Abstract
Purpose
To evaluate the capability of optical coherence tomography (OCT), retinal nerve fiber layer (RNFL) thickness, and visual field (VF) measurements in glaucoma progression detection.
Methods
The study examined 62 eyes of 37 glaucoma patients observed over a 3-year period. All eyes underwent at least four serial RNFL measurements performed by Cirrus OCT, with the first and last measurements separated by at least 3 years. VF testing was performed by using the Swedish interactive threshold algorithm (SITA) Standard 30-2 program of the Humphrey field analyzer (HFA) on the same day as the RNFL imaging. Both serial RNFL thicknesses and VF progression were assessed by the guided progression analysis (GPA) software program. RNFL thickness progression was evaluated by event analysis. Total deviation (TD) in the superior or inferior hemifield was also examined.
Results
A total of 295 OCT scans and 295 VFs were analyzed. Five eyes exhibited progression by OCT only and 8 eyes exhibited progression by VF GPA only. When the analysis was based on the combined measurement findings, progression was noted in 6 eyes. The average of the progressive hemifield TD at baseline for combined RNFL and VF progression was −3.21 ± 1.38 dB, while it was −2.17 ± 1.14 dB for RNFL progression and −9.12 ± 3.75 dB for VF progression. The average of the progressive hemifield TD indicated a significant advancement of VF progression as compared to RNFL progression (P = 0.002).
Conclusions
When a mild VF defect is present, OCT RNFL thickness measurements are important in helping discern glaucoma progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Glaucoma is a progressive optic neuropathy characterized by a progressive loss of the ganglion cells and retinal nerve fiber layer (RNFL) [1]. It is known that 30 % or more of the retinal ganglion cells (RGCs) are lost before visual field (VF) abnormalities become apparent [2]. Detection of RGC loss is crucial for the early diagnosis of glaucoma and for glaucomatous eye detection. Furthermore, monitoring disease progression is essential in the management of glaucoma patients. During the earliest stages of the disease, structural damage seemingly precedes perimetrically detectable functional loss [2]. However, during the later stages, functional progression is more readily apparent than structural progression [3].
Visual field changes are not easy to identify. The reasons for this include the fact that glaucoma patients exhibit both short- and long-term threshold fluctuations, the changes are more consistent in glaucoma than in healthy eyes, there is a lack of defined criteria for progression, and cataract can influence the general sensitivity threshold [4, 5]. Identification of progressive functional damage to the VF from serial examinations derived by standard automated perimetry (SAP) is based on a variety of subjective clinical criteria [6–10]. In the Early Manifest Glaucoma Trial (EMGT) [9], VF progression was defined as a deterioration that exceeded the 95 % confidence interval for the pattern deviation at three or more locations that were each examined during three consecutive VF tests. This method, referred to as the guided progression analysis (GPA), is now available as commercial software that can be used in conjunction with the Humphrey field analyzer II (Carl Zeiss Meditec, Inc., Dublin, CA, USA).
Thinning of the RNFL is indicative of glaucoma progression, and optical coherence tomography (OCT) can be used to determine changes in the RNFL thickness. In fact, these tests currently serve as one of the primary ways of diagnosing glaucoma [11, 12]. The RNFL progression analysis algorithm, GPA, has recently been incorporated into the software used by the Cirrus HD-OCT device (Carl Zeiss Meditec). By tracking RNFL changes using serial, registered RNFL thickness maps, the GPA is able to compare the RNFL thickness of individual pixels between the baseline and the follow-up images, thereby providing a visual display of the area and the location of significant change.
The purpose of the current study was to evaluate the relationship between the RNFL thickness progression and the VF progression in glaucoma patients.
