Abstract
Background
Although esophagectomy is the standard treatment for resectable esophageal cancer, chemoradiotherapy or radiotherapy alone is also selected for some cases. However, there have been very few detailed studies conducted on a large scale on the efficacy of these treatments in Japan.
Methods
Of the patients enrolled in the Comprehensive Registry of Esophageal Cancer in Japan by the Japan Esophageal Society for the 2015–2017 surveys (patients treated between 2009 and 2011), the data of 388 patients treated by definitive radiotherapy alone (RTx) and 1964 patients treated by definitive chemoradiotherapy (CRTx) were analyzed.
Results
The median age of the patients was 78 years in the RTx group and 69 years in the CRTx group; thus, the proportion of elderly patients was significantly higher in the RTx group than in the CRTx group (p < 0.0001). With regard to the rates of treatment by the two modalities according to the depth of invasion, extent of lymph node metastasis, and disease stage, the treatment rate by CRTx increased more significantly than that by RTx as the disease progressed (p < 0.0001). With regard to the distribution of the total irradiation dose, 11.4% and 2.3% of patients in the RTx and CRTx groups, respectively, received a dose of 67 Gy or more; thus, the RTx group received significantly higher total irradiation doses (p < 0.0001). In the RTx group, the 5-year overall survival rate was 23.2%, and the rates in patients with cStage 0–I, II, III, and IV disease were 41.8%,18.5%, 9.3%, and 13.9%, respectively. In the patients of the RTx group showing complete response (CR), the 5-year overall survival rate was 46.6% and the rates in patients with cStage 0–I, II, III, and IV disease were 54.8%, 39.6%, 32.4%, and 38.9%, respectively. In the CRTx group, the 5-year overall survival rate was 30.6% and the rates in patients with cStage 0–I, II, III, and IV disease were 57.8%, 47.8%, 23.4%, and 13.0%, respectively. In the patients of the CRTx group showing CR, the 5-year overall survival rate was 59.2% and the rates in patients with cStage 0–I, II, III, and IV disease were 67.9%, 59.5%, 56.5%, and 39.6%, respectively.
Conclusion
This study revealed the current status of treatment of esophageal cancer in Japan, and we think that we have been able to establish the grounds for explaining to patients with esophageal cancer and their families the treatment decisions made for them in daily clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Japan, esophagectomy is the standard treatment for resectable esophageal cancer [1, 2]. However, since this procedure is associated with excessive surgical stress and non-surgical treatment also offers a relatively high probability of complete cure [3,4,5], chemoradiotherapy (CRTx) is also often selected for patients with esophageal cancer. Treatment with radiation alone (RTx) is also sometimes selected in clinical practice, considering the general condition of the patient. However, most of the reports on the efficacy of RTx have been based on the experience gained at a single or a few institutions, and there have been very few detailed studies conducted on a large scale on curative RTx in many cases [6].
According to a report by Nishimura et al. in 2016 [7], 11 Japanese institutions belonging to the Japanese Radiation Oncology Study Group (JROSG) studied 990 cases with good performance status treated by RTx with curative intent between 2004 and 2008. They reported a 5-year overall survival rates in patients with stage I (n = 259: 48 by RTx, 181 by CRTx and 30 by RTx/CRTx with intraluminal brachytherapy), resectable stage II–III (n = 333: all by CRTx), and unresectable stage III–IVA (n = 398: all by CRTx) disease of 73%, 40%, and 18%, respectively; however, there was a wide disparity in the results among the JROSG institutions at stage I and resectable stage II–III. Furthermore, in “a phase II study of chemoradiotherapy in patients with stage II, III esophageal squamous cell carcinoma (JCOG9906)” conducted by the Japan Clinical Oncology Group (JCOG), the 3- and 5-year survival rates in the 76 patients enrolled between 2000 and 2002 were 44.7% and 36.8%, respectively [4]. However, these studies were based on data obtained from the so-called major institutions and included patients treated in the days when treatment plans were based on plain radiography, and the efficacy of radiotherapy in the current scenario in Japan, where mainly three-dimensional treatment planning is used, remains unclear.
