Abstract
A multiplex PCR assay was devised and compared with standard conventional methods for quality evaluation of pharmaceutical raw materials and finished products with low levels of microbial contamination. Samples which were artificially contaminated with <10 colony forming units of Escherichia coli, Staphylococcus aureus, Pseudomonas aeruginosa, and Salmonella species and possibly contaminated samples were incubated for 16 h with different enrichment media. Primers that deduce 559 bp fragment of the 16S rRNA gene was employed in amplifying E. coli species, similarly invasion protein gene with 275 bp fragment size was used as target for detecting Salmonella spp., in case of S. aureus a 461 bp amplicon from m-RNA nuclease gene, and an 709 bp fragment from oprL gene was used for amplifying P. aeruginosa. The detection limits for artificially contaminants by multiplex PCR was 1 CFU/g, where as in case of conventional method the detection limit was >2 CFU/g. Similarly, when tested with possibly contaminated samples, 35% were detected for E. coli, Salmonella spp., S. aureus and P. aeruginosa species with multiplex PCR, while only 21% were detected with standard conventional microbial methods. Multiplex PCR assay provides sensitive and reliable results and allows for the cost-effective detection of all four bacterial pathogens in single reaction tube.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
United States Pharmacopoeia (USP) microbial limit test necessitates the determination of total microbial content of bacteria, yeast, and molds in non-sterile pharmaceutical samples. In addition to microbial content, microbiological analysis needs to determine the safety of a given product by the presence or absence of indicator microorganisms which are hazardous to consumers. For this purpose, USP microbial limits test requires absence of four different bacterial indicators: Salmonella spp., Staphylococcus aureus, Pseudomonas aeruginosa, and Escherichia coli. In spite of regulatory guidelines and recommended methods, microbial contamination is still one of the major causes for products recalls world wide. Of four USP and EP (European Pharmacopoeia) bacterial indicators S. aureus, P. aeruginosa, and E. coli were found in samples of toothpastes, topical products, shampoos, oral solutions, drugs, and disinfectants [2, 7, 10, 18, 21, 26]. Contamination was due to the presence of objectionable microorganisms in raw materials and water or from poor practices during product manufacturing.
The development of rapid, sensitive, and infallible methods of detecting indicator pathogens has received much impetus in the recent years owing to an increased awareness of the health hazards associated with microbial contamination of pharma samples. Conventional methods of detecting bacteria in pharma contaminants comprise propagation in selective enrichment media followed by confirmation and biochemical tests, which are cumbersome and time-consuming. The advent of nucleic acid-based assay systems like the polymerase chain reaction (PCR) has led to the emergence of improved, expedient, and reliable methods of microbial identification and surveillance, capable of even detecting non-viable cells [17]. The direct detection of indicator pathogens in pharma contaminants is a challenging task, hampered by the presence of PCR-inhibitory substances frequently associated with enrichment media, DNA isolation reagents and the matrix itself and additionally compounded by the presence of high numbers of indigenous microorganisms [42].
Rapid release of samples has resulted in the optimization of manufacturing, product testing, and release allowing high throughput and simultaneous analysis of pharmaceutical formulations. ATP bioluminescence, impedance, direct viable counts, and flow cytometry determine the total microbial content in a given pharmaceutical sample, while PCR and immunoassays detect the presence or absence of specific microbial species. Rapid methods provide reliable and cost-effective analysis for the microbiological evaluation of pharmaceutical environments. Molecular methodologies such as ATP bioluminescence and PCR-based assays provide rapid quality control analysis of cosmetic and pharmaceutical finished products and raw materials. The presence of objectionable microorganisms in cosmetics and pharmaceutical products represents a serious health threat to consumers in world wide [27, 37].
Furthermore, microbial growth has a negative impact on product integrity [35]. Microbial contamination indicates a lack of process control and good manufacturing practices (GMP). Therefore, reducing the frequency or avoiding microbial contamination will optimize quality evaluation and process control. Even though, there is increasing demand for new pharmaceutical products, optimization of resources and constant pressures for cost reduction, there is urgent call for all pharmaceutical industries to develop and implement rapid microbiological procedures for quality control evaluation [25]. However, these new procedures must accomplish rapid sample screening without compromising efficacy and resolution.
Pharmaceutical raw material is defined as every active or inactive substance used in the manufacturing process of a pharmaceutical dosage form. This substance can remain unchanged or suffer any modification during the process. According to their function performed in the medicament, they are classified in two groups: (1) active ingredients with pharmacological activity and (2) excipients that allow the dosage of the active ingredient and its suitability to the administering route.
