Abstract
Blood-oxygenation-level-dependent (BOLD) contrast in magnetic resonance (MR) imaging of skeletal muscle mainly depends on changes of oxygen saturation in the microcirculation. In recent years, an increasing number of studies have evaluated the clinical relevance of skeletal muscle BOLD MR imaging in vascular diseases, such as peripheral arterial occlusive disease, diabetes mellitus, and chronic compartment syndrome. BOLD imaging combines the advantages of MR imaging, i.e., high spatial resolution, no exposure to ionizing radiation, with functional information of local microvascular perfusion. Due to intrinsic contrast provoked via changes in hemoglobin oxygen saturation, it is a safe and easy applicable procedure on standard whole-body MR devices. Therefore, BOLD MR imaging of skeletal muscle is a potential new diagnostic tool in the clinical evaluation of vascular, inflammatory, and muscular pathologies. Our review focuses on the current evidence concerning the use of BOLD MR imaging of skeletal muscle under pathological conditions and highlights ways for future clinical and scientific applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Blood-oxygenation-level-dependent (BOLD) magnetic resonance imaging (MRI) was introduced in functional neuroimaging studies in 1990 [1]. Since that time, BOLD MRI has become the mainstay for analyzing activated neuronal tissues. Neuronal activation induces changes of the ratio between oxy- and deoxyhemoglobin concentration in the local microcirculation [2]. Oxygen saturation influences T2* signal intensity (SI) in gradient echo MRI sequences. According to experimental setup and MR sequence selection, other confounding variables, such as inflow, blood volume, and extravascular contributions, are reduced to a large extent. The correlation between T2/T2* SI and blood oxygen concentration made BOLD MRI the ideal diagnostic tool for functional neuroanatomical studies and clinical applications, such as neurosurgical planning and monitoring of treatment outcomes.
In the 1990s, BOLD MRI was also evaluated as a diagnostic tool in other human tissues. Myocardial infarction has been shown to create a significantly reduced BOLD response in damaged muscle tissue [3]. The same study also demonstrated that BOLD SI changes are reversible after coronary intervention via percutaneous transluminal angioplasty. Rest and stress-induced BOLD MRI also differentiated successfully between ischemic, nonischemic, and normal myocardial segments in a population of patients with coronary artery disease [4]. Besides myocardial pathologies, BOLD MRI is valuable for investigating physiological blood oxygenation level changes in the human kidney and uterine myometrium [5, 6]. As human tumors tissues are often characterized by increased oxygen consumption leading to hypoxic conditions and neoangiogenesis, BOLD MRI could also be a valuable tool for functional tumor imaging. However, in breast and prostate cancer, BOLD measurements showed heterogeneous results with respect to extent of hypoxia prior to chemotherapy, most likely due to differing tumor neovascularization and stroma tissue [7, 8].
Concerning MRI of the musculoskeletal system, BOLD MRI has been extensively studied in recent years because of the easy accessibility of human skeletal muscle to different kinds of imaging paradigms (i.e., exercise- and cuff compression paradigms that allow generation of ischemic and hyperemic conditions) and the great variation of perfusion strength between resting and activation state. As BOLD MRI relies on hemoglobin oxygen saturation as endogenous contrast, one has to provoke changes in the local ratio of oxy- and deoxyhemoglobin prior to MRI. The musculoskeletal system permits several different imaging paradigms to shift the tissue oxygenation level: Oxygen delivery to skeletal muscle can be increased via increased oxygen inhalation or vasodilator drugs and decreased via temporal vascular occlusion or vasoconstrictors. Oxygen consumption can be increased via muscular exercise. By using these experimental setups, a large number of studies has focused on the origin of skeletal muscle BOLD signal and its physiological dependencies. This information is helpful for interpreting results of clinical muscle BOLD MRI studies. As skeletal muscle is the end organ of the peripheral vascular system, BOLD MRI provides important information of vascular pathologies, such as peripheral arterial occlusive disease, diabetes mellitus, and rheumatic diseases.
In this review, we focus on the clinical implications of skeletal muscle BOLD MRI. We highlight current evidence concerning the diagnostic application of functional MRI of the skeletal muscle and discuss recent and future developments. After a short overview of the theory behind skeletal muscle BOLD effect, the technical principles of the procedure are reviewed in detail with a focus on the current interpretation of skeletal muscle BOLD signal.
The BOLD effect
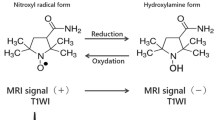
Functional MRI is based on the principle that transverse relaxation rate of water protons inside or in the vicinity of small blood vessels is influenced by the oxygenation status of hemoglobin [1]. Oxyhemoglobin concentration in the microvascular environment of a certain tissue is mainly influenced by blood flow, intravascular volume, and capillary oxygen extraction. A sole increase of tissue perfusion with oxygenated hemoglobin at constant levels of oxygen extraction results in a higher oxy- and lower deoxyhemoglobin concentration in the local microcirculation and small venous vessels [9–11]. Deoxyhemoglobin is paramagnetic and thus causes local magnetic field distortions in its vicinity. At conditions of increased tissue perfusion, the lower local deoxyhemoglobin content leads to a decrease of the apparent transverse relaxation rate (1/T2) of water protons and an increase of T2 and T2* signal through a reduced intravoxel spin dephasing (i.e., positive BOLD contrast) [1, 9]. Due to a phase dispersion of water proton signals, GRE MRI sequences emphasize this effect [9, 12].
Different physiological parameters have been postulated to influence skeletal muscle BOLD signal, such as blood flow, intravascular blood volume, cellular pH and fluid shifts, vessel diameter, and orientation. However, it is generally accepted that the bulk of BOLD signal alterations in GRE sequences of skeletal muscles are due to the oxygenation level of hemoglobin [10, 13–21]. Regarding macro- and microvascular tissue blood flow, good correlations with the muscular BOLD signal have been found in various studies using different paradigms to provoke BOLD responses and different techniques for flow measurements such as plethysmography, arterial spin labelling, and laser Doppler flowmetry [14, 17, 22–24]. The relative extent of other factors contributing to BOLD contrast depends on the imaging protocol. Alterations of blood volume, for example, can lead to changes in T2* signal [23]. According to a recent study using short isometric muscle contractions to provoke BOLD SI changes in the calf muscles, these changes depend on the oxygenation status of hemoglobin [24]. Thus, if blood oxygen saturation is at high levels, near 100%, an increase of blood volume in the leg will cause an increase of T2/T2*, whereas a low oxygen saturation of about 50% results in a T2* decrease. Furthermore, two studies found a prolongation of the BOLD signal increase after increased muscular blood flow had normalized [25, 26]. This could be explained by increased oxygen saturation of venous blood and increased tissue oxygen tension. Exercise-induced osmotic changes of the intracellular milieu (i.e., water shift from the circulation to the intracellular space) could also alternate the T2 signal from muscle tissue [27]. However, metabolic changes during ischemia, such as increasing lactate or phosphate concentration or pH-decrease, have been reported to occur later than usually measured BOLD signal changes [28]. Additionally, vessel orientation has been proposed to influence muscle BOLD signal, as most capillaries and small vessels are oriented along the axis of the muscle fibers and thus have a determined orientation inside the static magnetic field [29]. However, a study using a leg rotation protocol found no influence on BOLD signal in an arterial occlusion paradigm [15]. Primarily due to secondary alterations of the variables and mechanisms discussed above, physiological parameters of the imaged person such as age, training state, and intake of vasoactive drugs can have impact on BOLD signal [26, 30–32].