The Comprehensive Registry of Esophageal Cancer in Japan by the Japan Esophageal Society has collected data not only on surgical cases, but also on cases that had received other treatments, such as radiotherapy and chemotherapy, and transmitted information on the overall survival of the registered patients by the stage as Registry [8,9,10] every year. Approximately 900 curative chemoradiotherapy or radiotherapy-alone cases with the treatment outcomes determined at least 5 years after the treatment from approximately 300 institutions providing treatment for esophageal cancer throughout Japan have been registered so far every year. However, although data on registration items other than the overall survival, including the age, sex, and radiation dose have also been registered, no detailed studies have been conducted on the relationship of these variables with the therapeutic efficacy or overall survival of the patients. The purpose of this study was to clarify the current status of curative chemoradiotherapy and radiotherapy alone for esophageal cancer in Japan using data from the Registry treated between 2009 and 2011. This study involved patients treated more recently as compared to those in references 4, 6, and 7 and is expected to provide useful information for determining the treatment strategies for patients by clarifying the reality of recent curative chemoradiotherapy and radiotherapy alone in Japan.
Patients and methods
Patient characteristics
Of the patients enrolled in the Comprehensive Registry of Esophageal Cancer in Japan by the Japan Esophageal Society for the 2015–2017 surveys (patients treated between 2009 and 2011) [8,9,10], the data of those who had received RTx alone or CRTx with sufficiently effective cumulative dose delivered to whole macroscopic lesions were analyzed. Only cases that had received external irradiation were included, and patients with cervical/abdominal esophageal cancer and pediatric cases were excluded. A total of 388 patients who had received RTx alone and 1964 patients who had received CRTx (2352 cases in total) met the above criteria for the 3-year period mentioned above. For these cases, the date of start of radiotherapy and the final date of survival confirmation in a national survey or the prognosis at least 5 years after the treatment were available from the registry. The characteristics of the study subjects are shown in Table 1.
Statistical analysis
The subjects were selected from the database of the Comprehensive Registry of Esophageal Cancer in Japan by the Japan Esophageal Society, and the following items were examined to assess their correlations with the therapeutic efficacy (response) and the prognosis, separately for the RTx and CRTx groups: sex, age, histological type, tumor site, depth of invasion, presence/absence of lymph node metastasis, clinical stage (the Union for International Cancer Control-Tumor-Node-Metastasis [UICC-TNM] classification, 7th edition), irradiation dose, and the complete response (CR) rate. For the all items, cases with missing data were excluded from the analysis. The Chi-square test was used to compare each factor between the RTx and CRTx groups and to analyze the relationship between each factor and the CR rate.
Survival curves were drawn using the Kaplan–Meier method, and the log-rank test was used to compare the results among groups excluding that of all cases. For the survival rate, the overall survival was calculated. Therefore, additional treatment in the non-CR cases and endoscopic and surgical salvage treatments for recurrence in the CR cases would be expected to affect the results; however, information on these treatments is not contained in the Comprehensive Registry. SAS 9.4 (SAS Institute Inc., Cary, NC, USA) was used for the statistical analysis, with the significance level set at 5%.
Results
Comparison of each variable between the RTx and CRTx groups (Table 1)
The mean age (minimum–maximum) was 78 (38–96) years in the RTx group and 69 (37–91) years in the CRTx group, and the proportion of elderly patients was significantly higher in the RTx group than in the CRTx group (p < 0.0001).
With regard to the treatment rates by the two modalities according to the tumor histological type, squamous cell carcinoma and adenocarcinoma accounted for approximately 97% and slightly more than 1%, respectively, of both the RTx and CRTx groups, with no significant differences between the groups. There was also no difference in the treatment rate by RTx and CRTx depending on the main lesion site.
With regard to the rates of treatment by the two modalities according to the depth of invasion, extent of lymph node metastasis and disease stage, the treatment rate by CRTx increased more significantly as compared to that by RTx as the disease progressed (p < 0.0001). In other words, these results suggest that RTx alone is often selected for patients with relatively early disease.
