Abstract
Object
Over the last decade, the number of clinical MRI studies at 7 T has increased dramatically. Since only limited information about the safety of implants/tattoos is available at 7 T, many centers either conservatively exclude all subjects with implants/tattoos or have started to perform dedicated tests for selected implants. This work presents our experience in imaging volunteers with implants/tattoos at 7 T over the last seven and a half years.
Materials and methods
1796 questionnaires were analyzed retrospectively to identify subjects with implants/tattoos imaged at 7 T. For a total of 230 subjects, the type of local transmit/receive RF coil used for examination, imaging sequences, acquisition time, and the type of implants/tattoos and their location with respect to the field of view were documented. These subjects had undergone examination after careful consideration by an internal safety panel consisting of three experts in MR safety and physics.
Results
None of the subjects reported sensations of heat or force before, during, or after the examination. None expressed any discomfort related to implants/tattoos. Artifacts were reported in 52 % of subjects with dental implants; all artifacts were restricted to the mouth area and did not affect image quality in the brain parenchyma.
Conclusion
Our initial experience at 7 T indicates that a strict rejection of subjects with tattoos and/or implants is not justified. Imaging can be conditionally performed in carefully selected subjects after collection of substantial safety information and evaluation of the detailed exposure scenario (RF coil/type and position of implant). Among the assessed subjects with tattoos, no side effects from the exposure to 7 T MRI were reported.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) is a non-invasive imaging technique that was introduced into clinical diagnostics in the 1980s. Since then, MRI has proven to be the imaging modality of choice for a variety of diseases as expressed by more than 30,000 installations worldwide and over 70 million examinations per year [1]. Although most of the MR systems around the world operate at 1.5 Tesla (T) or 3 T, the number of installations of 7 T MR systems has increased very rapidly over the last 10 years [2]. The rise of 7 T MR systems has led to promising results obtained for both anatomical and functional imaging studies [3–6].
Furthermore, with the increasing number of clinically-oriented MRI studies at 7 T, the examination of patients with implants has become relevant. Also, artistic tattoos and permanent make-up have become mainstream and are increasingly encountered in both patients and healthy volunteers to be included in MRI studies. However, as 7 T MRI is currently not medically indicated and as ultra high-field (UHF) MRI facilities tend to be rightly very cautious with respect to the higher resonance frequency and various transmit radiofrequency (RF) coil configurations, the general question of contraindications for a 7 T scan is regularly discussed. Within the UHF community, some sites conservatively exclude all subjects with tattoos or metallic implants regardless of type or location, while other sites have already performed dedicated safety tests for certain implants [7–11] or have included carefully selected subjects with implants or tattoos [12].
In general, performing an MR scan on patients with metallic implants at any field strength is contraindicated unless the implant manufacturer includes “MR Safe” or “MR Conditional” labeling for the specific implant in the instructions for use [13]. However, no standards or test methods currently explicitly address MR safety testing for implants at 7 T, although some standards describe the MR environment in general or imply a transfer of test methods to MR field strengths other than 1.5 and 3 T.
At a field strength of 7 T, some complex and specific challenges arise. The increase of the field strength leads to a reduction of the Larmor wavelength λ, which is roughly 14 cm at 7 T in the human body (example given for liver tissue with a permittivity of 53.6) [14], much less than the Larmor wavelength of 29 and 52 cm for 3 and 1.5 T, respectively. Incident RF electric fields induce currents on the metal surface of an implant which subsequently generate concentrated current densities inside the body tissue at the ends and edges of the implant, leading to an elevation of the specific absorption rate (SAR) and potential temperature rise. Hence, the short wavelength at 7 T not only introduces strong inhomogeneities in MR images due to B1 artifacts, but can also lead to strong coupling (high current densities) between the electromagnetic field and conducting implants. The reduced RF wavelength at 7 T in human tissue (generally in the range of 10–15 cm) can produce resonance effects in implanted medical devices of shorter dimensions compared to 1.5 or 3 T. In a study at 1.5 T on RF-induced temperature elevations on metallic wires, Armenean et al. [15] showed that heating peaks occur between classical resonant lengths at multiples of λ/4 for the implant. Furthermore, heating not only occurs at the tip, but also along the implant. Hence, avoiding classical resonant lengths (λ/2, or λ) is not sufficient to ensure patient safety. Besides the antenna effect of implants with a certain length or circumference, any metallic structure distorts the incident electromagnetic field, which may lead to changes in the SAR (and temperature) distribution, particularly for UHF imaging where the coupling of the electromagnetic field to the human body and to implants becomes more complex [16, 17]. Implants with small linear dimensions relative to the wavelength can be expected to have only minimal impact on the local SAR. Nevertheless, Winter et al. [18] found an increase in the local 1-g SAR of roughly 50 % for stent-like structures with a length of 1 cm at 7 T, with a lower impact on the local 10-g SAR.
