Abstract
Background and objective
Monitoring of central venous blood oxygen saturation (ScvO2) has recently become easier and safer to perform, but its clinical usefulness following esophagectomy has yet to be established. This study evaluated the use of continuous monitoring of ScvO2 in this setting, focusing on its relationship with hemoglobin (Hb) concentrations, and reconsideration about an appropriate indication of red blood cell transfusion from the aspect of tissue oxygen balance.
Methods
A total of 40 patients were assessed following transthoracic esophagectomy for carcinoma. ScvO2 was measured via a fiberoptic central venous oximetry catheter, postoperatively until discharge from the ICU. Hb was also measured preoperatively and every 8 h postoperatively.
Results
In correlation between ScvO2 and Hb values, ScvO2 could still be greater than 70% in patients with a Hb around 7 g/dl who did not have a bleeding event and maintained a stable circulation. Even when Hb dilution ratio (sampling Hb/preoperative Hb) decreased to around 60% of the preoperative value, ScvO2 could remain above 65%. Patients who had severe bleeding exhibited a marked decrease of the ScvO2 value before blood transfusion, but the trend was clearly seen to be a gradual increase of ScvO2 during transfusions.
Conclusions
Hb supply is essentially unnecessary if the balance of oxygen supply/demand in tissues is well maintained. ScvO2 may be a better indicator of a physiological need for blood than Hb in postesophagectomy patients. ScvO2 is not influenced by hemodilution and lowering of Hb to around 60% of the preoperative value. As well as being a useful start indicator for blood transfusions, ScvO2 could also become a stop indicator.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A balance of oxygen consumption, oxygen delivery, and oxygen extraction is important for normal functioning, but variations occur in several clinical situations or diseases. In 1988, Shoemaker et al. [1] reported that hemodynamic therapy to raise oxygen delivery to supranormal levels was associated with improved survival of surgical patients. In patients who undergo esophagectomy for esophageal cancer, maintenance of adequate tissue oxygenation is believed to be a beneficial strategy to prevent the development of fatal postoperative complications [2]. On the other hand, Gattinoni et al. [3] noted that therapy aimed at achieving supranormal cardiac index values or normal values for mixed venous oxygen saturation (SvO2) did not reduce morbidity or mortality among critically ill patients. Nevertheless, SvO2 remains an excellent index of systemic blood flow as it is directly proportional to cardiac output when arterial oxygen content and oxygen consumption remain constant. In addition, SvO2 has also been advocated as a useful parameter for reflecting the adequacy of tissue oxygenation, although the benefit of using pulmonary artery catheters (PACs) in the acute care of critically ill or high-risk surgical patients has been questioned [4, 5].
Rather than SvO2 measured by a PAC, continuous fiberoptic measurement of central venous blood saturation (ScvO2) has the potential to become a reliable and convenient tool that can rapidly warn of acute changes in oxygen supply and demand [6]. An earlier study noted that reversal of the normal relationship between SvO2 and ScvO2 in heart failure or clinical shock was affected by redistribution of blood flow away from the femoral, splanchnic, and renal circulations with preferential preservation of cerebral blood flow [7]. More recently, central venous catheterization of the superior vena cava has become part of the standard of care for any critically ill patient. Although ScvO2 monitoring has become easier and safer to perform, evaluation of the relationship between ScvO2 and clinical outcome is still being investigated. An analysis of trauma patients revealed a correlation between ScvO2 and blood loss, suggesting that ScvO2 is a useful parameter for determining whether blood transfusion is indicated [8], and a recent prospective, randomized study in patients with severe sepsis showed that maintenance of continuously measured ScvO2 above 70% resulted in a 15% absolute reduction in mortality compared with the same management without ScvO2 monitoring [9]. Moreover, a multicenter study of peri- and postoperative ScvO2 monitoring in high-risk surgical patients revealed that a low perioperative ScvO2 is related to an increased risk of postoperative complications [10], although the types of surgical procedures performed and the complications experienced were unclear.