Scientific evidence supports the fact that the BOLD signal of skeletal muscle is influenced by different factors which are—to a certain extent—paradigm dependent. However, using optimized GRE MRI sequences and experimental conditions, muscle BOLD signal reflects changes of hemoglobin oxygenation in muscle microvessels that primarily depend on perfusion and oxygen consumption. As muscle tissue is the end organ of the limb vasculature, BOLD MRI is a promising noninvasive imaging method for functional evaluation of diseases affecting peripheral macro- and microvasculature. The following section describes methodological principles that are usually applied in muscle BOLD studies. Several of these principals are necessary to measure true BOLD effects and reduce the influence of confounding parameters.
Principles of skeletal muscle BOLD MRI
Patient selection
BOLD MRI of skeletal muscle can be a valuable diagnostic tool under many different clinical conditions that impair peripheral vasculature and thus result in a reduced oxygen delivery to skeletal muscle [14, 33–35]. Patients undergoing muscle BOLD imaging therefore usually bear cardiovascular risk factors, such as hypertension, smoking, hypercholesterolemia, diabetes mellitus, and obesity. In diagnostic studies comprising a patient and control group, both groups must be controlled for these confounding variables. Moreover, patient age and training state influence skeletal muscle BOLD signal [24, 25, 30, 31, 36]. To date, there is no literature concerning muscle BOLD signal under inflammatory vascular or skeletal muscle diseases, but—as an influence on tissue oxygenation and perfusion cannot ruled out—one should also control for these disorders. Further exclusion criteria for muscle BOLD studies are typical contraindications of MRI examination, e.g., claustrophobia and ferromagnetic implants.
Experimental setup
BOLD MRI of human skeletal muscle is usually performed in a whole-body MRI device that, in principle, allows imaging of every muscle within the patient’s body; however, according to typical clinical questions, routinely, arm or leg muscles are examined [11, 17, 26, 37]. The extremity is placed within a vascular array coil, and foam braces can be used to minimize motion artifacts in exercise paradigms [22]. Prior to imaging, a resting period of 5–15 min of the examined individual is required due to the influence of position changes on the venous filling state and functional vascular adaptations that have been shown to influence BOLD SI [23]. To evoke changes in the local hemoglobin oxygen saturation that correspond to voxel contrastation in T2/T2* MRI sequences, typically, one of the following paradigms is applied: (1) arterial occlusion; (2) muscle exercise; (3) oxygen inhalation.
-
1.
Arterial occlusion has been widely used in a variety of muscle BOLD studies [10, 11, 13, 14, 23, 30, 38]. It requires an easily applicable experimental setup with a standard air cuff wrapped around the proximal part of the examined extremity (Fig. 1a). If the pressure manometer contains ferromagnetic parts, a safe distance from the magnet should be achieved by using an extended tube [30]. Ischemia is achieved by fast inflation of the cuff to an occlusion pressure at least 50 mmHg above the individual brachial systolic blood pressure [14, 30, 33, 36, 38–40]. Extensive arterial calcification will make higher cuff pressures necessary, especially in patients with diabetes. Fast inflation is necessary to prevent immoderate filling of the venous system. This can be achieved via automatic cuff inflation systems or fast manual inflation. However, manual inflation lasts over several cardiac cycles and thus could lead to increased venous filling. Applied cuff pressure and duration of ischemic phase is always a compromise between patient compliance, degree of discomfort and pain, possible complications, and assumed optimal muscle BOLD effect (also refer to “Paradigm selection in clinical settings” below). MRI measurements can be started during resting state, ischemic phase, or after cuff deflation, i.e., during reactive hyperemia phase. Besides sustaining suprasystolic cuff compression in the examined leg, this paradigm is mostly independent from patient compliance. However, in patients with critical leg ischemia or ulcerations, BOLD MRI examination via cuff compression should be considered with caution due to massive pain or even worsening of the clinical condition.
Fig. 1 a Experimental setup of the widely used cuff compression paradigm in skeletal muscle blood-oxygenation-level-dependent (BOLD) magnetic resonance imaging (MRI). Inflation of a standard air cuff at midthigh level allows BOLD examination of the calf microvasculature during ischemia and reactive hyperemia. In T2* maps calculated from echo planar imaging (EPI) data, regions of interest (ROIs) are usually positioned at the maximal calf muscle diameter. Areas with larger vessels are excluded. As T2* images offer a low spatial resolution, T1-weighted images of the corresponding calf region are concomitantly acquired for anatomical reference. b Extracted T2* (BOLD) time course of a healthy 46-year old woman volunteer with a 60-s resting period, 6 min of ischemia, and 6 min of reactive hyperemia
In healthy individuals, a fast T2* signal decay is observed at the beginning of ischemia, followed by a slower decrease (Fig. 1b) [13, 14, 38]. During reactive hyperemia, a fast surge in BOLD signal is observed with peak values after approximately 30–60 s and a subsequent decrease to a steady state value around baseline [30, 33]. The extent of BOLD signal changes depends on experimental setup, physiological variables of the examined patient, and magnetic field strength [11, 13, 17]. To analyze muscle BOLD data in a quantitative manner, several time-course parameters can be calculated, including:
-
T2 *min or MIV: minimal T2* value in percent during ischemia;
-
T2 *max or HPV: maximal T2* value during reactive hyperemia;
-
Time to peak (TTP): time from cuff deflation to hyperemia T2* peaking;
-
Declining slope (DS): average decline of T2* curves during ischemia or reactive hyperemia.
-
2.
