Abstract
Background
Pachychoroid, or the structural and functional abnormalities of the choroid, is one of the most important causes of exudative maculopathies. The purpose of this article is to review the current definitions of pachychoroid and their potential consequences.
Summary of findings
Most publications are from Asian countries. Although no consensus diagnosis has been reached, pachychoroid is defined by thickened choroid and choroidal vascular hyperpermeability, pachyvessels with inner choroidal attenuation; it is closely linked to pachydrusen. Although some studies suggest choroidal congestion may play a role in its pathogenesis, the exact causes of this condition are still unknown. Pachychoroid is associated with exudative maculopathies including central serous chorioretinopathy, pachychoroid neovasculopathy and polypoidal choroidal vasculopathy (PCV). It is widely accepted that macular neovascular membranes may develop secondary to pachychoroid. Recent clinical observations illustrate the importance of pachychoroid in the etiology of macular neovascularization including neovascular age-related macular degeneration (nAMD).
Conclusion
Pachychoroid is an important cause of exudative maculopathies. Both drusen and pachychoroid are increasingly recognized as important causes of macular neovascularization, and eyes formally categorized as typical nAMD or PCV can be further sub-categorized based on the presence or absence of pachychoroid and drusen. There is a need to develop a consensus definition, which will greatly enhance our understanding of pachychoroid and facilitate the development of individual interventions in pachychoroid diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Our understanding of the choroid has expended exponentially with the advent of high-resolution imaging modalities. In the 1990s, after the introduction of indocyanine green angiography (ICGA), researchers immediately noted marked abnormalities of the choroid in macular diseases, especially in exudative maculopathies such as central serous chorioretinopathy (CSC) [1,2,3] and neovascular age-related macular degeneration (nAMD). Choroidal vascular hyperpermeability (CVH) was first reported in eyes with CSC and the area of CVH was found to have filling defects in the early phase of ICGA. ICGA boosted the research of the choroid; many subsequent studies have confirmed CVH is highly prevalent not only in CSC but also in polypoidal choroidal vasculopathy (PCV) [4]. Furthermore, in the latter part of 2000, there was a rapid advance in optical coherence tomography (OCT) imaging technology. Among others, enhanced depth imaging (EDI) OCT provided novel insight into the choroidal structure for the first time [5] and drastically helped deepen our understanding of exudative macular diseases [6]. Quantitative studies using EDI-OCT disclosed that CSC is characterized by thickened choroid [7]. Many studies, especially from Asian countries, also note that the choroid is generally thicker in patients with PCV as compared to those with typical nAMD [8, 9]. Concomitantly, CVH was observed more frequently in eyes with PCV compared to eyes with typical nAMD. Initially, such features were thought to represent underlying differences in the pathogenesis between typical nAMD and PCV. However, there was a significant overlap in the choroidal thickness of typical nAMD and PCV. Additionally, not only PCV patients, but also typical nAMD patients, had CVH. Thus, major exudative maculopathies including CSC, PCV, and possibly typical nAMD, must share at least partly a common pathologic process in the choroid. The term, “pachychoroid”, was coined to systematically define such choroidal abnormalities [10]. The concept may also explain why there is a progression from one condition to another. In the late 2010s, growing appreciation of the structural and functional abnormalities of pachychoroid led to substantial improvements in our understanding and management of exudative maculopathies. The idea underlying pachychoroid is not difficult and the importance of the choroid in the management of patients’ eyes is now widely recognized. However, in spite of an abundance of publications, lack of consensus on the diagnostic criteria may lead to confusion in this field [11] and objective and reliable diagnosis of pachychoroid-related diseases might be difficult to come by. The areas that need expert consensus include diagnosis of pachyvessels, pachydrusen, pachychoroid neovasculopathy, pachychoroid pigment epitheliopathy (PPE), and their relationship with PCV and nAMD. This article will explain some of the basic ideas of pachychoroid and elaborate on their impact on our understanding of neovascular AMD based on an exhaustive literature review.
Methods
Publications dealing with pachychoroid and pachychoroid diseases were searched in December 2019 using PubMed. English-language studies were identified by the keywords: pachychoroid, pachydrusen and pachyvessel. Non-English-language studies were also reviewed if English abstracts were available. We identified 139 publications. Country name(s) of the publication, as documented in the affiliation, was determined by inserting the name of the country in the “affiliation” field in the advanced section of the PubMed search engine. This verified that most publications were from Asian countries. There were 28 from Korea, 20 from Japan, 6 from China, 4 Thailand, 3 from Hong Kong and 2 from Taiwan, whereas 11 were from the US and 4 from the UK. All were published after 2013. Additional information relevant to this review was also included using the reference lists of the publications. Clinical trials were searched with ClinicalTrials.gov in December 2019, which disclosed two completed studies; one dealing with treatment of PCV in pachychoroid and the other regarding OCT-A and CSC. All the above information was used to construct the current review.
Main findings
Pachychoroid is increasingly associated with macular diseases including those without exudative changes such as pachychoroid pigment epitheliopathy, and those with exudative changes such as CSC, pachychoroid neovasculopathy and PCV (Fig. 1).
Pachychoroid diseases. The term pachychoroid diseases encompasses a disease spectrum characterized by functional and structural abnormalities of the choroid. Pachychoroid diseases include, but are not confined to, pachychoroid pigment epitheliopathy, central serous chorioretinopathy, pachychoroid neovasculopathy and polypoidal choroidal vasculopathy. PCV polypoidal choroidal vasculopathy, PPE pachychoroid pigment epitheliopathy, PNV pachychoroid neovasculopathy, CSC central serous chorioretinopathy
Characteristic clinical features of pachychoroid
Multimodal imaging is used to diagnose pachychoroid. Key imaging modalities include ICG angiography, OCT and OCT-angiography (OCT-A). ICG provides detailed choroidal vascular structures including dilation of the choroidal vessels, as well as CVH. OCT provides information about the structure of the choroid such as choroidal thickness and choroidal vessel dilatation. OCT-A visualizes the choroidal flow. It is generally agreed that pachychoroid is characterized by (1) CVH, (2) thick choroid, (3) dilated choroidal vessels (pachyvessels) with inner choroidal attenuation and is closely linked to (4) drusen like deposits (pachydrusen). There is no consensus on the quantitative definition of pachychoroid. Each study uses its own definition and maximum caution should be exercised when comparing papers that use quantitative values. A set of the following multimodal imaging findings is recommended for use in the diagnosis of pachychoroid.
Choroidal vascular hyperpermeability
ICGA was the first imaging modality used to investigate choroidal abnormalities and implicated functional abnormalities, including CVH, in macular diseases. ICGA still holds a place in the diagnosis and management of pachychoroid spectrum diseases, although recent studies are focused more on the utility of non-invasive imaging devices, such as OCT and OCT-A, which also clarify structural and morphological abnormalities. CVH is defined as multifocal areas of hyperfluorescence with blurred margins in the late phase of ICGA [3] (Fig. 2b, d, e–g). This is usually accompanied by dilated and hyperpermeable choroidal veins. In the early phase of the ICG angiography, filling defects are also observed (Fig. 2c). Thus, CVH is still a most salient feature of pachychoroid. However, CVH is not always part of pachychoroid diseases.
