Abstract
Purpose
To analyze the influence of oxidative stress on retinal ganglion cells (RGCs) by using a selective culture system of rat RGCs.
Methods
Rat RGCs were purified by a two-step immunopanning procedure and cultured either with or without antioxidant (AO) compounds. Reactive oxygen species (ROS) in RGCs were analyzed using dihydroethidium. Expression of angiotensin II, cleaved caspase 3, and netrin-1 was analyzed by immunocytochemistry. Live RGCs were detected by use of calcein-acetoxymethyl ester. The roles of angiotensin II type 1 receptor (AT1R) signaling and netrin-1 were analyzed by use of an AT1R blocker (telmisartan) and an anti-netrin-1 neutralizing antibody, respectively.
Results
ROS and angiotensin II were induced in RGCs cultured without AO compounds (AO−). In these cultures, the number of live RGCs decreased and expression of cleaved and activated caspase 3 increased, but these changes were attenuated by addition of the AT1R blocker. Reduction in netrin-1 expression under the AO− condition was also prevented by the AT1R blocker. The AT1R blocker’s effects on RGC survival and reduction in cleaved caspase 3-positive cells were cancelled by the anti-netrin-1 neutralizing antibody.
Conclusions
Oxidative stress induced cell death through AT1R signaling and netrin-1 reduction in cultured RGCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive oxidative stress induces cellular dysfunction and precocious cell death, which can contribute to the pathogenesis of ocular diseases and visual dysfunction [1]. We have reported that the death of retinal ganglion cells (RGCs) is accelerated in superoxide dismutase-1 knockout mice, in response to excessive accumulation of reactive oxygen species (ROS) [2]. This vulnerability of the RGCs would contribute to the pathogenesis of glaucomatous optic neuropathy [2, 3]. However, the mechanism underlying excessive ROS-induced RGC death is not fully understood. Here, we analyzed this mechanism by using a selective culture system of rat RGCs.
It has been shown that an angiotensin II type 1 receptor (AT1R) blocker (ARB), candesartan, inhibits the decrease in RGCs in a rat glaucoma model induced by cauterization of 3 episcleral vessels and subsequent chronic elevation of intraocular pressure (IOP) [4]. This protective effect was obtained without reducing the IOP, suggesting that the ARB had a neuroprotective effect on RGCs. In addition, clinical data show a suppressive effect of angiotensin-converting enzyme (ACE) on the progression of visual field defects in normal tension glaucoma [5], supporting the idea that the renin–angiotensin system (RAS) is involved in the molecular mechanism of RGC impairment. Genetic data from glaucoma patients are consistent with these findings: glaucoma is reported to be associated with polymorphisms of an angiotensin receptor [6] and ACE [7]. Moreover, RAS is closely related to ROS levels in some disease conditions, for example diabetes [8, 9], further indicating its possible involvement in the mechanism of ROS-induced RGC impairment and death.
Neuronal development and survival are supported by neurotrophic factors. One such factor, netrin-1, was first reported as a diffusible attractant for axon guidance, and was later shown to be required for formation of the optic nerve head and optic chiasm [10]. It regulates cell migration by binding to its receptor, DCC (deleted in colorectal cancer) [11]. RGCs express both netrin-1 and its receptor [12].
Recent reports reveal that netrin-1 is also involved in angiogenesis [13, 14]. Netrin-1 is upregulated in the retina of oxygen-induced retinopathy models, and it induces neovascularization [15]. It also acts as an anti-apoptotic factor [16–18]. Neuronal death in the neural tube is increased in netrin-1 knockout mice, and this neuronal death is inhibited by adding netrin-1 to the primary culture [17]. Netrin-1 also has a neuroprotective function in mouse brain ischemia [19].
In this study, we analyzed the mechanism of oxidative stress-induced neuronal cell death, focusing on RAS and netrin-1, using a selective RGC culture.