As skeletal muscle work results in local increases of blood flow due to local vasodilation triggered by the accumulation of metabolites, voluntary contractions of the imaged individual can be used to provoke a skeletal muscle BOLD response. Several studies showed that brief contractions of about 1–3 s are sufficient to produce a measurable BOLD response [17, 18, 25]. Motion artifacts are one major drawback in these studies, so that sophisticated fixation devices or foam braces need to be installed prior to imaging. Significant BOLD responses appear 8–15 s after individual muscle contractions [17, 18]. As contraction intensity is related to BOLD SI changes, this paradigm depends largely on patient compliance [22].
-
3.
By sequential inhalation of ambient air and 100% oxygen from a mask with a reservoir, BOLD response of skeletal muscle can be provoked by repeatedly increasing and decreasing blood oxygen content (O2-enhanced MRI) [10]. However, this kind of paradigm has some drawbacks that constrain its widespread use in scientific or clinical applications. As oxygen saturation of hemoglobin in healthy young individuals is near 100%, oxygen ventilation primarily leads to an increase of dissolved O2 in the blood, whereas the ratio between oxy- and deoxyhemoglobin does not change extensively. O2 is paramagnetic and leads to changes of T1, T2, and T2*. Studies using this paradigm therefore must be analyzed with care regarding true BOLD effects that depend on hemoglobin oxygenation. Furthermore, the paradigm has not been extensively evaluated with regard to how large the influence on true BOLD signal or perfusion is.
Muscle BOLD MRI needs high-speed image acquisition methods, typically based on echoplanar imaging (EPI) [41]. Spiral imaging techniques are more prone to image artifacts due to a higher sensitivity to off-resonance effects compared with EPI [42]. Water proton susceptibility differences depending on oxygen hemoglobin saturation are emphasized on gradient-echo MRI sequences [1, 12]. BOLD signal alterations of conventional single-shot EPI are sensitive to changes in T2* and T2—reflecting oxygenation—and initial BOLD signal intensity (S0) [30, 33]. S0 is influenced by several confounding parameters, such as blood inflow, changes in T1, and baseline drifts [16, 43]. Multiecho GRE EPI sequences with fat suppression can be used to separate oxygenation-related changes (T2*) from these other effects [16, 33]. EPIs are superposed to a corresponding T1-weighted spin-echo (SE) image of the same acquisition plane to allow exact placement of the region of interest (ROI) in a designated muscle (Fig. 1a).
Image analysis
Regarding image analysis, T2* sequences (multiecho acquisition) comprise the highest sensitivity for studying the true BOLD effect in skeletal muscle. In case of multiecho EPI, T2* maps are generated by using a pixel-by-pixel least-square fit of a monoexponential decay to the signal intensities of the different echo images [14, 30]. T2* values, normalized to a baseline value set to 100% (i.e., at resting state) can then be extracted for every examined ROI. Larger vessels should be excluded to minimize inflow artifacts. A BOLD time course can be calculated subsequently (Fig. 1b).
Peripheral arterial occlusive disease
Assessment and diagnosis
Peripheral arterial occlusive disease (PAOD) is one of the leading manifestations of atherosclerosis. Existence of this disease has a significant impact on the survival of patients with generalized atherosclerosis [44, 45]. Due to stenoses and occlusions in the macrovasculature, malperfusion of the distal tissues (skeletal muscle and skin) occurs [46]. Specifically, in the skeletal muscle, the process of atherosclerosis seems to lead to changes in microvessel architecture and composition of muscle fiber types [47–49]. These factors interact and may significantly reduce oxygen delivery to and alter oxygen consumption in the skeletal muscle microcirculation [10].
MR angiography (MRA) detects and localizes stenoses and occlusions on a macrovascular level but does not allow a statement about the function of the microvasculature in the distal tissues [50, 51]. The ankle brachial index (ABI) is an easily applicable but observer-dependent diagnostic tool to evaluate the functional status of patients with PAOD [52, 53]. Performing this method is limited when the patient has incompressible calcified arteries. This is due to a much larger cuff pressure necessary to compress the vessel under this condition [54]. PAOD in a patient with arterial calcification thus will not be detected by ABI measurements. Moreover, there is a lack of noninvasive diagnostic tools to detect and quantify PAOD disease improvement in terms of adaption of the vascular system and effectiveness of vessel stimulation therapies [40, 55]. As previously mentioned, BOLD MRI allows conclusions about alterations in tissue oxygenation of the skeletal muscle, with a high spatial resolution [19, 43, 56–60]. Thus, it is a potential diagnostic tool for evaluating microcirculation function in the skeletal muscle of patients with PAOD.
There are three studies investigating muscle BOLD MRI in PAOD: Ledermann et al. [33] compared skeletal muscle BOLD signal of 17 patients with symptomatic PAOD to a control group consisting of 11 healthy volunteers of similar age. They performed a T2*-weighted single-shot multiecho EPI sequence on a whole-body magnetic resonance scanner at 1.5 T and used an arterial occlusion paradigm with cuff compression to provoke postischemic reactive hyperemia. The patient group demonstrated a lower T2 *max and a more than twofold prolongation of the TTP value. Both differences were highly significant. Impaired microcirculation in the human skeletal muscle of the patient group is accompanied by a change in the T2* time course. The delayed TTP might be explained by the lack of oxygenated blood in the microvasculature, most possibly due to diminished microperfusion after vascular stenoses. It is difficult to understand the underlying mechanisms of the significant T2 *max -decrease. A variety of effects could underly this mechanism. For instance, the longer contact time of the blood with the capillaries might lead to a more efficient deoxygenation of hemoglobin inside the capillaries. Another factor might be the circulation of a lower blood volume in patients with PAOD owing to damaged capillaries in the skeletal muscle [61, 62]. Further studies correlating BOLD measurements with the assessment of perfusion (e.g., via laser Doppler flowmetry or arterial spin labeling) and oxygenation (e.g. via near-infrared spectroscopy) are warranted to elucidate the exact pathophysiological mechanisms underlying theses BOLD time-course changes in PAOD patients. An example of a T2* time course during reactive hyperemia from a patient suffering from PAOD is shown in Fig. 2a.
a T2* time courses during reactive hyperemia of a 79-year-old woman suffering from peripheral arterial occlusive disease (PAOD) with signs of intermittent claudication and restrictions of pain-free walking distance >200 m (Fontaine Stage IIa, red line) and a 46-year old healthy woman volunteer (blue line). b T2* time courses during the ischemic period of a 74-year-old woman suffering from PAOD with severe claudication and a pain-free walking distance of about 80 m (Fontaine Stage IIb, red line) and the same volunteer as in a (blue line)
Another study investigated muscle BOLD response during the ischemic phase in 15 patients with PAOD versus ten healthy volunteers also using a cuff compression paradigm [38]. Differences in mean T2 *min values and T2* time courses were observed between both groups: In the patient group, a rapid decrease of the T2* time course was followed by a slower decrease and finally ending in a constant T2 *min value that did not change over time. The control group revealed a rapid decrease of the T2* value during the entire ischemic period, resulting in a significantly lower T2 *min compared with the patient group. The observed differences in the T2* time course are most likely explained by a reduced oxygen consumption in patients with PAOD, because T2* decrease was not only diminished but also retarded when compared with healthy individuals. This effect may be caused by morphological (i.e., reduced capillary density) and/or metabolic alterations in the skeletal muscle of patients with PAOD, leading to reduced oxygen consumption in the distal muscle tissue [47, 63]. In Fig. 2b, an example of a T2* time course during ischemia from a patient suffering from PAOD is demonstrated.
