Abstract
Purpose
To determine the clinical features of patients diagnosed with superior segmental optic hypoplasia (SSOH) and to quantitatively compare retinal nerve fiber layer (RNFL) thickness in SSOH eyes, to that in normal subjects.
Study design
Retrospective comparative case series.
Methods
We examined the medical charts of 106 eyes of 59 patients with SSOH and 35 eyes of 35 normal subjects as controls. Forty-four of 59 patients had been examined by spectral-domain optical coherence tomography (SD-OCT). Eyes with SSOH were classified into a definite and a suspect type determined by standard automated perimetry. The definite type had inferior visual field (VF) defects, while the suspect type did not have inferior VF defects. The findings of the SD-OCT images of 35 eyes with SSOH were compared to those of the 35 normal eyes.
Results
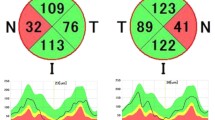
Of the 106 eyes with SSOH, 56 (52.8%) were classified as the definite type and 50 (47.2%) as the suspect type. OCT showed that the average of the total RNFL thickness was significantly thinner in the SSOH group than in the normal group (P < 0.001; Mann-Whitney U test). Sectorial analysis demonstrated that the RNFL was thinner than controls in all quadrants (all P < 0.001; Mann-Whitney U test). The comparison of the hourly sectors showed that the RNFL was thinner at 10, 11, 12, 1, 2, 3, 5, and 6 o’clock sectors in the SSOH group than controls.
Conclusions
Approximately one-half of eyes with SSOH had a detectable VF defect. OCT showed that eyes with SSOH have a thinner RNFL than controls except in 4 o`clock and from 7 o’clock to 9 o’clock.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Superior segmental optic hypoplasia (SSOH) is a congenital anomaly of the optic nerve head with a relative hypoplasia of the superior part of the optic nerve head and the retinal nerve fiber layer. It is characterized by 4 findings: pallor of the superior optic disc, thinning of the superior retinal nerve fiber layer (RNFL) corresponding to the optic disc pallor, superior entrance of the central retinal vessels, and superior peripapillary scleral halo [1,2,3,4,5]. The prevalence of SSOH in Japan and Korea is estimated to be 0.08 to 0.30% [6,7,8]. Yamamoto et al. [6] report that the prevalence of SSOH is 0.3% in the Japanese based on a large-scale screening for eye diseases. This would be equivalent to one-tenth the prevalence of normal tension glaucoma (NTG) in the Japanese [9, 10].
Although most patients with SSOH have an inferior altitudinal or sector-like visual field (VF) defect connected to the blind spot with relatively good best-corrected visual acuity (BCVA), some patients with optic disc satisfying the requirements of SSOH have atypical VF defects. This can lead to a misdiagnosis of SSOH, and it is essential to differentiate patients with SSOH from those with open angle glaucoma (OAG) including NTG. Unoki et al. [11] examined 7 of 10 eyes with SSOH with time-domain optical coherence tomography (TD-OCT), and report that the TD-OCT images revealed mild segmental hypoplasia that had not been previously detected. Thereafter, investigators attempted to differentiate the SSOH from normal subjects [12, 13] as well as from glaucoma patients [14] by TD-OCT.
The introduction of spectral-domain OCT (SD-OCT), an OCT instrument with higher resolution and better imaging speed [15, 16], has made it possible for clinicians to examine the retina and optic disc in greater detail. However, to the best of our knowledge, only a few reports compare the circumpapillary retinal nerve fiber layer (RNFL) thickness of eyes with SSOH to that of normal controls using SD-OCT [17, 18].
The purpose of this study was to classify patients diagnosed with SSOH based on the VF defects determined by standard automated perimetry (SAP) and to assess the RNFL thickness in SSOH quantitatively in the SD-OCT images.