With regard to the distribution of the irradiation dose, 11.4% and 2.3% of patients in the RTx and CRTx groups, respectively, received a dose of 67 Gy or more; thus, the irradiation doses were significantly higher in the RTx group (p < 0.0001).
Relationship between each variable and the CR rate (Table 2)
Comparison by sex showed that, in the CRTx group, the CR was significantly higher in the female patients. Comparison by the histological type revealed no difference in the CR rate between patients with squamous cell carcinoma and adenocarcinoma. The CR rate decreased with disease progression according to the cT, cN, and cStage classification. In patients with cT1b or less advanced disease, the CR rate was as high as 65% or more in the RTx group and approximately 75% in the CRTx group.
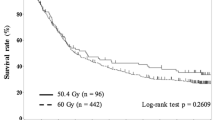
Comparison by the irradiation dose revealed that, in the CRTx group, the CR rate was the highest for a dose of 56–66 Gy, with a significant difference in the CR rate between patients receiving higher and lower doses.
Overall survival by clinical stage in the RTx group: all cases and CR cases (Fig. 1)
In the RTx group, the 5-year overall survival rate was 23.2% and the rates in patients with cStage 0–I, II, III, and IV disease were 41.8%, 18.5%, 9.3%, and 13.9%, respectively (p < 0.001). Among the patients of the RTx group who showed CR, the 5-year overall survival rate was 46.6% and the rates in the patients with cStage 0–I, II, III, and IV disease were 54.8%, 39.6%, 32.4%, and 38.9%, respectively (p < 0.05).
Overall survival by the clinical stage in the CRTx group: all cases and CR cases (Fig. 2)
In the CRTx group, 5-year overall survival rate was 30.6%, and the rates in patients with cStage 0–I, II, III, and IV disease were 57.8%, 47.8%, 23.4%, and 13.0%, respectively (p < 0.001). Among the patients of the CRTx group who showed CR, the 5-year overall survival rate was 59.2% and the rates in the patients with cStage 0–I, II, III, and IV disease were 67.9%, 59.5%, 56.5%, and 39.6%, respectively (p < 0.001).
Discussion
This study clarified the current status and therapeutic efficacy of CRTx and RTx alone for patients with thoracic esophageal cancer in Japan. Until now, there have been no nationwide studies on their current status, and the present study is considered to be highly relevant.
In this study, with regard to the proportions of the histological types treated by RTx and CRTx, adenocarcinoma accounted for approximately 1% of the cases in both the treatment groups (Table 1). Among the cases treated by esophagectomy in 2011, squamous cell carcinoma accounted for approximately 84.4% and adenocarcinoma for approximately 5.1% (approximately 7.0%, if cases of Barrett’s esophageal cancer were included) [10]. Comparison of the proportion of cases of “squamous cell carcinoma” and “adenocarcinoma” (excluding other histological types) treated by surgery (during the 3-year period from 2009 to 2011) and radiotherapy (RTx or CRTx) revealed that the proportion of “adenocarcinoma” cases was significantly lower among the cases treated by radiotherapy (data not shown; p < 0.0001), suggesting that radiotherapy may be avoided in patients with adenocarcinoma. In cases of adenocarcinoma treated by radiotherapy, common in patients with cancer of the lower esophagus, it may be difficult to use radical irradiation at 60 Gy in some cases, because a certain volume of the stomach will also be irradiated. Although the number of cases was small, there was no difference in the CR rate between these two histological types (Table 2), which may be a significant result.
In the RTx group, patients with cStage 0–I disease showed a 5-year overall survival of 41.8%; in particular, those in whom CR was achieved showed a 5-year overall survival rate of 54.8% (Fig. 1). At this stage, CR can be expected in 55.8% of patients (Table 2), indicating that RTx could be a curative treatment for patients who are unsuitable candidates for surgery and who are unsuitable to receive concurrent chemotherapy because of the general condition.