Choroidal vascular hyperpermeability. Choroidal vascular hyperpermeability can be observed in eyes with pachychoroid. a PCV eye with no choroidal vascular hyperpermeability. b PCV eye with choroidal vascular hyperpermeability. Early (c) and late (d) phase in ICGA of an eye with choroidal vascular hyperpermeability. Note that in the early phase, there are areas of choroidal filling delay. In the late phase of ICGA, the corresponding area becomes hyperfluorescent. The area of central hyperfluorescence, corresponding to the PCV lesion, i.e., branching vascular network and polypoidal lesion, should not be confused with choroidal vascular hyperpermeability. e–g Eyes with choroidal vascular hyperpermeability with various degrees. e Mid phase ICGA showing prominent hyperfluorescence. f, g Late phase ICGA showing a wide area of hyperfluorescence, illustrating the importance of wide field ICGA in detecting choroidal vascular hyperpermeability. Black areas with blurred margins in g are due to vitreous opacity
CVH was first described in CSC [3], and eyes with CSC were also found to have dilated choroidal veins [12]. Thereafter, eyes with PCV were found to have CVH, although CVH was less frequently observed in eyes with PCV compared to eyes with CSC [4]. In eyes diagnosed as typical neovascular AMD, a substantial portion (9–38%) had CVH [4, 9, 13]. Similarly, a study investigating the characteristics of eyes with CNV accompanied by CVH reports that type 1 CNV [beneath the retinal pigment epithelium (RPE)] was more frequent than previously thought, although type 2 CNV (between the sensory retina and RPE) and PCV were also observed [14]. Previously, type 1 CNV was found to develop after chronic CSC [15], however, as some studies conclude, “CNV secondary to CVH” is more appropriate than “CNV secondary to CSC” in describing most of the nAMD cases with CVH [14, 16], because CNV secondary to CSC constitutes only a subset of CNV secondary to CVH. Additionally, observational studies clarify that nAMD with CVH presents with broad changes in the RPE and choroid, and may have distinguishing clinical characteristics [14, 16]. Thus, type 1 CNV accompanied by CVH appears to be a distinct disease entity. This led to the concept of pachychoroid neovasculopathy. The detailed definition of pachychoroid neovasculopathy will be discussed later.
Choroidal thickening
As the prefix “pachy” suggests, thickened choroid is the most prominent feature of pachychoroid (Figs. 3a, b, 4a). Therefore, cross-sectional OCT images with clearly visualized choroid are most important in the diagnosis of pachychoroid. The increase in choroidal thickness suggests that elevated hydrostatic pressure within the choroid may be a key pathophysiological factor in pachychoroid diseases.
Pachyvessels and inner choroidal attenuation on cross sectional OCT. Pachyvessels with thick (a, c) and thin (b) choroids. a, b Note that inner choroid attenuation colocalizes with pachyvessel (asterisk). Right panels (magnified images) show that the inner choroid overlying pachyvessels is attenuated (arrows). Borders of the inner and outer choroid are indicated by dashed lines. b Pachyvessels with thin choroids. Note the relatively large-diameter choroidal vein occupying most of the stroma. A choroidal vessel (asterisk) is dilated, extends into the inner choroid, and colocalizes with the area of the inner choroidal atrophy. The shape of the pachyvessel is non-circular and irregular, suggestive of the dilatation of the vessel. c There is an increased “luminal” volume, black patches, in the choroid throughout the scan, suggestive of diffuse dilatation of the choroidal veins. There is a shadowing artifact at the central choroid, which partly obscures pachyvessels
Pachyvessels and inner choroidal attenuation on en face OCT. En face OCT generated using SS-OCT scans of the case from Fig. 3a. a Choroidal thickness map shows focally increased choroid. b En face image at the level of choriocapillaris shows attenuation of choriocapillaris as a dark area of reduced reflectivity (arrowhead). The dark area corresponds to the dilated choroidal vessel(s) at the inner choroidal (c, arrow head) and deep choroidal layers (d, arrows)
Earlier studies defined “pachychoroid” as (1) choroidal thickness in excess of 270 μm and (2) the presence of dilated choroidal vessels (pachyvessels) [17]. Additionally, cases with an extrafoveal focus of maximal choroidal thickness exceeding subfoveal choroidal thickness by at least 60 μm were included [10]. However, such cut-off values are arbitrary and other studies used different cut-off values [18, 19]. When interpreting the choroidal thickness, it is important to note that there is an age-dependent decrease in the choroidal thickness and that there are also diurnal variations and gender differences. There are differences in measurement depending on OCT technology. There is also no consensus as to whether we should use choroidal thickness or volume as the measurements’ standard.
It is also important to note that thick choroid is not equivalent to pachychoroid. For example, eyes with Vogt–Koyanagi–Harada disease are characterized by thickened choroid [20], however, these should not be considered as pachychoroid, since choroidal thickening is due to inflammation, and is not characterized by dilated choroidal vessels. As is already well accepted, CSC is caused by increased choroidal osmotic pressure, as evidenced by increased choroidal thickness and breakdown of the outer blood retinal barrier, which leads to serous retinal detachment [3, 21]. As such, rather than a thickened choroid itself, dilation of the choroidal vessels (pachyvessels) is the important hallmark of pachychoroid as discussed in the next section; therefore, qualitative analysis of OCT is also important.
Although pachychoroid diseases are characterized by thickened choroid, its thickness is different depending on the disease type. As is demonstrated in studies using cross-sectional OCT, when the choroidal thickness was compared among pachychoroid spectrum diseases, the choroidal thickness was reportedly thickest in CSC, followed by PPE and then, PCV [22].
Pachyvessels (dilated choroidal vessels) with inner choroidal attenuation
Dilated choroidal vessels in Haller’s layer are referred to as pachyvessels (Fig. 3). Most recent studies suggest that pachyvessels may play a pivotal role in the pathogenesis of pachychoroid. Pachyvessels can be best visualized by en face SS-OCT images [23] (Fig. 4). ICGA is also useful in detecting pachyvessels. Cross sectional OCT can be used to diagnose pachyvessels. However, the diagnosis of abnormally dilated choroidal vessels is complicated by the great variability in the shape of these vessels. Not all that appears as black patches in the choroid on cross sectional OCT are pachyvessels. It is generally believed that pachyvessels are associated with inner choroidal attenuation (Figs. 3a, b, 4b–d).
Some studies focus on the morphological features of pachyvessels. Morphologically, vascular density in the large choroidal vessel layer and pachyvessel pattern was similar between CSC and thick choroid PCV and between AMD and thin choroid PCV [24]. There are several attempts to classify choroidal veins, or “macular vortex veins”, based on their morphology on en face OCT [25, 26]. Asymmetrical watershed zone (or asymmetrical “macular vortex veins”) or disappearance of horizontal choroidal watershed may be a characteristic finding of the pachychoroid spectrum diseases [25]. It is also hypothesized that anastomosis between the superior and inferior vortex veins may be a characteristic feature of pachychoroid [26]. Such hypotheses, if proven, may support the presence of longstanding congestion of choroidal veins in pachychoroid, and may facilitate our understanding of the pathogenesis of pachychoroid diseases; however, there are also cases without choroidal anastomosis in pachychoroid diseases. Moreover, asymmetry of the watershed zone may be observed in normal subjects as well [27]. Therefore, further studies are warranted to assess this idea.
Several studies try to identify stromal and luminal areas using cross sectional OCT, and show that the increase of luminal to total choroidal area was most prominent in eyes with CSC compared with PPE and pachychoroid neovasculopathy (PNV), suggesting somewhat different predominant pathogenic processes involving these three conditions [22, 28]. However, other studies found the opposite, showing that the choroidal stroma and lumen ratio were not different among CSC, PPE and uncomplicated pachychoroid [22]. Further studies are needed to clarify whether differences exist between these three pachychoroid diseases.
Importantly, pachyvessels are typically associated with inner choroidal attenuation (Figs. 3, 4), although sometimes it is not explicitly mentioned in papers analyzing pachyvessels. Inner choroidal attenuation and ischemia of the choriocapillaris may subsequently upregulate angiogenic factors such as vascular endothelial growth factor (VEGF). They may also lead to outer retinal atrophy due to ischemic changes. Therefore, inner choroidal attenuation may be directly linked to the progression of pachychoroid diseases.
