Abstract
Purpose
To compare binocular visual function of myopic pseudophakic patients with myopic monovision to patients without monovision.
Study design
Randomized comparative study
Methods
Sixty patients were randomized to one of two groups: patients whose refraction was targeted to -2.75 diopters (D) in the dominant eye and -1.75D in the nondominant eye (myopic monovision group), and patients whose refraction was targeted to -2.75D bilaterally (non-monovision group). Binocular uncorrected and corrected visual acuity at various distances was measured using an all-distance vision tester, and contrast visual acuity and near stereoacuity were examined.
Results
In the myopic monovision group mean refraction was -2.74D in the dominant eyes and -1.94D in the nondominant eyes, and in the non-monovision group it was -2.96D bilaterally. Mean binocular uncorrected distance (UDVA) and intermediate visual acuity (UIVA) from 0.5 m to 5.0 m were significantly better in the myopic monovision group than in the non-monovision group (P≤ 0.0134), while binocular uncorrected near visual acuity (UNVA) at 0.3 m did not differ significantly between groups. The distribution of UIVA and UDVA was significantly better in the myopic monovision group (P≤ 0.0035). Corrected visual acuity at any distance, photopic and mesopic contrast visual acuity, and stereoacuity did not differ significantly between groups.
Conclusion
Patients with myopic monovision exhibited significantly better binocular UIVA and UDVA than those without monovision, while UNVA, corrected visual acuity, contrast sensitivity, and stereoacuity were comparable between groups, suggesting that this method is useful for patients who want to see near and intermediate distances without spectacles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For highly and moderately myopic patients, cataract surgery provides one of the best options to decrease myopia and produce a preferred refraction [1,2,3,4]. Target refraction by implantation of an intraocular lens (IOL) must be appropriate for the lifestyle of individuals receiving a monofocal IOL. A certain percentage of myopic patients prefer to see near distances without spectacles. The refraction of such patients is generally targeted to near or reading distance, equivalent to -2.5 to -3.0 diopters (D) of myopia [5,6,7].
Advances in information technology prompting the widespread use of computers and mobile phones have led to greater requirements for intermediate vision, even for pseudophakic patient. To see both near and intermediate distances without spectacles, we previously suggested an optimal refraction of approximately -2.0D for myopic patients [8]. When the refraction in both eyes was adjusted to -2.0D, however, binocular uncorrected near vision was insufficient. Furthermore, although conventional pseupdophakic monovision with anisometropia of 1.5D or greater provides good near vision, stereopsis deteriorates considerably [9, 10]. To improve near and intermediate vision, we recently began to adjust the refraction of some patients to predominantly near distance in the dominant eye and intermediate distance in the nondominant eye because for these patients near vision is thought to be more important than intermediate vision. Because this method is based on the underlying principle of monovision [9,10,11,12], we termed this method myopic pseuodophakic monovision.
The purpose of the present study was to examine binocular visual function in patients with myopic monovision. To allow for strict assessment of binocular function, patients without monovision whose eyes were adjusted to near distance vision served as controls.
Patients and methods
Patients
This study was a prospective randomized comparative study. A clinical research coordinator began screening all consecutive highly or moderately myopic patients scheduled for bilateral cataract surgery at the Hayashi Eye Hospital on July 22, 2015. Exclusion criteria were eyes with any pathology of the optic nerve, macula, or cornea; severe opaque media other than cataract; eyes scheduled for planned extracapsular cataract extraction; history of previous ocular surgery or inflammation; abnormal ocular position; post full pupil dilation pupillary diameter smaller than 4.5 mm; patient refusal; and any difficulty during examination or follow-up. Screening was continued until April 4, 2016, when 60 patients were recruited. This research adhered to the tenets of the Declaration of Helsinki. The Institutional Review Board/Ethics committee of the Hayashi Eye Hospital, Fukuoka, Japan, approved the study protocol, and all patients provided written informed consent to participate. This study was registered in the University Hospital Medical Information Network (UMIN00013909).
