Summary
There is little research investigating polypharmacy and potentially inappropriate medications (PIM) in connection with cognitive status in residents of Austrian nursing homes. Our findings result from a cross-sectional survey of 425 residents (315 women, 110 men, mean 83.6 years) from 12 Austrian nursing homes. The number of systemically administered permanent prescription drugs was 8.99 ± 3.9 and decreased significantly with increasing cognitive impairment. Irrespective of cognitive status, polypharmacy (> 5 individual substances) was present in approximately 75 % of the residents. Hyper-polypharmacy (> 10 individual substances) was present among almost 50 % of the cognitively intact residents, and hence, significantly more frequent as compared with the group with the lowest cognitive performance (23.4 %). At least one PIM was found in 72.4 % of residents regardless of cognitive status. Predominantly, PIMs consisted of tranquilizers, antipsychotics, osmotic laxatives, non-steroidal anti-inflammatory drugs (NSAIDs) and anticholinergics, where only the number of NSAIDs decreased significantly with increasing cognitive impairment. In summary, our study shows a continued high prevalence of polypharmacy and PIM in long-term care institutions in Austria.
Zusammenfassung
Die Datenlage zu Polypharmazie und potentiell inappropriaten Medikamenten (PIM) bei Bewohnern von österreichischen Langzeitpflegeeinrichtungen in Abhängigkeit vom kognitiven Status ist unzureichend. Unsere Ergebnisse resultieren aus einer Querschnitterhebung von 425 Bewohnern (315 Frauen, 110 Männer, mean 83,6 Jahre) in 12 österreichischen Altenpflegeheimen. Die Zahl der systemisch verabreichten Dauermedikamente betrug 9,0 ± 3,9 und sank mit zunehmender kognitiver Beeinträchtigung signifikant. Polypharmazie (> 5 Einzelsubstanzen) fand sich unabhängig vom kognitiven Status bei etwa 75 % der Bewohner. Hyperpolypharmazie (> 10 Einzelsubstanzen) war mit knapp 50 % bei den kognitiv leistungsfähigeren Bewohnern signifikant häufiger als in der Gruppe mit der geringsten kognitiven Leistungsfähigkeit (23,4 %). Mindestens 1 PIM fand sich bei 72,4 % der Bewohner ohne signifikante Unterschiede in Bezug auf den kognitiven Status. Unter den PIM dominierten Tranquilizer, Antipsychotika, osmotische Laxantien, nicht steroidale Antirheumatika (NSAID) und Anticholinergika., wobei lediglich die Zahl der NSAID mit zunehmender kognitiver Beeinträchtigung signifikant abnahm. Zusammenfassend zeigt unsere Studie eine anhaltend hohe Prävalenz von Polypharmazie und PIM in Einrichtungen der Langzeitpflege in Österreich.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In Austria, an estimated 72,700 people live in nursing homes (NH) [1]. These mostly old and frail residents typically suffer from multiple chronic diseases, often in addition to functional and cognitive deficits. Medication treatment for this population is particularly challenging and requires particular sensitivity to maximise intended benefits and prevent potential harm. Due to the prevalence of multiple chronic diseases, polypharmacy is a common phenomenon [2] resulting in the increased risk of adverse drug events. Previous studies have shown that NH residents with cognitive impairment are given daily drug bundles of between 7 and 8 different medications [3], which are preferentially targeted at treatment of chronic conditions consistent with current guidelines rather than to manage symptoms, with questionable benefits to the residents [4]. Cognitively impaired individuals are particularly vulnerable to the substances that negatively affect the cognitive functions or trigger delirium. The progressive loss of communication skills associated with increasing cognitive impairment also negatively affects the ability to report disease symptoms and adverse drug events [5]. Data from the SHELTER study [2] show an inverse relationship between cognitive performance and hyper-polypharmacy (> 10 substances). However, the same study also found an unusually high use of psychoactive substances in the shape of excessive prescriptions of antipsychotics (35.6 %), tranquilizers (35.3 %) and antidepressants (31.8 %). Hyper-polypharmacy was directly associated with the presence of pain, which the authors interpreted as an explanation for the frequent use of analgesics (30 %) [2, 6]. Both, psychoactive substances as well as numerous analgesics are considered to be potentially inadequate medication (PIM) for old and frail people [7, 8].
The prevalence of PIM differs significantly across European countries [9], for the Austrian province of Vorarlberg, a recent study reported a PIM prevalence of 70 % in NH residents [10].