Materials and methods
We examined the medical records of 106 eyes of 59 patients diagnosed with SSOH and 35 eyes of 35 healthy volunteers. All were examined between 2004 and 2015 in the Department of Ophthalmology, Gifu University Hospital, Japan. The procedures used conformed to the tenets of the Declaration of Helsinki, and were approved by the Ethics Committee of Gifu University Graduate School of Medicine.
All patients underwent routine ophthalmological examinations including measurements of the best-corrected visual acuity (BCVA), subjective refraction with a refractometer (KP-8100PA, Topcon), slit-lamp biomicroscopy, intraocular pressure (IOP) measurements with a Goldmann applanation tonometer (Haag-Streit AG), ophthalmoscopy, and optic nerve imaging with a SD-OCT (Carl Zeiss Meditec). If glaucoma or optic nerve hypoplasia was suspected, perimetry with a Humphrey Field Analyzer (Humphrey Instruments) was performed with the central 30-2 Swedish Interactive Threshold Algorithm (SITA) standard program.
We used the same diagnostic criteria of SSOH as those of the Tajimi Health Care Project [6]; a thinning of the optic nerve head rim most prominent in the superior nasal region with corresponding nerve fiber layer defects (NFLD) in the superior nasal region. All eyes diagnosed with SSOH were rated either as definite SSOH type that had inferior visual field (VF) defects, or suspect SSOH type that did not have inferior VF defects. One of the authors (TY) made the diagnosis of all cases.
After the introduction of SD-OCT in our department in 2008, the optic discs were assessed in 44 of 59 patients diagnosed with SSOH by the SD-OCT images (15 patients had not visited our hospital since 2007). Thirty-five eyes of 35 patients with SSOH and 35 age, sex, refractive error-matched normal controls were studied in the same way. The exclusion criteria were: prior intraocular surgery including laser treatment, other ocular diseases, disorders of the central nervous system, decimal BCVA ≤ 0.9, refractive error ≤ -6 diopters or astigmatism ≥ 3 D, and ≤ 18 years. For normal control subjects, one eye of each subject was randomly chosen for assessment. For cases with bilateral SSOH, eye with worse mean deviation (MD) was selected.
The optic disc cube scan images in an area of 6 x 6 mm2 (200 x 200 pixels) were analyzed. Following this, a circumpapillary RNFL thickness map was generated. A 3.46 mm diameter circle consisting of 256 A-scans was then automatically centered around the optic disc. The global, four-quadrants, and 12 hourly circumpapillary thicknesses of the RNFL were determined. The scanned images with signal strength ≥7/10 were used for the analyses, and values obtained from left eyes were converted into the right eye format.
Unpaired t-tests were used to determine the significance of the differences in the demographic data between patients with SSOH and normal subjects. The sex distribution in the two groups was evaluated with the chi-square test. Mann-Whitney U tests were used to compare the data between SSOH and control eyes. A P value of < 0.05 was taken to be statistically significant. For the multiple comparison of OCT sectorial parameters, a Bonferroni-corrected P value < 0.0125 (0.05/4 quadrants) or < 0.0042 (0.05/12 hours) was considered as statistically significant. All the statistical analyses were performed with the SPSS software (IBM SPSS statistics, version 23).
Results
The demographics and clinical findings of the 27 men and 32 women with SSOH are shown in Table 1. The mean age was 35.7 ± 15.7 (mean ± standard deviation) years. The mean IOP was 14.9 ± 3.4 mmHg. The mean refraction error (spherical equivalent) was -3.63 ± 3.38 D. The averaged MD was -2.51 ± 4.00 decibels (dB).
Six of the SSOH cases were diagnosed with open angle glaucoma including normal tension glaucoma. There were 2 cases that had a family history of diabetes mellitus, however both were limited to their mothers and were type I diabetes mellitus [2, 5]. None of the patients had a family history of optic nerve hypoplasia.