Randomization
All patients were randomly assigned to one of two groups the day before surgery; patients whose refraction was targeted to -2.75D in the dominant eye and -1.75D in the nondominant eye to the myopic monovision group, and those whose refraction was targeted to -2.75D bilaterally to the non-monovision group. Because near vision is considered more important than intermediate vision for patients in the myopic monovision group, we intended to adjust the focal point of their dominant eye to a near distance of approximately 35 cm, and that of the non-dominant eye to an intermediate distance of approximately 60 cm. The dominant eye was determined by the hole-in-card test (sighting dominance) in which the patients were asked to look at a Landolt target at 5 m through a 1-cm hole in the center of a cardboard. The coordinator generated a randomization code with equal numbers using appropriate software, and assigned each patient to one of the two groups according to the randomization code. The group to which each patient was assigned was communicated by the coordinator to a member of the operating room staff who prepared the IOL. The surgeon performing the surgery was not informed to which group the patients were assigned. The coordinator at the Hayashi Eye Hospital collected all the data. The coordinator did not disclose the assignment schedule until all data were collected on August 6, 2016. Neither the patients, examiners, nor data analysts were aware of the group to which the patients were assigned.
IOL power calculation
Preoperative axial length was measured using the IOLMaster 700 (Carl Zeiss Meditech AG, Jena, Germany). Preoperative corneal curvature at the steepest and flattest meridians was measured using an autorefractometer/keratometer (Tonoref® II; Nidek, Gamagori, Japan), and the mean value of these meridians was used for the IOL power calculation. The IOL power was calculated using the SRK/T formula with the optimized A-constants [13]. A single-piece aspheric hydrophobic acrylic IOL was implanted in all eyes (SN60WF; Alcon Laboratories, Fort Worth, TX, USA).
Surgical procedures
A single surgeon (KH) performed all surgery using previously described procedures [14, 15]. First, a continuous curvilinear capsulorrhexis was made using a 25-gauge bent needle. Next, a 2.4-mm clear corneal incision was made using a steel keratome, and phacoemulsification of the nucleus and aspiration of the residual cortex were performed. Without enlarging the incisions, the lens capsule was inflated with 1% sodium hyaluronate (Hyaguard; Nihon Tenganyaku Kenkyusyo, Tokyo, Japan), after which a single-piece hydrophobic acrylic IOL (SN60WF, Alcon) was placed into the capsular bag using the Monarch II injector with a D cartridge (Alcon).
Main outcome measures
All patients underwent examinations at approximately 3 months postoperatively. Binocular uncorrected and distance-corrected decimal VA from far to near distances were measured using an all-distance vision tester (AS-15; Kowa, Tokyo, Japan), as described previously [16]. This device measures equivalent VA on logarithm of the minimum angle of resolution (LogMAR) scale at infinity (∞), and at 5.0-, 3.0-, 2.0-, 1.0-, 0.7-, 0.5-, and 0.3-m distances by placing a spherical lens and variously-sized visual targets at appropriate distances. In this study, we define VA at 1.0-, 0.7-, and 0.5-m distances as intermediate VA, and VA at 0.3 m as near VA.
Binocular uncorrected and distance-corrected VA at high to low contrast levels (contrast VA) and that with a glare source (glare VA) under photopic and mesopic conditions were examined using the Contrast Sensitivity Accurate Tester (CAT-2000; Menicon, Nagoya, Japan) [16]. The CAT-2000 measured the logMAR VA using five contrast percentages of visual targets under photopic and mesopic conditions. Measurement under the photopic lighting condition was made with chart lighting of 100 candelas (cd)/mm2, while chart lighting under the mesopic condition was 2 cd/mm2. A glare source of 200 lux was located in the periphery around the visual axis.
Near stereoacuity at 0.4 m was examined without distance correction using the Titmus stereo test under photopic conditions (80 – 100 cd/m2) [16]. Near stereoacuity was determined by the number of circles for which a patient answered correctly, and the number was converted to seconds of arc for statistical analysis. The stereoacuity of 100 sec.of arc (arc sec) or less is thught to be useful stereoacuity [17].
The objective refraction (spherical and cylindrical powers) and corneal astigmatism were measured using an autorefractometer/keratometer (Tonoref® II; Nidek). The manifest spherical equivalent value (MRSE) was determined as the spherical power plus half the cylindrical power. Experienced ophthalmic technicians who were unaware of the purpose of the study performed all examinations.
Spectacle dependency for distance and near vision, and patient satisfaction for distance, intermediate, and near vision were evaluated by administering a patient questionnaire. The patients were asked if they wore spectacles for either distance or near vision in daily life. If the response was yes, the patients were asked if the spectacles were worn always, occasionally, or only when necessary. Patient satisfaction was classified according to the patient’s response; very satisfied, satisfied, not applicable, or unsatisfied.