There are very few publications depicting the relationship between the extent of cognitive impairment and the prevalence of polypharmacy and PIM in nursing homes, with no data or publications from Austria to date. Therefore, the aim of our study was to answer the question whether the medication habits in nursing homes differ depending on residents’ levels of cognitive functioning, with a focus on polypharmacy and PIM.
Materials and methods
The present cross-sectional analysis of baseline data is part of a non-experimental pre-post study for optimising pain management in nursing homes in Austria ‘OSiA’ (“Optimiertes Schmerz-Management in Altenpflegeheimen”, German for: Optimized Pain Management in Nursing Homes).
Institutions and study participants
The study was conducted in 12 sites of one private nursing home operator in Austria, which were selected from a total of 29 nursing homes using a one-stage cluster sampling design. Baseline data were collected in 2011/12. The selected nursing homes are located in 7 of the 9 federal Austrian states. Participants were recruited by specially trained study coordinators and anonymised using code allocation for further exploitation of data by coordinators.
For inclusion and exclusion criteria see Table 1.
Data on medical diagnoses and prescriptions were recorded from the nursing homes’ documentation. The residents’ prescribed medication was classified according to the Anatomical Therapeutic Chemical classification system recommended by the World Health Organisation [11].
Classification according to cognitive state
The Mini Mental Status Examination (MMSE) modified by Kaiser et al. [12] was engaged to classify residents according to their cognitive abilities. Residents with MMSE > 17 were selected into group 1 (cognition intact—slightly impaired), residents with MMSE of 17 and lower were selected into group 2 (cognition moderately—severely impaired). Depending on the ability to communicate (i.e. verbal pain reporting using the verbal rating scale (VRS), since the primary focus of the project was pain management), group 2 was sub-divided: residents who were able to communicate were termed group 2s (s for self-report), residents unable to communicate were termed group 2p (p for proxy-assessment, i.e. non-verbal indications of pain).
Data analysis was performed using the statistical programme IBM®SPSS. Sample characteristics were presented using descriptive statistics. Group differences between the three cognitive groups were tested by analysis of variance (ANOVA) or Kruskal–Wallis test. Bonferroni or Dunn’s test were utilised in the post hoc analysis. The level of significance for a two-sided hypothesis testing was set a priori at 5 %.
This study was approved by the Ethics Committee of Salzburg (415-E/1412/8-2012 v. 19.6.2012).
A written consent what obtained from the nursing home residents or from their legal representatives.
Results
An overview of the participants’ characteristics is depicted in Table 2.
The number of systemically administered permanent prescription drugs was 8.99 ± 3.9, the sum of all permanent medications averaged at 10.35 ± 4.6, drugs prescribed as needed (PRN = pro re nata) averaged at 4.06 ± 3.8, resulting in a total amount of drugs of 14.37 ± 6.5 (mean ± SD).
In group 1, the average number of prescribed systemic permanent medications was 9.67 ± 3.93 (mean ± SD), in group 2s the average was 8.82 ± 3.86 and group 2p averaged at 6.81 ± 3.22. As opposed to drugs prescribed as needed, the number of (systemic) permanent medications showed significant differences in the context of cognitive performance. Group-related differences in prescribing behaviour are summarised in Table 3.
Polypharmacy (more than five permanent systemic medications) was found in all three groups with similar frequency (group 1 76.1 %, group 2s 79.1 %, group 2p 74.1 %, not significant (n.s)). More than 10 systemic permanent medications (hyper-polypharmacy) were present in 43.2 % of all cases, in group 1 the frequency was 48.7 %, in group 2s it was 42.6 % and in group 2p hyper-polypharmacy was significantly less frequent with 23.4 %.
As already shown in other studies, there is a clear domination of analgesics and anti-inflammatory drugs (NSAIDs), followed by antihypertensives, gastrointestinal therapeutics, dermatologics, anti-allergic agents and laxatives. A fairly significant percentage is also made-up of central nervous system-active substances. An overview of the types of prescribed drugs is listed in Table 4.
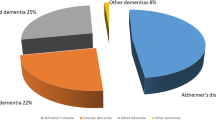
Following the PRISCUS and the Austrian PIM lists [7, 8], 72.4 % of nursing home residents received at least one potentially inappropriate medication, with no significant differences between the groups (group 1 74 %, group 2s 73.9 % and group 2p 64.1 %, n.s). Among the potentially inappropriate medications were predominantly tranquilizers, antipsychotics, osmotic laxatives, NSAIDs and anticholinergics. Significant differences were found only for NSAIDs, which were prescribed more frequently in group 1 (Fig. 1).