Several studies identify inner choroidal flow impairment in eyes with, or fellow eyes of CSC as well as other pachychoroid diseases [29,30,31]. Inner choroidal attenuation overlying pachyvessels can be observed by close inspection of the cross-sectional OCT scans, and some studies point out that the pachyvessels colocalized with the area of inner choroidal attenuation. Flow signal deficit associated with inner choroidal attenuation can also be visualized by OCT-A. Using OCT-A, choriocapillaris flow deficits, or flow voids, were observed in eyes with PPE, overlying pachyvessels [30, 31]. Reduced choriocapillaris’ flow appeared to be associated with increased choroidal thickness and CVH [32]. Even in eyes with earlier stages of pachychoroid, i.e., pachychoroid without PPE, the area of choriocapillaris flow impairment was larger than controls [33]. In eyes with CSC, choriocapillaris’ vessel density may be reduced in CSC [34], however, caution should be paid to its interpretation because there may be artefacts due to signal attenuation caused by serous detachment in CSC.
These observations generated the hypothesis that pachyvessels are compressing the inner choroid and causing attenuation. However, no studies clarify its underlying causality. It is also possible that pachyvessels are secondary to inner choroidal attenuation.
Pachydrusen (drusen-like deposits)
Classifications of drusen and drusenoid deposits are gaining importance. There are differences in the morphology of drusen between Asians and Caucasians [35] and soft drusen, especially with an indistinct border, have long been accepted as a risk for developing late AMD in Caucasian populations. However, it is not clear which drusen subtypes are at risk of late developing AMD in Asians. Recently a new type of extracellular deposits was recognized as drusen-like deposits, or pachydrusen [36,37,38,39]. These are supposedly prevalent in Asian AMD eyes at a relatively high frequency. Pachydrusen are traditionally categorized into soft drusen based on their size, and distinct-type drusen based on their contour. Importantly, they are found in eyes with thick choroids [36, 40]. Eyes with pachydrusen and soft drusen seem to have different characteristics when considering their risk for developing exudative changes. Hence, pachydrusen should be differentiated from typical soft drusen.
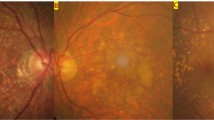
Pachydrusen have the following characteristics: (1) size > 125 μm (large drusen), (2) irregular outer contours with better defined outer borders, (3) scattered distribution over the posterior pole, (4) present in isolation or in groups of only a few yellow-white deposits and (5) typically associated with thick choroids (reduced tessellation), especially when located at the macula (Fig. 5). The distribution pattern of pachydrusen is different from that of typical soft drusen. Prevalence and association with pachychoroid features have been studied intensively over the last few years. There are significantly more eyes with pachydrusen in Asians than in Caucasians [36, 41]. Among Asians, the prevalence of pachydrusen seems to be low in Indians [42, 43].
Pachydrusen. Color fundus photographs showing an eye with soft drusen (a) and pachydrusen (b–d). Pachydrusen has the following characteristics: (1) size > 125 μm (categorized as large drusen), (2) irregular outer contour with clearly defined outer border, (3) a scattered distribution over the posterior pole, (4) present in isolation (c, d) or in groups of only a few yellow-white deposits (b) and (5) typically associated with thick choroids (reduced tessellation), especially when located at the macula. There is a great variability in the location and the number of pachydrusen. Some are located at the nasal to the optic disc (d)
Importantly, accumulating evidence supports the idea that pachydrusen is associated with the pachychoroid. In Asian cohorts, patients with PCV were more likely to have thicker choroids and pachydrusen, whereas pseudodrusen were associated with a thin choroid. In an Asian cohort, pachydrusen were shown to be prevalent in typical nAMD (40.4%) and PCV (47.8%) but not in retinal angiomatous proliferation (RAP), whereas no drusen were found in 24.3% of typical nAMD, nor in 43.3% of PCV [36]. In eyes with typical nAMD, the prevalence of CVH was higher in the pachydrusen group than in other groups. The prevalence of pachydrusen in PCV was similar in another Korean cohort where pachydrusen were found in 49.1%, while soft drusen was found in 12.3% and pseudodrusen in 6.9% [36]. CVH was noted only in the pachydrusen group. Additionally, pachydrusen reportedly colocalized with pachyvessels and attenuated choriocapillaris [39]. Pachydrusen are also present in eyes with CSC, and colocalized with choriocapillaris filling delay and pachyvessels [38]. CVH was found in 41.1% and pachyvessels were detected in 80.6% of eyes with pachychoroid [37]. Although further studies are needed to clarify how specific pachydrusen are for pachychoroid, these studies show a strong association between pachydrusen and pachychoroid.
Initially, pachydrusen were considered to confer a risk of PCV [40]. However, it seems pachydrusen may not be a high risk factor for developing exudative changes [44, 45]. In a study which investigated the fellow eyes of unilateral nAMD, soft drusen, pseudodrusen and combination of both had a higher risk of developing nAMD, but pachydrusen did not confer significantly higher risk of exudative changes compared to the non-drusen group [45]. Similarly, in another retrospective study of a Japanese cohort, eyes with pachydrusen were less likely to develop exudative changes compared with soft drusen and pseudodrusen (plus soft drusen) group [44].
Pachychoroid diseases
Pachychoroid spectrum diseases include diseases characterized by the aforementioned choroidal findings (pachychoroid). “Uncomplicated pachychoroid (UCP)” refers to pachychoroid without epitheliopathy or exudative changes. CSC, PPE, PNV and PCV share similar morphologic changes in the choroid; i.e., increased choroidal thickness, dilated outer choroidal vessels, and disease foci colocalizing with dilated choroidal vessels.
Pachychoroid pigment epitheliopathy
Pachychoroid pigment epitheliopathy is a condition characterized by pigmentary changes and/or small pigment epithelial detachments, and pachychoroid features such as CVH and choroidal thickening (Fig. 6), which likely represents a “forme fruste” of CSC [10]. Since none of the eyes with pachychoroid pigment epitheliopathy had clinically evident subretinal fluid in the initial report, CVH and/or choroidal thickening alone was considered to cause pigment epitheliopathy. This may be partially supported by the fact CVH was more frequent in eyes with PPE compared to eyes with UCP [46]. Pachychoroid pigment epitheliopathy is observed commonly in the fellow eyes of patients with unilateral CSC [47]. A retrospective study demonstrates that eyes with pachychoroid pigment epitheliopathy may develop CSC. The study classified pachychoroid pigment epitheliopathy into four patterns; RPE thickening, pigment epithelial detachment, and RPE elevation with microbreak appearance and suspects that RPE elevation with microbreak appearance may be a precursor lesion for pachychoroid disease [48].
Pachychoroid Pigment Epitheliopathy. Pachychoroid pigment epitheliopathy is a condition characterized by pigmentary changes (a, color fundus photo and b: fundus autofluorescent image) and pachychoroid features such as CVH and choroidal thickening (c), with no prior history of exudative maculopathies and other degenerative diseases
Pachychoroid pigment epitheliopathy may precede outer retinal atrophy (Fig. 1). A study found that outer retinal atrophy (i.e., thinning of outer nuclear layer and the outer plexiform layer) in eyes with pachychoroid pigment epitheliopathy is more common than in eyes with uncomplicated pachychoroid and controls, suggesting that the degenerative process begins with RPE alterations before fluid accumulation [49]. Another study found focal disruption of both the ellipsoid and interdigitation zones on SD-OCT in eyes with pachychoroid pigment epitheliopathy, supporting the idea that pachychoroid pigment epitheliopathy may precede outer retinal atrophy [50]. Pachychoroid is also found in eyes with geographic atrophy (GA). Pachychoroid GA is genetically and morphologically different from drusen-associated GA [51].
Pachychoroid pigment epitheliopathy may be complicated with quiescent pachychoroid-associated neovascularization. Recent studies also focus on pachychoroid pigment epitheliopathy in the fellow eyes of unilateral nAMD. Roughly 20% eyes with unilateral nAMD and PCV have non-exudative CNV, and the presence of pachychoroid pigment epitheliopathy was the only factor associated with non-exudative neovascular membrane [52, 53]. Therefore, the presence of PPE in the fellow eyes of unilateral nAMD poses a risk of pachychoroid neovasculopathy and subsequent exudative changes. It should also be noted that intraretinal fluid (retinoschisis) may be accompanied with focal RPE atrophy, even without CNV [54].