Furthermore, only local transmit RF coils of various designs and specifications are used at 7 T, whereas nearly all MR scans at clinical field strength are performed with integrated whole-body RF transmit coils. This aspect is particularly important in high-field MRI, since field distribution and polarization are significantly non-uniform in the human body and, moreover, depend on the design of the local transmit coil and the size and tissue distribution of the body [19]. Of course, also other features of UHF MRI need to be considered when discussing MR safety, such as travelling wave effects and altered field distribution and polarization when using parallel transmission techniques (RF shimming, Transmit SENSE) [20, 21], which can have a substantial impact on SAR [22].
Whether in clinical settings or at research sites, dental implants are the most common implants seen. Dental implants are generally of no concern at clinical field strength [23], but may be at 7 T, especially since intracranial imaging is one of the most frequently performed applications at 7 T. One of the major concerns of scanning dental implants at clinical field strength is the induction of artifacts due to the presence of metal that may render imaging results useless [24–27].
In addition to dental implants, there are a wide variety of other metallic implants that might be encountered in subjects being considered for a 7 T MR examination. Also, patients and healthy volunteers with artistic tattoos and/or permanent make-up are more and more encountered in MRI studies. Since tattoos are a relative contraindication at clinical field strength [28], an active topic is whether a tattoo should be considered an absolute contraindication at 7 T or not [12]. Especially tattoos older than approximately 20 years, as well as body art not obtained in proper studios (e.g., among inmates), are suspected to include iron oxide and other metals to a high degree [29, 30]. Among the millions of MR scans that have been performed since the advent of MRI, very few incidents at clinical field strengths related to tattoos or permanent make-up have been reported. Even if incidents with RF-induced skin burns [31–38] or skin irritations allegedly induced by torques and attractive forces on ferromagnetic ink particles [39, 40] have sporadically happened, there is a strong general history of safe use in imaging patients with tattoos up to 3 T [41]. Such history has not yet been established at 7 T. On the other hand, at 7 T, the majority of examinations are performed with local transmit RF coils, e.g., transmit head coils; thus, RF-induced skin burns in tattoos located outside the RF-exposed body areas are unlikely. The use of local transmit RF coils at 7 T can be seen here as advantageous for implants or tattoos that are at a sufficient distance from the exposure volume of the RF coil. This study presents 7.5 years of experience at our institute in imaging patients and healthy volunteers with implants and/or tattoos at 7 T.
Materials and methods
Questionnaires and screening forms from October 2006 to April 2014 (7.5 years) were analyzed retrospectively to identify all subjects with implants and/or tattoos cleared for imaging at our institution. During this period, 230 out of 1796 healthy volunteers and volunteers with known pathologies had implants or tattoos and underwent an MR examination on a whole-body 7 T MR system (Magnetom 7 T, Siemens Healthcare, Germany). Of the 230 subjects, 109 presented with one or several tattoos and 135 reported one or several implants; 14 subjects had both tattoos and implants. For the 135 subjects with implants, 93 of them had their implant located in the orofacial region (dental implants), whereas the other implants were located elsewhere in the body (Fig. 1a).
a Distribution of a number of implants imaged at 7 T. b Location of implants and tattoos with respect to head scans. The red area represents the exposure volume of the transmit coil. The orange part shows locations of tattoos or implants less than 30 cm from the exposure volume of the transmit coil. c Circularly polarised (CP) birdcage transmit coil with a 32-channel receive array (Nova Medical, USA)
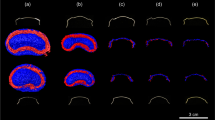
All subjects were cleared for 7 T on a case by case basis by an MR safety expert panel in our institute, consisting of three physicists and engineers with extensive experience in MRI and RF effects. The types of implants (material, dimension, geometry) were carefully examined as well as their location with respect to the exposure volume of the transmit coil of each study. The decision-making process was basically divided into three categories which are explained in Table 1. Here, a distance of 30 cm between an implant and the local RF coil was used to define the categories, as this distance yielded almost no stray RF fields at the location of the implant for the head coil (Fig. 1c and Table 2) and body coil used (Table 2). Numerical simulations (SEMCAD X SPEAG, Zurich, Switzerland) conducted with two heterogeneous body models (‘Duke' and ‘Ella') [42] confirm a significant decrease of the local SAR in the trunk beyond 30 cm, as shown in Fig. 2a, b. Furthermore, the SAR in the extremities, particularly in the arms, is also substantially lower (local SAR 10- and 20-times lower in the wrist than in the head for the female and male model, respectively). This behavior is substantially different to clinical routine (1.5 and 3 T using body coils) where the maximum local SAR is often located in peripheral extremities [43, 44]. Of course, in general, travelling wave effects need to be considered, especially for implants with dimensions near resonance or larger than a quarter of the wavelength, even when they are located a large distance from the transmit coil. These implants should be excluded without detailed simulations in which the full magnet bore, including the shield of the gradient coil, are included to confirm that the aforementioned rule of thumb remains valid for each individual exposure scenario. If applicable, information about the exact location of the reported implant was assessed from previous computer tomography (CT) or plain X-ray imaging retrieved from the picture archiving and communication system (PACS) of the referring hospital.