A study from Versluis et al. [64] deals with reproducibility of different MRI imaging methods, including muscle BOLD MRI for assessing patients with PAOD. Postischemic reactive hyperemia with a cuff compression paradigm was provoked in healthy volunteers and PAOD patients and a multishot single-echo EPI sequence with fat suppression for acquiring the BOLD response was performed. All muscles were assessed together with one large ROI over the entire cross-section of the calf. A poor interscan reproducibility was determined in this study for the maximal T2* change [patients: T2 *max = 13.2 ± 6.4%, coefficient of variation (CV) = 26.7%, repeatability coefficient (RC) = 9.7%; volunteers: T2 *max = 13.3 ± 5.9%, CV = 21.5%, RC = 7.9%]. However, for the TTP value, fair reproducibility was demonstrated (patients: TTP = 116 ± 26.8 s, CV = 10.6%, RC = 33.8 s; volunteers: TTP = 60.7 ± 15.9 s, CV = 15.9%, RC = 26.7 s). According to the authors, tissue oxygenation might change over time. This can be explained by many intrinsic and extrinsic factors that influence the day-to-day oxygenation status of the calf muscle, including but not limited to hormones, insulin secretion, temperature, day time, and eating habits [65]. The authors concluded that acquiring reliable functional data with muscle BOLD MRI in patients with peripheral arterial disease using a 1.5-Tesla MRI scanner is not advisable in clinical settings, with the exception of the TTP value. A further cause of the poor interscan reproducibility could be the missing exclusion of larger vessels from the ROI that included the entire soft tissue of the analyzed calf diameter. This may have caused inflow artefacts in the acquired T2* data. Additionally, the used single-echo EPI sequences makes the BOLD measurement even more prone to alterations of inflow, T1-, and baseline changes. Considering these limitations and the fact that several other published studies evaluating BOLD muscle MRI in PAOD patients showed significant time course alterations in relatively small patient collectives, reproducibility of skeletal muscle BOLD MRI could be higher than evaluated by Versluis et al. [64]. However, due to lack of supporting evidence, it is necessary to investigate the reproducibility of muscle BOLD signal in larger studies. This must inevitable include taking care of maximal standardization during the imaging procedure and the use of multiecho sequences to minimize confounding parameters.
In summary, noninvasive diagnosis and follow-up MRI investigations in patients with PAOD are feasible with muscle BOLD MRI. By evaluating microcirculation function in the calf, muscle BOLD MRI has the potential to serve a noninvasive low-risk (no radiation dose, no contrast agent) diagnostic tool for monitoring conservative and invasive therapeutic approaches. Moreover, skeletal muscle BOLD MRI assesses end-organ function and serves as a quantitative method for functional imaging in PAOD. In contrast to other MRI imaging techniques developed with the same purpose, such as first-pass gadolinium-enhanced MRI, muscle BOLD MRI does not require any contrast agent, making repeated measurements possible [66]. With MRI as a comprehensive diagnostic tool in PAOD, a macrovascular morphological visualization could be combined with microvascular functional measurements using muscle BOLD MRI [21, 67, 68]. Such a comprehensive diagnostic tool might be of high value in clinical settings. Further investigations in larger patient cohorts are warranted to confirm these encouraging results and to determine the value of muscle BOLD MRI in clinical settings, including sensitivity and specificity.
Treatment evaluation
Muscle BOLD MRI has the potential to serve as an objective tool for planning and assessing the success of different therapeutic approaches to vascular diseases, such as conservative treatment with drugs or invasive procedures such as stenting or bypass surgery. This is of particular interest due to the capability of muscle BOLD MRI to reveal end-organ function rather than global function of macrocirculation [33]. The study by Hügli et al. [40] investigated the response of muscle BOLD MRI in ten patients with PAOD 1 day before and 6 weeks after percutaneous transluminal angioplasty of the superficial femoral artery. A cuff compression paradigm was used to provoke reactive hyperemia. Treatment of stenoses should lead to improved macrovascular and consecutively also microvascular function. Although not reaching significance level, the investigators found homogenous improvements of the key BOLD parameters TTP (decreased), T2 *max (increased), and end value (decreased) from the first to the second measurement. The fact that these changes in key BOLD parameters did not reach significance level was explained by the low number of patients, the inhomogeneous patient group, and the relative short follow-up period. Blood inflow over the normal anatomical course of the arteries is faster than over the collateral vessels. That could be the reason TTP decreased in this study. T2 *max could have increased due to a diminished oxygen extraction at higher microcirculatory flow, according to the Fick principle. This increase of blood inflow could also lead to a faster washout of blood from the calf muscle, thus leading to decreased T2* values at the end of hyperemia. The increased maximal T2* change might be based on increased blood oxygen supply. This optimized blood oxygen supply has already been demonstrated with transcutaneous oxygen pressure measurements in PAOD patients [69, 70]. New therapeutic concepts in PAOD aim to induce collateral formation and to improve function of existing arteries by angiogenic growth factors or stem cell administration [71–74]. It might be interesting to see whether muscle BOLD MRI can demonstrate the success of these approaches by showing improved microcirculatory function.
Compartment syndrome
Chronic compartment syndrome has an unclear underlying pathophysiology. The main problem seems to be an exercise-induced increase of tissue pressure in one of the four compartments of the calf, resulting in a compression of muscles and vessels [34]. Patients show symptoms during and after exercise (i.e., walking, cycling) such as burning, pain, and cramping, which normally resolve under resting conditions [75]. Most often, the anterior compartment of the calf is affected. The elevated compartment pressure (>15 mmHg) causes decreased blood inflow, leading to ischemic pain. To assess chronic pressure effects in muscle compartments, BOLD signal is an attractive method to noninvasively detect microvasculature changes.