With regard to patients with cStage II/III disease (it is not easy to distinguish between stage II and stage III disease in clinical practice, and they are also often handled together in clinical studies), which accounted for many of the cases, patients with these stages in whom CR was achieved with RTx alone showed 5-year overall survival rates of 39.6% and 32.4%, respectively, suggesting that if patients with these stages of esophageal cancer whose general condition does not permit them to receive concurrent chemotherapy (the proportion of such patients is particularly high in the elderly) could show CR to RTx alone, there is a high possibility of complete cure being achieved. However, the treatment results were not satisfactory, and the CR rates were only 40.4% and 19.6%, respectively. It would be desirable to develop treatments that would increase the CR rate without necessitating the use of concurrent chemotherapy. In this process, it is essential to select patients through examining the radiosensitivity of the disease before treatment selected by genetic analysis (individualized treatment, precision medicine).
In the CRTx group, patients with cStage 0–I disease showed a 5-year overall survival rate of 57.8%, and the rate was 67.9% in those who had achieved CR (CR rate 74.6%) (Fig. 2; Table 2). These patients showed a 4-year overall survival of 64.9% and 73.5%, respectively (data not shown). These results were clearly poorer than the 4-year overall survival rate of 80.5% achieved in patients with cStage I esophageal squamous cell carcinoma who had received CRTx in a study conducted in Japan (JCOG9708) [3]. In addition, in the present study, patients with cStage II/III disease in the CRTx group showed a 5-year overall survival of 27.6% and a CR rate of 33.8% (n = 961, data not shown), which were also lower than the 5-year overall survival rate of 36.8% and CR rate of 62.2% achieved in patients with disease of the same stage who had received CRTx in a study conducted in Japan (JCOG9906) [4].
As described above, the results of the present study were clearly inferior to those of clinical studies, but they are considered to represent the current status of the outcomes including patients unsuitable for surgery in clinical practice. Jingu et al. reported that cStage I esophageal cancer patients in a general condition that is allowing resection showed a significantly better outcome of CRTx as compared to those who were unsuitable to undergo surgery [11].
Among the limitations of this study is that the reason for selecting RTx or CRTx in the patients, and the patients’ general condition, remained unknown. There was no information on whether the general condition of the patients was sufficiently good to allow surgery or concurrent chemotherapy, and a simple comparison of the treatment results would be meaningless. In addition, since the accuracy of the data depends on the institution, their reliability may also come into question. Furthermore, there were no records of the adverse events of treatment and no information on the subsequent treatment given to the patients who did not show CR or the treatment given for recurrence in CR patients. These are some of the limitations of current national surveys.
Even in patients who showed CR, the prognosis after RTx alone was inferior to that after CRTx. This may be because the RTx group included patients whose general condition was not good enough to allow concurrent chemotherapy, resulting in a poor overall survival. It was reported that among patients with cT1 disease for whom radiotherapy (± chemotherapy) was selected, the majority (24 of 44 deaths) died of causes other than esophageal cancer [12]. This is considered to be the case for all patients fit for surgery for whom radiotherapy was selected instead, and may greatly affect the treatment results. It will be necessary to examine not the overall survival, but the disease-specific mortality. In addition, chemotherapy may also control recurrences outside the radiation field. To investigate this, the patterns of recurrence leading to death need to be studied. In the first place, it is difficult to evaluate the therapeutic efficacy for primary lesions of esophageal cancer by imaging, which may make data interpretation difficult.
In the future, it will be important to study the optimal method for irradiation of esophageal cancer in RTx. Reportedly, the shorter the duration of treatment is, the better the treatment results in RTx alone are [13]; therefore, it is necessary to improve the method of accelerated fractionation [14]. In addition, research on the application of particle therapy to esophageal cancer must be promoted [15,16,17].
Conclusion
This study clarified the current status of treatment of esophageal cancer in Japan, and we believe that we have established the grounds for explaining to patients with esophageal cancer and their families the treatment decisions made in daily clinical practice.
References
Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: part 1. Esophagus. 2019;16:1–24.
Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: part 2. Esophagus. 2019;16:25–43.