Distribution of the local 10 g-averaged SAR obtained with a finite-difference time-domain (FDTD) solver (SEMCAD-X, SPEAG, Zurich, Switzerland) for a custom-built meander stripline head coil [63] in heterogeneous body models of the 'Virtual Family' [42] (a Duke, b Ella). The total input power was scaled so that the local 10 g-averaged SAR reached the International Electrotechnical Commission (IEC) limit of 10 W/Kg [65]. Both a and b show a significant decrease of the local SAR at a distance of 30 cm from the transmit coil for both trunk (between 40- and 1000-times lower than the maximum value in the head) and arms (10- and 20-times lower than the maximum value in the head for the female and male model, respectively). In b, the local SAR is reduced by a factor greater than 100 in the pelvic region where intrauterine devices are located
Regarding tattoos, tattoos located less than 30 cm from the RF coil or located within the RF coil were cleared for imaging if they were made after the year 2000 and in countries of the European Union as well as in proper tattoo studios. This limit was set based on a survey from Tope et al. [41], which showed that only 2 out of 135 subjects with tattoos experienced slight tingling or a sensation of burning associated with MRI. The rising popularity of tattoos in Europe has increased awareness of official bodies regarding the potential presence of toxic substances in the ink. As a result, two resolutions of the Council of Europe were ratified. The resolution ResAP (2003) 2 [45] published in 2003 lists substances that should not be included in tattoo ink. In 2008, the revised resolution ResAP (2008) 1 [46] superseded ResAP (2003) 2 and introduced maximum allowable concentrations of (metallic) impurities. Nevertheless, in Germany it can be assumed that almost all tattoo studios already started using approved ink approximately in the year 2000, as the Cosmetic Commission from the Federal Institute for Risk Assessment (Bundesinstitut für Risikobewertung) recommended regulations for tattoo ink in this year [47].
Figure 1b shows the location of the implants and tattoos with respect to the exposure volume of a transmit head coil. For implants inside the exposure volume of the transmit coil, the acquired 7 T MR images were screened for the presence of artifacts. The impact of these artifacts was assessed qualitatively by visual inspection as to whether their disturbances were confined to the direct vicinity of the implants or if they impaired the depiction and delineation of the structure of interest. The different transmit/receive RF coils used to acquire images from subjects with implants and/or tattoos are listed in Table 2, and one of them is exemplarily shown in Fig. 1c.
Dental implants
A total of 93 carefully selected volunteers underwent a 7 T head scan with a known dental implant. Details regarding the individual numbers and types of dental implants are provided in Table 3. Among these 93 subjects, 83 had their implants directly in the exposure volume of the transmit coil (head coil; CP, no parallel transmission techniques). Subjects with retainers were cleared for 7 T based on the work of Wezel et al. [10, 11], who found no substantial heating around retainer wires of up to 47 mm length when scanning within SAR guidelines for the head. Additionally, all implants were rather small with respect to the wavelength and located in or near non-critical tissue known to have many highly sensitive thermoreceptors. In all cases a magnetization-prepared rapid gradient-echo (MPRAGE) sequence was used with imaging parameters described by, e.g., Wrede et al. [48], while the remaining imaging protocol included other MRI sequences depending on the scope of the study such as time-of-flight (TOF), susceptibility weighted imaging (SWI), two dimensional (2D) and three dimensional (3D) echo planar imaging (EPI), fast low angle shot (FLASH), and turbo spin echo (TSE). The MPRAGE sequence applied approximately 45 % of the allowed SAR (head local SAR limit: 10 W/Kg) with an acquisition time of 6 min. In several cases, directly comparable imaging was performed at 1.5 or 3 T using a combined head/neck receive array coil (Siemens Healthcare, Erlangen, Germany). Table 3 summarizes the data of the subjects with dental implants.
Other implants
A total of 42 subjects with miscellaneous implants underwent imaging: 22 subjects presented with orthopedic implants, 2 with vascular prostheses, 1 with an implanted port, 1 subject with surgical clips, 15 with intrauterine devices (IUD), and 2 with infusion pumps. One subject appeared with both an orthopedic implant and an intrauterine device. Details are summarized in Tables 4 and 5. MPRAGE was again the most common sequence used in the examinations, with other MRI sequences used depending on the scope of the study.