In a prospective study, Andreisek et al. [39] investigated muscle BOLD signal alterations in chronic compartment syndrome patients. They expected a lower T2* signal in patients with chronic compartment syndrome because of impaired perfusion and therefore delayed reoxygenation of the working calf muscle. Nine patients and ten controls underwent muscle BOLD MRI before and after exercise, and T2* signal in the lower extremity was registered. An immediate response after exercise concomitantly with an increase in T2* in both groups could be demonstrated. Although the patients reported higher levels of symptoms during exercise than did controls, a significant difference in terms of the T2* signal between groups could not be found. Moreover, the level of pain or muscle weakness did not show a correlation with the T2* signal. The T2* signal 15 min after muscle exercise was still elevated, which is most likely not due to a real BOLD effect but rather to much larger and longer-lasting T2/T2* effects caused by osmotic changes in muscle after repetitive exercise [76–78].
Another study used frequency-dependent signal intensity mapping after Fourier transformation to show alterations in BOLD response of a patient with chronic compartment syndrome [34]. This method relied on the disappearance of physiological cardiac and respiratory frequency peaks in the ROIs of the affected compartment. As spectral SI changes of BOLD signals after Fourier transformation are absent when excluding visible vessels from the defined ROIs, this method depends on blood inflow rather than oxygenation [79]. Hence, a sufficient imaging paradigm for the diagnosis of chronic compartment syndrome in the clinical setting is still lacking.
Diabetes mellitus
Diabetes mellitus is associated with impaired macro- and microcirculation [80–82]. Especially in this patient group, the early diagnosis of disturbances in the vascular system is crucial to prevent secondary disease complications. Macrovasculature can be visualized with Doppler ultrasound, MR angiography, or plethysmography [83, 84]. Detecting changes of the microvasculature still remains a challenge. BOLD signal time course and corresponding values reflect the peripheral microvascular function and thus might be an interesting diagnostic tool that can be applied in patients with diabetes mellitus [24, 31]. In a study from Slade et al. microvascular function was assessed in patients with diabetes mellitus types I and II and in a matched control group using muscle BOLD MRI. An exercise paradigm with single-muscle contractions was performed. Regarding BOLD signal of ankle dorsiflexors, no differences were found between the patients and healthy controls. This was explained by the relatively short duration of persistent diabetes in the patient group. In this study, it could be confirmed that the BOLD response depends significantly on age. Influence of age on the BOLD signal during ischemia and reactive hyperemia was already demonstrated in previous studies using arterial occlusion paradigms [30, 36]. Another BOLD study aimed at detecting blood volume and oxygenation status in diabetes mellitus type 2 patients and obese and lean individuals following isometric dorsiflexion contractions [85]. A dual GRE EPI sequence with two different echo times of 6 and 46 ms was applied to measure MRI signal intensity alterations. The postcontraction signal intensity differences were calculated, predominantly indicating altered blood volume (for TE of 6 ms) or oxygenation status (for TE of 46 ms) [20]. Considering the echo time of 6 ms, signal intensity differences were lower in diabetic and obese individuals compared with the lean group with respect to the extensor digitorum longus muscle. When evaluating the echo time of 46 ms, signal intensity differences were only lower in diabetic patients compared with lean controls. These findings reveal altered blood volume status in diabetic and obese individuals and altered oxygenation status only in diabetic patients. These studies show that small-vessel impairment in patients with diabetes or obesity can be detected with functional MRI in the absence of overt macro- or microvascular complications. This technique might thus be helpful for detecting preclinical disease states.
Paradigm selection in clinical settings
Muscle BOLD signal shows a dynamic response to vascular diseases such as PAOD. To induce measurable changes in the T2* signal, it is necessary to apply a suitable paradigm. Under resting conditions, patients with vascular diseases could have a nearly normal oxygenation status in the calf muscle, but under cuff compression an impaired microcirculation function is seen because the usual metabolic demand cannot be compensated by a sufficient blood inflow. All muscle BOLD MRI studies in PAOD patients used an arterial occlusion paradigm to provoke either ischemia or reactive hyperemia. This paradigm has some advantages, particularly when investigating vascular diseases:
-
`1.
Blood inflow and outflow can be completely prevented by the suprasystolic pressure.
-
2.
Through fast cuff inflation, the influence of venous filling on the BOLD signal is minimized.
-
3.
Patient compliance is not required.
-
4.
This paradigm can be standardized for use in clinical settings.
-
5.
Motion artifacts are a well-known problem in functional MRI of the brain; in the cuff-compression paradigm, such motion artifacts could be kept to a minimum.
Points 3 and 5 are particularly relevant advantages of this paradigm in the clinical setting when compared with muscle-contraction paradigms. Furthermore, paradigm selection is a matter of measurable BOLD SI changes. Regarding patients with diabetes mellitus, oxygenation-sensitive functional MRI revealed smaller T2 signal intensity changes than did sequences sensitive for blood volume [31, 85]. Arterial occlusion paradigms, showing promising results in PAOD evaluation, have not been tested in diabetic or obese individuals. For clinical implementation of skeletal-muscle BOLD MRI, the diagnostic power of different paradigms should be further evaluated through mutual analysis. Prior to doing this in patient collectives, we see the potential to test exercise and arterial occlusion in older volunteers, where both paradigms successfully showed BOLD signal alterations.
As for muscle exercise, arterial occlusion has also some important drawbacks. A subset of patients complains about discomfort. In one study, mild to moderate discomfort was reported [33]. In another study, however, severe discomfort during cuff inflation was observed in three of eight patients with PAOD and in three of ten healthy volunteers [64]. In the third study, all patients tolerated the cuff-compression paradigm well [40]. Patients with necrosis or gangrene should be excluded from this paradigm, because suprasystolic cuff compression implies the risk of disease progression. In patients with bypass surgery, safety concerns exist regarding the theoretical risk of bypass occlusion through the suprasystolic cuff pressure.
Conclusion
The authors of this study conclude that muscle BOLD MRI is a valuable tool to noninvasively assess peripheral microvasculature. In PAOD, BOLD MRI of skeletal muscle has been proven to successfully differentiate between patients and healthy individuals. To what extent BOLD imaging bears sufficient sensitivity and specificity for routine clinical implementation is yet to be demonstrated. Initial reports on other vascular diseases, such as compartment syndrome and diabetes, have revealed somewhat controversial results. This may reflect the need for consistent and efficient experimental muscle BOLD imaging setups and the use of effective imaging paradigms. However, several pathological conditions affect the peripheral vasculature not yet studied by BOLD imaging, i.e., vasculitides, connective tissue diseases, and other inflammatory conditions. With well-designed studies, it will be possible to show under which of these conditions BOLD MRI of skeletal muscle is helpful in basic research, diagnostics, classification, and treatment evaluation. As BOLD MRI predominantly reflects oxygenation changes in the microvasculature, new insights into the pathogenesis of these diseases may be revealed.