Kato H, Sato A, Fukuda H, et al. A phase II trial of chemoradiotherapy for stage I esophageal squamous cell carcinoma: Japan Clinical Oncology Group Study (JCOG9708). Jpn J Clin Oncol. 2009;39:638–43.
Kato K, Muro K, Minashi K, et al. Phase II study of chemoradiotherapy with 5-fluorouracil and cisplatin for Stage II–III esophageal squamous cell carcinoma: JCOG trial (JCOG 9906). Int J Radiat Oncol Biol Phys. 2011;81:684–90.
Sasaki Y, Kato K. Chemoradiotherapy for esophageal squamous cell cancer. Jpn J Clin Oncol. 2016;46:805–10.
Kawashima M, Kagami Y, Toita T, et al. Prospective trial of radiotherapy for patients 80 years of age or older with squamous cell carcinoma of the thoracic esophagus. Int J Radiat Oncol Biol Phys. 2006;64:1112–21.
Nishimura Y, Jingu K, Itasaka S, et al. Clinical outcomes of radiotherapy for esophageal cancer between 2004 and 2008: the second survey of the Japanese Radiation Oncology Study Group (JROSG). Int J Clin Oncol. 2016;21:88–94.
Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive registry of esophageal cancer in Japan, 2009. Esophagus. 2016;13:110–37.
Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive registry of esophageal cancer in Japan, 2010. Esophagus. 2017;14:189–214.
Tachimori Y, Ozawa S, Numasaki H, et al. Comprehensive registry of esophageal cancer in Japan, 2011. Esophagus. 2018;15:127–52.
Jingu K, Matsushita H, Takeda K, et al. Results of chemoradiotherapy for stage I esophageal cancer in medically inoperable patients compared with results in operable patients. Dis Esophagus. 2013;26:522–7.
Nemoto K, Matsumoto Y, Yamakawa M, et al. Treatment of superficial esophageal cancer by external radiation therapy alone: results of a multi-institutional experience. Int J Radiat Oncol Biol Phys. 2000;46:921–5.
Nishimura Y, Ono K, Tsutsui K, et al. Esophageal cancer treated with radiotherapy: impact of total treatment time and fractionation. Int J Radiat Oncol Biol Phys. 1994;30:1099–105.
Zhao KL, Shi XH, Jiang GL, Wang Y. Late-course accelerated hyperfractionated radiotherapy for localized esophageal carcinoma. Int J Radiat Oncol Biol Phys. 2004;60:123–9.
Verma V, Lin SH, Simone CB 2nd, Mehta MP. Clinical outcomes and toxicities of proton radiotherapy for gastrointestinal neoplasms: a systematic review. J Gastrointest Oncol. 2016;7:644–64.
Okada T, Kamada T, Tsuji H, et al. Carbon ion radiotherapy: clinical experiences at National Institute of Radiological Science (NIRS). J Radiat Res. 2010;51:355–64.
Warren S, Hurt CN, Crosby T, et al. Potential of proton therapy to reduce acute hematologic toxicity in concurrent chemoradiation therapy for esophageal cancer. Int J Radiat Oncol Biol Phys. 2017;99:729–37.
Acknowledgements
The authors thank all the institutions which cooperated to the Comprehensive Registry of Esophageal Cancer in Japan by the Japan Esophageal Society for the 2015–2017 surveys for their contributions.
Funding
None.
Author information
Authors and Affiliations
Contributions
Planning of the study and writing: Y.To, T.U., K.J., K.N. Data analysis: Y.To, H.N. Discussion and advices: Y.Ta, H.M.
Corresponding author
Ethics declarations
Ethical statement
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later versions.
Conflict of interest
All authors declare that they have no potential conflict of interest in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toh, Y., Numasaki, H., Tachimori, Y. et al. Current status of radiotherapy for patients with thoracic esophageal cancer in Japan, based on the Comprehensive Registry of Esophageal Cancer in Japan from 2009 to 2011 by the Japan Esophageal Society. Esophagus 17, 25–32 (2020). https://doi.org/10.1007/s10388-019-00690-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-019-00690-z