Forty-two cases were the definite type in at least one eye, with the remaining 17 cases the suspect type. Of the 42 definite cases, 14 were bilateral, and 20 cases were definite in one eye and suspect in the contralateral eye; the remaining 8 cases were unilateral. Of the 17 suspect cases, 13 were bilateral and 4 were unilateral. Of the 56 eyes judged as the definite type, 14 eyes had the inferior VF defects contiguous to the blind spot. Furthermore, 1 eye had VF defect in both hemi-fields.
The demographics data of 35 eyes with SSOH and 35 eyes of the normal controls are shown in Table 2. Of 44 SSOH patients with SD-OCT image, 9 were excluded because of prior intraocular surgery (1 patient), a worse BCVA (1 patient), a smaller refractive error (5 patient), a larger astigmatism (1 patient), and younger age (1 patient). Among the 35 eyes with SSOH, 22 cases were the definite type and 13 were the suspect type. There were no significant differences in age, sex distribution, refractive error, and MDs between the eyes with SSOH and normal controls. The OCT disc area was significantly smaller in SSOH eyes than in the control group (P = 0.010; Mann-Whitney U test).
The average total RNFL thickness was significantly thinner in the SSOH patients than of the control group (P < 0.001; Mann-Whitney U test; Table 3). The RNFL thickness in all quadrants were significantly thinner in the SSOH eyes than in the normal control eyes (all P <0.001; Mann-Whitney U tests; Table 3). In the hourly analyses, the RNFL was significantly thinner at the 10, 11, 12, 1, 2, 3, 5, and 6 o’clock sectors than in the normal controls (all P < 0.001; Mann-Whitney U tests; Table 3).
Discussion
Our results showed that approximately one-half of the 106 SSOH eyes were the definite type (56 eyes, 52.8%) and one-half the suspect type (50 eyes, 47.2%). Twenty-two of the SSOH cases (37.3%) were only the definite type, 17 cases (28.8%) were only the suspect type, and 20 cases (33.9%) had both types OU. Forty-two cases (71.2%) had definite type in at least one eye. Although none of our cases had reduced BCVA, the severity of the VF defects varied among the definite type of SSOH eyes (Fig. 1).
Disc photographs of representative superior segmental optic hypoplasia (SSOH) cases in the study. Definite SSOH cases: a,b,e,f; Suspect SSOH cases: c,d. a The right eye of 27-year-old woman; b The left eye of 45-year-old woman; c The left eye of 69-year-old man; d The right eye of 44-year-old woman; e The left eye of 64-year-old man; f The right eye of 23-year-old woman. y.o. = years old
Yamamoto et al. [6] estimate that the prevalence of SSOH in the Japanese population was about 0.3%, and approximately two-thirds of the SSOH patients were the definite type. They found 54 eyes of 37 cases with SSOH. Their results show that approximately one-half of the 54 SSOH eyes were the definite type (28 eyes, 51.9%) and one-half the suspect type (26 eyes, 48.1%). Eighteen of the SSOH cases (48.6%) were only the definite type, 14 cases (37.8%) were only the suspect type, and 5 cases (13.5%) had both types in their two eyes. Twenty-three cases (62.2%) had definite type in at least one eye. Although the subjects were from a large-scale eye disease screening study, and the participants’ age was limited to those >40 years [6], the proportion of definite SSOH type is comparable to our findings.
