Abstract
Submucosal abscess of the esophagus is extremely rare, and treatment has yet to be well established. A 58-year-old man with no relevant past medical history visited an otolaryngological clinic with a chief complaint of throat irritation. Computed tomography revealed submucosal abscess extending the full length of the esophagus after abnormally high white blood cell count and C-reactive protein levels were noted. A fish bone was removed surgically via the right side of the neck, and the submucosal abscess was drained by endoscopic mucosal incision. Oral intake was started on postoperative day 10 and the patient was discharged without any complications. Endoscopic submucosal incision is a useful and less-invasive therapy for treating esophageal submucosal abscess.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal abscess localized in the submucosal layer is extremely rare and has previously been reported in only two cases, both due to tuberculosis [1, 2]. Esophageal submucosal abscess (ESA) caused by a foreign body does not appear to have been reported in the English literature to date. In contrast, fish bone is a common cause of foreign body injuries in the esophagus and has been reported as a cause of fatal injury, esophago-aortic fistula, and mediastinitis [3–7].
Due to the rarity of ESA, consensus regarding the treatment of this condition has yet to be reached. Two cases of ESA due to tuberculosis were treated surgically via right thoracotomy [1, 2], but the use of minimally invasive endoscopic therapy has yet to be reported.
We report here successful endoscopic treatment for this extremely rare condition, along with a review of the literature.
Case report
A 58-year-old man visited an otolaryngological clinic with a chief complaint of throat irritation. No clear findings were apparent on laryngoscopic examination at the initial visit. The patient visited again 1 week later due to continued symptoms, and neck swelling and fever were identified. White blood cell count was 19,020/mm3 and C-reactive protein level was 37.39 mg/dl, so the patient was referred to our hospital.
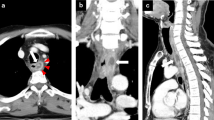
Computed tomography (CT) was immediately performed, revealing a half of fish bone within the esophageal wall and the rest outside the wall at the border between the neck and chest. An accumulation of low-density fluid collection, suspected to represent abscess, was detected extending almost the entire length of the esophageal submucosal layer (Fig. 1a–d). Endoscopic examination revealed mucosal undulation due to submucosal fluid collection from the cervico-thoracic border to the lower thoracic esophagus (Fig. 2).
Computed tomography (CT) before surgery. a, c A fish bone is apparent in the para-esophageal region in the neck. b, d A homogeneous low-density area was observed extending half the circumference of the esophageal wall, and extending the entire longitudinal length of the esophagus. These findings corresponded to the submucosal abscess in the esophagus
Endoscopic findings obtained before treatment. a Spotty discoloration of the esophageal mucosa at 23 cm from the frontal incisors, indicating localized mucosal necrosis. b Undulating mucosa extending from 22 to 38 cm from the frontal incisors, indicating the submucosal abscess extending longitudinally through the esophageal wall
Under general anesthesia, because it was located outside the esophagus and could be palpated, the fish bone was easily removed surgically via a small neck incision; however, no abscess formation was identified within the surgical field. An approximately 16 cm longitudinal mucosal incision was endoscopically made starting distally at 22 cm from the frontal incisor teeth to allow the drainage of ESA using an electrosurgical knife. This endoscopic mucosal incision released approximately 30 ml of pus and the pus culture detected Prevotella sp. (Fig. 3). Doripenem hydrate was administered intravenously for 1 week after treatment.
Serum C-reactive protein level improved immediately after treatment (Fig. 4). ESA was no longer apparent on CT performed 5 days postoperatively. Oral intake was resumed 10 days postoperatively, after ulcer healing and epithelial regeneration over the shallow longitudinal esophageal ulcer had been observed endoscopically (Fig. 5).
The patient was discharged from hospital after 18 days with an uneventful postoperative course.
Discussion
Fish bone is one of the most common foreign bodies encountered in the esophagus, and can lead to fatal conditions such as esophago-aortic fistula and mediastinitis [3–7]. Thyroid abscess due to fish bone migration has also been reported, although this seems very rare [8]. Early diagnosis and removal, made possible by the popularization of endoscopic techniques, have led to good clinical outcomes; however, delays in diagnosis might increase the risk of mortality. Das reviewed four reports and stated that CT offered almost 100 % sensitivity and 100 % positive predictive value for the detection of fish bone, although plain radiography was equally useful [9]. However, CT was very effective in the present case, not only for detecting fish bone, but also for evaluating the area of abscess, and was indispensable in determining the limits of ESA.