In patients with esophageal squamous cell carcinoma who undergo radical esophagectomy together with extended lymphadenectomy, surgical stress leads to perioperative cardiopulmonary instability requiring careful postoperative management [11]. In the past decade, postoperative monitoring via a PAC has been a standard procedure following transthoracic esophagectomy, but introduction of the PreSep central venous oximetry catheter (Edwards, USA) has provided the means for routine monitoring of ScvO2 in the intensive care unit (ICU), although its clinical usefulness is not yet established. The purpose of the present study was to evaluate the use of continuous monitoring of ScvO2 in the management of patients after radical esophagectomy, focusing particularly on the relationship of ScvO2 with the hemoglobin (Hb) concentration and on assessment of the reasonable indication of red blood cell transfusion without depending on Hb value alone.
Methods
Patients studied
A total of 40 patients (all men; mean age, 66.8 years) underwent transthoracic esophagectomy by thoracoscopy-guided mini-thoracotomy with extended mediastinal lymphadenectomy for esophageal carcinoma at Hakodate Goryoukaku Hospital between May 2006 and May 2009. Reconstruction was performed by cervical anastomosis via the posterior mediastinal route with a gastric tube placed at the greater curvature of the stomach. All patients were histologically diagnosed with squamous cell carcinoma, at histopathological stage 0 in 6, I in 8, II in 12, III in 8, and IVa in 6 patients, according to the Japanese guidelines for clinical and pathological studies on carcinoma of the esophagus [12]. Three patients had received preoperative chemoradiotherapy to control the invasive cancer.
Before surgery, written informed consent was obtained from all patients according to the guidelines of the Declaration of Helsinki. All drugs (and dosages) and devices used in this study are approved by the Ministry of Health, Labor and Welfare of Japan for the optimal care of patients during and after major surgery.
Postoperative procedures and assessments
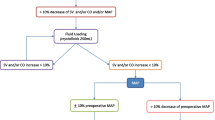
All patients were assessed using the Vigileo Monitor system (Edwards Lifesciences, Tokyo, Japan), to which they were connected via a PreSep oximetry catheter (Edwards Lifesciences). The PreSep catheter for ScvO2 measurement was inserted through the internal jugular vein with the optic sensor sited in the superior vena cava near an orifice of the right atrium [13]. Assessment by Vigileo Monitor was started during the operation and continued postoperatively until discharge from the ICU. During the surgical procedure, intravenous (IV) fluids containing crystalloids and hydroxyethylated starch were administered at a rate of 12–15 ml/kg/h. Immediately after surgery, all patients were transferred to the ICU where they received synchronized intermittent mandatory ventilatory support without positive end-expiratory pressure under continuous infusions with midazolam and morphine until at least the first postoperative morning. In the ICU, IV fluid administration in the early postoperative period was started at a rate of 3.5 ml/kg/h and continued until a diuretic state, defined as the time when urinary output increased to more than 1.5 ml/kg/h, was achieved. To prevent the adverse effects of neutrophil elastase induced by inflammatory cytokines [14], a selective neutrophil elastase inhibitor [sivelestat sodium hydrate (Elaspol); Ono Pharmaceutical, Osaka, Japan] was administered IV at a dosage of 0.2 mg/kg/h beginning within 1 h after completion of surgery and continuing during mechanical ventilation support. After a diuretic state was achieved, the IV fluid infusion rate was reduced to 1.5 ml/kg/h.
The postoperative management protocol for all patients did not include ‘renal-dose’ dopamine, protease inhibitors, or corticosteroids. During the first 12 h after surgery, volume loading for fluid resuscitation was considered necessary when a systolic arterial pressure <80 mmHg lasted more than 15 min without an increase in central venous pressure (CVP). During the patient’s ICU stay, hemoglobin was measured every 8 h by a blood gas analysis system ABL 700 (Radiometer Medical, Copenhagen, Denmark). ScvO2 and SVI were measured simultaneously by the Vigileo Monitor system.
The effect of hemodilution was analyzed in patients who did not receive blood transfusions. The Hb dilution ratio was calculated as follows:
Hb dilution ratio (%) = sampling Hb ÷ preoperative Hb × 100.