Statistical analysis
Data were tested for normality of distribution by inspecting histograms. Because some of the data did not follow a normal distribution, nonparametric tests were used. Binocular uncorrected or corrected logMAR VA from far to near distances, contrast VA and glare VA under photopic and mesopic conditions, near stereoacuity, and other continuous variables were compared between the myopic monovision and non-monovision groups using the Mann-Whitney U test. The ratio of men to women, the incidence of right eye dominance, and other categorical variables were compared between the two groups using the chi-square or Fisher exact test where applicable. Any difference with a P value of less than 0.05 was considered statistically significant.
Results
Because the surgical procedures and perioperative medications were identical between groups and the allocation schedule was kept concealed by a clinical research coordinator and an operating room nurse until the study was completed, the examiners, surgeon, and data analyst were unaware of the group to which the patients were assigned. The patients were unaware of the group to which they had been assigned because the patients in both groups could see near distance with comparable ability.
Of the 60 patients, one in the myopic monovision group was lost to follow-up due to a scheduling conflict, and one in the non-monovision group was hospitalized. Accordingly, 29 patients in each group remained in the analysis. Mean patient age (± standard deviation [SD]) was 64.2 ± 8.5 years (range 50 - 80 years). Baseline characteristics of each group are shown in Table 1. Age, ratio of men to women, incidence of right eye dominance, corneal astigmatism, and pupillary diameter did not differ significantly between groups.
Postoperative refraction
In the myopic monovision group the mean (± SD) MRSE was -2.71 ± 0.61D in the dominant eyes and -1.94 ± 0.44D in the nondominant eyes, and in the non-monovision group it was -2.88 ± 0.52D in the dominant eyes and -2.88 ± 0.49D in the nondominant eyes (Table 1). Mean MRSE in the dominant eyes did not differ significantly between groups, whereas in the nondominant eyes it was significantly greater in the myopic monovision group than in the non-monovision group (P < 0.0001). The difference in the mean absolute MRSE between groups was significantly greater in the myopic monovision group than in the non-monovision group (P < 0.0001).
Binocular VA from far to near distances
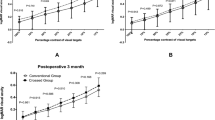
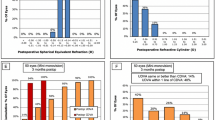
Mean binocular uncorrected distance and intermediate VA (UDVA and UIVA) at distances of ∞, 5.0, 3.0, 1.0, 0.7, and 0.5 m were significantly better in the myopic monovision group than in the non-monovision group (P ≤ 0.0335) (Fig. 1), while mean binocular uncorrected near VA (UNVA) at 0.3 m did not differ significantly between groups (P = 0.6339). Mean binocular distance-corrected VA did not differ significantly between the two groups at any distance (P ≥ 0.1728) (Table 2). The distribution of binocular UIVA at 1.0 m and UDVA at 5.0 m was significantly better in the myopic monovision group than in the non-monovision group (P ≤ 0.0035) (Fig. 2), while that of UNVA at 0.3 m was similar between groups (P ≥ 0.9999).
Binocular contrast VA and glare VA under photopic and mesopic conditions
For uncorrected and distance-corrected contrast VA, mean (± SD) binocular photopic and mesopic contrast VA did not differ significantly between the myopic monovision and non-monovision groups (P ≥ 0.0876) (Fig. 3). For uncorrected and corrected glare VA, mean binocular glare VA under photopic and mesopic conditions did not differ significantly (P ≥ 0.0779), except for glare VA at 25% contrast (P = 0.0184) between groups (Fig. 4).
Near stereoacuity
Mean (± SD) near stereoacuity was 63.6 ± 22.2 arc sec in the myopic monovision group and 54.6 ± 15.0 arc sec in the non-monovision group with no significant difference between groups (P = 0.0856). The number (percentage) of patients who achieved a disparity threshold of 100 arc sec or less was 27 (93.1%) in the myopic monovision group and 29 (100.0%) in the non-monovision group with no significant difference between groups (P = 0.4912).
