Abstract
This study prospectively investigated the incidence of vocal fold immobility, unilateral and bilateral, and its influence on aspiration status in a referred population of 1452 patients for a dysphagia evaluation from a large, urban, tertiary-care, teaching hospital. Main outcome measures included overall incidence of vocal fold immobility and aspiration status, with specific emphasis on age, etiology, and side of vocal fold immobility, i.e., right, left, or bilateral. Overall incidence of vocal fold immobility was 5.6% (81 of 1452 patients), including 47 males (mean age 55.7 yr) and 34 females (mean age 59.7 yr). In the subgroup of patients with vocal fold immobility, 31% (25 of 81) exhibited unilateral right, 60% (49 of 81) unilateral left, and 9% (7 of 81) bilateral impairment. Overall incidence of aspiration was found to be 29% (426 of 1452) of all patients referred for a swallow evaluation. Aspiration was observed in 44% (36 of 81) of patients presenting with vocal fold immobility, i.e., 44% (11 of 25) unilateral right, 43% (21 of 49) unilateral left, and 57% (4 of 7) bilateral vocal fold immobility. Left vocal fold immobility occurred most frequently due to surgical trauma. A liquid bolus was aspirated more often than a puree bolus. Side of vocal fold immobility and age were not factors that increased incidence of aspiration. In conclusion, vocal fold immobility, with an incidence of 5.6%, is not an uncommon finding in patients referred for a dysphagia evaluation in the acute-care setting, and vocal fold immobility, when present, was associated with a 15% increased incidence of aspiration when compared with a population already being evaluated for dysphagia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Aspiration does not always occur in the presence of vocal fold immobility and, conversely, aspiration can occur when the true vocal folds are functioning normally. The relationship, therefore, between dysphagia and laryngeal functioning is more complex than simply a lack of glottic closure during swallowing [1]. As a result, glottic closure for airway protection is important but not sufficient to prevent aspiration, i.e., dysphagia associated with vocal fold immobility is not due solely to impaired laryngeal deglutitive kinetics [2]. Other independent pharyngeal function dysmotility factors contribute to pharyngeal dysphagia and aspiration [1–3].
A successful pharyngeal swallow results from a series of coordinated, interrelated, and sequentially timed motor events. Base-of-tongue driving force, pharyngeal stripping wave, elevation of the hyolaryngeal complex in conjunction with relaxation and opening of the upper esophageal sphincter, and true vocal fold closure all work together in an integrated fashion that results in a successful swallow. A protective cough reflex acts as the final barrier to tracheal aspiration [4]. Weakness or absence of one (or more) of these events does not automatically result in aspiration because compensation may allow for a successful swallow [5]. Pharyngeal dysphagia resulting in aspiration will occur only when the pharyngeal swallow is altered enough to prevent efficient bolus passage from the oral cavity through the pharynx and into the esophagus.
Patients with unilateral tenth nerve paralysis as well as isolated recurrent laryngeal nerve injury not only demonstrate ipsilateral vocal fold immobility but often present with multiple abnormalities of supraglottic laryngeal and pharyngeal functions [2,3,6]. These findings were corroborated in a recent retrospective study that found the incidence of aspiration to be 38% in patients presenting with unilateral vocal fold immobility [5]. Aspiration was attributed to supraglottic factors which impaired airway protection, i.e., incomplete laryngeal elevation resulting in abnormal epiglottic tilt, an abnormal pharyngeal stripping wave, and pharyngeal retention. These abnormalities can cause aspiration independent of vocal fold mobility status [3]. Vocal fold immobility, therefore, appears not to be the single causative variable for aspiration but rather is one of a number of factors contributing to pharyngeal dysphagia and aspiration.
The purpose of the present study was to investigate prospectively the incidence of vocal fold immobility, unilateral and bilateral, and its influence, if any, on aspiration status in patients referred for dysphagia evaluations in the tertiary care setting.
Methods
Subjects
In a prospective manner, 1452 hospitalized patients referred for a swallowing evaluation were included. Fiberoptic endoscopic evaluation of swallowing (FEES) [7,8] was used to determine both aspiration status and vocal fold immobility. All FEES evaluations were performed within 48 hours of the referral. Vocal fold immobility, rather than vocal fold paralysis, was used to describe laryngeal function without stating or implying etiology [5]. Eighty-one patients were identified with either unilateral or bilateral true vocal fold immobility (Table 1). No patient had prior vocal fold medialization therapy.