Pachychoroid neovasculopathy
Pachychoroid neovasculopathy is macular neovascularization in eyes with pachychoroid features, which typically do not have drusen or other risk factors for neovascularization [17] (Fig. 7). Pachychoroid neovasculopathy in middle aged patients may have been diagnosed as CSC, and in elderly patients it may have been diagnosed as nAMD. Specifically, eyes with long-standing CSC, and those which had a known history of CSC were initially found to develop type 1 neovascular membranes over their course of follow up, probably due to choroidal changes [15]. Later on, the term pachychoroid neovasculopathy was introduced to describe the condition characterized by type 1 neovascular membrane secondary to pachychoroid, not only secondary to CSC. It is suggested that “pachychoroid neovasculopathy falls within a spectrum of diseases associated with choroidal thickening that includes pachychoroid pigment epitheliopathy, CSC, and PCV, which should be considered as a possible diagnosis for eyes with features of type 1 neovascular membrane and choroidal thickening in the absence of characteristic age-related macular degeneration or degenerative changes.” A thick choroid is not necessarily required for diagnosis, because pachychoroid neovasculopathy may occur as a focal abnormality within the macula (Fig. 3c) and it may occur even in myopic eyes [17], provided that pachychoroid features are present.
Pachychoroid Neovasculopathy. Pachychoroid neovasculopathy, or macular neovascularization in eyes with pachychoroid feature(s). a Color fundus photograph showing subretinal fluid. Note reduced tessellation, suggestive of thick choroid. There are no drusen or other degenerative changes associated with neovascularization (b) OCT showing choroidal thickening, pachyvessels with inner choroidal attenuation (asterisks). Flat irregular RPE detachment is indicated by arrows. Early (c) and late (d) phase of fluorescein angiography, showing late leakage of a smoke stack pattern. Neovascular membrane is not noticeable on fluorescein angiography (e, f). ICGA shows hypercyanescence in the early (e) and late (f) phase. Note there are areas of CVH in the late phase ICGA (f, temporal to the fovea), indicative of pachychoroid. En face OCT images from the outer retinal (g) and choriocapillaris (h) slab, clearly showing the neovascular membrane. As shown in this case, OCTA is most useful in detecting neovascular membrane in pachychoroid
The peculiar flat irregular morphology of type 1 neovascular membrane in pachychoroid neovasculopathy is described in various works on pachychoroid-driven neovascularization. In general, type 1 neovascular membrane can be categorized into (at least) two subtypes; one with high RPE elevation, typically observed as fibrovascular pigment epithelial detachment (PED) on fluorescein angiography, and the other with shallow RPE elevation, typically found in eyes with late leakage of undetermined source [55]. Among them, shallow (or flat) irregular RPE detachment was initially considered as a finding peculiar for PCV and reported as double layer sign [56, 57]. The RPE detachment corresponds with branching vascular network in PCV. Thereafter, the shallow irregular RPE detachment is also reported in occult CNV, and has become widely accepted as a special form of type 1 neovascular membrane between RPE basement membrane and Bruch membrane [57]. Type 1 neovascular membrane presenting as a shallow irregular RPE detachment was also found to be characteristic for pachychoroid neovasculopathy [17] (Fig. 7b). Many publications confirm that neovascular membranes in pachychoroid are characterized by shallow irregular RPE detachment with moderate reflectivity. The growth pattern of this type 1 CNV appears to be different from CNV characterized by higher PED, including fibrovascular PED. There is additional evidence to support flat irregular RPE detachment as specific for pachychoroid neovasculopathy. Eyes with CSC sometimes are known to be complicated by PED. The two major types of PED are focal and flat irregular; among these types, flat irregular PED in CSC could be a form of pachychoroid neovasculopathy [58, 59].
Type 1 neovascular membrane in shallow irregular RPE detachment can be better diagnosed with OCT-A than with dye angiography [60]; importantly, OCT-A also detects substantial proportion of eyes with pachychoroid neovasculopathy at a quiescent stage [61, 62].
Aqueous humor cytokines are important biomarkers that reflect pathogenesis and/or activity of CNV. Several studies tried to differentiate aqueous humor cytokines from pachychoroid neovasculopathy and other causes (such as nAMD) in macular neovascularization [63,64,65]. The results suggest VEGF concentration and angiogenic factors may be lower in pachychoroid neovasculopathy compared to CNV due to AMD.
Eyes with pachychoroid neovasculopathy respond to anti-VEGF therapy and PDT differently from eyes with nAMD. These eyes reportedly responded favorably to anti-VEGF therapy [66,67,68,69] as well as photodynamic therapy (PDT) [70], and a combination of both [71]. Several reports show that pachychoroid neovasculopathy needed fewer injections compared to typical nAMD [67, 69, 72]. A retrospective study compared the efficacy of ranibizumab and aflibercept reducing the subfoveal choroidal thickness at 3 months, and aflibercept was reportedly superior to ranibizumab in achieving dry macula and reducing choroidal thickness at 3 months [68]. As pachychoroid neovasculopathy may be diagnosed as CSC with type 1 neovascular membrane, some physicians also treat the affected eyes with PDT [70]. Choroidal thickness decreased after anti-VEGF injections, which might be attributable to a reduction in CVH [67, 68, 72] However, one study shows that CVH was associated with poor response to intravitreal aflibercept [73]. Large-scale studies are needed to confirm the treatment efficacy of the various modalities; there is a lack of reliable evidence and clinical guidance to support treatment with anti-VEGF therapy, PDT or combination of both.
Polypoidal choroidal vasculopathy
The concept of PCV is still evolving. For interested readers, a recent extensive review is recommended [74]. This section details brief historical perspectives. How has PCV become considered as pachychoroid disease and why is there an argument of pachychoroid neovasculopathy being its precursor.
Why is PCV considered pachychoroid-related?
First, similarities between CSC and PCV are well documented. CVH on ICGA was first described in CSC but subsequently also reported in eyes with PCV. Thus, CVH was not considered unique to CSC and was also considered as a characteristic finding in PCV. Other pachychoroid features, including a focal or diffuse increase in choroidal thickness, CVH, and dilated choroidal vessels, were first described in eyes with CSC. A retrospective study clarified that 2.2% of patients with typical nAMD and 12.3% of patients with PCV had a history of CSC [75]. As anticipated from the history of CSC, it has now been found that the choroid is thicker in the macular region of patients with PCV than in eyes with typical AMD [9]. Subsequently, in patients with PCV, the subfoveal choroid was found to be thicker in eyes with CVH, compared to those without CVH.
Second, evidence suggests that pachychoroid-associated neovascularization may be a precursor lesion for PCV. As has been discussed in previous sections, pachychoroid neovasculopathy is sometimes found at an indolent stage without exudation [52, 62]. Such quiescent pachychoroid neovasculopathy may develop flank exudations without developing polypoidal lesions. However, over a long term, polypoidal lesions may develop indolently at the terminal of pachychoroid neovasculopathy. Such lesions may eventually cause serosanguinous changes typically found in PCV. Indeed, a study of the fellow eyes of unilateral typical nAMD and PCV suggests that “branching vascular network” may present in 18.8% of the fellow eyes of unilateral nAMD, and was the significant risk factor for developing PCV or CNV [53]. It is possible that such “branching vascular networks” were actually pachychoroid neovasculopathy and may develop polypoidal dilatation at the terminal point in some of the eyes. This is, at least in part supported by the finding that branching vascular networks, and even polypoidal lesions, are found long before the development of exudative changes in the fellow eyes of unilateral PCV [76]. Thus, the recent expansion of our understanding of pachychoroid has raised fundamental questions as to whether PCV differs from pachychoroid neovasculopathy and that these 2 conditions are not distinct diseases but simply represent different stages of the same spectrum disorder [17]. It is, however, still unclear whether all PCV cases develop from pachychoroid neovasculopathy as discussed in the last section.