Patients and methods
Patients
Between October 2008 and September 2012, 62 eyes of 37 glaucoma patients were followed up at Kagawa University Hospital. Each of the eyes underwent at least four serial RNFL measurements, with the first and last measurements separated by at least 3 years. All eligible subjects received a detailed explanation of the study and signed an informed consent form in accordance with the principles embodied in the Declaration of Helsinki. This study was approved by the institutional review board of Kagawa University Hospital. At the baseline examination, all subjects underwent a complete ophthalmic examination that included visual acuity testing with refraction, intraocular pressure, and dilated fundus examination with stereoscopic biomicroscopy of the optic nerve head using slit lamp and indirect ophthalmoscopy. To be included in the study, all subjects had to have a best corrected visual acuity of 20/40 or better, a spherical error within a range between +4.0 and −6.0 D, and a cylinder within ±2.0 D. Exclusion criteria included a history of any kind of retinal pathology, retinal laser procedure, retinal surgery, or neurologic disease. Glaucomatous eyes were defined as eyes exhibiting structural glaucomatous changes (vertical cup-disc asymmetry between fellow eyes of ≥0.2, a cup-disc ratio of ≥0.6, and a neuroretinal rim narrowing, notches, localized pallor, or RNFL defects with glaucomatous VF loss in the corresponding hemifield). A glaucomatous VF was defined as a glaucoma hemifield test (GHT) outside normal limits on at least two consecutive baseline tests and the presence of at least three contiguous test points within the same hemifield on the pattern deviation plot at P < 1 %, with at least one at P < 0.5 % excluding points on the edge of the field or those directly above and below the blind spot. VF testing and RNFL imaging were performed at the same visit.
Cirrus HD-OCT RNFL measurement
The Cirrus HD-OCT uses spectral domain technology. This technique utilizes an optic disc cube that is generated from a 3-dimensional data set composed of 200 A-scans from each of 200 B-scans that cover a 6 mm2 area centered on the optic disc. After creating an RNFL thickness map from the cube, the software automatically determines the center of the disc and then extracts a circumpapillary circle (1.73 mm radius) from the data set. All the images obtained in the current study had signal strengths of at least 6. The RNFL thickness deviation and the RNFL thickness change maps were automatically generated from the OCT instrument and exported to a computer for analysis of the progression pattern of the RNFL defects. The RNFL defects were visualized in the RNFL thickness deviation map, which was composed of 50 × 50 pixels. A pixel was coded in yellow if the RNFL measurement was below the lower 95 % and coded in red if below 99 % of the percentile ranges for that particular pixel.
The RNFL thickness change map is a component of the GPA, which provides both event- and trend-based analysis of the RNFL progression based on the serial RNFL thickness maps. The software automatically aligned and registered the baseline and follow-up OCT images so that the same pixel locations could be measured for change. At least four visits are necessary in order to be able to generate a GPA report. The GPA overlays serial RNFL thickness against the duration of follow-up.
Visual field examination
Standard visual field testing was performed using static automated white-on-white threshold perimetry (Humphrey field analyzer II; Carl Zeiss Meditec), using the 30-2 Swedish interactive threshold algorithm (SITA) standard test. The visual field was defined as reliable only when the fixation losses and the false-positive and false-negative rates were less than 20 %. In all of our analyses, only the reliable test data were used.
The GPA software compared the patient’s baseline visual field to each subsequent visual field determined during the series of follow-up examinations. All baseline values were obtained by averaging the data from the first two exams. The progression evaluation was performed relative to the baseline. The evaluation of the progression was carried out by comparing the threshold modifications to a database of stable glaucoma patients who were tested over a very short period of time. These evaluations took into account the fluctuations related to eccentricity and advancing disease. Each of the consecutive tests examined the same locations (≥3) and determined if there was progression in the consecutive VF tests. As per the findings of a previous study [9], the GPA printouts reported “possible progression” when two locations showed progression and “likely progression” when there were three locations.
Glaucoma clinical severity was assessed based on mean deviation (MD) thresholds from the modified Hodapp–Anderson–Parish classification scheme [13, 14]. Stage 1 through 4 indicate early (mild) (MD >−6.00 dB), moderate (−6.01 to −12.00 dB), advanced (−12.01 to −20.00 dB), and severe (−20.00 dB) glaucoma stage, respectively.