Exposure scenario used to determine potential SAR elevations near a generic hip implant during a head examination with a custom-built 8-channel transceiver meander stripline head coil [63]. The total input power was scaled so that the maximum local 10 g-averaged SAR, which is located in the head, reached the IEC limit of 10 W/kg [65]. a Heterogeneous male body model (Duke) with the generic implant at the right hip. b The 10 g-averaged SAR distribution. No significant SAR elevation occurred near the generic hip implant. SAR levels at the implant were at least 100 times lower compared to the SAR generated in the head region
Exposure scenario used to determine potential SAR elevations near an implantable port when exciting with a custom-built 8-channel transceiver meander stripline body coil [49] placed around the pelvis of a heterogeneous male model (Duke). b Local SAR distribution (10 g-averaged) obtained with an FDTD numerical solver (CST Microwave Studio, CST GmbH, Germany) in a slice containing the implantable port. Although SAR elevations are present at the port, the local SAR values are a factor of 100 lower compared to the local SAR generated by the RF coil alone in the pelvic region
Tattoos and permanent make-up
One hundred and eight (108) volunteers with one or multiple tattoos underwent 7 T imaging. One subject with permanent make-up at the eyebrows was cleared for imaging at 7 T. Of the 108 subjects with tattoos, 2 had them directly in the exposure volume of the transmit coil and 24 had them close to but not directly within the exposure volume; i.e. the tattoo was at the shoulder while the subject underwent a head exam. Eighty-two had their tattoos at least 30 cm away from the RF coil. All subjects were questioned regarding the origin of the tattoo and, if possible, regarding the composition of the ink. The two tattoos located directly in the exposure volume of the transmit coil were both at the lower part of the back and were imaged with a custom-built 8-channel transceiver stripline body coil [49]. Figure 6a shows one of the tattoos. For the 24 tattoos located less than 30 cm away from the exposure volume of the transmit coil, only head scans were performed. The orange part of Fig. 1b shows the location of these tattoos. Nine of these were located on the upper part of the back, 14 on the shoulder, and 1 on the upper part of the chest. All tattoos were drawn in Germany and one in Thailand, the largest having a maximum size of roughly 10 cm by 40 cm, as shown in Fig. 6b. Since the subject with the tattoo drawn in Thailand had been imaged at 1.5 and 3 T several times without any side effects, the subject was cleared for imaging at 7 T. Fig. 6c–e show three other examples of tattoos close to the exposure volume of the transmit coil. Eight subjects were scanned with an 8-channel head coil (P-H08L-070-00114, Rapid Biomed, Rimpar, Germany). Fifteen subjects were scanned with a birdcage transmit and 32-channel receive head coil (Nova Medical, Wilmington, MA, USA) The final two subjects were scanned with a quadrature birdcage head coil (Invivo Corp., Gainesville, FL, USA). One subject was scanned with both birdcage head coils (CP transmit/receive quadrature birdcage from Invivo Corp. and birdcage transmit head coil with 32-channel receive from Nova Medical).The subject with permanent make-up at the eyebrows underwent a liver examination using the custom-built 8-channel transceiver stripline body coil [49]. Although this subject was not cleared for a head scan at 7 T because of the known presence of high levels of iron oxide (typically between 7 and 25 %) in the pigment of the permanent make-up, clearance was given for the abdominal scan. All scans were performed using the described local transmit/receive RF coils. While all head scans were performed with standard circular polarization (CP+), static RF shimming was applied in examinations with the 8-channel meander stripline body coil.
a Tattoo located at the lower part of the back, drawn in Germany in 2003 and composed of black and blue ink. It was directly in the exposure volume of the transmit coil and imaged with a custom-built 8-channel transmit/receive meander stripline body coil. b–e Four examples of tattoos close to the examination exposure volume of the transmit coil (orange zone according to Fig. 1b). The tattoo shown in b was drawn in Germany and had a width of approx. 25 cm. Tattoos shown in c–e were drawn in Germany. Examinations were performed with head coils for the latter four tattoos
Results
None of the subjects reported sensations of heat or force during or after imaging, nor regarding discomfort related to the implants or tattoos. For the metallic implants located within the imaging volume, artifacts were clearly visible in the 7 T images, but these remained restricted to the direct vicinity of the implants and did not affect image quality in the areas of interest. Table 6 gives an overview of the results obtained in this study.
Dental implants
Example artifacts due to metallic dental implants close to the imaging area of interest are shown in Figs. 7 and 8.
Comparison of MPRAGE images obtained at 1.5 and 7 T in a healthy volunteer (m, 38y) with a retainer wire behind the teeth. Both sequences were measured with 1-mm isotropic resolution and similar parameters (1.5 T: echo time (TE) 3.6 ms, bandwidth (BW) 360 Hz/pixel; 7 T: 2.0 ms, BW 210 Hz/pixel). Signal loss and incomplete inversion are visible. Subsequent SWI and EPI scans with focus on the cerebellum remained unaffected by the wire. At 7 T, the 32-ch coil (Nova Medical) was used. Note Window-leveling was adjusted to better demonstrate artifacts from the retainer wire
Images of a volunteer (f, 53y) with dental implants on the right and left side of her jaw. Strong signal loss around the implants is visible in the 7 T 3D-FLASH image (a), correlating well with a CT image of the patient (b). In c, the 7 T TOF angiography of the subject’s aneurysm (arrow) remained artifact-free. The 7 T images were obtained with an 8-ch head coil (Rapid Biomed)
Other implants
Artifacts were clearly visible for one subject with two titanium endobuttons in the knee area, as shown in Fig. 9a. In Fig. 9b, the artifacts associated with the two endobuttons are clearly visible in a corresponding CT image. For the subject with a polymer screw, no artifacts close to the screw were visible and the implant was clearly identifiable, as shown in Fig. 9c.
a, b Images obtained in a subject (m, 36 years) with two titanium endobuttons for the reconstruction of the ACL. Signal loss is clearly visible in the 7 T proton density (PD)-weighted turbo spin echo sequence (a, arrow). A corresponding CT image is given in (b). Endobuttons are clearly visible (arrows). c 3D-FLASH image obtained at 7 T in a patient (f, 25y) with a bioabsorbable polymer screw. The gradient echo sequence was measured with 1-mm isotropic resolution, TE 3.1 ms, and BW 200 Hz/pixel. The screw is clearly visible (arrow)
Tattoos
No reddening was visible in the region of the tattoos subsequent to imaging.
