muscle strength preoperatively. Fearon et al. considered that 3 weeks might be sufficient to obtain a moderate gain in aerobic and muscle strength reserve, although the preoperative period was limited [31]. Therefore, it is necessary to design an effective program in the outpatient department in addition to in-patient EP training. Nutritional support is also important to improve sarcopenia in addition to resistance training [9, 32]. Because patients with esophageal cancer often have dysphagia due to weight loss and malnutrition, nutritional assessment and support are essential [33]. The knowledge of sufficient nutritional support including appropriate calorie and protein administration that matched the strength of exercise is uncertain. This examination should be conducted in the future.
The present study has demonstrated that EP is safe and effective in reducing the incidence of postoperative respiratory complications. However, our study has certain limitations. First, this was a retrospective cohort study with a small population. Second, selection bias was undeniable because the patients had been judged able to withstand surgery. Third, there may have been other confounders that could affect the outcomes. Therefore, a prospective randomized control study is required to obtain more robust findings.
Conclusions
EP was performed safely for patients before esophagectomy. EP improved the exercise tolerance of patients before esophagectomy and might be useful in preventing the occurrence of respiratory complications. Further research is needed to verify the usefulness of EP in the future.
References
Low DE, Alderson D, Cecconello I, et al. International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg. 2015;262:286–94.
Takeuchi H, Miyata H, Gotoh M, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. 2014;260:259–66.
Markar S, Gronnier C, Duhamel A, et al. Pattern of postoperative mortality after esophageal cancer resection according to center volume: Results from a large european multicenter study. Ann Surg Oncol. 2015;22:2615–23.
Baba Y, Yoshida N, Shigaki H, et al. Prognostic Impact of Postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg. 2016;264:305–11.
Akiyama Y, Iwaya T, Endo F, et al. Effectiveness of intervention with a perioperative multidisciplinary support team for radical esophagectomy. Support Care Cancer. 2017;25:3733–9.
Carli F, Gillis C, Scheede-Bergdahl C. Promoting a culture of prehabilitation for the surgical cancer patient. Acta Oncol. 2017;56:128–33.
Boujibar F, Bonnevie T, Debeaumont D, et al. Impact of prehabilitation on morbidity and mortality after pulmonary lobectomy by minimally invasive surgery: a cohort study. J Thorac Dis. 2018;10:2240–8.
Soares SM, Nucci LB, da Silva MM, et al. Pulmonary function and physical performance outcomes with preoperative physical therapy in upper abdominal surgery: a randomized controlled trial. Clin Rehabil. 2013;27:616–27.
Minnella EM, Awasthi R, Loiselle SE, et al. Effect of exercise and nutrition prehabilitation on functional capacity in esophagogastric cancer surgery: a randomized clinical trial. JAMA Surg. 2018;153:1081–9.
Inoue T, Ito S, Ando M, et al. Changes in exercise capacity, muscle strength, and health-related quality of life in esophageal cancer patients undergoing esophagectomy. BMC Sports Sci Med Rehabil. 2016;8:34.
Inoue J, Ono R, Makiura D, et al. Prevention of postoperative pulmonary complications through intensive preoperative respiratory rehabilitation in patients with esophageal cancer. Dis Esophagus. 2013;26:68–74.
Japan Esophageal Society. Japanese classification of esophageal cancer. 11th ed. Tokyo: Kanehara; 2015.
Brierley JD, Gospodarowicz MK, Wittekind C. TNM classification of malignant tumors: International union against cancer. 8th ed. Oxford: Wiley; 2017.
Akiyama Y, Iwaya T, Endo F, et al. Investigation of operative outcomes of thoracoscopic esophagectomy after triplet chemotherapy with docetaxel, cisplatin, and 5-fluorouracil for advanced esophageal squamous cell carcinoma. Surg Endosc. 2018;32:391–9.
Akiyama Y, Iwaya T, Endo F, et al. Thoracoscopic esophagectomy with total meso-esophageal excision reduces regional lymph node recurrence. Langenbecks Arch Surg. 2018;403:967–75.
