Abstract
Purpose
To determine the characteristics of eyes with late in-the-bag dislocation of an intraocular lens (IOL) after pars plana vitrectomy (PPV).
Methods
Fourteen eyes of 14 patients with a dislocated IOL after PPV were studied retrospectively. The data collected from the medical charts included the age, sex, history of eye diseases, axial length, and interval from PPV to time of IOL dislocation. The surgical procedures used during the PPV were also recorded.
Results
Seven eyes had undergone PPV for rhegmatogenous retinal detachment; 6 eyes, for proliferative diabetic retinopathy; and 1 eye, for retinal vein occlusion. The average interval between the PPV and the diagnosis of the dislocated IOL was 6.2 years (range 2.3–10.1 years). In all eyes, the peripheral vitreous was thoroughly removed with scleral depression during the PPV.
Conclusions
The IOL dislocation was most likely caused by damage to the zonular fibers by the peripheral vitrectomy with scleral depression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Modern surgery for cataracts includes phacoemulsification and aspiration of the crystalline lens and implantation of an intraocular lens (IOL). Recent developments in surgical instruments have allowed these procedures to be performed through very small incisions, and the patient’s discomfort has become minimal. The surgery is performed safely, and the surgical outcome is excellent, with good vision for years after the cataract surgery.
Although cataract surgery has become standardized and safe, some complications can still reduce the vision severely. One of these complications is late-onset dislocation of the IOL, with an incidence of 0.05–3% [1,2,3]. The number of cases with late-onset IOL dislocation requiring surgical retreatment has been reported to increase at 5 years after the cataract surgery [4]. The main reason for the late-onset dislocation of in-the-bag IOL was suggested to be the weakness of the zonular fibers in older persons. On the other hand, early-onset IOL dislocation is usually caused by inadequate IOL fixation onto the capsule during the cataract surgery. With the increase in the aging population, the number of patients requiring surgery for a dislocated IOL will probably increase in the future [4].
Weakened zonules have been reported in eyes with pseudoexfoliation syndrome [5, 6], history of trauma [7], uveitis [8, 9], high myopia with long axial length [10, 11], or retinitis pigmentosa [12].
Dislocation of an IOL has also been observed in eyes with a history of pars plana vitrectomy (PPV) [13, 14]. Information on the dislocated IOL after PPV is limited, probably because the number of these cases is not large. Therefore, the purpose of this study was to investigate the characteristics of patients with in-the-bag dislocated IOL after PPV.
Patients and methods
This was a nonrandomized chart review of 14 eyes of 14 patients with a dislocated in-the-bag IOL who were consecutively treated at the Chiba University Hospital from October 2005 to October 2015. Eyes with ocular trauma and uneventful cataract surgery alone were excluded. Eyes with mild dislocation of the IOL that did not require surgical repair were not included. Eyes were also excluded if the dislocation was due to inadequate fixation on a damaged capsule or interruption of the fixation sutures on the ciliary sulcus.
The procedures used in this study were approved by the institutional review board of Chiba University Graduate School of Medicine, and they conformed to the tenets of the Declaration of Helsinki. Patients signed a consent form for the surgery, which also included permission for the use of the information collected during the examination and surgery for future research studies.
The collected data included the age, sex, laterality, axial length (AL), preoperative best-corrected visual acuity (BCVA), intraocular pressure, interval from prior PPV, and underlying ocular diseases. The information on the prior PPV included the disease that required the PPV, gauge of the instruments for the PPV, surgical times, presence of same-session cataract surgery (phacovitrectomy), and use of photocoagulation, scleral buckling, and intraocular tamponade. The amount of peripheral vitreous removed with scleral depression was estimated based on the description of the operation record. The type of IOL implanted was also recorded. Any complications encountered during surgery were recorded. The BCVA was determined with a Snellen chart, and the decimal values were converted to logarithm of minimal angle of resolution (logMAR) units for the statistical analyses. The refractive error was measured with a TONOREF II auto-refractometer (Nidek, Aichi, Japan), and the AL was measured with an OA-1000 Optical Biometer (Tomey, Aichi, Japan).
Results
Between 2005 and 2015, 53 eyes with dislocated IOL were treated at our hospital. Three eyes had a history of blunt trauma and 30 eyes had a history of uneventful cataract surgery alone with implantation of an intraocular lens. In 6 eyes with prior PPV, the on-the-bag fixed IOL was dislocated. Eventually, 14 eyes with in-the-bag dislocation of the IOL after PPV were studied.