Other pachychoroid spectrum diseases
It is likely that pachychoroid is also associated with focal choroidal excavation [77] peripapillary exudative changes (peripapillary retinoschisis [78] and peripapillary pachychoroid syndrome [79]). For interested readers, an excellent review published recently is recommended [80].
Asian nAMD and pachychoroid
Asian nAMD
There are both important similarities and differences between traditional and Asian nAMD. In both Asians and Caucasians, AMD is classified into early and late, the latter consisting of geographic atrophy and neovascular AMD (nAMD) [81]. Traditionally, as the word implies, nAMD is a condition characterized by the presence of any signs of AMD (i.e., drusen and pigment abnormalities) [82], and eyes with no visible drusen or pigmentary abnormalities should be considered to have no association with AMD. However, in Asian countries, the diagnosis relies mainly on dye angiography and the presence of drusen is not always required. Thus, nAMD can manifest with widely diverse clinical features and can be categorized into “typical” nAMD, PCV and type 3 CNV or RAP [83]. Although there is no definite diagnostic criteria to distinguish between the 3 conditions [84] elderly patients with macular neovascularization (MNV) are commonly diagnosed as nAMD after excluding possible other causes, such as degenerative myopia and uveitis. Diagnostic criteria agreed by Japanese experts state that the diagnosis of nAMD is certain when one of the following conditions in present: (1) choroidal neovascularization, (2) serous retinal pigment epithelial detachment, (3) hemorrhagic retinal pigment epithelial detachment, or (4) fibrotic scar in the macula [85]. These clinical criteria are considered useful because in Asia drusen are rare and PCV is highly prevalent in eyes with MNV [83].
Diagnosis of typical AMD is made only after excluding PCV and RAP. PCV has been classified as part of the late stage of AMD because it meets the late age related maculopathy (ARM) criteria of the International ARM Epidemiological Study Group [81]. The diagnosis of PCV is made if the diagnostic criteria (Japanese or EVEREST criteria) are met [85, 86]. RAP is diagnosed by the presence of characteristic intraretinal neovascularization (IRN) [87, 88]. As such, typical nAMD does not necessarily represent nAMD associated with drusen, although the term “typical” nAMD (sometimes abbreviated as tAMD) is used in many AMD papers from Asian countries often interchangeably with the term “CNV-AMD” or “typical AMD” [89].
It is accepted that drusen act as a driver for chronic inflammation conferring a risk of neovascular AMD and are considered as an important contributor to the pathogenesis of AMD [90]. However, in Asians, MNV development may differ from the classic, well-documented drusen-dependent pathways [84, 91] and pachychoroid-driven pathways may also exist (Fig. 8).
Two major pathways in macular neovascularization. The classical pathway of macular neovascularization (upper side) involves age-related generation, clinically defined by drusen. Drusen-associated macular neovascularization in AMD is associated with VEGF. The pachychoroid pathway (lower panel) is characterized by structural and functional abnormalities of the choroid. Pachychoroid pathway starts with pachychoroid pigment epitheliopathy and CSC, and subsequently triggers neovascular process. Both pathways may lead to the formation of neovascular membrane, and eventually exudative and hemorrhagic changes
Subclassification of typical nAMD
The diverse pathologic processes involved in “typical nAMD” make it imperative that we further sub-classify it, basing the subclassification on pachychoroid and drusen. Because the evidence suggests MNV characterized by pachychoroid is not necessarily dependent on VEGF, detailed classification may aid in the development of novel treatment strategies. Therefore, the choroidal structure may not only play a role in assessing the risk of developing MNV, but also aid in developing individualized treatment. There is, therefore, a need to classify typical nAMD into drusen-driven MNV and pachychoroid driven MNV; lack of such argument had been limiting our ability to systematically compare Asian nAMD and Caucasian nAMD.
How can pachychoroid neovasculopathy be distinguished from nAMD? The current diagnostic criteria of pachychoroid neovasculopathy can be summarized as (1) presence of pachychoroid features and (2) absence of drusen [17, 19, 63, 64, 66, 80]. This may be predicated on the idea that MNVs belong to two clearly defined categories, those with pachychoroid and those with drusen. However, there are MNV with pachychoroid features and concomitant drusen (Fig. 9), as well as cases without pachychoroid features or drusen. Additionally, most studies were conducted before the notion of pachydrusen was introduced, and probably excluded eyes with pachydrusen from pachychoroid neovasculopathy, even if the characteristic pachychoroid features had been observed. However, there is a close link between pachydrusen and pachychoroid. Therefore, pachychoroid neovasculopathy in previous reports cannot be associated with eyes afflicted by pachydrusen and pachychoroid, thus limiting the applicability of the data in these works to clinical practice. As such, using “pachychoroid” and “non-pachychoroid” classification in typical nAMD is problematic in patient care; there also remains ambiguity about how best to diagnose pachydrusen.
Pachychoroid driven MNV with multiple soft drusen. Drusen (a) are considered a typical manifestation of AMD; therefore, the eye shown is not diagnosed as “pachychoroid neovasculopathy” by the current definition. While the eye does not meet current definitions of pachychoroid neovasculopathy, the presence of choroidal vascular hyperpermeability and pachyvessels on ICGA (d) is suggestive of pachychoroid-driven. In addition, the neovascular membrane, which is not noticeable on dye angiographies (c, d), is clearly detected on OCTA (e). Furthermore, flat irregular RPE detachment on OCT (b) is also suggestive of pachychoroid driven mechanism
How should we classify eyes with typical nAMD? A logical approach would be to categorize MNVs into 4 groups (Fig. 10), based on the presence or absence of drusen and pachychoroid. Eyes with drusen but without pachychoroid features can be classified into drusen-associated macular neovascularization. This type would be the closest to Caucasian nAMD. Those with pachychoroid features but without drusen can be categorized into pachychoroid-driven macular neovascularization. This subtype represents pachychoroid neovasculopathy. Those with both drusen and pachychoroid can be classified into mixed type MNV. In such cases, attention should be paid to other clinical features to determine whether drusen or pachychoroid is the main driver of the MNV. Specifically, typical MNVs secondary to pachychoroid is type 1 CNV, accompanied by serous exudative changes, rather than hemorrhagic changes. Lastly eyes without drusen or pachychoroid may be regarded as “idiopathic” MNV.
Proposed classification of “typical nAMD”. *ICGA: choroidal vascular hyperpermeability, dilated choroidal vessels, CSC/PPE-like RPE abnormalities. †Drusen associated (Caucasian-type) nAMD, ‡Pachychoroid driven. CNV pachychoroid neovasculopathy, CSC central serous chorioretinopathy, PPE pachychoroid pigment epitheliopathy
There are several issues that pose challenges to the subclassification of typical nAMD into the 4 groups. Most importantly, there are no standardized diagnostic guidelines for pachychoroid. Even among experts in this field, the interpretation of cases with ambiguous borderline clinical presentation might be challenging. Nonetheless, for better treatment strategies and patient care, the 4-group classification system proposed in this review would be useful to complement conventional classification.
Subclassification of PCV
Even before the introduction of the pachychoroid theory, some investigations suggested that PCV can be classified into two types, typical (idiopathic) and polypoidal CNV (secondary polyps associated with nAMD) [92,93,94]. These classifications are based on the hypothesis that these two subtypes differ in their etiology and, therefore, there are morphological and genetic differences between the two groups. More recent classification is based on the presence of pachychoroid, and distinguishes pachychoroid and non-pachychoroid eyes according to the presence of pachychoroid or AMD features and the previously described subtypes of PCV are shown to be different in terms of angiographic and tomographic features, as well as visual outcomes [95].
Based on choroidal findings, PCV could be subdivided into pachychoroid and non-pachychoroid. Such classification looks rational; recent studies support that pachychoroid PCV and non-pachychoroid PCV respond differently to photodynamic therapy (PDT). Pachychoroid PCV responds poorly to anti-VEGF therapy; PDT is reportedly more effective and anti-VEGF therapy is less effective in terms of vision compared to non-pachychoroid PCV [18, 71, 96]. Therefore, it seems rational to divide PCV into these two subtypes. It is likely that PCV originates, at least in part, in pachychoroid neovasculopathy.