Akiyama Y, Iwaya T, Endo F, et al. Stability of cervical esophagogastrostomy via hand-sewn anastomosis after esophagectomy for esophageal cancer. Dis Esophagus. 2017;30:1–7.
Akiyama Y, Iwaya T, Endo F, et al. Evaluation of the need for routine feeding jejunostomy for enteral nutrition after esophagectomy. J Thorac Dis. 2018;10:6854–62.
American Thoracic Society. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Duggan M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology. 2005;102:838–54.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Pehlivan E, Turna A, Gurses A, et al. The effects of preoperative short-term intense physical therapy in lung cancer patients: a randomized controlled trial. Ann Thorac Cardiovasc Surg. 2011;17:461–8.
Nagamatsu Y, Shima I, Yamana H, et al. Preoperative evaluation of cardiopulmonary reserve with the use of expired gas analysis during exercise testing in patients with squamous cell carcinoma of the thoracic esophagus. J Thorac Cardiovasc Surg. 2001;121:1064–8.
Nagamatsu Y, Shima I, Hayashi A, et al. Preoperative spirometry versus expired gas analysis during exercise testing as predictors of cardiopulmonary complications after lung resection. Surg Today. 2004;34:107–10.
Gillis C, Li C, Lee L, Awasthi R, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology. 2014;121:937–47.
Lee L, Schwartzman K, Carli F, et al. The association of the distance walked in 6 min with pre-operative peak oxygen consumption and complications 1 month after colorectal resection. Anaesthesia. 2013;68:811–6.
Nagarajan K, Bennett A, Agostini P, et al. Is preoperative physiotherapy/pulmonary rehabilitation beneficial in lung resection patients? Interact Cardiovasc Thorac Surg. 2011;13:300–2.
Licker M, Karenovics W, Diaper J, et al. Short-term preoperative high-intensity interval training in patients awaiting lung cancer surgery: a randomized controlled trial. J Thorac Oncol. 2017;12:323–33.
Nishigori T, Okabe H, Tanaka E, et al. Sarcopenia as a predictor of pulmonary complications after esophagectomy for thoracic esophageal cancer. J Surg Oncol. 2016;113:678–84.
Nakashima Y, Saeki H, Nakanishi R, et al. Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Ann Surg. 2018;267:1100–4.
Doganay E, Moorthy K. Prehabilitation for esophagectomy. J Thorac Dis. 2019;11:S632–S638638.
Fearon KC, Jenkins JT, Carli F, et al. Patient optimization for gastrointestinal cancer surgery. Br J Surg. 2013;100:15–27.
Yamamoto K, Nagatsuma Y, Fukuda Y, et al. Effectiveness of a preoperative exercise and nutritional support program for elderly sarcopenic patients with gastric cancer. Gastric Cancer. 2017;20:913–8.
Low DE, Allum W, De Manzoni G, et al. Guidelines for perioperative care in esophagectomy: enhanced recovery after surgery (ERAS®) society recommendations. World J Surg. 2019;43:299–330.
Acknowledgements
We thank all the participants of this study, physical therapists, and the nursing and laboratory staff of Iwate Medical University Hospital.
Author information
Authors and Affiliations
Contributions
Conception and design: YA, TI, and YN. Administrative support: YH, TK, TT, KO, HiN, KK, and AS. Provision of study materials or patients: FE and SB. Collection and assembly of data: YF, RF, NS, and HaN. Data analysis and interpretation: YA, YF, and TI. Manuscript writing: all authors. Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Ethical statement
All study procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Declaration of Helsinki of 1964 and later versions. Informed consent or its substitute was obtained from all patients for being included in the study.
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akiyama, Y., Sasaki, A., Fujii, Y. et al. Efficacy of enhanced prehabilitation for patients with esophageal cancer undergoing esophagectomy. Esophagus 18, 56–64 (2021). https://doi.org/10.1007/s10388-020-00757-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00757-2