Discussion
Since no dedicated safety tests for 7 T are recommended in current standards, careful attention was paid to obtain the fullest possible information about implants. Important for the decision-making process was the American Society for Testing and Materials (ASTM) classification which includes "MR Safe", "MR Conditional" and "MR Unsafe" labeling [13] based on four tests (force, torque, RF heating, and artifacts) [50–53]. Implants outside the exposure volume of the RF coil were required to have "MR Conditional" labeling at 1.5 or 3 T, as the gradient systems utilized at 7 T are similar in maximum gradient strength and slew rate compared to the gradients at lower field strengths. A conditionality regarding the SAR could be neglected if a sufficient distance between the RF exposure volume and implant was retained, as only local transmit RF coils were used at 7 T. Of course, implants were required to exhibit no significant forces or torques from the static magnetic field. Here, it may be noted that, due to lower gradients in the stray field, a passively shielded 7 T magnet yields similar forces compared to an actively shielded, state-of-the-art, short-bore 3 T magnet. Labeling information may, for example, be gained from specific websites [54, 55] or directly from the website of the implant manufacturer. In general, few implants have already been labeled "MR Conditional" at 7 T by utilizing ASTM standards [55]. Furthermore, as in all MR examinations, communication with the subjects should be maintained to enable them to indicate any trouble or discomfort during the scan. Also, an intensive interview with the subjects prior to the scans is highly recommended to identify all implants and their type. All implants scanned at our institution were either made of non-ferromagnetic material, mostly titanium, or made of non-metallic and non-conductive material, such as biopolymer screws. Titanium is a biocompatible material and has a low magnetic susceptibility (χ ≈ 182 × 10−6) [56] and is, therefore, an advantageous material for MRI. Forces and torques on implants as a consequence of the strong static magnetic field are significantly reduced with low magnetic susceptibility (diamagnetic and paramagnetic materials). A total-knee prosthesis was made of zirconium (also a non-ferromagnetic material), and a total-hip prosthesis was made of a cobalt-chrome-molybdenum (CoCrMo) alloy already tested "MR Conditional" at 3 T. For this implant, restrictions of the "MR Conditional" labeling regarding RF exposure with a transmit body coil were not applicable for the 7 T scans, where a distance of more than 30 cm was retained between the implant and local transmit head coil. Similarly, copper (IUD) and nitinol (stents) were also permitted to be exposed to the static magnetic field but not to be within the direct exposure volume of the RF coil. During the screening interview and prior to the research scan at 7 T, women with IUD were advised to see a gynecologist to ensure sufficient contraceptive protection after the 7 T scan. However, force measurements performed by Rauschenberger et al. [57] showed no deflection and no torque at 3 or 7 T for copper IUD. For the 2 volunteers with stents who were imaged with head coils, 1 had his stent in the femoral artery and the other reported 2 stents, 1 Y stent for repair of the abdominal bifurcation (more than 30 cm from the exposure of the transmit coil) and 1 coronary stent located 15 cm from the exposure volume of the coil. The latter was cleared for 7 T based on a study of Santoro et al. [8] and after evaluation of detailed implant information and previously obtained CT images that showed the exact location and dimension of the stent, as well as that only a single and not multiple stents had been used. It should be mentioned that some stents may be made of stainless steel [58] and should, therefore, to be excluded from any scan at 7 T. Some dental implants, such as retainer wires, are also suspected to contain magnetic stainless steel and, hence, to produce measurable displacement forces in the testing, according to the ASTM [59]. However, general experience with dental implant scanning shows a safe history even if some dental implants are made of ferromagnetic materials. In the group of subjects presented here, retainer wires that form closed loops were excluded from imaging at 7 T, and only straight wires up to 47 mm length were cleared. Implants made of non-metallic materials such as the Mirena and Nuvaring IUD and Teflon needles (MiniMed Paradigm Pumps, Model 512, Medtronic) were not expected to generate any force or torque. For the infusion pumps, particular vigilance was observed in determining the needle material, since some needle material may be metallic [60]. RF field interactions with potentially metallic compositions of tattoo ink were considered to be unlikely under the condition that the tattoos were located outside the exposure volume of the transmit coil. Image artifacts were clearly visible at 7 T, especially for dental implants. However, the artifacts remained localized to the vicinity of the implants and did not impair the quality in the imaging areas of interest (Figs. 7, 8).