What is “non-pachychoroid” PCV? Now that we are elucidating the different prognosis of pachychoroid and non-pachychoroid PCV, we need to focus on its etiology. There are two possibilities. First, PCV may be a distinct condition with a single etiology characterized by pachychoroid. In this regard, it should be noted that pachychoroid features can be found in PCV eyes even when the choroid is thin [97]. Second, PCV may be an etiologically heterogenous condition. For example, although the prevalence of drusen is low in PCV, drusen are still sometimes present in eyes with PCV; PCV can develop in eyes with drusen-driven nAMD. The question arises whether in eyes with PCV, the MNV had been initiated by drusen similar to nAMD. Further studies are needed regarding this pathogenesis using standardized diagnostic criteria.
Future directions
Pachychoroid is a research field that is advancing at a fast pace. This article is the result of a comprehensive literature review conducted in December 2019 that identified more than 100 publications. However, despite the large number of publications, due to the lack of expert consensus on the definition of this condition it is still difficult to diagnose pachychoroid unambiguously. There is an urgent need to establish common diagnostic criteria for pachychoroid.
In the future, studies need to include the identification of the gene(s) involved in this condition, as this review did not include genetic studies because only a few limited studies in this field seem to have replicated studies [19, 51, 98,99,100]. Molecular mechanisms and pathophysiology underlying pachychoroid are yet to be confirmed too. Although obstruction of the scleral outflow can cause choroidal vessel dilatation, there is disagreement as to whether congestion of the choroidal veins can induce changes observed in pachychoroid in an animal model.
Modern multimodal imaging technologies and newer analytic methods are beginning to elucidate common choroidal features among pachychoroid diseases. At the same time, it has become clear that there is a great variability in the degree of the choroidal abnormalities in an apparently homogenous disease entity. For example, although clinical manifestations of CSC may not be different among patients, the choroid in CSC looks very heterogenous in terms of the extent of CVH, diameter of pachyvessels and the degree of inner choroidal attenuation, and choroidal thickness - to say nothing of pachychoroid neovasculopathy and PCV. Is the inner choroidal attenuation the main etiology of pachychoroid spectrum diseases? Etiology-based classifications of exudative maculopathies are needed, as they will facilitate the development of individual interventions in pachychoroid diseases. There is also a need to develop a consensus definition which is essential to our understanding of pachychoroid diseases.
References
Spaide RF, Hall L, Haas A, Campeas L, Yannuzzi LA, Fisher YL, et al. Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina. 1996;16:203–13.
Hayashi K, Hasegawa Y, Tokoro T. Indocyanine green angiography of central serous chorioretinopathy. Int Ophthalmol. 1986;9:37–41.
Guyer DR. Digital indocyanine green videoangiography of central serous chorioretinopathy. Arch Ophthalmol. 1994;112:1057.
Sasahara M, Tsujikawa A, Musashi K, Gotoh N, Otani A, Mandai M, et al. Polypoidal choroidal vasculopathy with choroidal vascular hyperpermeability. Am J Ophthalmol. 2006;142:601–7.e1.
Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147:811–5.
Spaide RF, Koizumi H, Pozonni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146:496–500.
Imamura Y, Fujiwara T, Margolis R, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina. 2009;29:1469–73.
Jirarattanasopa P, Ooto S, Nakata I, Tsujikawa A, Yamashiro K, Oishi A, et al. Choroidal thickness, vascular hyperpermeability, and complement factor h in age-related macular degeneration and polypoidal choroidal vasculopathy. Investig Opthalmol Vis Sci. 2012;53:3663.
Koizumi H, Yamagishi T, Yamazaki T, Kinoshita S. Relationship between clinical characteristics of polypoidal choroidal vasculopathy and choroidal vascular hyperpermeability. Am J Ophthalmol. 2013;155:305–13.e1.
Warrow DJ, Hoang QV, Freund KB. Pachychoroid pigment epitheliopathy. Retina. 2013;33:1659–72.
Siedlecki J, Schworm B, Priglinger SG. The pachychoroid disease spectrum—and the need for a uniform classification system. Ophthalmol Retina. 2019;3:1013–5.
Iida T, Hagimura N, Takahashi K, Muraoka K. Study of choroidal vascular lesions in bullous retinal detachment by indocyanine green angiography. J Jpn Ophthalmol Soc. 1995;99:945–54 (in Japanese).
Yanagi Y, Ting DSW, Ng WY, Lee SY, Mathur R, Chan CM, et al. Choroidal vascular hyperpermeability as a predictor of treatment response for polypoidal choroidal vasculopathy. Retina. 2018;38:1509–17.
Miyake M, Tsujikawa A, Yamashiro K, Ooto S, Oishi A, Tamura H, et al. Choroidal neovascularization in eyes with choroidal vascular hyperpermeability. Investig Opthalmology Vis Sci. 2014;55:3223.
Fung AT, Yannuzzi LA, Freund K. Type 1 (sub-retinal pigment epithelial) neovascularization in central serous chorioretinopathy masquerading as neovascular age-related macular degeneration. Retina. 2012;32:1829–37.
Nomura Y, Takahashi H, Tan X, Obata R, Yanagi Y. Widespread choroidal thickening and abnormal midperipheral fundus autofluorescence characterize exudative age-related macular degeneration with choroidal vascular hyperpermeability. Clin Ophthalmol. 2015;9:297–304.
Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015;35:1–9.
Chang Y-C, Cheng C-K. Difference between pachychoroid and nonpachychoroid polypoidal choroidal vasculopathy and their response to anti-vascular endothelial growth factor therapy. Retina. 2019. https://doi.org/10.1097/iae.0000000000002583.
Miyake M, Ooto S, Yamashiro K, Takahashi A, Yoshikawa M, Akagi-Kurashige Y, et al. Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep. 2015;5:16204.
Nakayama M, Keino H, Okada AA, Watanabe T, Taki W, Inoue M, et al. Enhanced depth imaging optical coherence tomography of the choroid in Vogt–Koyanagi–Harada disease. Retina. 2012;32:2061–9.
Spaide RF, Goldbaum M, Wong DWK, Tang KC, Iida T. Serous detachment of the retina. Retina. 2003;23:820–46.
Lee M, Lee H, Kim HC, Chung H. Changes in stromal and luminal areas of the choroid in pachychoroid diseases: insights into the pathophysiology of pachychoroid diseases. Investig Ophthalmol Vis Sci. 2018;59:4896–908.
Dansingani KK, Balaratnasingam C, Naysan J, Freund KB. En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina. 2016;36:499–516.
Baek J, Lee JH, Jung BJ, Kook L, Lee WK. Morphologic features of large choroidal vessel layer: age-related macular degeneration, polypoidal choroidal vasculopathy, and central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:2309–17.
Hiroe T, Kishi S. Dilatation of asymmetric vortex vein in central serous chorioretinopathy. Ophthalmol Retina. 2018;2:152–61.
Matsumoto H, Kishi S, Mukai R, Akiyama H. Remodeling of macular vortex veins in pachychoroid neovasculopathy. Sci Rep. 2019;9:14689.
Mori K. Asymmetry of choroidal venous vascular patterns in the human eye. Ophthalmology. 2004;111:507–12.
Daizumoto E, Mitamura Y, Sano H, Akaiwa K, Niki M, Yamanaka C, et al. Changes of choroidal structure after intravitreal aflibercept therapy for polypoidal choroidal vasculopathy. Br J Ophthalmol. 2017;101:56–61.
Yun C, Huh J, Ahn SM, Lee B, Kim JT, Hwang SY, et al. Choriocapillaris flow features and choroidal vasculature in the fellow eyes of patients with acute central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2019;257:57–70.
Rochepeau C, Kodjikian L, Garcia M-AA, Mathis T. Optical coherence tomography angiography quantitative assessment of choriocapillaris blood flow in central serous chorioretinopathy. Am J Ophthalmol. 2018;194:26–34.