Comparisons of the RNFL thicknesses measured by OCT between eyes with SSOH and normal controls showed a thinning of the superior RNFL sectors, and this thinning may be useful in differentiating cases with SSOH from normal controls [11,12,13, 16, 17]. Unoki et al. [11] report that the RNFL thickness in 7 eyes with SSOH was reduced significantly in only the 12 and 1 o’clock sectors compared to 13 normal eyes as determined by analyzing the TD-OCT images. RNFL thinning, however, is reported to expand into wider areas in SSOH eyes by other subsequent studies using both TD- and SD-OCT instruments. Lee et al. [12] report a decrease in the RNFL thickness in all segments except the 8-9 o’clock sector in eyes with SSOH compared to normal subjects using TD-OCT. Fuse et al. [13] report that, studies using TD-OCT showed that the thinning of the RNFL in eyes with SSOH was present in all sectors except at the 7 to 10 o’clock segments, i.e., the inferotemporal to temporal segments. Hayashi et al. [17] using SD-OCT, report that the RNFL in eyes with SSOH was significantly thinner than that of normal subjects in the superotemporal to nasal region, 41 to 230 degrees. Recently, Han et al. [18] compared the RNFL thickness in 31 SSOH eyes, 33 NTG eyes, and 49 normal eyes using SD-OCT. They also found thinner RNFL in a wider area, e.g., all except at 6 to 9 o’clock segment, in SSOH eyes compared to normal eyes. We showed that not only the superior sectors, i.e., 11-12-1-2 o’clock, but also the 3, 5, and 6 o’clock sectors were thinner. This is in agreement with the results from previous studies [11,12,13, 17, 18]. However, the slight differences among reports might result from the difference in the OCT device used and the SSOH patients studied. There is also a possibility that our SSOH cases may include cases concomitant with nasal or inferior optic hypoplasia. Frisen et al. [19] report that the degree of optic nerve hypoplasia varied considerably ranging from severe to minimal hypoplasia. In fact, they also describe that some cases of optic nerve hypoplasia reveal much less blur of the disc margin than expected from the disc size [19].
There are limitations to this study including the relatively small sample size, a hospital-based cohort, and a cross-sectional study. Because our diagnosis was based on the ocular findings at the initial visit, a future development of glaucoma cannot be ruled out. The incidence of SSOH eyes accompanied by open angle glaucoma was 10.6% (6/59). In Lee et al.’s [20] study it was 19.7%. The estimated incidence of SSOH eyes coexisting in eyes with OAG was nearly 2 to 5 times higher than the prevalence of OAG observed in the Tajimi Health Care Project [9] although our study and that of Lee et al. [20] were not epidemiologic studies.
In conclusion, SD-OCT examinations showed that the RNFL in eyes with SSOH is significantly thinner than that of normal controls except in 4 o`clock and from 7 o`clock to 9 o`clock. Evaluation of the RNFL thicknesses especially the 11, 12, and 1 o’clock segments was useful for differentiating normal from SSOH eyes. Although the hypoplasia in SSOH eyes is generally thought to be non-progressive [21, 22], care should be taken not to overlook coexisting glaucoma and the future development of NTG [23]. Further large-scaled population-based investigations will be required to address this issue because of the variations in the degree of RNFL thickness in SSOH eyes.
References
Kim RY, Hoyt WF, Lessell S, Narahara MH. Superior segmental optic hypoplasia. A sign of maternal diabetes mellitus. Am J Ophthalmol. 1989;107:1312–5.
Landau K, Djahanshahi-Bajka J, Kirchschläger BM. Topless optic disks in children of mothers with type I diabetes mellitus. Am J Ophthalmol. 1998;125:605–11.
Petersen RA, Walton DS. Optic nerve hypoplasia with good visual acuity and visual field defects. Arch Ophthalmol. 1997;95:254–8.
Bjork A, Laurell CG, Laurell U. Bilateral optic nerve hypoplasia with good visual acuity. Am J Ophthalmol. 1978;86:524–9.
Nelson M, Lessell S, Sadun AA. Optic nerve hypoplasia and maternal diabetes mellitus. Arch Neurol. 1986;43:20–5.
Yamamoto T, Sato M, Iwase A. Superior segmental optic hypoplasia found in Tajimi Eye Health Care Project participants. Jpn J Ophthalmol. 2004;48:578–83.
Han SB, Park KH, Kim DM, Kim TW. Prevalence of superior segmental optic nerve hypoplasia in Korea. Jpn J Ophthalmol. 2009;53:225–8.