Equipment
Equipment consisted of a 3.6-mm-diameter flexible fiberoptic rhinolaryngoscope (Olympus, ENF-P3), light source (Olympus, CLK-4), camera (ELMO, MN401E), and color monitor (Magnavox, RJ4049WA01).
Procedures
The basic FEES protocol [7,8] was done at bedside, with the patient between 60° and 90° upright, and without administration of topical anesthesia to the nasal mucosa, thereby eliminating any potential adverse anesthetic reactions and ensuring a reliable physiologic evaluation [9]. Identification of vocal fold immobility was made by the first author based on no movement of the vocal fold(s) with repeated phonations of /ee/. Specific findings identified as contributing to pharyngeal dysphagia were (1) the stage transition characterized by depth of bolus flow to at least the vallecula prior to the pharyngeal swallow, (2) evidence of bolus retention in the vallecula or pyriform sinuses after the pharyngeal swallow, (3) laryngeal penetration defined as material in the laryngeal vestibule but not passing below the level of the true vocal folds either before or after the pharyngeal swallow, and (4) tracheal aspiration defined as material below the level of the true vocal folds either before or after the pharyngeal swallow [4].
Results
Table 1 shows participant demographics. Overall incidence of aspiration was observed to be 29% (426 of 1452) of all subjects referred for a swallow evaluation. Overall incidence of vocal fold immobility was 5.6% (81 of 1452 subjects), i.e., 47 males (mean age 55.7 yr) and 34 females (mean age 59.7 yr). In the subgroup of patients with vocal fold immobility, 60% (49 of 81) exhibited unilateral left, 31% (25 of 81) unilateral right, and 9% (7 of 81) bilateral vocal fold immobility. Aspiration was observed in 44% (36 of 81) of subjects presenting with vocal fold immobility, i.e., 8% (3 of 36) before the swallow and 92% (33 of 36) during or after the swallow.
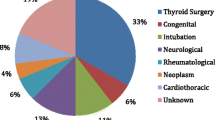
Table 2 groups the etiologies of vocal fold immobility by categories, i.e., iatrogenic, idiopathic, neurologic, and trauma. Some etiologies were associated more strongly with side of vocal fold immobility. Cardiac surgery and esophageal surgery were associated with left vocal fold immobility in 71% (10 of 14) and 85% (11 of 13) of patients, respectively. Head/neck surgery (including thyroid surgery) was less associated with left vocal fold immobility in 62% (8 of 13) of patients. Medical, neurosurgical, neurologic and trauma were not associated with side of vocal fold immobility.
Table 3 shows incidences of bolus flow before the pharyngeal swallow, bolus retention after the pharyngeal swallow, and laryngeal penetration for both liquid and puree bolus consistencies in patients who aspirated. Liquids were aspirated more frequently than puree. Signs of pharyngeal dysphagia were more prevalent with liquid vs. puree bolus consistencies and many patients exhibited more than one sign, i.e., liquid bolus retention (86%) and/or laryngeal penetration of (53%) vs. puree bolus retention (58%) and/or laryngeal penetration (47%). (Note: Five participants were deferred liquids due to severe pharyngeal dysphagia and aspiration with puree. Extrapolating this missing data, liquid bolus retention increases to 100% and laryngeal penetration increases to 67%.)
Table 4 shows aspiration status based on age and side of vocal fold immobility, i.e., right, left, or bilateral. Data indicated that 44% (11 of 25) of patients with unilateral right, 43% (21 of 49) of patients with unilateral left, and 57% (4 of 7) of patients with bilateral vocal fold immobility aspirated. Mean ages based on aspiration status for unilateral right, unilateral left, and bilateral vocal fold immobility were 62.5, 64.3, and 68.8 years, respectively. No differences in aspiration status were observed due to side of vocal fold immobility or age.
Discussion
The present study is the first to report on the overall incidence of vocal fold immobility in patients presenting with symptoms of dysphagia based on a heterogeneous referral base from a large, urban, tertiary-care, teaching hospital. It was found that 5.6% of patients exhibited either unilateral or bilateral vocal fold immobility. Previous studies [1,5,10] did not report population statistics from which their subjects were drawn. Vocal fold mobility impairment, therefore, in patients referred for swallowing evaluations in the acute-care setting is not an uncommon finding.