Spectacle independency, patient satisfaction, and glare and halo symptoms
The number (%) of patients in the myopic monovision group who did not wear spectacles for distance vision was 6 (20.7%) and 3 (10.3%) in the non-monovision group, and 24 (82.8%) in the myopic monovision group did not wear spectacles for near vision, whereas in the non-monovision group there were 26 (89.7%), with no significant difference between groups (P = 0.5827) (Table 3). Patient satisfaction with intermediate vision was significantly better in the myopic monovision group than in the non-monovision group (P = 0.0416) (Table 3), while that for distance or near vision did not differ significantly between groups (P ≥ 0.3857). There was no significant difference between groups in the percentage of patients who reported glare and halo symptoms (P ≥ 0.4463) (Table 3).
Discussion
The present study demonstrates that mean binocular UIVA and UDVA were significantly better in the myopic monovision group than in the non-monovision group, while mean binocular UNVA at 0.3 m did not differ significantly between groups. Additionally, the distribution of binocular UIVA and UDVA was significantly better in the myopic monovision group than in the non-monovision group, while the distribution of binocular UNVA did not differ significantly between groups. Specifically, in the myopic monovision group, mean binocular UIVA at 0.7 m was 0.89, while binocular UDVA at 5.0 m was 0.30. Furthermore, the binocular distance-corrected VA from far to near distances did not differ significantly between groups. These findings suggest that myopic monovision provides excellent intermediate and near vision, as well as useful distance vision without spectacles.
Contrast VA and that with glare under photopic and mesopic conditions were comparable between patients with myopic monovision and patients without monovision. Additionally, stereoacuity did not differ significantly between the myopic monovision and non-monovision groups. The percentage of patients who achieved stereoacuity of 100 arc sec or less, the lowest limit of useful stereoacuity [17], was 93.1% in the myopic monovision group, and did not differ significantly from the non-monovision group. These findings suggest that binocular visual function in eyes with myopic monovision was not impaired compared with that in eyes without monovision.
According to the results of the questionnaire, spectacle dependency for distance and near vision was not significantly different between groups. Patient satisfaction for intermediate vision, however, was significantly better in the myopic monovision group than in the non-monovision group, although that for distance or near vision did not differ significantly between groups. These findings indicate that patients with myopic monovision were aware of the substantial improvement in binocular intermediate vision compared with that of patients without monovision. When producing the spectacles for distance vision for patients with myopic monovision, full distance correction in both eyes may be better because these patients can achieve sufficient intermediate vision.
Preoperatively, the mean refractive and corneal astigmatism as well as MRSE did not differ significantly between the myopic monovision and non-monovision groups. Furthermore, postoperative refractive and corneal astigmatism was not significantly different between the two groups. Thus, because both the preoperative and postoperative refraction, specifically refractive astigmatism, were comparable between groups, the difference in the MRSE and astigmatism between groups did not affect the outcome of the present study.
Intermediate vision work, including computer and smart phone use, has become essential even for pseudophakic patients. For originally myopic patients who want to see near or reading distance without spectacles, it is also necessary to provide for intermediate vision in cataract surgery. To see both near and intermediate distances, we previously suggested that the refraction of myopic patients should be adjusted to approximately -2.0D OU [8]. When we adjusted the bilateral refraction to -2.0D, however, near vision was not sufficient. Furthermore, although conventional pseudophakic monovision with anisometropia of 1.5D or greater provides good near vision, stereopsis deteriorates considerably [9, 10]. To achieve good near and intermediate vision without compromising stereoacuity, we recently began to adjust the focal point of the dominant eye to near distance and that of the nondominant eye to intermediate distance because near vision is thought more important than intermediate vision for these patients. Since this method is based on the principle of monovision [9,10,11,12],
we termed this method “myopic monovision.” The present study is the first to demonstrate that myopic monovision provides excellent binocular near and intermediate vision, and useful distance vision without compromising binocular function.
In conclusion, pseudophakic patients with myopic monovision had significantly better binocular uncorrected VA at far to intermediate distances than patients without monovision, while they had comparable uncorrected near VA and distance-corrected VA at any distance. Particularly, myopic monovision provided excellent intermediate distance vision. Furthermore, binocular visual function, including contrast sensitivity with and without glare, and stereoacuity was similar between patients with and without myopic monovision. These findings suggested that myopic pseudophakic monovision is a useful method for originally myopic patients who want to see both near and intermediate distances after cataract surgery. The optimal degree of anisometropia for myopic monovision remains unclear at present. Further studies are necessary to examine the optimal degree of anisometropia to widen the region of apparent accommodation between the dominant and nondominant eyes.