Materials and methods
Animals
Six to eight-day-old Wistar rats were purchased from Saitama Laboratory Animal Supply (Saitama, Japan). All the animal experiments were conducted with approval from the Animal Care and Use Committee of Keio University and under the guidelines of the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Purification and culture of rat RGCs
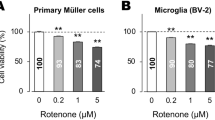
RGCs were purified by a two-step immunopanning procedure, as described elsewhere [20, 21]. Briefly, the retinal cells from Wister rats were dissociated by papain using a cell-dissection kit (Worthington Biochemical, Lakewood, NJ, USA). The dissociated retinal cells were then incubated in flasks (Nunc, Roskilde, Denmark) coated with an anti-rat macrophage monoclonal antibody (1:50, OX-41; Chemicon, Temecula, CA, USA) to exclude macrophages, and then incubated in tubes (Corning, Acton, MA, USA) coated with an anti-rat Thy1.1 monoclonal antibody (1:300, OX-7; Chemicon). RGCs that adhered to the tubes were collected by centrifugation at 60 × g for 5 min and seeded on 13-mm glass coverslips that had been coated with 50 μg/ml poly-l-lysine (Sigma, St Louis, MO, USA) and 1 μg/ml laminin (Invitrogen, Carlsbad, CA, USA) in a 24-well plate. Purified RGCs were plated at a density of 1,000 cells per well. The RGCs were cultured under basal conditions in serum-free B27 complete medium containing B27 supplement (Invitrogen) which includes vitamin E, vitamin E acetate, superoxide dismutase, catalase, and glutathione as antioxidants, together with neurobasal medium (Invitrogen) containing 1 mM l-glutamine (Sigma), 40 ng/ml human recombinant brain-derived neurotrophic factor (Sigma), 40 ng/ml rat recombinant ciliary neurotrophic factor, 10 μM forskolin (Sigma), 100 U/ml penicillin, and 100 μg/ml streptomycin, with a humidified atmosphere of 5 % CO2 and 95 % air at 37 °C for 3 days. The RGCs were then further cultured with the medium containing either B27 supplement or B-27 supplement minus antioxidants (AO−) (Invitrogen), together with all the additional reagents described above, and evaluated. Cell viability was determined by use of a fluorescent viability agent, calcein-acetoxymethyl ester (calcein-AM; 1 mM; Invitrogen). An AT1R blocker, telmisartan (a gift from Boehringer Ingelheim, Germany), was added at 5 μM, or a neutralizing antibody against netrin-1 (AF1109; R&D Systems, Minneapolis, MN, USA) was added at 20 μM, after optimizing the concentration for the best cell survival or death, respectively. Survival of RGCs using telmisartan at 10 μM, the concentration which has a neuroprotective effect on a neuronal cell line, PC12D, as we previously showed [22], was equal to that at 5 μM (results not shown), so subsequent experiments were performed at 5 μM. Vehicle was added to some wells as a control. Each experiment was performed using triplicate samples from each group, and repeated 3 times.
Measurement of ROS
Live cells were dyed with dihydroethidium (DHE; Invitrogen-Molecular Probes, Eugene, OR, USA) for 5 min at 37 °C as described elsewhere [23]. The cells were examined with a laser-scanning confocal microscope (LSM510, Carl Zeiss, Germany) and the intensity of the staining was measured by use of ImageJ software.
Immunohistochemistry
Live cells were dyed with calcein-acetoxymethyl ester, then fixed with paraformaldehyde. After being incubated at room temperature with blocking reagent for 1 h, the cells were incubated at 4 °C overnight with rabbit antibodies against angiotensin I/II (1:200, H-300; Santa Cruz Biotechnology, Santa Cruz, CA, USA), cleaved caspase 3 (1:600; 9664; Cell Signaling Technology, Danvers, MA, USA), or netrin-1 (1:600, Ab-1; Calbiochem, Darmstadt, Germany). They were then incubated for 30 min with biotin-conjugated goat anti-rabbit IgG at room temperature for 1 h, and reagents prepared to form the avidin–biotin–peroxidase complex (Vector, Southfield, MI, USA). Finally, the immunoreactions were detected with a tyramide signal amplification (TSA) fluorescein system (Perkin Elmer Life Science, San Diego, CA, USA). Nuclei were stained with the nuclear dye bisbenzimide (Hoechst 33258) diluted 1:1000 from a 10-mg/ml stock solution (Sigma). Samples were examined with a laser-scanning confocal microscope (LSM510; Carl Zeiss, Berlin, Germany).
Statistical analysis
All the results shown in graphs are expressed as mean ± SD. The values were analyzed by one-way ANOVA with Tukey’s post-hoc test or Student’s t test, and differences were considered statistically significant at P < 0.05.
Results
Induction of ROS and angiotensin II in RGCs in the absence of antioxidants
After being cultured under basal conditions for 3 days, RGCs were further cultured for 1 h either in medium lacking anti-oxidants (AO− RGCs) or under control conditions (AO+ RGCs). Although the DHE staining could barely be detected in the AO+ RGC cultures, the ROS detected by DHE staining were clearly upregulated (Fig. 1a–c) in the AO− RGC cultures. At the same time, slight immunoreactivity of angiotensin II was observed in the AO+ RGC cultures (Fig. 1d), but in the AO− RGCs it was clearly visible throughout the cell bodies and neurites (Fig. 1e).