Interestingly, vocal fold immobility was an incidental finding first identified during FEES, i.e., not the primary reason for a referral for a dysphagia evaluation. Three explanations may account for this: (1) There may be no immediate perceptual change in vocal quality because the mobile fold crosses the midline to adduct with the immobile fold. (2) Knowledge of the vocal change characteristic of vocal fold immobility, i.e., breathy not hoarse, may not be well understood. (3) Vocal quality change may be attributed to other etiologies, e.g., intubation trauma, neurologic deficits, or overall physical weakness.
It is generally accepted that the probability of aspiration is increased in the presence of vocal fold immobility [5], but the actual increased incidence has not been known. In this large series, 29% of all patients referred for a swallow evaluation aspirated, while aspiration was noted in 44% of the subset of patients who exhibited vocal fold immobility. Presence of vocal fold immobility, therefore, is associated with a 15% increased incidence of aspiration in patients referred for a dysphagia evaluation. This association underscores the importance of assessing swallowing in all newly diagnosed cases. Since a number of pharyngeal function dysmotility factors, including but not limited to vocal fold immobility, contribute to pharyngeal dysphagia and aspiration [1–3], it is important to determine if dysphagia is present in order to implement appropriate intervention strategies to promote safe swallowing [1,10].
The present findings are corroborated by a number of recent studies. Since there are redundant safeguards to prevent aspiration, loss of one (or more) features does not automatically result in aspiration, i.e., 56% of patients with vocal fold immobility did not aspirate, while 44% of patients with vocal fold immobility aspirated. Other studies which investigated vocal fold immobility and aspiration status reported slightly lower incidences of aspiration, i.e., 23.4% [1] and 38% [5]. The differences may be attributed to swallowing compensations occurring between the time of identification of vocal fold immobility and the swallow evaluation, e.g., 1–2 days in the present study vs. 8.9 weeks [1].
Consistent with previous research, aspiration occurred more frequently on liquid consistency [10] and after the swallow [5] (Table 3) because factors other than impaired laryngeal deglutitive kinetics contributed to a disordered pharyngeal swallow [1–3,10]. Puree consistency, although retained in the vallecula, pyriform sinuses, and even laryngeal vestibule, was aspirated less often because it did not flow quickly into the trachea, allowing time for pharyngeal clearing with a subsequent swallow. It is recommended, therefore, that when puree consistencies are swallowed successfully but liquids are aspirated, thickened liquids be trialed to promote safer swallowing [10].
In the present study, left vocal immobility occurred most frequently (60%), which is similar to other studies with adequate sample size to determine distribution [1]. This was due to more patients referred for a swallow evaluation after cardiac and esophageal surgery than any other category [1,11,12]. Incidence of aspiration was not different based upon left (44%), right (43%), or bilateral (57%) vocal fold immobility. Age did not differentiate aspirators versus nonaspirators with vocal fold immobility.
Since timing of aspiration often varies during the same examination, i.e., it can occur before, during, and/or after the pharyngeal swallow, it is important to know both why and when aspiration occurs. The majority of aspiration events in the present study, i.e., 92%, occurred either during or after the swallow due to a weak pharyngeal swallow and impaired airway protection [1,5], i.e., bolus retention in the vallecula, pyriform sinuses, or laryngeal vestibule, followed by tracheal aspiration. This is, in part, due to the nature of FEES. Some instances of aspiration may have occurred during the swallow and were not identified as such because of the brief “whiteout” period caused by the base of tongue and pharyngeal walls contacting the optical tip of the endoscope. Regardless of the timing, the underlying pathophysiology of the aspiration event is due to (1) premature loss of the bolus into the trachea before the swallow, (2) lack of laryngeal rise during the pharyngeal swallow leading to aspiration when the vocal folds are not fully adducted, (3) lack of laryngeal rise during the swallow leading to residual upper airway penetration with aspiration after the swallow, and (4) bolus retention and spillover from the pyriform sinuses after the pharyngeal swallow due to weak pharyngeal swallow, poor passage of the bolus through the upper esophageal sphincter, or backflow from a Zenker’s diverticulum. Therefore, other independent pharyngeal function dysmotility factors, not just disruption of laryngeal deglutitive kinetics, contribute to pharyngeal dysphagia and aspiration [1–3].