Statistical analysis
Tests of correlation between an occurrence of complication and ScvO2 value were analyzed statistically using StatView-J 5.0 software (Abacus Concepts, Berkeley, CA, USA), with values of P < 0.05 considered statistically significant. Quantitative parametric values were determined as mean ± standard deviation (SD).
Results
Patient data and postoperative course
The mean preoperative Hb concentration in the 40 patients was 12.8 ± 1.9 g/dl and the mean preoperative blood albumin concentration was 3.9 ± 0.4 g/dl. In all patients, blood tests revealed normal serum creatinine and blood urea nitrogen levels as markers of renal function. Preoperative echocardiography showed a mean left ventricular ejection fraction of 67 ± 6.9%, and all patients had a stable general condition without apparent dehydration. The mean operative time was 288 ± 55 min and mean blood loss was 355 ± 299 g. During the first 12 h after surgery, hypovolemic hypotension requiring fluid resuscitation occurred in 24 (60%) patients, and 2 also needed an inotropic agent to treat a low cardiac output. Lung complications, which constituted failure to remove the tracheal tube or the development of pneumonia or acute respiratory distress syndrome (ARDS), occurred in 3 patients (7.5%). Mean duration of ICU stay of all patients was 4.6 ± 2.8 days, and there was no mortality by 30 postoperative days.
A total of 308 measurements of ScvO2, Hb, and lactate values were made; the mean number of samplings per patient was 7.7. Postoperatively, all patients exhibited normal blood lactate concentrations on all days. From our series, we could not show any statistical correlation between a low perioperative ScvO2 value and occurrence of postoperative complications.
Correlation between hemoglobin and ScvO2 and influence of hemodilution on ScvO2
Three patients received postoperative red blood cell transfusions; Table 1 shows their characteristics. In one patient who experienced severe blood loss of 1,460 g during surgery, the Hb concentration decreased from 13.6 g/dl preoperatively to 6.7 g/dl postoperatively, and ScvO2 fell to less than 60% before a blood transfusion was given. Figure 1 shows the postoperative course of this patient during the first postoperative day. On entering the ICU, the ScvO2 value was 56%, but a cardiac output greater than 4 l/min maintained a stable circulation. After beginning a blood transfusion, the Hb and ScvO2 values gradually improved to 11.3 g/dl and 72%, respectively. Two other patients who received blood transfusions without a clear physiological need had ScvO2 values greater than 65% just before their transfusion.
Postoperative course of central venous blood oxygen saturation (ScvO 2 ) and cardiac output in a patient with severe bleeding. The patient, a 62-year-old man, had undergone transthoracic esophagectomy and experienced intraoperative bleeding of 1,469 g. The chart shows his postoperative course after surgery. Closed circles, ScvO2 values; closed squares, cardiac output (CO). A blood transfusion was started on entering the ICU with 840 ml concentrated red blood cells (CRC)
From a retrospective analysis, Hb concentration and ScvO2 value in 40 patients every 8 h during ICU stay are plotted in Fig. 2. In patients with a Hb value around 7 g/dl who did not have a bleeding event and maintained a stable circulation, the ScvO2 could be greater than 70%. On the other hand, when the Hb level was less than 7 g/dl, some measurement points of ScvO2 did not become lower than 65%, and this patient could leave the ICU without any complication.
We also analyzed the influence of hemodilution on ScvO2 (Fig. 3). Unexpectedly, some points of Hb dilution ratio (sampling Hb/preoperative Hb) show more than 100%, which is supposed to be caused by hemoconcentration following an early shift to the diuretic state. The Hb dilution ratio did not show any correlation with ScvO2. Even when Hb was diluted to about 60% of the preoperative value, ScvO2 could remain above 65%.