Gal-Or O, Dansingani KK, Sebrow D, Dolz-Marco R, Freund KB. Inner choroidal flow signal attenuation in pachychoroid disease : optical coherence tomography angiography. Retina. 2018;38:1984–92.
Sakurada Y, Fragiotta S, Leong BCS, Parikh R, Hussnain SA, Freund KB. Relationship between choroidal vascular hyperpermeability, choriocapillaris flow density, and choroidal thickness in eyes with pachychoroid pigment epitheliopathy. Retina. 2019. https://doi.org/10.1097/iae.0000000000002635.
Baek J, Kook L, Lee WK. Choriocapillaris flow impairments in association with pachyvessel in early stages of pachychoroid. Sci Rep. 2019;9:5565.
Demirel S, Değirmenci MFK, Batıoğlu F, Özmert E. Evaluation of the choroidal features in pachychoroid spectrum diseases by optical coherence tomography and optical coherence tomography angiography. Eur J Ophthalmol. 2019. https://doi.org/10.1177/1120672119887095.
Nichole J, Mitchell P, Younan C, Burlutsky G, Cheng C, Cheung CMG, et al. Ethnic variation in early age-related macular degeneration lesions between white Australians and Singaporean asians. Investig Ophthalmol Vis Sci. 2014;55:4421–9.
Lee J, Kim M, Lee CS, Kim SS, Koh HJ, Lee SC, et al. Drusen subtypes and choroidal characteristics in asian eyes with typical neovascular age-related macular degeneration. Retina. 2020;40:490–8.
Lee J, Byeon SH. Prevalence and clinical characteristics of pachydrusen in polypoidal choroidal vasculopathy: multimodal image study. Retina. 2019;39:670–8.
Matsumoto H, Mukai R, Morimoto M, Tokui S, Kishi S, Akiyama H. Clinical characteristics of pachydrusen in central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2019;257:1127–32.
Baek J, Lee JH, Chung B, Lee K, Lee WK. Choroidal morphology under pachydrusen. Clin Exp Ophthalmol. 2019;47:498–504.
Spaide RF. Disease expression in nonexudative age-related macular degeneration varies with choroidal thickness. Retina. 2018;38:708–16.
Cheung CMG, Gan A, Yanagi Y, Wong TY, Spaide R. Association between choroidal thickness and drusen subtypes in age-related macular degeneration. Ophthalmol Retina. 2018;2:1196–205.
Singh S, Chakurkar R, Goud A, Rasheed M, Vupparaboina K, Chhablani J. Pachydrusen in polypoidal choroidal vasculopathy in an Indian cohort. Indian J Ophthalmol. 2019;67:1121–6.
Singh SR, Oli A, Mohan S, Goud A, Rasheed MA, Vupparaboina KK, et al. Pachydrusen in Indian population: a hospital-based study. Indian J Ophthalmol. 2019;67:371–5.
Fukuda Y, Sakurada Y, Yoneyama S, Kikushima W, Sugiyama A, Matsubara M, et al. Clinical and genetic characteristics of pachydrusen in patients with exudative age-related macular degeneration. Sci Rep. 2019;9:11906.
Lee J, Choi S, Lee CS, Kim M, Kim SS, Koh HJ, et al. Neovascularization in fellow eye of unilateral neovascular age-related macular degeneration according to different drusen types. Am J Ophthalmol. 2019;208:103–10.
Ersoz MG, Arf S, Hocaoglu M, Sayman Muslubas I, Karacorlu M. Indocyanine green angiography of pachychoroid pigment epitheliopathy. Retina. 2018;38:1668–74.
Ersoz MG, Karacorlu M, Arf S, Hocaoglu M, Sayman Muslubas I. Pachychoroid pigment epitheliopathy in fellow eyes of patients with unilateral central serous chorioretinopathy. Br J Ophthalmol. 2017;102:473–8.
Karacorlu M, Ersoz MG, Arf S, Hocaoglu M, Sayman Muslubas I. Long-term follow-up of pachychoroid pigment epitheliopathy and lesion characteristics. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:2319–26.
Ersoz MG, Karacorlu M, Arf S, Hocaoglu M, Sayman Muslubas I. Outer nuclear layer thinning in pachychoroid pigment epitheliopathy. Retina. 2018;38:957–61.
Lee JH, Kim JY, Jung BJ, Lee WK. Focal disruptions in ellipsoid zone and interdigitation zone on spectral-domain optical coherence tomography in pachychoroid pigment epitheliopathy. Retina. 2019;39:1562–70.
Takahashi A, Ooto S, Yamashiro K, Tamura H, Oishi A, Miyata M, et al. Pachychoroid geographic atrophy. Ophthalmol Retina. 2018;2:295–305.
Yanagi Y, Mohla A, Lee WK, Lee SY, Mathur R, Chan CM, et al. Prevalence and risk factors for nonexudative neovascularization in fellow eyes of patients with unilateral age-related macular degeneration and polypoidal choroidal vasculopathy. Investig Opthalmology Vis Sci. 2017;58:3488–95.
Kim K, Kim JM, Kim DG, Yu S-Y, Kim ES. Five-year follow-up of unaffected fellow eyes in patients with polypoidal choroidal vasculopathy. Ophthalmologica. 2019. https://doi.org/10.1159/000501212.
Baek J, Lee JH, Lee WK. Retinoschisis in eyes with pachychoroid and retinal pigment epithelial atrophy. Graefe’s Arch Clin Exp Ophthalmol. 2019;257:1863–71.
Hariri A, Heussen FM, Nittala MG, Sadda SVR. Optical coherence tomographic correlates of angiographic subtypes of occult choroidal neovascularization. Investig Ophthalmol Vis Sci. 2013;54:8020–6.
Sato T, Kishi S, Watanabe G, Matsumoto H, Mukai R. Tomographic features of branching vascular networks in polypoidal choroidal vasculopathy. Retina. 2007;27:589–94.
Sheth J, Anantharaman G, Chandra S, Sivaprasad S. “Double-layer sign” on spectral domain optical coherence tomography in pachychoroid spectrum disease. Indian J Ophthalmol. 2018;66:1796–801.
Pichi F, Morara M, Veronese C, Ciardella AP. The overlapping spectrum of flat irregular pigment epithelial detachment investigated by optical coherence tomography angiography. Int Ophthalmol. 2018;38:975–83.
Hwang H, Kim JY, Kim KT, Chae JB, Kim DY. Flat irregular pigment epithelium detachment in central serous chorioretinopathy. Retina. 2019. https://doi.org/10.1097/iae.0000000000002662.
Dansingani KK, Balaratnasingam C, Klufas MA, Sarraf D, Freund KB. Optical coherence tomography angiography of shallow irregular pigment epithelial detachments in pachychoroid spectrum disease. Am J Ophthalmol. 2015;160:1243–54.e2.
Carnevali A, Capuano V, Sacconi R, Querques L, Marchese A, Rabiolo A, et al. OCT angiography of treatment-naïve quiescent choroidal neovascularization in pachychoroid neovasculopathy. Ophthalmol Retina. 2017;1:328–32.
Forte R, Coscas F, Serra R, Cabral D, Colantuono D, Souied EH. Long-term follow-up of quiescent choroidal neovascularisation associated with age-related macular degeneration or pachychoroid disease. Br J Ophthalmol. 2019. https://doi.org/10.1136/bjophthalmol-2019-315189.
Terao N, Koizumi H, Kojima K, Yamagishi T, Nagata K, Kitazawa K, et al. Association of upregulated angiogenic cytokines with choroidal abnormalities in chronic central serous chorioretinopathy. Investig Opthalmol Vis Sci. 2018;59:5924–31.
Hata M, Yamashiro K, Ooto S, Oishi A, Tamura H, Miyata M, et al. Intraocular vascular endothelial growth factor levels in pachychoroid neovasculopathy and neovascular age-related macular degeneration. Investig Ophthalmol Vis Sci. 2017;58:292–8.