Conclusion
In conclusion, our initial experience at 7 T indicates that an overly conservative exclusion of all subjects with implants and/or tattoos from 7 T examinations is not warranted. Nevertheless, imaging should only be performed in carefully selected subjects after acquiring substantial information to enable a proper risk assessment.
References
Ladd ME, Bock M (2013) Problems and chances of high field magnetic resonance imaging. Radiologe 53(5):401–410
Moser E, Stahlberg F, Ladd ME, Trattnig S (2012) 7-T MR-from research to clinical applications? NMR Biomed 25(5):695–716
Kollia K, Maderwald S, Putzki N, Schlamann M, Theysohn JM, Kraff O, Ladd ME, Forsting M, Wanke I (2009) First clinical study on ultra-high-field MR imaging in patients with multiple sclerosis: comparison of 1.5 T and 7 T. Am. J Neuroradiol 30(4):699–702
Krug R, Carballido-Gamio J, Banerjee S, Burghardt AJ, Link TM, Majumdar S (2008) In vivo ultra-high-field magnetic resonance imaging of trabecular bone microarchitecture at 7 T. J Magn Reson Imag 27(4):854–859
Nakada T, Matsuzawa H, Igarashi H, Fujii Y, Kwee IL (2008) In vivo visualization of senile-plaque-like pathology in Alzheimer’s disease patients by MR microscopy on a 7 T system. J Neuroimaging 18(2):125–129
Pfeuffer J, Adriany G, Shmuel A, Yacoub E, Van De Moortele PF, Hu X, Ugurbil K (2002) Perfusion-based high-resolution functional imaging in the human brain at 7 Tesla. Magn Reson Med 47(5):903–911
Sammet CL, Yang X, Wassenaar PA, Bourekas EC, Yuh BA, Shellock F, Sammet S, Knopp MV (2013) RF-related heating assessment of extracranial neurosurgical implants at 7 T. Magn Reson Imag 31(6):1029–1034
Santoro D, Winter L, Muller A, Vogt J, Renz W, Ozerdem C, Grassl A, Tkachenko V, Schulz-Menger J, Niendorf T (2012) Detailing radio frequency heating induced by coronary stents: a 7.0 Tesla magnetic resonance study. PLoS ONE 7(11):e49963
Kraff O, Wrede KH, Schoemberg T, Dammann P, Noureddine Y, Orzada S, Ladd ME, Bitz AK (2013) MR safety assessment of potential RF heating from cranial fixation plates at 7 T. Med Phys 40(4):042302
Wezel J (2012) Assessing the MR compatibility of dental retainer wires at 7 Tesla, MSc Thesis, Delft University of Technology. http://repository.tudelft.nl/view/ir/uuid%3Aba429538-dd04-4229-adb7-8a6c249172a9/. Accessed 26 July 2015
Wezel J, Kooij BJ, Webb AG (2014) Assessing the MR compatibility of dental retainer wires at 7 Tesla. Magn Reson Med 72(4):1191–1198
Van der Berg CA, Van Osch MJ (2013) ISMRM scientific workshop, ultra high field MRI: What is in Full bloom and what is sprouting? Oral session 6 ultra high field safety and poster session 1: safety of implants at 7 T. Noordwijk aan Zee, The Netherlands
Standard Practice for Marking Medical Devices and Other Items for Safety in the MR Environment (2013). ASTM F2503-13
Hasgall PA, Neufeld E, Gosselin MC, Klingenböck A, Kuster N (2014) Hasgall PA, Neufeld E, Gosselin MC, Klingenböck A, Kuster N (August 1, 2014) IT’IS Database for thermal and electromagnetic parameters of biological tissues, Version 2.5. www.itis.ethz.ch/database. Accessed 26 July 2015
Armenean C, Perrin E, Armenean M, Beuf O, Pilleul F, Saint-Jalmes H (2004) RF-induced temperature elevation along metallic wires in clinical magnetic resonance imaging: influence of diameter and length. Magn Reson Med 52(5):1200–1206
Van Lier AL, Kotte AN, Raaymakers BW, Lagendijk JJ, van den Berg CA (2012) Radiofrequency heating induced by 7 T head MRI: thermal assessment using discrete vasculature or Pennes’ bioheat equation. J Magn Reson Imag 35(4):795–803
Ibrahim TS, Tang L, Kangarlu A, Abraham R (2007) Electromagnetic and modeling analyses of an implanted device at 3 and 7 Tesla. J Magn Reson Imag 26(5):1362–1367
Winter L, Oberacker E, Ozerdem C, Ji Y, von Knobelsdorff-Brenkenhoff F, Weidemann G, Ittermann B, Seifert F, Niendorf T (2014) On the RF heating of coronary stents at 7.0 Tesla MRI. Magn Reson Med. doi:10.1002/mrm25483
Van de Moortele PF, Akgun C, Adriany G, Moeller S, Ritter J, Collins CM, Smith MB, Vaughan JT, Ugurbil K (2005) B(1) destructive interferences and spatial phase patterns at 7 T with a head transceiver array coil. Magn Reson Med 54(6):1503–1518
Ibrahim TS, Lee R, Baertlein BA, Abduljalil AM, Zhu H, Robitaille PM (2001) Effect of RF coil excitation on field inhomogeneity at ultra high fields: a field optimized TEM resonator. Magn Reson Imag 19(10):1339–1347