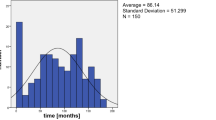
The baseline demographics of the patients are presented in Table 1. The interval between the prior PPV to the IOL dislocation ranged from 2.3 to 10.1 years, with a mean of 6.2 ± 2.2 years. The type of IOL was a single-piece IOL with haptics in 9 eyes and a 3-piece IOL in 3 eyes. None of the eyes had a single-piece IOL without haptics, e.g., plate-type IOL.
Seven eyes had undergone vitrectomy for rhegmatogenous retinal detachment (RRD); 6 eyes, for proliferative diabetic retinopathy (PDR); and 1 eye, for macular edema due to branch retinal vein occlusion (Table 2). Vitrectomy was performed with a 20-gauge system in 9 eyes, a 23-G system in 3 eyes, and a 25-G system in 2 eyes. The peripheral vitreous was extensively removed near the ora serrata with a vitreous cutter and scleral depression in all the patients. The mean surgical time was 140 min, with a range from 90 to 180 min. Phacovitrectomy had been performed in 10 eyes and vitrectomy alone in the other eyes, which were pseudophakic. Retinal photocoagulation was performed in all the eyes, and no scleral buckling was used. Room air was used for intraocular tamponade in 3 eyes; sulfa hexafluoride, in 7 eyes; and silicone oil, in 1 eye. The silicone oil was removed and the retina remained attached. No intraoperative complications were observed.
After dislocation of the IOL was diagnosed, another PPV was performed. In 10 eyes, a new IOL was fixed with transscleral sutures and 2 eyes had a new IOL with intrascleral haptics fixation. The other 2 eyes were highly myopic, with axial lengths of 29.9 and 30.0 mm, and did not have an IOL implant at this time.
Discussion
Our results support the conclusions of a previous study that stated that RRD and PDR were the 2 major pathologies that required PPV for eyes with dislocation of an IOL [14]. As suggested by earlier authors [13, 14], manipulation of the vitrectomy ports and aggressive peripheral vitrectomy with scleral depression may damage the zonules and result in a dislocation of the IOL at a later time.
A total of 5445 PPVs were performed during the study period and included 880 cases of RRD, 1490 cases of PDR, 945 cases of ERM, 686 cases of MH, 289 cases of diabetic macular edema, and 64 cases of vitreomacular traction. In-the-bag dislocation of the IOL was observed after the PPV for only RRD and PDR. The percentage of in-the-bag dislocations of the IOL was 0.26% after any PPV and 0.80% after PPV for RRD and 0.40% after PPV for PDR. Interestingly, no eyes had dislocation after PPV for macular disease including ERM and MH. This suggests that the surgical procedures commonly used during PPV for RRD and PDR but not for ERM and MH played a role in the IOL dislocation. We suggest that peripheral vitrectomy with scleral depression caused damage to the zonules, which then resulted in the dislocation of the IOL.
The main zonular fibers are fixed to the ciliary sulci, which consist of gaps between the ciliary processes at the pars plicata [15]. The posterior part of the main zonular fibers then extends to the pars plana [16]. When a peripheral vitrectomy is performed with scleral depression, the fibers covering the pars plana are likely to be shredded by the vitreous cutter [14]. On the other hand, none of the patients with macular disease underwent extensive peripheral vitrectomy. In general, we remove the peripheral vitreous only partially in macular cases because the peripheral vitreous does not play an important role in the development of macular diseases.
The recent increase in late in-the-bag IOL dislocations is partly explained by the growing number of surgeries for complicated cases that were previously considered unsuitable for surgery [4]. Similarly, late in-the-bag dislocation of the IOL may increase as more PPV are performed for RRD and PDR in the future, especially in older populations.
The interval between prior PPV and dislocation of the IOL was 6.2 years on average. It has been reported that the mean interval between cataract surgery and dislocation of the IOL was 8.04 years [4]. The time for dislocation of the IOL may be shortened by performing PPV, especially in eyes with RRD and PDR.
To treat the dislocated IOL, we performed PPV with removal of the dislocated IOL and implantation of a new IOL with transscleral sutures or intrascleral haptics fixation. The postoperative visual acuity was stable in most cases, but one eye had a decrease in vision because of worsening cystoid macular edema. This patient was diabetic and postoperative inflammation might have caused the recurrence of a preexisting macular edema.
This study has some limitations. Because it was a retrospective study, no control eyes were studied. We found that PPV for RRD and PDR was the treatment of choice in the majority of the cases, but a direct comparison with PPV for other ocular disease such as macular hole (MH) and epiretinal membrane (ERM) was difficult. However, during this 10-year study period, more than 1000 eyes with an implanted IOL underwent vitrectomy for MH or ERM, and none of these eyes had late in-the-bag dislocation of the IOL. This supports the idea that PPV for RRD and PDR is more likely to cause IOL dislocation than is PPV for macular disease. This study was conducted at a single site but several surgeons performed the PPV, which might have caused some bias because the thoroughness of peripheral vitrectomy may depend on the surgeon’s preference.