Terao N, Koizumi H, Kojima K, Yamagishi T, Yamamoto Y, Yoshii K, et al. Distinct aqueous humour cytokine profiles of patients with pachychoroid neovasculopathy and neovascular age-related macular degeneration. Sci Rep. 2018;8:10520.
Azuma K, Tan X, Asano S, Shimizu K, Ogawa A, Inoue T, et al. The association of choroidal structure and its response to anti-VEGF treatment with the short-time outcome in pachychoroid neovasculopathy. PLoS One. 2019;14:e0212055.
Cho HJ, Jung SH, Cho S, Han JO, Park S, Kim JW. Intravitreal anti-vascular endothelial growth factor treatment for pachychoroid neovasculopathy. J Ocul Pharmacol Ther. 2019;35:174–81.
Jung BJ, Kim JY, Lee JH, Baek J, Lee K, Lee WK. Intravitreal aflibercept and ranibizumab for pachychoroid neovasculopathy. Sci Rep. 2019;9:2055.
Matsumoto H, Hiroe T, Morimoto M, Mimura K, Ito A, Akiyama H. Efficacy of treat-and-extend regimen with aflibercept for pachychoroid neovasculopathy and Type 1 neovascular age-related macular degeneration. Jpn J Ophthalmol. 2018;62:144–50.
Roy R, Saurabh K, Shah D, Goel S. Treatment outcomes of pachychoroid neovasculopathy with photodynamic therapy and anti-vascular endothelial growth factor. Indian J Ophthalmol. 2019;67:1678.
Baek J, Lee JH, Jeon S, Lee WK. Choroidal morphology and short-term outcomes of combination photodynamic therapy in polypoidal choroidal vasculopathy. Eye. 2019;33:419–27.
Padrón-Pérez N, Arias L, Rubio M, Lorenzo D, García-Bru P, Català-Mora J, et al. Changes in choroidal thickness after intravitreal injection of anti-vascular endothelial growth factor in pachychoroid neovasculopathy. Investig Ophthalmol Vis Sci. 2018;59:1119–24.
Hara C, Wakabayashi T, Toyama H, Fukushima Y, Sayanagi K, Sato S, et al. Characteristics of patients with neovascular age-related macular degeneration who are non-responders to intravitreal aflibercept. Br J Ophthalmol. 2019;103:623–9.
Cheung CMG, Lai TYY, Ruamviboonsuk P, Chen SJ, Chen Y, Freund KB, et al. Polypoidal choroidal vasculopathy. Ophthalmology. 2018;125:708–24.
Ueta T, Obata R, Inoue Y, Iriyama A, Takahashi H, Yamaguchi T, et al. Background comparison of typical age-related macular degeneration and polypoidal choroidal vasculopathy in Japanese patients. Ophthalmology. 2009;116:2400–6.
Ueta T, Iriyama A, Francis J, Takahashi H, Adachi T, Obata R, et al. Development of typical age-related macular degeneration and polypoidal choroidal vasculopathy in fellow eyes of Japanese patients with exudative age-related macular degeneration. Am J Ophthalmol. 2008;146:96–101.e2.
Chung H, Byeon SH, Freund KB. Focal choroidal excavation and its association with pachychoroid spectrum disorders. Retina. 2017;37:199–221.
Lee JH, Park H-YL, Baek J, Lee WK. Alterations of the lamina cribrosa are associated with peripapillary retinoschisis in glaucoma and pachychoroid spectrum disease. Ophthalmology. 2016;123:2066–76.
Phasukkijwatana N, Freund KB, Dolz-Marco R, Al-Sheikh M, Keane PA, Egan CA, et al. Peripapillary pachychoroid syndrome. Retina. 2018;38:1652–67.
Cheung CMG, Lee WK, Koizumi H, Dansingani K, Lai TYY, Freund KB. Pachychoroid disease. Eye. 2019;33:14–33.
Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. Surv Ophthalmol. 1995;39:367–74.
Ferris FL 3rd, Wilkinson CP, Bird A, Chakravarthy U, Chew E, Csaky K, et al. Clinical classification of age-related macular degeneration. Ophthalmology. 2013;120:844–51.
Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007;144:15–22.e2.
Yoshimura N. Age-related Macular Degeneration in the Japanese. Nihon Ganka Gakkai Zasshi. 2016;120:163–88 (discussion 189, in Japanese).
Takahashi K, Ishibashi T, Ogur Y, Yuzawa M. Classification and diagnostic criteria of age-related macular degeneration. Nihon Ganka Gakkai Zasshi. 2008;112:1076–84 (in Japanese).
Tan CS, Ngo WK, Chen JP, Tan NW, Lim TH. EVEREST study report 2: imaging and grading protocol, and baseline characteristics of a randomised controlled trial of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2015;99:624–8.
Yannuzzi LA, Negrão S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter J, et al. Retinal angiomatous proliferation in age-related macular degeneration. Retina. 2001;21:416–34.
Freund KB, Ho IV, Barbazetto IA, Koizumi H, Laud K, Ferrara D, et al. Type 3 neovascularization: the expanded spectrum of retinal angiomatous proliferation. Retina. 2008;28:201–11.
Wong CW, Yanagi Y, Lee WK, Ogura Y, Yeo I, Wong TY, et al. Age-related macular degeneration and polypoidal choroidal vasculopathy in Asians. Prog Retin Eye Res. 2016;53:107–39.
Hageman G. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch’s membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res. 2001;20:705–32.
Yanagi Y, Foo VHX, Yoshida A. Asian age-related macular degeneration: from basic science research perspective. Eye. 2019;33:34–49.
Yuzawa M. The origins of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2005;89:602–7.
Tanaka K, Mori R, Kawamura A, Nakashizuka H, Wakatsuki Y, Yuzawa M. Comparison of OCT angiography and indocyanine green angiographic findings with subtypes of polypoidal choroidal vasculopathy. Br J Ophthalmol. 2017;101:51–5.
Coscas G, Lupidi M, Coscas F, Benjelloun F, Zerbib J, Dirani A, et al. Toward a specific classification of polypoidal choroidal vasculopathy: idiopathic disease or subtype of age-related macular degeneration. Investig Ophthalmol Vis Sci. 2015;56:3187–95.
Jang JW, Kim JM, Kang SW, Kim SJ, Bae K, Kim KT. Typical polypoidal choroidal vasculopathy and polypoidal choroidal neovascularization. Retina. 2019;39:1995–2003.
Hata M, Tagawa M, Oishi A, Kawashima Y, Nakata I, Akagi-Kurashige Y, et al. Efficacy of photodynamic therapy for polypoidal choroidal vasculopathy associated with and without pachychoroid phenotypes. Ophthalmol Retina. 2019;3:1016–25.
Lee WK, Baek J, Dansingani KK, Lee JH, Freund KB. Choroidal morphology in eyes with polypoidal choroidal vasculopathy and normal or subnormal subfoveal choroidal thickness. Retina. 2016;36:S73–82.
Hosoda Y, Yoshikawa M, Miyake M, Tabara Y, Ahn J, Woo SJ, et al. CFH and VIPR2 as susceptibility loci in choroidal thickness and pachychoroid disease central serous chorioretinopathy. Proc Natl Acad Sci. 2018;115:6261–6.
Lehmann M, Bousquet E, Beydoun T, Behar-Cohen F. Pachychoroid. Retina. 2015;35:10–6.
Hosoda Y, Yamashiro K, Miyake M, Ooto S, Oishi A, Miyata M, et al. Predictive genes for the prognosis of central serous chorioretinopathy. Ophthalmol Retina. 2019;3:985–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Y. Yanagi, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Organizer: Akitaka Tsujikawa, MD
Corresponding Author: Yasuo Yanagi
About this article
Cite this article
Yanagi, Y. Pachychoroid disease: a new perspective on exudative maculopathy. Jpn J Ophthalmol 64, 323–337 (2020). https://doi.org/10.1007/s10384-020-00740-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-020-00740-5