Analysis
The RNFL thickness progression was assessed by event analysis using GPA. The baseline values were obtained by averaging the data from the first two exams. After completing a series of RNFL thickness measurements, the GPA software compares the baseline RNFL thickness value to the final measurement value that was obtained. In the current study, if the RNFL thickness map progression indicated that there was a “likely loss” or “possible loss”, we defined the RNFL thickness as having progressed (Fig. 1).
This study also examined the total deviation (TD) in the superior or inferior hemifield, with the TD evaluated in each hemifield. For example, if there was progression noted in the inferior RNFL thickness, we then evaluated the TD of the superior hemifield.
Statistics
The Levene test was used to assess the equality of variance in the data. All statistical values are presented as mean ± standard deviation (SD), with P values <0.05 considered to be statistically significant. Statistical analyses were performed using SPSS version 19.0 (IBM, New York, USA).
Results
This study analyzed 62 eyes of 37 glaucoma patients. A total of 295 OCT scans and 295 VF tests were performed in the patients and there was a follow-up duration that ranged from 36 to 47 (mean 45.5 ± 3.4) months. Table 1 presents the demographic characteristics for the study patients.
Structure and functional concordance
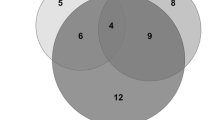
When data from both techniques were used to analyze the patients, progression was found in 6 eyes (Fig. 2). Topographical correspondence between the VF progression and the RNFL progression was present in all 6 eyes. In 2 of the 6 eyes, OCT identified damage before it was detected by HFA. The average of the progressive hemifield TD at baseline was −3.21 ± 1.38 dB (hemifield TD of each eye; −1.97, −2.06, −2.12, −3.46, −4.52, −5.15 dB).
Event analysis of RNFL
The GPA reported that 5 eyes of 4 subjects exhibited progression (Fig. 2). The average of the progressive hemifield TD at baseline was −2.17 ± 1.14 dB (hemifield TD of each eye; −1.12, −1.39, −2.03, −2.27, −4.03 dB).
Event analysis of VF
Visual field GPA showed there was progression in 8 eyes (Fig. 2). The average of the progressive hemifield TD at the baseline was −9.11 ± 3.75 dB (hemifield TD of each eye; −3.67, −6.00, −6.30, −9.15, −9.55, −10.52, −12.39, −15.29 dB), which was significantly more advanced than the progression reported by the OCT GPA (P = 0.002, independent Student’s t-test) The Levene test demonstrated that the assumption of variances was accepted (P = 0.07).
Discussion
Glaucoma can progress structurally and/or functionally. Once glaucoma progression is confirmed, then treatments need to be modified or enhanced to prevent further irreversible loss of visual function. In this study, we evaluated the use of Cirrus HD-OCT GPA for early stage and HFA GPA for moderate and advanced stages of glaucoma progression.
It is recommended that glaucoma be monitored by using both VF and digital imaging devices [15]. However, several studies report finding poor agreement regarding the extent of the progression between the structure- and function-based results [16–18]. Our current data provide additional support for the findings of the latter studies. For example, although we found 6 eyes that exhibited both structural and functional progression, there were 5 that exhibited structural progression and 8 that showed functional progression. All VFs were measured on a logarithmic scale (dB). Since the use of a logarithm scale tends to minimize changes at higher decibels, this can lead to a less apparent change in the VF during the early stages of the disease. A further study reports that detection of glaucoma progression based on the OCT RNFL thickness may not be as effective as VF measurements in cases of moderate and advanced glaucoma [19]. This apparent discrepancy is in agreement with the curvilinear structure–function relationship that has been observed in other cross-sectional studies. These studies report that progression denoted by RNFL thickness was more noticeable than progression by VF during the early stages of glaucoma. Conversely, in cases of advanced glaucoma, the progression found by VF was more noticeable than the progression shown by the RNFL thickness when the VF measurements were expressed on a decibel scale [20–22]. For this reason, it is not surprising that a poor agreement has been observed between the functional and structural tests performed during evaluations of glaucoma progression.