Induction of ROS and angiotensin II in the RGCs in the absence of antioxidants. a–c DHE staining and d, e immunohistochemistry of angiotensin II after 1 h of either AO+ or AO− culture following 3 days of basal conditioning culture. a, b ROS levels detected by DHE and c measured using ImageJ software were upregulated, and d, e angiotensin II was induced in the RGCs in the absence of antioxidant compounds. a, d AO+ and b, e AO− conditions. RGCs retinal ganglion cells, AO antioxidants
Suppression of oxidative stress-induced RGC death by an AT1R blocker
After being cultured under basal conditions for 3 days, RGCs were cultured for 24 h either with or without AO, and the live cells were dyed with a fluorescent viability agent, calcein-acetoxymethyl ester, and counted (Fig. 2a). The dyed cell bodies and neurites were both clearly visible in the live cells. The number of the surviving AO− RGCs decreased at a higher rate than the AO+ RGCs (Fig. 2b, d). However, this decrease was attenuated by addition of an AT1R blocker, telmisartan, to the AO− culture medium (Fig. 2c, d).
Suppression of oxidative stress-induced RGC death by an AT1R blocker. a–c Live and surviving RGCs detected by calcein-acetoxymethyl ester after 24 h of culture b in the absence of AO a were decreased compared with culture under AO+ condition. c The number of live RGCs under the AO− condition was increased by adding an AT1R blocker (telmisartan) to the culture medium. d The live RGCs were counted. Bar graph values are relative to those of AO+ RGCs. Values are mean ± SD. *p < 0.05. RGCs retinal ganglion cells, AO antioxidants, AT1R angiotensin II type 1 receptor
Suppression of oxidative stress-induced caspase-3 activation by the AT1R blocker
After being cultured under basal condition for 3 days, the RGCs were cultured for 3 h either with or without AO, then immunostained for cleaving and activating caspase 3. The staining of the cleaved caspase 3 was stronger and filled more of the cytoplasmic space, including the neurites, in the AO− RGCs than in the AO+ RGCs. This caspase 3 activation was also suppressed by the AT1R blocker, telmisartan (Fig. 3a). To quantify this observation, the cleaved caspase 3-positive cells in which the caspase 3 activation had spread to the neurites were counted. The proportion of live cells that was positive for the cleaved caspase 3 increased in the AO− condition, and this increase was suppressed by the AT1R blocker (Fig. 3b).
Suppression of the oxidative stress-induced caspase-3 activation by the AT1R blocker. a, b Caspase 3 activation was more highly induced in RGCs selectively cultured for 3 h in the absence of AO than in RGCs cultured under the AO+ condition; this activation was suppressed by the AT1R blocker, telmisartan. a Immunohistochemistry of cleaved caspase 3, shown in pink; live cells, green; Hoechst nuclear staining, white. Arrowheads in b, cleaved caspase 3 expression. b Proportion of live cells that was cleaved caspase 3-positive. Values are mean ± SD. *p < 0.05. RGCs retinal ganglion cells, AO antioxidants, AT1R angiotensin II type 1 receptor, cl. caspase 3 cleaved caspase 3
Oxidative stress-induced decrease in netrin-1 expression, and prevention of this decrease by the AT1R blocker
Next, we analyzed the netrin-1 expression in the RGCs cultured for 3 h under oxidative stress subsequent to the basal condition culture for 3 days (Fig. 4a). In the AO+ RGCs, netrin-1 was observed in the cell bodies and neurites. In contrast, less netrin-1 staining that was particularly missing from the neurites was observed for the AO− RGCs. However, after treatment of the AO− RGCs with the AT1R blocker, netrin-1 became clearly expressed in the neurites. The reduction in the proportion of live cells that expressed netrin-1 under the AO− conditions was prevented in those cultures incubated with the AT1R blocker (Fig. 4b).