References
Ogawa S, Lee TM, Kay AR, Tank DW (1990) Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci USA 87(24):9868–9872
Glover GH (2011) Overview of functional magnetic resonance imaging. Neurosurg Clin N Am 22(2):133–139
Wacker CM, Bock M, Hartlep AW, Bauer WR, van Kaick G, Pfleger S, Ertl G, Schad LR (1999) BOLD-MRI in ten patients with coronary artery disease: evidence for imaging of capillary recruitment in myocardium supplied by the stenotic artery. Magn Reson Mater Phys 8(1):48–54
Manka R, Paetsch I, Schnackenburg B, Gebker R, Fleck E, Jahnke C (2010) BOLD cardiovascular magnetic resonance at 3.0 tesla in myocardial ischemia. J Cardiovasc Magn Reson 12:54
Kido A, Koyama T, Kataoka M, Yamamoto A, Saga T, Turner R, Togashi K (2007) Physiological changes of the human uterine myometrium during menstrual cycle: preliminary evaluation using BOLD MR imaging. J Magn Reson Imaging 26(3):695–700
Prasad PV, Edelman RR, Epstein FH (1996) Noninvasive evaluation of intrarenal oxygenation with BOLD MRI. Circulation 94(12):3271–3275
Li SP, Taylor NJ, Makris A, Ah-See ML, Beresford MJ, Stirling JJ, d’Arcy JA, Collins DJ, Padhani AR (2010) Primary human breast adenocarcinoma: imaging and histologic correlates of intrinsic susceptibility-weighted MR imaging before and during chemotherapy. Radiology 257(3):643–652
Alonzi R, Padhani AR, Maxwell RJ, Taylor NJ, Stirling JJ, Wilson JI, d’Arcy JA, Collins DJ, Saunders MI, Hoskin PJ (2009) Carbogen breathing increases prostate cancer oxygenation: a translational MRI study in murine xenografts and humans. Br J Cancer 100(4):644–648
Ogawa S, Menon RS, Tank DW, Kim SG, Merkle H, Ellermann JM, Ugurbil K (1993) Functional brain mapping by blood oxygenation level-dependent contrast magnetic resonance imaging. A comparison of signal characteristics with a biophysical model. Biophys J 64(3):803–812
Noseworthy MD, Bulte DP, Alfonsi J (2003) BOLD magnetic resonance imaging of skeletal muscle. Semin Musculoskelet Radiol 7(4):307–315
Toussaint JF, Kwong KK, Mkparu FO, Weisskoff RM, LaRaia PJ, Kantor HL (1996) Perfusion changes in human skeletal muscle during reactive hyperemia measured by echo-planar imaging. Magn Reson Med 35(1):62–69
Weisskoff RM, Zuo CS, Boxerman JL, Rosen BR (1994) Microscopic susceptibility variation and transverse relaxation: theory and experiment. Magn Reson Med 31(6):601–610
Lebon VB-SC, Bloch G, Leroy-Willig A, Carlier PG (1998) Evidence of muscle BOLD effect revealed by simultaneous interleaved gradient-echo NMRI and myoglobin NMRS during leg ischemia. Magn Reson Med 40:551–558
Ledermann HP, Heidecker HG, Schulte AC, Thalhammer C, Aschwanden M, Jaeger KA, Scheffler K, Bilecen D (2006) Calf muscles imaged at BOLD MR: correlation with TcPO2 and flowmetry measurements during ischemia and reactive hyperemia–initial experience. Radiology 241(2):477–484
Sanchez OA, Copenhaver EA, Elder CP, Damon BM (2010) Absence of a significant extravascular contribution to the skeletal muscle BOLD effect at 3 T. Magn Reson Med 64(2):527–535
Schulte AC, Speck O, Oesterle C, Hennig J (2001) Separation and quantification of perfusion and BOLD effects by simultaneous acquisition of functional I(0)- and T2(*)-parameter maps. Magn Reson Med 45(5):811–816
Meyer RA, Towse TF, Reid RW, Jayaraman RC, Wiseman RW, McCully KK (2004) BOLD MRI mapping of transient hyperemia in skeletal muscle after single contractions. NMR Biomed 17(6):392–398
Hennig JSK, Schreiber A (2000) Time resolved observation of BOLD effect in muscle during isometric exercise. Proc Int Soc Magn Reson Med 8:122
Jordan B, Kimpalou J, Beghein N, Dessy C, Feron O, Gallez B (2004) Contribution of oxygenation to BOLD contrast in exercising muscle. Magn Reson Med 52(2):391–396
Damon BM, Hornberger JL, Wadington MC, Lansdown DA, Kent-Braun JA (2007) Dual gradient-echo MRI of post-contraction changes in skeletal muscle blood volume and oxygenation. Magn Reson Med 57(4):670–679
Carlier PG, Bertoldi D, Baligand C, Wary C, Fromes Y (2006) Muscle blood flow and oxygenation measured by NMR imaging and spectroscopy. NMR Biomed 19(7):954–967
Wigmore DM, Damon BM, Pober DM, Kent-Braun JA (2004) MRI measures of perfusion-related changes in human skeletal muscle during progressive contractions. J Appl Physiol 97(6):2385–2394
Duteil S, Wary C, Raynaud JS, Lebon V, Lesage D, Leroy-Willig A, Carlier PG (2006) Influence of vascular filling and perfusion on BOLD contrast during reactive hyperemia in human skeletal muscle. Magn Reson Med 55(2):450–454
Towse TF, Slade JM, Ambrose JA, Delano MC, Meyer RA (2011) Quantitative analysis of the post-contractile blood-oxygenation-level-dependent (BOLD) effect in skeletal muscle. J Appl Physiol 111(1):27–39
Towse TF, Slade JM, Meyer RA (2005) Effect of physical activity on MRI-measured blood oxygen level-dependent transients in skeletal muscle after brief contractions. J Appl Physiol 99(2):715–722
Utz W, Jordan J, Niendorf T, Stoffels M, Luft FC, Dietz R, Friedrich MG (2005) Blood oxygen level-dependent MRI of tissue oxygenation: relation to endothelium-dependent and endothelium-independent blood flow changes. Arterioscler Thromb Vasc Biol 25(7):1408–1413
Damon BM, Gore JC (2005) Physiological basis of muscle functional MRI: predictions using a computer model. J Appl Physiol 98(1):264–273
Wilkie DR, Dawson MJ, Edwards RH, Gordon RE, Shaw D (1984) 31P NMR studies of resting muscle in normal human subjects. Adv Exp Med Biol 170:333–347