Discussion
This study evaluated ScvO2 monitoring as a useful parameter for reflecting the adequacy of tissue oxygenation and attempted to clarify what is a better indicator of a physiological need for red blood cells in patients following transthoracic esophagectomy. Our findings clearly show that a low Hb concentration, even as a result of hemodilution, is not always correlated with a critical ScvO2 level. The findings further suggest that the trigger for red blood cell transfusions to improve oxygen supply should ideally be based primarily on ScvO2 rather than on the Hb value.
Traditionally, the indication for blood transfusion has been based primarily on Hb concentration [15], and in some instances blood transfusions are administered because of an arbitrary transfusion trigger rather than a physiological need for blood [16]. From our experience in using a PreSep oximetry catheter, it can be hypothesized that ScvO2 data could be better utilized to make this decision in a patient who has a risk of a massive bleeding accident during the perioperative period. Such patients often have a low Hb level even before esophagectomy, and then the Hb value is usually further decreased postoperatively by hemodilution of fluid administration during anesthesia or fluid resuscitation to correct circulatory instability. In such circumstances, as the original volume of Hb is unchanged in the patient’s body, basing the indication for blood transfusion principally on the Hb level is questionable. The primary objective of red blood cell transfusions is to improve Hb volume to increase oxygen transport capacity, and Hb supply is essentially unnecessary if the balance of oxygen supply and demand in tissues is well maintained. From that point, our study focused on usage of ScvO2 monitoring, which information would be a reasonable indication for Hb provision. The data of the relationship between Hb and ScvO2 assume that a grading decrease of Hb is not always correlated to a change of ScvO2 value (see Fig. 2). Therefore, it became apparent that so long as ScvO2 is adequately maintained above 65%, red blood cell transfusions should not be started too hastily for this type of anemia.
Postoperative hemodilution by not only fluid resuscitation but also caused by a shift from the third space to the vascular compartment often leads to a marked decrease of Hb concentration to around 7 g/dl. In this situation, there is a concern about how best to administer blood transfusions. The present study also evaluated the effect of hemodilution on oxygen supply/demand from the perspective of the ScvO2 value on Fig. 3. In patients who do not experience active bleeding and who maintain a stable circulation, ScvO2 can be greater than 65%, even if the Hb concentration is reduced to 60% of the preoperative value. In a pig model, Krantz et al. [17] reported the same finding: during progressive hemodilution, SvO2 and ScvO2 remained statistically unchanged until the hemoglobin concentration was reduced by 50%. It has been reported that severe penetrating injuries with 50% hemorrhage (in a pig model) [18] and cardiac arrest (in patients) [19] are associated with impaired systemic oxygen utilization and result in venous hyperoxia followed by increased plasma lactate. However, the patient in the present study who had an operative hemorrhage of about 1,460 g and a 50% fall in Hb from the preoperative level (Fig. 1) did not exhibit an abnormal plasma lactate concentration. Although his circulatory dynamics were maintained by adequate fluid resuscitation, a low ScvO2 of 50% suggested a reduction of tissue oxygen delivery. After starting a blood transfusion, the Hb level improved in this patient and ScvO2 returned to normal. This finding indicates that provision of Hb by red blood cell transfusion was appropriate for reversing the fall in ScvO2 and improving the patient’s clinical course. From the changes in ScvO2 levels in this patient, we can predict that measurement of ScvO2 may become both an indicator for starting blood transfusion therapy and an indicator for stopping transfusion. On the other hand, the ScvO2 value of two other patients before receiving a blood transfusion was more than 65%, which indicates oxygen supply in tissues is well maintained. Retrospectively, it may be possible to say that these patients has no physiological need or indication of Hb provision.
In conclusion, continuous measurement of ScvO2 with a fiberoptic central venous catheter can be accomplished more easily than with a PAC. Especially, the introduction of a PreSep oximetry catheter allows routine and safe monitoring of continuous ScvO2 values in the ICU, but the usefulness of the data thus acquired has been unclear. Another question is when we should start red blood cell transfusion and when we should stop it. From the present analysis of 40 patients in the postoperative period following transthoracic esophagectomy, it may be concluded that (1) ScvO2 is a better indicator of a physiological need for blood than the Hb concentration; (2) ScvO2 is not affected by hemodilution and lowering of Hb to around 60% of the preoperative value; and (3) the ScvO2 value become a indicator of not only a start but also a stop for blood transfusion.