Reduction of netrin-1 expression induced by oxidative stress and its prevention by the AT1R blocker. a, b Netrin-1 expressed in the cell bodies and neurites of RGCs cultured under AO+ condition was reduced under the AO− condition. However, the AT1R blocker, telmisartan, suppressed this decrease. a Immunohistochemistry of netrin-1. b Netrin-1-positive cells among live cells. Values are mean ± SD. *p < 0.05. RGCs retinal ganglion cells, AO antioxidants, AT1R angiotensin II type 1 receptor
Involvement of netrin-1 in the neuroprotective effect of the AT1R blocker
We further analyzed the involvement of netrin-1 in the neuroprotective action of the AT1R blocker, by inhibiting netrin-1 in the presence of the AT1R blocker under the AO− condition. The number of surviving cells in the culture was reduced 24 h after addition of anti-netrin-1 subsequent to the basal condition culture (Fig. 5a). Moreover, the proportion of live cells that expressed cleaved caspase 3 was increased 3 h after adding the anti-netrin-1 (Fig. 5b).
Involvement of netrin-1 in the neuroprotective effect of the AT1R blocker. a Inhibiting netrin-1 cancelled the effect of the AT1R blocker, and so promoted RGC survival and b inhibited caspase 3 activation under the AO− condition. a Bar graph values are relative to those of AO− RGCs cultured with the AT1R blocker. b Proportion of live cells that was cleaved caspase 3-positive. Values are mean ± SD. *p < 0.05. RGCs retinal ganglion cells, AO antioxidants, AT1R angiotensin II type 1 receptor, cl. caspase 3 cleaved caspase 3
Discussion
We demonstrated that ROS and angiotensin II were produced in the RGCs in the absence of antioxidants (Fig. 1), which led to RGC death through AT1R signaling (Figs. 2, 3). Oxidative stress reduced the level of the anti-apoptotic factor netrin-1 in the RGCs (Fig. 4), and inhibition of netrin-1 cancelled the neuroprotective effect of the AT1R blockade (Fig. 5). Thus, the oxidative stress-induced RGC death was mediated by AT1R signaling, at least in part through a decrease in the netrin-1 signal.
The components of RAS, such as pro-renin (a precursor of renin), angiotensinogen, and ACE, are expressed in the retina, which is composed of six types of neuron and one type of glial cell [24]. This local induction system is called tissue RAS, and is regulated separately from systemic RAS. Because most of the RAS components are secreted from cells and diffusible, several kinds of retinal cell could be involved in angiotensin II induction in the retina. However, interestingly, we observed that the angiotensin II signal was induced in a selective culture of RGCs. Moreover, because caspase 3 was activated downstream of AT1R signaling in the RGCs within 3 h, the angiotensin II induction by ROS may be promoted by protein modification rather than by gene expression. Because angiotensin II is induced by several steps of the enzymatic pathway, it is natural to deduce that all the RAS component proteins are present under the control conditions and ready to produce angiotensin II rapidly in response to stress, although the protein levels were not practically measurable because of the small number of RGCs available in this primary selective culture. Furthermore, the RAS was active in the selective RGC culture, suggesting that it exerted its effect on the RGCs in an autocrine and/or paracrine manner. This is consistent with our previous finding that AT1R is expressed in RGCs [25]. RGCs could be vulnerable to oxidative stress because of this accessibility to the RAS.
Glaucomatous optic neuropathy is related to oxidative stress which may be caused by several pathways. Whatever the direct cause of ROS is, it may cause tissue RAS activation, and there would be a possibility of avoiding the effect of accumulated ROS in RGCs of glaucomatous optic neuropathy by AT1R blockers.
Another disease that involves oxidative stress in its pathogenesis is diabetes. We have reported that AT1R signaling causes pathological changes in neurons; it affects synapses that are abundant in the inner retinal layer, through ERK activation [9, 22]. AT1R signaling promotes degradation of the synaptic protein, synaptophysin, through the ubiquitin proteasome system. A similar phenomenon is caused by ROS [9, 23]; ROS inhibition suppresses ERK activation and synaptophysin reduction. ROS can be induced by AT1R signaling through NADPH oxidase, as reported for the diabetic retina [8], and now we have shown that tissue RAS is induced by ROS. Taken together, these findings suggest that RAS and ROS engage in cross-talk, and that their cross-talk worsens the condition of the diseased retina via a positive feedback mechanism. In the presence of this cross-talk, the disease may progress rapidly; however, the disease might be treated by suppressing one of these factors. Therefore, tissue RAS suppression may be an effective therapy against ROS-induced pathogenesis, and this therapy could be performed in addition to the definitive therapy.