References
Colin J, Robinet A. Clear lensectomy and implantation of low-power posterior chamber intraocular lens for the correction of high myopia. Ophthalmology. 1994;101:107–12.
Colin J, Robinet A. Clear lensectomy and implantation of a low-power posterior chamber intraocular lens for correction of high myopia: a four-year follow-up. Ophthalmology. 1997;104:73–8.
Jiménez-Alfaro I, Miguélez S, Bueno JL, Puy P. Clear lens extraction and implantation of negative-power posterior chamber intraocular lenses to correct extreme myopia. J Cataract Refract Surg. 1998;24:1310–6.
Güell JL, Rodriguez-Arenas AF, Gris O, Malecaze F, Velasco F. Phacoemulsification of the crystalline lens and implantation of an intraocular lens for the correction of moderate and high myopia: four-year follow-up. J Cataract Refract Surg. 2003;29:34–8.
Kora Y, Yaguchi S, Inatomi M, Ozawa T. Preferred postoperative refraction after cataract surgery for high myopia. J Cataract Refract Surg. 1995;21:35–8.
Pearce JL. Capsular fixated posterior chamber lenses in high myopia. Trans Ophthalmol Soc U K. 1985;104:586–7.
Ochi T, Gon A, Kora Y, Kawai K, Fukado Y. Intraocular lens implantation and high myopia. J Cataract Refract Surg. 1988;14:403–8.
Hayashi K, Hayashi H. Optimum target refraction for highly and moderately myopic patients after monofocal intraocular lens implantation. J Cataract Refract Surg. 2007;33:240–6.
Ito M, Shimizu K, Iida Y, Amano R. Five-year clinical study of patients with pseudophakic monovision. J Cataract Refract Surg. 2012;38:1440–5.
Hayashi K, Ogawa S, Manabe S, Yoshimura K. Binocular visual function of modified pseudophakic monovision. Am J Ophthalmol. 2015;159:232–40.
Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002;28:1439–43.
Finkelman YM, Ng JQ, Barrett GD. Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg. 2009;35:998–1002.
Retzlaff JA, Sanders DR, Kraff MC. Development of the SRK/T intraocular lens power calculation formula. J Cataract Refract Surg. 1990;16:333–40 (Erratum, 1990; 16:528).
Hayashi K, Yoshida M, Yoshimura K. Immediate changes in intraocular pressure after clear corneal micro-incision versus small-incision cataract surgery. Jpn J Ophthalmol. 2014;58:402–8.
Hayashi K, Ogawa S, Yoshida M, Yoshimura K. Wound stability and surgically induced corneal astigmatism after transconjunctival single-plane sclerocorneal incision cataract surgery. Jpn J Ophthalmol. 2017;61:113–23.
Hayashi K, Manabe S, Yoshimura K, Hirata A. Binocular visual function with a diffractive multifocal intraocular lens in patients with unilateral cataract. J Cataract Refract Surg. 2013;39:851–8.
Isomura Y, Awaya S. Studies on aniseikonia and binocular fusion with special reference to stereoacuity. Nippon Ganka Gakkai Zasshi. 1980;84:1619–28 (in Japanese).
Acknowledgements
The authors thank SciTechEdit International (Highlands Ranch, CL, USA) for editorial assistance, and Kozi Yonemoto, PhD (The Biostatistics Center, Kurume University, Kurume, Japan) for statistical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
K. Hayashi, Grant (Alcon Japan, Bayer Yakuhin, Santen Pharmaceutical, Wakamoto Pharmaceutical); M. Yoshida, Grant (Alcon Japan, Bayer Yakuhin, Santen Pharmaceutical, Wakamoto Pharmaceutical); H. Sasaki, Grant (Alcon Japan, Bayer Yakuhin, Santen Pharmaceutical, Wakamoto Pharmaceutical); A. Hirata, Grant (Alcon Japan, Bayer Yakuhin, Santen Pharmaceutical, Wakamoto Pharmaceutical).
About this article
Cite this article
Hayashi, K., Yoshida, M., Sasaki, H. et al. Binocular visual function of myopic pseudophakic monovision. Jpn J Ophthalmol 62, 357–364 (2018). https://doi.org/10.1007/s10384-018-0564-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-018-0564-y