Seo S, Lee CE, Kim DW, Kim YK, Jeoung JW, Kim CY, et al. Prevalence and risk factors of superior segmental optic hypoplasia in a Korean population: the Korea National Health and Nutrition Examination Survey. BMC Ophthalmol. 2014;14:157.
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S, et al. The prevalence of primary open-angle glaucoma in Japanese. The Tajimi study. Ophthalmology. 2004;111:1641–8.
Shiose Y, Kitazawa Y, Tsukahara S, Akamatsu T, Mizokami K, Katsushima H, et al. Epidemiology of glaucoma in Japan. A nationwide glaucoma survey. Jpn J Ophthalmol. 1991;35:133–55.
Unoki K, Ohba N, Hoyt WF. Optical coherence tomography of superior segmental optic hypoplasia. Br J Ophthalmol. 2002;86:910–4.
Lee HJ, Kee C. Optical coherence tomography and Heidelberg retina tomography for superior segmental optic hypoplasia. Br J Ophthalmol. 2009;93:1468–73.
Fuse N, Aizawa N, Yokoyama Y, Nakamura M, Omodaka K, Sado K, et al. Analysis of retinal fiber layer thickness in superior segmental optic hypoplasia (SSOH). Nippon Ganka Gakkai Zasshi. 2012;116:575–80 (in Japanese).
Yamada M, Ohkubo S, Higashide T, Nitta K, Takeda H, Sugiyama K. Differentiation by imaging superior segmental optic hypoplasia and normal-tension glaucoma with inferior visual field defects only. Jpn J Ophthalmol. 2013;57:25–33.
Wojtkowski M, Bajraszewski T, Targowski P, Kowalczyk A. Real-time in vivo imaging by high-speed spectral optical coherence tomography. Opt Lett. 2003;28:1745–7.
Nassif N, Cense B, Park BH, Yun SH, Chen TC, Bouma BE, et al. In vivo human retinal imaging by ultrahigh-speed spectral domain optical coherence tomography. Opt Lett. 2004;29:480–2.
Hayashi K, Tomidokoro A, Konno S, Mayama C, Aihara M, Araie M. Evaluation of optic nerve head configurations of super segmental optic hypoplasia by spectral-domain optical coherence tomography. Br J Ophthalmol. 2010;94:768–72.
Han JC, Choi DY, Kee C. The different characteristics of cirrus optical coherence tomography between superior segmental optic hypoplasia and normal tension glaucoma with superior retinal nerve fiber defect. J Ophthalmol. 2015;2015:641204.
Frisen L, Holmegaard L. Spectrum of optic nerve hypoplasia. Br J Ophthalmol. 1987;62:7–15.
Lee HJ, Ozaki M, Okano M, Kee C. Coexistence and development of an open-angle glaucoma in eyes with superior segmental optic hypoplasia. J Glaucoma. 2015;24:207–13.
Hayashi K, Tomidokoro A, Aihara M, Tsuji H, Shirato S, Araie M. Long-term follow-up of superior segmental optic hypoplasia. Jpn J Ophthalmol. 2008;52:412–4.
Takagi M, Abe H, Hatase T, Yaoeda K, Miki A, Shirakashi M. Superior segmental optic nerve hypoplasia in youth. Jpn J Ophthalmol. 2008;52:468–74.
Fujimoto N. Differentiation and combination of optic nerve hypoplasia and glaucoma. Neuroophthalmol Jpn. 2007;24:426–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A. Yagasaki, None; A. Sawada, None; Y. Manabe, None; T. Yamamoto, None. The authors have no proprietary or financial interest in any products used in this study.
Additional information
Corresponding author: Ayaka Yagasaki
About this article
Cite this article
Yagasaki, A., Sawada, A., Manabe, Y. et al. Clinical features of superior segmental optic hypoplasia: hospital-based study. Jpn J Ophthalmol 63, 34–39 (2019). https://doi.org/10.1007/s10384-018-0634-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-018-0634-1