Netrin-1 and one of its receptors, DCC, are both expressed in RGCs [12], suggesting that netrin-1’s protective effect in RGCs may be elicited through its binding to DCC. DCC is known as a “dependence receptor”, a type of receptor that is pro-apoptotic when its ligand is absent [26–28]. Dependence receptors involve p75NTR, TrkC, neogenin, and RET. The absence of ligand results in the caspase-mediated cleavage of these receptors, which releases proapoptotic peptides [28]. The loss of receptor function by caspase-induced cleavage also leads to a shutdown of their ligand-induced survival signals and promotes apoptotic cell death [28]. The cultured RGCs showed cleaved caspase 3 in their neurites, suggesting that a vicious cycle of caspase 3 activation and cleavage of the dependence receptor might be involved in the death signal of oxidative stress-induced RAS.
A paradoxical phenotype is, however, observed for DCC-knockout mice [29]—apoptosis of RGCs is increased. For mice expressing DCC with a mutation in the P3 domain, which is required for its netrin-1-mediated function, the increase in apoptosis is also observed. These results show that the netrin-1 signal itself may also be required for cell survival.
The mechanism by which RAS suppresses netrin-1 expression is currently unknown, but it is interesting that netrin-1’s organ-protective role is also observed in the kidney [30], in which RAS plays a major pathogenic role. Netrin-1 deficiency enhances and netrin-1 overexpression inhibits the acute kidney injury caused by transient ischemia. In this model, renal angiotensin II, and oxidative stress, increases and causes kidney injury as a result of apoptosis of the renal tubular epithelial cells. Further studies to reveal the molecular mechanisms underlying these events are expected.
In summary, we show that oxidative stress-induced RGC death involves the autocrine and/or paracrine pathway of AT1R signaling and causes a decrease in the survival factor, netrin-1. The use of AT1R blockade to relieve the vulnerability of RGCs to oxidative stress may lead to a new therapeutic approach.
References
Ozawa Y, Sasaki M, Takahashi N, Kamoshita M, Miyake S, Tsubota K. Neuroprotective effects of lutein in the retina. Curr Pharm Des. 2012;18:51–6.
Yuki K, Ozawa Y, Yoshida T, Kurihara T, Hirasawa M, Ozeki N, et al. Retinal ganglion cell loss in superoxide dismutase 1 deficiency. Invest Ophthalmol Vis Sci. 2011;52:4143–50.
Yuki K, Murat D, Kimura I, Ohtake Y, Tsubota K. Reduced-serum vitamin C and increased uric acid levels in normal-tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 2010;248:243–8.
Yang H, Hirooka K, Fukuda K, Shiraga F. Neuroprotective effects of angiotensin II type 1 receptor blocker in a rat model of chronic glaucoma. Invest Ophthalmol Vis Sci. 2009;50:5800–4.
Hirooka K, Baba T, Fujimura T, Shiraga F. Prevention of visual field defect progression with angiotensin-converting enzyme inhibitor in eyes with normal-tension glaucoma. Am J Ophthalmol. 2006;142:523–5.
Hashizume K, Mashima Y, Fumayama T, Ohtake Y, Kimura I, Yoshida K, et al. Genetic polymorphisms in the angiotensin II receptor gene and their association with open-angle glaucoma in a Japanese population. Invest Ophthalmol Vis Sci. 2005;46:1993–2001.
Ozkur M, Erbagci I, Gungor K, Nacak M, Aynacioglu S, Bekir NA. Angiotensin-converting enzyme insertion–deletion polymorphism in primary open-angle glaucoma. Ophthalmologica. 2004;218:415–8.
Chen P, Guo AM, Edwards PA, Trick G, Scicli AG. Role of NADPH oxidase and ANG II in diabetes-induced retinal leukostasis. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1619–29.
Ozawa Y, Kurihara T, Sasaki M, Ban N, Yuki K, Kubota S, et al. Neural degeneration in the retina of the streptozotocin-induced type 1 diabetes model. Exp Diabetes Res. 2011;108328.
Inatani M. Molecular mechanisms of optic axon guidance. Naturwissenschaften. 2005;92:549–61.
Chan SS, Zheng H, Su MW, Wilk R, Killeen MT, Hedgecock EM, et al. UNC-40, a C. elegans homolog of DCC (deleted in colorectal cancer), is required in motile cells responding to UNC-6 netrin cues. Cell. 1996;87:187–95.
Deiner MS, Kennedy TE, Fazeli A, Serafini T, Tessier-Lavigne M, Sretavan DW. Netrin-1 and DCC mediate axon guidance locally at the optic disc: loss of function leads to optic nerve hypoplasia. Neuron. 1997;19:575–89.