Among the overall systemic medications, the proportion of potentially inappropriate medications was 11.3 % for both groups 1 and 2s, and 10.74 % for group 2p (n.s). Moreover, subjects receiving at least 1 PIM were found to receive an average of 1.9 PIMs.
Discussion
Our study provides first data about polypharmacy and PIM in the context of various levels of cognitive impairment in residents of Austrian long-term care facilities. It shows that in systemic medication prescription, the proportion of polypharmacy (approximately 75 %) and hyper-polypharmacy (approximately 43 %) is very high, exceeding figures from previous publications. In the European SHELTER study, polypharmacy was present in 49.7 % and hyper-polypharmacy in 24.3 % of cases [2]. Publications from North America evidence polypharmacy in nursing home residents of up to 40 % [13, 14]. These differences can not solely be explained by different research methods (timeframe, inclusion or exclusion of prescribed topical substances and PRN medication, definition of polypharmacy), but also reflect different regulatory frameworks and prescribing habits [9].
Our study shows that the number of prescribed systemic medication significantly decreases with increasing cognitive impairment, but in contrast, the proportion of potentially inappropriate medications remains unchanged. This finding is contrary to other studies that showed decreasing cognitive or functional skills to result in a decline in PIM [15, 16].
Among the potentially inappropriate medications, we found a clear trend towards psychoactive substances (tranquilizers and antipsychotics), confirming their continued high prevalence in Austrian nursing home residents, mostly used for treatment of agitation and sleep disorders and contributing to adverse events like falls, delirium and cognitive decline [10, 17]. To date, there is no trend reversal in prescribing behaviour as a result of numerous international publications on adverse side-effects of psychotropic drugs in geriatric populations. In our study, NSAIDs have also been prescribed fairly often with the prescription numbers significantly decreasing as cognitive impairment increased (group 1 27.3 %, group 2s 10.6 %, group 2p 4.9 %). This is in agreement with results from the SHELTER study [2, 6], and further proves—in line with other studies—that people with cognitive impairment receive fewer analgesics [18–20]. The proportion of residents receiving at least one PIM was 72.4 %, a figure similar to the frequency of 71 % found in a recent French publication [16]. Some data suggest that reduction of permanent prescriptions can be done according to a published algorithm without any significant adverse events, but a global improvement in health [21].
It should be noted that our study is based on PIM lists, while expert consensus recommendations for the ‘appropriateness’ of medications in advanced dementia that are based on care goals define other substances as inappropriate [22]. Among these are first and foremost lipid-lowering agents, antiplatelet medication (except aspirin), anticholinergics, antidementia drugs and vitamin K antagonists, but also laxatives and proton-pump inhibitors.
Our results confirm the high prevalence of polypharmacy decreasing with increasing cognitive impairment. Although to date, several studies have dealt with this issue, none of them could provide valid explanations for this phenomenon [6]. So far, various explanations have been considered: drugs that influence cognition should not be given to demented patients, partly due to the increasing difficulty of oral medication delivery in this patient population. In addition, increasing cognitive impairment is associated with limited life expectancy leading to careful consideration of which drugs are still beneficial. Moreover, with increasing cognitive decline arise communication problems whereby only limited information about symptoms or adverse drug effects can be communicated. We provide evidence to support the latter explanation, because the lack of self-report was used as a criterion for advanced cognitive decline.
Our study also has some limitations: The investigation was conducted only in facilities of one private nursing home operator. However, since in Austria the conditions for the establishment and operation of a nursing home are regulated by law, it can be assumed that the data are representative of other facilities. Variances in prescription behaviour could be due to the fact that medical care is not provided by the physician-on-staff, but predominantly by primary care physicians, particularly with regard to the low availability of specialists. Since the study was conducted only in long-term care facilities, the findings cannot be applied to other types of settings. In addition, the chosen definition of various degrees of cognitive impairment does not allow conclusions about aetiology and is also not related to potentially relevant parameters, such as quality of life.
Conclusion
The present study shows a continued high prevalence of polypharmacy and PIM in long-term care facilities in Austria, irrespective of cognitive function. There is a continued need for action in order to lower the high proportions of polypharmacy and PIM and to optimise medication treatment in the particularly vulnerable group of nursing home residents. This requires implementation studies that show tools for reducing polypharmacy and PIM in various settings caring for older people can be applied successfully.