References
Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176–86.
Kusano C, Baba M, Takao S, Sane S, Shimada M, Shirao K, et al. Oxygen delivery as a factor in the development of fatal postoperative complications after oesophagectomy. Br J Surg. 1997;84:252–7.
Gattinoni L, Brazzi L, Pelosi P, Latini R, Tognoni G, Pesenti A, et al. SvO2 Collaborative Group. A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med. 1995;333:1025–32.
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA. 1996;276:889–97.
Sandham JD, Hull RD, Brant RF, Knox L, Pineo GF, Doig CJ, et al. A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med. 2003;348:5–14.
Reinhart K, Kuhn HJ, Hartog C, Bredle DL. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30:1572–8.
Scheinman MM, Brown MA, Rapaport E. Critical assessment of use of central venous oxygen saturation as a mirror of mixed venous oxygen in severely ill cardiac patients. Circulation. 1969;40:165–72.
Scalea TM, Hartnett RW, Duncan AO, Atweh NA, Phillips TF, Sclafani SJ, et al. Central venous oxygen saturation: a useful clinical tool in trauma patients. J Trauma. 1990;30:1539–43.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Jakob SM. Multicentre study on peri- and postoperative central venous oxygen saturation in high-risk surgical patients. Collaborative Study Group on Perioperative ScvO2 Monitoring. Crit Care. 2006;10:R158.
Ando N, Ohtaka H, Miyoshi H, Fujisaki M, Fukuda T, Abe R. Studies of pre- and postoperative extravascular lung water changes in patients with esophageal cancer. Jpn J Surg Soc. 1983;84:310–20. (in Japanese with English abstract).
Japanese Society for Esophageal Diseases. Guidelines for clinical and pathological studies on carcinoma of the esophagus, 9th edn. Esophagus. 2004;1:61–88.
Kobayashi M, Ko M, Kimura T, Meguro E, Hayakawa Y, Irinoda T, et al. Perioperative monitoring of fluid responsiveness after esophageal surgery using stroke volume variation. Expert Rev Med Devices. 2008;5:311–6.
Kobayashi M, Irinoda T, Akiyama Y, Meguro E, Hayakawa Y, Funato O, et al. Effect of a selective neutrophil elastase inhibitor on early recovery from body water imbalance after transthoracic esophagectomy. Dis Esophagus. 2010;23:565–71.
Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, et al. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340:409–17.
Corwin HL, Parsonnet KC, Gettinger A. RBC transfusion in the ICU. Is there a reason? Chest. 1995;108:767–71.
Krantz T, Warberg J, Secher NH. Venous oxygen saturation during normovolaemic haemodilution in the pig. Acta Anaesthesiol Scand. 2005;49:1149–56.
Moomey CB Jr, Melton SM, Croce MA, Fabian TC, Proctor KG. Prognostic value of blood lactate, base deficit, and oxygen-derived variables in an LD50 model of penetrating trauma. Crit Care Med. 1999;27:154–61.
Rivers EP, Rady MY, Martin GB, Fenn NM, Smithline HA, Alexander ME, et al. Venous hyperoxia after cardiac arrest. Characterization of a defect in systemic oxygen utilization. Chest. 1992;102:1787–93.
Acknowledgments
We thank Content Ed Net, who provided assistance with English language and whose work was funded by Edwards Lifesciences, Japan. The authors have reported no potential conflicts of interest with any company/organization whose products or services are discussed in this article. The concepts discussed in this paper were presented at the 37th Annual Meeting of the Japanese Society of Intensive Care Medicine in Hiroshima, Japan, 4–6 March 2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kobayashi, M., Ko, M., Irinoda, T. et al. Clinical usefulness of continuous central venous oxygen saturation measurement for postoperative management of patients following transthoracic esophagectomy for carcinoma. Esophagus 8, 53–58 (2011). https://doi.org/10.1007/s10388-011-0260-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-011-0260-1