Park KW, Crouse D, Lee M, Karnik SK, Sorensen LK, Murphy KJ, et al. The axonal attractant netrin-1 is an angiogenic factor. Proc Natl Acad Sci. 2004;101:16210–5.
Wilson BD, Ii M, Park KW, Suli A, Sorensen LK, Larrieu-Lahargue F, et al. Netrins promote developmental and therapeutic angiogenesis. Science. 2006;313:640–4.
Xu H, Liu J, Xiong S, Le YZ, Xia X. Suppression of retinal neovascularization by lentivirus-mediated netrin-1 small hairpin RNA. Ophthalmic Res. 2011;47:163–9.
Arakawa H. Netrin-1 and its receptors in tumorigenesis. Nat Rev Cancer. 2004;4:978–87.
Furne C, Rama N, Corset V, Chedotal A, Mehlen P. Netrin-1 is a survival factor during commissural neuron navigation. Proc Natl Acad Sci. 2008;105:14465–70.
Tang X, Jang SW, Okada M, Chan CB, Feng Y, Liu Y, et al. Netrin-1 mediates neuronal survival through PIKE-L interaction with the dependence receptor UNC5B. Nat Cell Biol. 2008;10:698–706.
Wu TW, Li WW, Li H. Netrin-1 attenuates ischemic stroke-induced apoptosis. Neuroscience. 2008;156:475–82.
Nakayama M, Aihara M, Chen YN, Araie M, Tomita-Yokotani K, Iwashina T. Neuroprotective effects of flavonoids on hypoxia-, glutamate-, and oxidative stress-induced retinal ganglion cell death. Mol Vis. 2011;17:1784–93.
Uchida S, Suzuki Y, Araie M, Kashiwagi K, Otori Y, Sakuragawa N. Factors secreted by human amniotic epithelial cells promote the survival of rat retinal ganglion cells. Neurosci Lett. 2003;341:1–4.
Kurihara T, Ozawa Y, Nagai N, Shinoda K, Noda K, Imamura Y, et al. Angiotensin II type 1 receptor signaling contributes to synaptophysin degradation and neuronal dysfunction in the diabetic retina. Diabetes. 2008;57:2191–8.
Sasaki M, Ozawa Y, Kurihara T, Kubota S, Yuki K, Noda K, et al. Neurodegenerative influence of oxidative stress in the retina of a murine model of diabetes. Diabetologia. 2010;53:971–9.
Wilkinson-Berka JL. Angiotensin and diabetic retinopathy. Int J Biochem Cell Biol. 2006;38:752–65.
Kurihara T, Ozawa Y, Shinoda K, Nagai N, Inoue M, Oike Y, et al. Neuroprotective effects of angiotensin II type 1 receptor (AT1R) blocker, telmisartan, via modulating AT1R and AT2R signaling in retinal inflammation. Invest Ophthalmol Vis Sci. 2006;47:5545–52.
Chao MV. Dependence receptors: what is the mechanism? Sci STKE. 2003. doi:10.1126/stke.2003.200.pe38.
Mehlen P, Thibert C. Dependence receptors: between life and death. Cell Mol Life Sci. 2004;61:1854–66.
Mehlen P, Rabizadeh S, Snipas SJ, Assa-Munt N, Salvesen GS, Bredesen DE. The DCC gene product induces apoptosis by a mechanism requiring receptor proteolysis. Nature. 1998;395:801–4.
Shi M, Zheng MH, Liu ZR, Hu ZL, Huang Y, Chen JY, et al. DCC is specifically required for the survival of retinal ganglion and displaced amacrine cells in the developing mouse retina. Dev Biol. 2010;348:87–96.
Grenz A, Dalton JH, Bauerle JD, Badulak A, Ridyard D, Gandjeva A, et al. Partial netrin-1 deficiency aggravates acute kidney injury. PLoS One. 2011;6:e14812.
Acknowledgments
We thank Dr Mao Nakayama, Dr Nyu Rong, and Ms Haruna Koizumi-Mabuchi for technical assistance. The telmisartan was kindly provided by Boehringer Ingelheim, Germany. This study was supported, in part, by a Keio University Gakujishinkoushikin grant to Y.O. The angiotensin II type 1 receptor blocker was a gift from Boehringer Ingelheim, Germany.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ozawa, Y., Yuki, K., Yamagishi, R. et al. Renin–angiotensin system involvement in the oxidative stress-induced neurodegeneration of cultured retinal ganglion cells. Jpn J Ophthalmol 57, 126–132 (2013). https://doi.org/10.1007/s10384-012-0204-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-012-0204-x