References
Statistik Austria 2013. Accessed June 2015. http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/soziales/sozialleistungen_auf_landesebene/betreuungs_und_pflegedienste/index.html.
Onder G, Liperoti R, Fialová D, et al. Polypharmacy in nursing home in Europe: results from the SHELTER Study. J Gerontol A Biol Sci Med Sci. 2012;67A(6):698–704.
Doshi JA, Shaffer T, Briesacher BA, et al. National estimates of medication use in nursing homes: findings from the 1997 medicare current beneficiary survey and the 1996 medical expenditure survey. J Am Geriatr Soc. 2005;53:438–43.
Tjia J, Rothman MR, Kiely DK, et al. Daily medication use in nursing home residents with advanced dementia. J Am Geriatr Soc. 2010;58:880–8.
Onder G, Gambassi G, Scales CJ, et al. Adverse drug reactions and cognitive function among hospitalized older adults. Eur J Clin Pharmacol. 2002;58:371–7.
Vetrano DL, Tosato M, Colloca G, et al. Polypharmacy in nursing home residents with severe cognitive impairment: results from the SHELTER Study. Alzheimers Dement. 2013;9:587–93.
Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medication in the elderly—PRISCUS list. Dtsch Arztebl Int. 2010;107:543–51.
Mann E, Böhmdorfer B, Frühwald T, et al. Potentially inappropriate medication in geriatric patients: the Austrian consensus panel list. Wien Klin Wochenschr. 2012;124(5–6):160–9.
Fialová D, Topinková E, Gambassi G, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005;293(11):1348–58.
Mann E, Haastert B, Böhmdorfer B, et al. Prevalence and associations of potentially inappropriate prescriptions in Austrian nursing home residents: secondary analysis of a cross-sectional study. Wien Klin Wochenschr. 2013;125:180–8.
WHO 2010. The anatomical therapeutic chemical classification system. Accessed Nov 2010. http://www.whocc.no/atc_ddd_index/.
Kaiser A, Gusner-Pfeiffer R, Griessenberger H, et al. Mini-Mental-State—Ein Screening in vielen Versionen. Z Gerontopsychol Psychiatr. 2009;22:11–6.
Dwyer LL, Han B, Woodwell DA, Rechtsteiner EA. Polypharmacy in nursing home residents in the United States: results of the 2004 National Nursing Home Survey. Am J Geriatr Pharmacother. 2010;8(1):63–72.
Bronskill SE, Gill SS, Paterson JM, et al. Exploring variation in rates of polypharmacy across long-term care homes. J Am Med Dir Assoc. 2012;13(3):309.e15–21.
Colloca G, Tosato M, Vetrano DL, Topinkova E, et al. Inappropriate drugs in elderly patients with severe cognitive impairment: results from the shelter study. PLoS One. 2012;7(10):e46669.
Cool C, Cestac P, Laborde C, et al. Potentially inappropriate drug prescribing and associated factors in nursing homes. J Am Med Dir Assoc. 2014;15(11):850.e1–9.
Mann E, Köpke S, Haastert B, et al. Psychotropic medication use among nursing home residents in Austria: a cross-sectional study. BMC Geriatr. 2009;9:18.
Morrison RS, Siu AL. A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage. 2000;19:240–8.
Closs SJ, Barr B, Briggs M. Cognitive status and analgesic provision in nursing home residents. Br J Gen Pract. 2004;54(509):919–21.
Cornali C, Franzoni S, Gatti S, et al. Diagnosis of chronic pain caused by osteoarthritis and prescription of analgesics in patients with cognitive impairment. J Am Med Dir Assoc. 2006;7(1):1–5.
Garfinkel D, Mangin D. Feasibility study of a systematic approach for discontinuation of multiple medications in older adults. Arch Intern Med. 2010;170:1648–54.
Holmes HM, Sachs GA, Shega JW, et al. Integrating palliative medicine into the care of persons with advanced dementia: identifying appropriate medication use. J Am Geriatr Soc. 2008;56:1306–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Alzner, U. Bauer, S. Pitzer, M. M. Schreier, J. Osterbrink, and B. Iglseder declare that there are no actual or potential conflicts of interest in relation to this article.
Rights and permissions
About this article
Cite this article
Alzner, R., Bauer, U., Pitzer, S. et al. Polypharmacy, potentially inappropriate medication and cognitive status in Austrian nursing home residents: results from the OSiA study. Wien Med Wochenschr 166, 161–165 (2016). https://doi.org/10.1007/s10354-015-0428-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-015-0428-8