In the acute-care setting the goal of a dysphagia consultation is to diagnose dysphagia and make recommendations for appropriate compensatory strategies, e.g., bolus consistency and volume, and feeding strategies, i.e., positioning and rate of feeding, to prevent aspiration and determine the safest and least restrictive oral intake. This goal continues in the rehabilitation setting with the addition of implementing appropriate treatments, e.g., muscle strengthening and retraining, based on the best determination of the pathophysiology of the pharyngeal swallow once the acute phase of illness has resolved.
Conclusion
Vocal fold immobility, with an incidence of 5.6% from a referred population for a dysphagia evaluation, is not an uncommon finding in the acute-care setting. Twenty-nine percent of the total referral population exhibited aspiration while 44% of patients with vocal fold immobility aspirated, indicating that vocal fold immobility was associated with a 15% increased incidence of aspiration in patients already suspected of dysphagia. Left vocal fold immobility occurred most frequently (60%) due to surgical trauma. A liquid bolus was aspirated more often than a puree bolus. Side of vocal fold immobility, i.e., left, right, or bilateral, and age were not factors associated with an increased incidence of aspiration.
References
N Bhattacharyya T Kotz J Shapiro (2002) ArticleTitleDysphagia, aspiration with unilateral vocal cord immobility: incidence, characterization, and response to surgical treatment Ann Otol Rhinol Laryngol 111 672–679 Occurrence Handle12184586
JA Wilson A Pryde A White L Maher AGD Maran (1995) ArticleTitleSwallowing performance in patients with vocal fold motion impairment Dysphagia 10 149–154 Occurrence Handle10.1007/BF00260968 Occurrence Handle7614853
O Ekberg S Lindgren T Schultze (1986) ArticleTitlePharyngeal swallowing in patients with paresis of the recurrent nerve Acta Radiol Diag 27 697–700
JA Logemann (1998) Evaluation and Treatment of Swallowing Disorders EditionNumber2 Pro-Ed Austin, TX
RF Heitmiller E Tseng B Jones (2000) ArticleTitlePrevalence of aspiration and laryngeal penetration in patients with unilateral vocal fold motion impairment Dysphagia 15 184–187 Occurrence Handle10.1007/s004550000026 Occurrence Handle11014880
S Perie B Roubeau JL St. Guily (2003) ArticleTitleLaryngeal paralysis: distinguishing Xth nerve from recurrent nerve paralysis through videoendoscopic swallowing study (VESS) Dysphagia 8 276–283 Occurrence Handle10.1007/s00455-003-0025-7
SE Langmore K Schatz N Olsen (1988) ArticleTitleFiberoptic endoscopic evaluation of swallowing safety: a new procedure Dysphagia 2 216–219
SE Langmore K Schatz N Olsen (1991) ArticleTitleEndoscopic and videofluoroscopic evaluations of swallowing and aspiration Ann Otol Rhinol Laryngol 100 678–681
SB Leder DA Ross KB Briskin CT Sasaki (1997) ArticleTitleA prospective, double-blind, randomized study on the use of topical anesthetic, vasoconstrictor, and placebo during transnasal flexible fiberoptic endoscopy J Speech Lang Hear Res 40 1352–1357 Occurrence Handle9430755
N Bhattacharyya T Kotz J Shapiro (2003) ArticleTitleThe effect of bolus consistency on dysphagia in unilateral vocal cord paralysis Otolaryngol Head Neck Surg 129 632–636 Occurrence Handle14663428
LD Holinger PC Holinger PH Holinger (1976) ArticleTitleEtiology of bilateral abductor vocal cord paralysis: a review of 389 cases Ann Otol Rhinol Laryngol 85 428–436 Occurrence Handle949150
GE Woodson RH Miller (1981) ArticleTitleThe timing of surgical intervention in vocal cord paralysis Otolaryngol Head Neck Surg 89 264–267 Occurrence Handle6787523
Author information
Authors and Affiliations
Corresponding author
Additional information
This research was supported in part by the McFadden, Harmon, and Mirikitani Endowments.
Rights and permissions
About this article
Cite this article
Leder, S.B., Ross, D.A. Incidence of Vocal Fold Immobility in Patients with Dysphagia. Dysphagia 20, 163–167 (2005). https://doi.org/10.1007/s10350-005-0002-4
Issue Date:
DOI: https://doi.org/10.1007/s10350-005-0002-4