ESA resulting from fish bone injury is extremely rare and no cases appear to have been reported in the English literature. In addition, no reports have described ESA extending the full length of the esophagus. The mechanism of extension also remains unclear; however, we think it is likely similar to that in descending necrotic mediastinitis, in which pus collection is forced downward by gravity along the submucosal layer. Therefore, a standard approach for treatment has yet to be determined. Two cases of ESA caused by tuberculosis were drained by posterolateral thoracotomy, although the procedure in those cases included the aim of pathological diagnosis by tissue sampling as well as surgical therapy [1, 2]. In the present case, diagnostic biopsy was unnecessary; therefore, minimally invasive therapy involving endoscopic drainage by mucosal incision and surgical removal of the fish bone via a neck incision was able to be performed. Endoscopic intra-esophageal drainage of the abscess is able to remove the pus and carries no risk of spreading infection to the thoracic cavity or causing osteomyelitis compared to thoracotomy.
A great care is needed during the endoscopic procedure so as not to allow the pus to flow outside the esophageal wall in order to prevent the spread of unwanted infection. Therefore, precise mucosal incision without injuring the muscle layer was performed in this case. Furthermore, a sufficient length of mucosal incision was required for the complete pus drainage, because the ESA was spread distally along the loose submucosal layer under the influence of gravity. A previous report of esophageal submucosal hematoma, not abscess, described formation of a shallow longitudinal ulcer and no leakage after falling off the esophageal mucosa [10]. Given that improvement of the extremely high C-reactive protein level by abscess drainage was the most critical goal, we therefore considered full-length mucosal incision as appropriate treatment.
In conclusion, we have reported an extremely rare case of ESA due to fish bone ingestion. Drainage by endoscopic mucosal incision offers a very efficient and minimally invasive therapy.
References
Eroğlu A, Kürkçüoğlu C, Karaoğlanoğlu N, Yilmaz O, Gürsan N. Esophageal tuberculosis abscess: an unusual cause of dysphagia. Dis Esophagus. 2002;15:93–5.
Lee KH, Kim HJ, Kim KH, Kim HG. Esophageal tuberculosis manifesting as submucosal abscess. AJR Am J Roentgenol. 2003;180:1482–3.
Kunishige H, Myojin K, Ishibashi Y, Ishii K, Kawasaki M, Oka J. Perforation of the esophagus by a fish bone leading to an infected pseudoaneurysm of the thoracic aorta. Gen Thorac Cardiovasc Surg. 2008;56:427–9.
Macchi V, Porzionato A, Bardini R, Parenti A, De Caro R. Rupture of ascending aorta secondary to esophageal perforation by fish bone. J Forensic Sci. 2008;53:1181–4.
Nozoe T, Kitamura M, Adachi Y, Funahashi S, Yoh R, Iso Y, Matsumata T, Sugimachi K. Successful conservative treatment for esophageal perforation by a fish bone associated with mediastinitis. Hepatogastroenterology. 1998;45:2190–2.
Nishimaki T, Ono K, Tada T, Hatakeyama K. Successful primary reinforced repair of esophageal perforation using a pedicled omental graft through a transhiatal approach. Dis Esophagus. 2001;14:155–8.
Katsetos MC, Tagbo AC, Lindberg MP, Rosson RS. Esophageal perforation and mediastinitis from fish bone ingestion. South Med J. 2003;96:516–20.
Chen CY, Peng JP. Esophageal fish bone migration induced thyroid abscess: case report and review of the literature. Am J Otolaryngol. 2011;32:253–5.
Das D, May G. Best evidence topic report. Is CT effective in cases of upper oesophageal fish bone ingestion? Emerg Med J. 2007;24:48–9.
Koike J, Matsushima M, Teraoka H, Igarashi M, Deguchi R, Suzuki T, Shirai T, Mine T. A case of submucosal hematoma of the esophagus and stomach, possibly caused by fish bone ingestion. Tokai J Exp Clin Med. 2010;35:46–56.
Ethical Statement
This case report was in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Conflict of interest
The authors have no conflicts of interest to disclose with respect to the present case and manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takeno, S., Moroga, T., Ono, K. et al. Endoscopic mucosal incision for successful treatment of submucosal abscess extending the full length of the esophagus due to fish bone: report of a case. Esophagus 12, 199–202 (2015). https://doi.org/10.1007/s10388-014-0413-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-014-0413-0