Katscher U, Bornert P, Leussler C, van den Brink JS (2003) Transmit SENSE. Magn Reson Med 49(1):144–150
van den Bergen B, van den Berg CA, Klomp DW, Lagendijk JJ (2009) SAR and power implications of different RF shimming strategies in the pelvis for 7 T MRI. J Magn Reson Imag 30(1):194–202
Gegauff AG, Laurell KA, Thavendrarajah A, Rosenstiel SF (1990) A potential MRI hazard: forces on dental magnet keepers. J Oral Rehabil 17(5):403–410
Costa AL, Appenzeller S, Yasuda CL, Pereira FR, Zanardi VA, Cendes F (2009) Artifacts in brain magnetic resonance imaging due to metallic dental objects. Med Oral Patol Oral Cir Bucal 14(6):E278–E282
Destine D, Mizutani H, Igarashi Y (2008) Metallic artifacts in MRI caused by dental alloys and magnetic keeper. Nihon Hotetsu Shika Gakkai zasshi 52(2):205–210
Hubalkova H, La Serna P, Linetskiy I, Dostalova T (2006) Dental alloys and magnetic resonance imaging. Int Dent J 56(3):135–141
Zho SY, Kim MO, Lee KW, Kim DH (2013) Artifact reduction from metallic dental materials in T1-weighted spin-echo imaging at 3.0 tesla. J Magn Reson Imag 37(2):471–478
U.S. FDA Cosmetics (2012), Tattoos and permanent makeup. http://www.fda.gov/Cosmetics/ProductsIngredients/Products/ucm108530.htm. Accessed 26 July 2015
Timko AL, Miller CH, Johnson FB, Ross E (2001) In vitro quantitative chemical analysis of tattoo pigments. Arch Dermatol 137(2):143–147
Abiona TC, Balogun JA, Adefuye AS, Sloan PE (2010) Body art practices among inmates: implications for transmission of bloodborne infections. Am J Infect Control 38(2):121–129
Franiel T, Schmidt S, Klingebiel R (2006) First-degree burns on MRI due to nonferrous tattoos. Am J Roentgenol 187(5):W556
Klitscher D, Blum J, Kreitner KF, Rommens PM (2005) MRT-induced burns in tattooed patients. Case report of an traumatic surgery patient. Unfallchirurg 108(5):410–414
Offret H, Offret M, Labetoulle M, Offret O (2009) Permanent cosmetics and magnetic resonance imaging. J Fr Ophtalmol 32(2):e131–e133
Ratnapalan S, Greenberg M, Armstrong D (2004) Tattoos and MRI. Am J Roentgenol 183(2):541
Ross JR, Matava MJ (2011) Tattoo-induced skin “burn” during magnetic resonance imaging in a professional football player: a case report. Sports health 3(5):431–434
Vahlensieck M (2000) Tattoo-related cutaneous inflammation (burn grade I) in a mid-field MR scanner. Eur Radiol 10(1):197
Wagle WA, Smith M (2000) Tattoo-induced skin burn during MR imaging. Am J Roentgenol 174(6):1795
Wagner M, Lanfermann H, Zanella F (2006) MR-induced burn-reaction in a female patient with “permanent make-up”. RoFo 178(7):728–730
Kanal E, Shellock FG (1998) MRI interaction with tattoo pigments. Plast Reconstr Surg 101(4):1150–1151
Kreidstein ML, Giguere D, Freiberg A (1997) MRI interaction with tattoo pigments: case report, pathophysiology, and management. Plast Reconstr Surg 99(6):1717–1720
Tope WD, Shellock FG (2002) Magnetic resonance imaging and permanent cosmetics (tattoos): survey of complications and adverse events. J Magn Reson Imag 15(2):180–184
Christ A, Kainz W, Hahn EG, Honegger K, Zefferer M, Neufeld E, Rascher W, Janka R, Bautz W, Chen J, Kiefer B, Schmitt P, Hollenbach HP, Shen J, Oberle M, Szczerba D, Kam A, Guag JW, Kuster N (2010) The Virtual Family–development of surface-based anatomical models of two adults and two children for dosimetric simulations. Phys Med Biol 55(2):N23–N38
Murbach M, Neufeld E, Kainz W, Pruessmann KP, Kuster N (2014) Whole-body and local RF absorption in human models as a function of anatomy and position within 1.5 T MR body coil. Magn Reson Med 71(2):839–845
Yeo DT, Wang Z, Loew W, Vogel MW, Hancu I (2011) Local specific absorption rate in high-pass birdcage and transverse electromagnetic body coils for multiple human body models in clinical landmark positions at 3 T. J Magn Reson Imag 33(5):1209–1217
Council of Europe, Resolution ResAP (2003) 2 on tattoos and permanent make-up. https://wcd.coe.int/ViewDoc.jsp?id=45869. Accessed 26 July 2015
Council of Europe, Resolution ResAP (2008) 1 on requirements and criteria for the safety of tattoos and permanent make-up. http://www.coe.int/t/e/social_cohesion/soc-sp/ResAP_2008_1%20E.pdf. Accessed 26 July 2015