Lebon VC, Carlier PG, Brillault-Salvat C, Bloch G, Leroy-Willig A (1998) Anisotropy of the BOLD effect in the skeletal muscle. Proceedings ISMRM Sydney: 1424
Schulte AC, Aschwanden M, Bilecen D (2008) Calf muscles at blood oxygen level-dependent MR imaging: aging effects at postocclusive reactive hyperemia. Radiology 247(2):482–489
Slade JM, Towse TF, Gossain VV, Meyer RA (2011) Peripheral microvascular response to muscle contraction is unaltered by early diabetes, but decreases with age. J Appl Physiol 111(5):1361–1371
Bulte DP, Alfonsi J, Bells S, Noseworthy MD (2006) Vasomodulation of skeletal muscle BOLD signal. J Magn Reson Imaging 24(4):886–890
Ledermann HP, Schulte AC, Heidecker HG, Aschwanden M, Jäger KA, Scheffler K, Steinbrich W, Bilecen D (2006) Blood oxygenation level-dependent magnetic resonance Imaging of the skeletal muscle in patients with peripheral arterial occlusive disease. Circulation 113(25):2929–2935
Noseworthy MD, Davis AD, Elzibak AH (2010) Advanced MR imaging techniques for skeletal muscle evaluation. Semin Musculoskelet Radiol 14(2):257–268
Gold GE (2003) Dynamic and functional imaging of the musculoskeletal system. Semin Musculoskelet Radiol 7(4):245–248
Kos S, Klarhofer M, Aschwanden M, Scheffler K, Jacob AL, Bilecen D (2009) Simultaneous dynamic blood oxygen level-dependent magnetic resonance imaging of foot and calf muscles: aging effects at ischemia and postocclusive hyperemia in healthy volunteers. Invest Radiol 44(11):741–747
Lebon V, Carlier PG, Brillault-Salvat C, Leroy-Willig A (1998) Simultaneous measurement of perfusion and oxygenation changes using a multiple gradient-echo sequence: application to human muscle study. Magn Reson Imaging 16(7):721–729
Potthast S, Schulte A, Kos S, Aschwanden M, Bilecen D (2009) Blood oxygenation level-dependent MRI of the skeletal muscle during ischemia in patients with peripheral arterial occlusive disease. Rofo 181(12):1157–1161
Andreisek G, White LM, Sussman MS, Langer DL, Patel C, Su JW, Haider MA, Stainsby JA (2009) T2*-weighted and arterial spin labeling MRI of calf muscles in healthy volunteers and patients with chronic exertional compartment syndrome: preliminary experience. AJR Am J Roentgenol 193(4):W327–W333
Huegli RW, Schulte AC, Aschwanden M, Thalhammer C, Kos S, Jacob AL, Bilecen D (2009) Effects of percutaneous transluminal angioplasty on muscle BOLD-MRI in patients with peripheral arterial occlusive disease: preliminary results. Eur Radiol 19(2):509–515
Howseman AM, Bowtell RW (1999) Functional magnetic resonance imaging: imaging techniques and contrast mechanisms. Philos Trans R Soc Lond B Biol Sci 354(1387):1179–1194
Block KT, Frahm J (2005) Spiral imaging: a critical appraisal. J Magn Reson Imaging 21(6):657–668
Speck O, Hennig J (1998) Functional imaging by I0- and T2*-parameter mapping using multi-image EPI. Magn Reson Med 40(2):243–248
Diehm C, Kareem S, Lawall H (2004) Epidemiology of peripheral arterial disease. Vasa 33(4):183–189
Selvin E, Erlinger TP (2004) Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation 110(6):738–743
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG (2007) Inter-Society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 45 Suppl S:S5–67
Clyne CA, Mears H, Weller RO, O’Donnell TF (1985) Calf muscle adaptation to peripheral vascular disease. Cardiovasc Res 19(8):507–512
Henriksson J, Nygaard E, Andersson J, Eklof B (1980) Enzyme activities, fibre types and capillarization in calf muscles of patients with intermittent claudication. Scand J Clin Lab Invest 40(4):361–369
Regensteiner JG, Wolfel EE, Brass EP, Carry MR, Ringel SP, Hargarten ME, Stamm ER, Hiatt WR (1993) Chronic changes in skeletal muscle histology and function in peripheral arterial disease. Circulation 87(2):413–421
Prince MR (1998) Peripheral vascular MR angiography: the time has come. Radiology 206(3):592–593
Rofsky NM, Adelman MA (2000) MR angiography in the evaluation of atherosclerotic peripheral vascular disease. Radiology 214(2):325–338
Begelman SM, Jaff MR (2006) Noninvasive diagnostic strategies for peripheral arterial disease. Cleve Clin J Med 73(Suppl 4):S22–S29
van Langen H, van Gurp J, Rubbens L (2009) Interobserver variability of ankle-brachial index measurements at rest and post exercise in patients with intermittent claudication. Vasc Med 14(3):221–226
Stein R, Hriljac I, Halperin JL, Gustavson SM, Teodorescu V, Olin JW (2006) Limitation of the resting ankle-brachial index in symptomatic patients with peripheral arterial disease. Vasc Med 11(1):29–33
Stewart KJ, Hiatt WR, Regensteiner JG, Hirsch AT (2002) Exercise training for claudication. N Engl J Med 347(24):1941–1951
Prielmeier F, Nagatomo Y, Frahm J (1994) Cerebral blood oxygenation in rat brain during hypoxic hypoxia. Quantitative MRI of effective transverse relaxation rates. Magn Reson Med 31(6):678–681
Prielmeier F, Merboldt KD, Hanicke W, Frahm J (1993) Dynamic high-resolution MR imaging of brain deoxygenation during transient anoxia in the anesthetized rat. J Cereb Blood Flow Metab 13(5):889–894
Villringer A (1997) Understanding functional neuroimaging methods based on neurovascular coupling. Adv Exp Med Biol 413:177–193
Barrett T, Brechbiel M, Bernardo M, Choyke PL (2007) MRI of tumor angiogenesis. J Magn Reson Imaging 26(2):235–249
Baudelet C, Cron GO, Gallez B (2006) Determination of the maturity and functionality of tumor vasculature by MRI: correlation between BOLD-MRI and DCE-MRI using P792 in experimental fibrosarcoma tumors. Magn Reson Med 56(5):1041–1049