The current study evaluated the TD in the superior and inferior hemifields. Figure 3 shows one example of progression with RNFL thickness without any corresponding VF progression. The mean deviation at baseline was −12.65 dB, and the TD at baseline in the superior and inferior hemifields were −24.18 and −2.03 dB, respectively. The TD of the progressive hemifield, which was indicated by the RNFL GPA, was mild, with a value of −2.03 dB. Since the progression of glaucoma in the superior and inferior hemifields is independent, we decided to evaluate each of the hemifields.
Although detection of glaucoma progression by the OCT RNFL thickness may be more effective than VF measurement in patients with a mild VF defect, our study shows that detection of glaucoma progression by the OCT RNFL thickness may be less effective than the VF measurement in cases of moderate to advanced VF defect. Thus, since the ability to detect progression may depend upon the severity of the VF defect, there may be considerable variability observed between the functional and structural tests.
A previous investigation reports finding a topographical relationship between structural damage to the RNFL thickness and functional damage to the VF [23]. In the current study, we demonstrate that there was a topographical correspondence between the RNFL and VF in all 6 eyes that exhibited both structural and functional progression.
The current study used an event-based approach for analysis of both the functional and structural progression. An important assumption in trend analysis is that the amount of change is linearly proportional to the duration of the follow-up. However, the rate of progression can also vary over time as a consequence of a loosening or tightening of the control of the glaucoma treatment, as well as due to changes in the natural progression of the disease. For this reason, this study assessed the functional and structural progressions using the event analysis of GPA for both the HFA and OCT.
Several studies examined the agreement regarding the extent of the progression between the structure- and function-based results and all of their studies enrolled both eyes [15–17]. Since the glaucoma progression was carried out by GPA software, this decision was independent in each eye. Thus, there might be no correlation between both eyes. For these reasons, we assume that there was no bias due to enrolling both eyes.
The limitations of the present work include a short follow-up period, a small sample size, and a small number of tests. Additionally, we cannot be completely sure of the suitability of the GPA criteria used in the identification of the structural and functional progression. Iester et al. [24] recently reported that the HFA GPA program proved useful in identifying points that were likely to exhibit significant progression and thus needed to be closely observed. Leung et al. [17] also recently showed that the OCT GPA made it possible to detect localized and diffuse loss of the RNFL.
In conclusion, the current study demonstrates that measuring the RNFL thickness with OCT is important for being able to discern glaucoma progression when the VF defect is mild. Based on these results, we suspect that glaucoma progression identified by OCT when the VF defect is mild might reflect the actual progression that occurs prior to the point where conventional methods are able to detect the presence of the disease. Further studies of larger populations over longer periods of time will need to be performed to definitively confirm our hypothesis.
References
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–20.
Quigley HA, Addicks EM, Green WR. Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol. 1982;100:135–46.
Caprioli J. Automated perimetry in glaucoma. Am J Ophthalmol. 1991;111:235–9.
Flammer J, Drance SM, Zulauf M. Differential light threshold. Short- and long-term fluctuation in patients with glaucoma, normal controls, and patients with suspected glaucoma. Arch Ophthalmol. 1984;102:704–6.
Boeglin RJ, Caprioli J, Zulauf M. Long-term fluctuation of the visual field in glaucoma. Am J Ophthalmol. 1992;113:396–400.
The AGIS Investigators. Advanced Glaucoma Intervention Study 2. Visual field test scoring and reliability. Ophthalmology. 1994;101:1445–55.
Katz J. Scoring systems for measuring progression of visual field loss in clinical trials of glaucoma treatment. Ophthalmology. 1999;106:391–5.
Gordon MO, Kass MA. The Ocular Hypertension Treatment Study: design and baseline description of the participants. Arch Ophthalmol. 1999;117:573–83.
Heijl A, Leske MC, Bengtsson B, Bengtsson B, Bengtsson M, Early Manifest Glaucoma Trial Group. Measuring visual field progression in the Early Manifest Glaucoma Trial. Acta Ophthalmol Scand. 2003;81:286–93.