Bericht des BfR über die 60. Sitzung der Kosmetik-Kommission (2000). http://www.bfr.bund.de/cm/206/kokobericht_60.pdf. Accessed 26 July 2015
Wrede KH, Dammann P, Monninghoff C, Johst S, Maderwald S, Sandalcioglu IE, Muller O, Ozkan N, Ladd ME, Forsting M, Schlamann MU, Sure U, Umutlu L (2014) Non-enhanced MR imaging of cerebral aneurysms: 7 Tesla versus 1.5 Tesla. PLoS ONE 9(1):e84562
Orzada S, Quick H, Ladd ME, Bahr A, Bolz T, Yazdanbakhsh P, Solbach K, Bitz AK (2009) A flexible 8-channel transmit/receive body coil for 7 T human imaging. In: Proceedings of the 17th scientific meeting, International Society for Magnetic Resonance in Medicine, Honululu, p 2999
Standard Test Method for Measurement of Magnetically Induced Displacement Force on Medical Devices in the Magnetic Resonance Environment (2006). ASTM F2052-06e1
Standard Test Method for Measurement of Magnetically Induced Torque on Passive Implants in the Magnetic Resonance Environment (2006). ASTM F2213-06
Standard Test Method for Measurement of Radio Frequency Induced Heating near Passive Implants During Magnetic Resonance Imaging (2011). ASTM F2182-11a
Standard Test Method for Evaluation of MR Image Artifacts from Passive Implants (2007). ASTM F2119-07
Online Database for MR safety information MagResource LLC (2015). www.magresource.com/www.magresource.eu. Accessed 26 July 2015
Shellock FG (2015) Reference manual for MR-safety, implants and devices, 2015 Th edn. Biomedical Publishing Group, Los Angeles
Schenck JF (1996) The role of magnetic susceptibility in magnetic resonance imaging: MRI magnetic compatibility of the first and second kinds. Med Phys 23(6):815–850
Rauschenberg J, Groebner J, Semmler W, Bock M (2011) How safe are intrauterine devices at MRI procedures with field strength beyond 1.5 T?. In: Proceedings of the 19th scientific meeting, International Society for Magnetic Resonance in Medicine, Montreal, p 1793
Taal BG, Muller SH, Boot H, Koops W (1997) Potential risks and artifacts of magnetic resonance imaging of self-expandable esophageal stents. Gastrointest Endosc 46(5):424–429
Shellock FG, Crues JV (1988) High-field-strength MR imaging and metallic biomedical implants: an ex vivo evaluation of deflection forces. Am J Roentgenol 151(2):389–392
Medtronic, Inc. (2015). http://www.medtronic-diabetes-me.com/polyfin.html. Accessed 26 July 2015
Brunner DO, De Zanche N, Frohlich J, Paska J, Pruessmann KP (2009) Travelling-wave nuclear magnetic resonance. Nature 457(7232):994–998
Rietsch S, Quick H, Orzada S (2015) Impact of different meander sizes on the RF transmit performance and coupling of microstrip line elements at 7 T. Med Phys 42(8):4542–4552
Orzada S, Kraff O, Schäfer L, Brote I, Bahr A, Bolz T, Maderwald S, Ladd ME, Bitz AK (2009) 8-Channel Transmit/receive Head Coil for 7 T human imaging using intrinsically decoupled strip line elements with meanders. In: Proceedings of the 17th scientific meeting, International Society for Magnetic Resonance in Medicine, Honululu, p 3010
Bitz AK, Kraff O, Orzada S, Herrmann T, Mallow J, Bernarding J, Ladd ME (2014) RF safety evaluation of different configurations of high-permittivity pads used to improve imaging of the cerebellum at 7 Tesla. In: Proceedings of the 22nd scientific meeting, International Society for Magnetic Resonance in Medicine, Milan, p 4892
International Electrotechnical Commission (2010) Medical electrical equipment Part 2-33: Particular requirements for the safety of magnetic resonance diagnostic devices. IEC 60601-2-33:2010
Acknowledgments
Funding within the Integrated Interventional Imaging Operating System (IIIOS) Project was received from the European Community’s Seventh Framework Programme (FP7/2007–2013) under Grant Agreement no. 238802.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MR:comp GmbH provided support in the form of salaries for authors Yacine Noureddine and Gregor Schaefers.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Rights and permissions
About this article
Cite this article
Noureddine, Y., Bitz, A.K., Ladd, M.E. et al. Experience with magnetic resonance imaging of human subjects with passive implants and tattoos at 7 T: a retrospective study. Magn Reson Mater Phy 28, 577–590 (2015). https://doi.org/10.1007/s10334-015-0499-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-015-0499-y