In conclusion, we studied the characteristics of patients with late in-the-bag IOL dislocation after prior PPV. In eyes with late IOL dislocation, RRD and PDR were the major reasons for the PPV. In these patients, extensive peripheral vitrectomy probably damaged the zonular fibers and resulted in the dislocation of the IOL. The small gauge vitrectomy system may have less damage on the peripheral vitreous and posterior section of the zonular fibers. The technique of peripheral vitrectomy with scleral depression is becoming less common during small gauge vitrectomy. Therefore, a future study is necessary to determine the trend in the incidence and to confirm the pathogenesis of dislocated IOL after PPV.
References
Jakobsson G, Zetterberg M, Lundstrom M, Stenevi U, Grenmark R, Sundelin K. Late dislocation of in-the-bag and out-of-the bag intraocular lenses: ocular and surgical characteristics and time to lens repositioning. J Cataract Refract Surg. 2010;36:1637–44.
Gimbel HV, Condon GP, Kohnen T, Olson RJ, Halkiadakis I. Late in-the-bag intraocular lens dislocation: incidence, prevention, and management. J Cataract Refract Surg. 2005;31:2193–204.
Stark WJ Jr, Maumenee AE, Datiles M, Fagadau W, Baker CC, Worthen D, et al. Intraocular lenses: complications and visual results. Trans Am Ophthalmol Soc. 1983;81:280–309.
Dabrowska-Kloda K, Kloda T, Boudiaf S, Jakobsson G, Stenevi U. Incidence and risk factors of late in-the-bag intraocular lens dislocation: evaluation of 140 eyes between 1992 and 2012. J Cataract Refract Surg. 2015;41:1376–82.
Jehan FS, Mamalis N, Crandall AS. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108:1727–31.
Naumann GO, Schlotzer-Schrehardt U, Kuchle M. Pseudoexfoliation syndrome for the comprehensive ophthalmologist: intraocular and systemic manifestations. Ophthalmology. 1998;105:951–68.
Marin MI, Tejero TR, Dominguez FM, Gutierrez ME. Ocular injuries in midfacial fractures. Orbit. 1998;17:41–6.
Davison JA. Capsule contraction syndrome. J Cataract Refract Surg. 1993;19:582–9.
Gross JG, Kokame GT, Weinberg DV. In-the-bag intraocular lens dislocation. Am J Ophthalmol. 2004;137:630–5.
Fernandez-Buenaga R, Alio JL, Perez-Ardoy AL, Larrosa-Quesada A, Pinilla-Cortes L, Barraquer R, et al. Late in-the-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye. 2013;27:795–801.
Rey A, Jurgens I, Dyrda A, Maseras X, Morilla A. Surgical outcome of late in-the-bag intraocular lens dislocation treated with pars plana vitrectomy. Retina. 2016;36:576–81.
Hayashi K, Hirata A, Hayashi H. Possible predisposing factors for in-the-bag and out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens exchange surgery. Ophthalmology. 2007;114:969–75.
Davis D, Brubaker J, Espandar L, Stringham J, Crandall A, Werner L, et al. Late in-the-bag spontaneous intraocular lens dislocation: evaluation of 86 consecutive cases. Ophthalmology. 2009;116:664–70.
Matsumoto M, Yamada K, Uematsu M, Fujikawa A, Tsuiki E, Kumagami T, et al. Spontaneous dislocation of in-the-bag intraocular lens primarily in cases with prior vitrectomy. Eur J Ophthalmol. 2012;22:363–7.
Rohen JW. Scanning electron microscopic studies of the zonular apparatus in human and monkey eyes. Investig Ophthalmol Vis Sci. 1979;18:133–44.
Hogan MJ. Ciliary body and posterior chamber. In: Hogan M, Alvarado JA, Weddell JE, editors. Histology of the human eye. Philadelphia: WB Saunders Company; 1971. p. 260–319.
Acknowledgements
The authors thank Professor Duco Hamasaki of the Bascom Palmer Eye Institute of the University of Miami for his critical discussion and editing of the final manuscript.
Conflicts of interest
T Koike, None; T. Baba, None; T. Nizawa, None; T. Oshitari, None; S. Yamamoto, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Koike, T., Baba, T., Nizawa, T. et al. Characteristics of patients with spontaneous dislocation of in-the-bag intraocular lens after pars plana vitrectomy. Jpn J Ophthalmol 61, 267–270 (2017). https://doi.org/10.1007/s10384-017-0507-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-017-0507-z