Cho JY, Sung KR, Yun SC, Na JH, Lee Y, Kook MS. Progression detection in different stage of glaucoma: mean deviation versus visual field index. Jpn J Ophthalmol. 2012;56:128–33.
Sung KR, Kim DY, Park SB, Kook MS. Comparison of retinal nerve fiber layer thickness measured by Cirrus HD and Stratus optical coherence tomography. Ophthalmology. 2009;116:1264–70.
Park SB, Sung KR, Kang SY, Kim KR, Kook MS. Comparison of glaucoma diagnostic capabilities of Cirrus HD and Stratus optical coherence tomography. Arch Ophthalmol. 2009;127:1603–9.
Mills RP, Budenz DL, Lee PP, Noecker RJ, Walt JG, Siegartel LR, et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol. 2006;141:24–30.
Spaeth GL, Shieldds MB. The stage of glaucoma. Am J Ophthalmol. 2006;141:147–8.
Consensus statements. In: Weinreb RN, Greve EL, editors. Glaucoma diagnosis structure and function: reports and consensus statements of the 1st Global AIGS meeting on “Structure and function in the management of glaucoma”. The Hague: Kugler; 2004. p. 155–6.
Wollstein G, Schuman JS, Price LL, Aydin A, Stark PC, Hertzmark E, et al. Optical coherence tomography longitudinal evaluation of retinal nerve fiber layer thickness in glaucoma. Arch Ophthalmol. 2005;123:464–70.
Leung CK, Cheung CY, Weinreb RN, Qiu K, Liu S, Li H, et al. Evaluation of retinal nerve fiber layer progression in glaucoma: a study on optical coherence tomography guided progression analysis. Invest Ophthalmol Vis Sci. 2010;51:217–22.
Leung CK, Liu S, Weinreb RN, Lai G, Ye C, Cheung CY, et al. Evaluation of retinal nerve fiber layer progression in glaucoma: a prospective analysis with neuroretinal rim and visual field progression. Ophthalmology. 2011;118:1551–7.
Hood DC, Anderson SC, Wall M, Raza AS, Kardon RH. A test of a linear model of glaucomatous structure–function loss reveals sources of variability in retinal nerve fiber and visual field measurements. Invest Ophthalmol Vis Sci. 2009;50:4254–66.
Leung CK, Medeiros FA, Zangwill LM, Sample PA, Bowd C, Ng D, et al. American Chinese glaucoma imaging study: a comparison of the optic disc and retinal nerve fiber layer in detecting glaucomatous damage. Invest Ophthalmol Vis Sci. 2007;48:2644–52.
Schlottmann PG, De Cilla S, Greenfield DS, Caprioli J, Garway-Heath DF. Relationship between visual field sensitivity and retinal nerve fiber layer thickness as measured by scanning laser polarimetry. Invest Ophthalmol Vis Sci. 2004;45:1823–9.
Leung CK, Chong KK, Chen WM, Yiu CK, Tso MY, Woo J, et al. Comparative study of retinal nerve fiber layer measurement by StratusOCT and GDx VCC, II: structure/function regression analysis in glaucoma. Invest Ophthalmol Vis Sci. 2005;46:3702–11.
Garway-Heath DF, Poinoosawmy D, Fitzke FW, Hitchings RA. Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology. 2000;107:1809–15.
Iester M, Capris E, De Feo F, Polvicino M, Brusini P, Capris P, et al. Agreement to detect glaucomatous visual field progression by using three different methods: a multicentre study. Br J Ophthalmol. 2011;95:1276–83.
Acknowledgments
The authors wish to thank Mr. Kazunori Santo for the statistical analysis of the data.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tenkumo, K., Hirooka, K., Baba, T. et al. Evaluation of relationship between retinal nerve fiber layer thickness progression and visual field progression in patients with glaucoma. Jpn J Ophthalmol 57, 451–456 (2013). https://doi.org/10.1007/s10384-013-0254-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-013-0254-8