Hickey NC, Hudlicka O, Simms MH (1992) Claudication induces systemic capillary endothelial swelling. Eur J Vasc Surg 6(1):36–40
Dawson JM, Hudlicka O (1990) Changes in the microcirculation in slow and fast skeletal muscles with long term limitations of blood supply. Cardiovasc Res 24(5):390–395
McGuigan MR, Bronks R, Newton RU, Sharman MJ, Graham JC, Cody DV, Kraemer WJ (2001) Muscle fiber characteristics in patients with peripheral arterial disease. Med Sci Sports Exerc 33(12):2016–2021
Versluis B, Backes WH, van Eupen MG, Jaspers K, Nelemans PJ, Rouwet EV, Teijink JA, Mali WP, Schurink GW, Wildberger JE, Leiner T (2011) Magnetic resonance imaging in peripheral arterial disease: reproducibility of the assessment of morphological and functional vascular status. Invest Radiol 46(1):11–24
Deanfield J, Donald A, Ferri C, Giannattasio C, Halcox J, Halligan S, Lerman A, Mancia G, Oliver JJ, Pessina AC, Rizzoni D, Rossi GP, Salvetti A, Schiffrin EL, Taddei S, Webb DJ (2005) Endothelial function and dysfunction. Part I: methodological issues for assessment in the different vascular beds: a statement by the working group on endothelin and endothelial factors of the European Society of hypertension. J Hypertens 23(1):7–17
Lutz AM, Weishaupt D, Amann-Vesti BR, Pfammatter T, Goepfert K, Marincek B, Nanz D (2004) Assessment of skeletal muscle perfusion by contrast medium first-pass magnetic resonance imaging: technical feasibility and preliminary experience in healthy volunteers. J Magn Reson Imaging 20(1):111–121
Mohajer K, Zhang H, Gurell D, Ersoy H, Ho B, Kent KC, Prince MR (2006) Superficial femoral artery occlusive disease severity correlates with MR cine phase-contrast flow measurements. J Magn Reson Imaging 23(3):355–360
Galbraith SM, Lodge MA, Taylor NJ, Rustin GJ, Bentzen S, Stirling JJ, Padhani AR (2002) Reproducibility of dynamic contrast-enhanced MRI in human muscle and tumours: comparison of quantitative and semi-quantitative analysis. NMR Biomed 15(2):132–142
Hanna GP, Fujise K, Kjellgren O, Feld S, Fife C, Schroth G, Clanton T, Anderson V, Smalling RW (1997) Infrapopliteal transcatheter interventions for limb salvage in diabetic patients: importance of aggressive interventional approach and role of transcutaneous oximetry. J Am Coll Cardiol 30(3):664–669
Wagner HJ, Schmitz R, Alfke H, Klose KJ (2003) Influence of percutaneous transluminal angioplasty on transcutaneous oxygen pressure in patients with peripheral arterial occlusive disease. Radiology 226(3):791–797
Markkanen JE, Rissanen TT, Kivela A, Yla-Herttuala S (2005) Growth factor-induced therapeutic angiogenesis and arteriogenesis in the heart gene therapy. Cardiovasc Res 65(3):656–664
Tammela T, Enholm B, Alitalo K, Paavonen K (2005) The biology of vascular endothelial growth factors. Cardiovasc Res 65(3):550–563
Aghi M, Chiocca EA (2005) Contribution of bone marrow-derived cells to blood vessels in ischemic tissues and tumors. Mol Ther 12(6):994–1005
Wahlberg E (2003) Angiogenesis and arteriogenesis in limb ischemia. J Vasc Surg 38(1):198–203
Fraipont MJ, Adamson GJ (2003) Chronic exertional compartment syndrome. J Am Acad Orthop Surg 11(4):268–276
Verleisdonk EJ, van Gils A, van der Werken C (2001) The diagnostic value of MRI scans for the diagnosis of chronic exertional compartment syndrome of the lower leg. Skeletal Radiol 30(6):321–325
Eskelin MK, Lotjonen JM, Mantysaari MJ (1998) Chronic exertional compartment syndrome: MR imaging at 0.1 T compared with tissue pressure measurement. Radiology 206(2):333–337
Litwiller DV, Amrami KK, Dahm DL, Smith J, Laskowski ER, Stuart MJ, Felmlee JP (2007) Chronic exertional compartment syndrome of the lower extremities: improved screening using a novel dual birdcage coil and in-scanner exercise protocol. Skeletal Radiol 36(11):1067–1075
Davies AD, Noseworthy MD (2011) Fourier analysis of muscle BOLD data after exercise. Int Soc Magn Reson Med 19:1163
Golster H, Hyllienmark L, Ledin T, Ludvigsson J, Sjoberg F (2005) Impaired microvascular function related to poor metabolic control in young patients with diabetes. Clin Physiol Funct Imaging 25(2):100–105
Cesarone MR, De Sanctis MT, Incandela L, Belcaro G, Griffin M, Cacchio M (2001) Methods of evaluation and quantification of microangiopathy in high perfusion microangiopathy (chronic venous insufficiency and diabetic microangiopathy). Angiology 52(Suppl 2):S3–S7
Caballero AE, Arora S, Saouaf R, Lim SC, Smakowski P, Park JY, King GL, LoGerfo FW, Horton ES, Veves A (1999) Microvascular and macrovascular reactivity is reduced in subjects at risk for type 2 diabetes. Diabetes 48(9):1856–1862
Fathi R, Marwick TH (2001) Noninvasive tests of vascular function and structure: why and how to perform them. Am Heart J 141(5):694–703
McCully KK, Posner JD (1995) The application of blood flow measurements to the study of aging muscle. J Gerontol A Biol Sci Med Sci 50:130–136
Sanchez OA, Copenhaver EA, Chance MA, Fowler MJ, Towse TF, Kent-Braun JA, Damon BM (2011) Postmaximal contraction blood volume responses are blunted in obese and type 2 diabetic subjects in a muscle-specific manner. Am J Physiol Heart Circ Physiol 301(2):H418–H427
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Partovi, S., Karimi, S., Jacobi, B. et al. Clinical implications of skeletal muscle blood-oxygenation-level-dependent (BOLD) MRI. Magn Reson Mater Phy 25, 251–261 (2012). https://doi.org/10.1007/s10334-012-0306-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-012-0306-y