Control of microbiological contamination of the raw materials is extremely important, because microorganisms may contaminate the finished product as well as the manufacturing plant, which cause an intermittent or continuous pollution of the product that is very difficult to eliminate [33]. The microorganisms that appear in the raw materials can be the origin of certain diseases or may cause spoilage of the medicaments. In recent times, different cases of infections caused by the use of contaminated medicaments have been reported in the scientific literature. Among those cases, it was shown that microbiological contaminations are the root cause for all the raw materials. Many cases have been described such as tetanus in talcum powder [10]; Salmonella infections in tyroidine tablets [18] or by coloring agent (caramine) of capsules [21] and by pancreatine powder [7]; bacteremia by Pseudomonas cepacia present in iodated povidone [2], urinary infections was stimulated by Pseudomonas species in chlorheximide [26], ocular infections were induced by P. aeruginosa in hydrocortisone ointment [18], wound infections caused by Pseudomonas multivorans in a chlorheximide solution [1], and finally skin infections by Mycobacterium chelonae in the gentiane violet used to mark the skin in surgery [34]. The animal raw materials exhibit a very high contamination, mainly due to non-pathogenic enterobacteria, though pathogenic strains of Salmonella and Shigella have also been found [36].
Food and Drug Administration microbiologist routinely examines microbial burden in non-sterile pharmaceutical and cosmetic products [32, 38]. Standard methods are based upon microbiological and biochemical characterization of microorganisms [5, 24, 28]. These methods are labor intensive, time-consuming, slow, and sometimes non-specific and were developed for the isolation of microorganisms from clinical samples. Standard microbiological analysis of pharmaceutical samples requires 5–7 days to be completed [4, 28, 39]. However, rapid methods have given results within 24–30 h [12, 13]. Nevertheless, companies have relied on these methods for quality evaluation of raw materials and finished products [4, 5]. The implementations of rapid methods by a few pharmaceutical companies have already contributed to significant cost-savings and resource optimization [6]. Furthermore, with the increasing complexity of analyses routinely performed in industrial microbiology laboratories, current standard methods do not fulfill those requirements.
Therefore considering above facts, there is demand to develop and apply new technologies for microbiological monitoring of products and raw materials which will be rapid, sensitive, accurate, and cost-effective method [40]. The use of rapid technologies for quality control evaluation of finished products and raw materials has resulted in optimization of product release and manufacturing [13].
However, new molecular methods are available that can rapidly detect microorganisms in contaminated samples. PCR amplifies genetic sequence of the microbial contaminant [11] without compromising specificity and sensitivity. Multiplex PCR assays have been developed and validated for environmental, food, and clinical analyses [3, 19, 23]. However, no multiplex PCR assay has been developed for the detection and identification of indicator bacteria in cosmetic/pharmaceutical raw materials or finished products. The purpose of this study was to develop multiplex PCR assay to detect the presence of bacterial contamination in cosmetic/pharmaceutical raw materials and finished products.
This assay has been shown to detect the target pathogens without interference by other commonly associated pharma bacteria. This is important because in most commercial and many research settings pure cultures would not be the subject of the assay, while the usefulness of the assay based upon speed, accuracy, and cost-effectiveness, has been demonstrated.
Materials and methods
Bacterial strains and growth conditions
The standard strains of Escherichia coli, Salmonella spp., Staphylococcus aureus and Pseudomonas aeruginosa, Pseudomonas fluorescence, Pseudomonas putida, Pseudomonas stutzeri, Burkholderia cepacia, Brevundimonas diminuta, Pseudomonas cepacia, Enterobacter aerogenes, Klebsiella pneumoniae, Shigella sonnei, Citrobacter freundii, Enterobacter cloacae, Staphylococcus intermedius, Stapylococcus epidermidis, Staphylococcus haemolyticus, Staphylococcus warneri were procured from National Collection of Industrial Microorganisms (NCIM), Pune and IMTECH (microbial type culture collection-MTCC), Chandigarh. The bacterial strains were spiked in the range of <10 CFU/g or ml in raw materials and finished products of pharma samples and 10 g of samples were enriched in 100 ml of trypticase soy broth containing 4% Tween-20 and 0.5% soy lecithin for E. coli, S. aureus and P.aeruginosa, and 10 g in 100 ml of BPW for Salmonella spp. and incubated at 37 °C for a period of 16 h. Exactly 10 ml of enriched culture were centrifuged at 12,000 rpm for 5 min at 4 °C from all the samples and the pellet was used for DNA extraction. For standard conventional analysis, the USP procedure was followed for the detection of E. coli, Salmonella spp., S. aureus and P. aeruginosa. Inoculated samples were incubated at 35 °C. Fluid lactose broth enrichments were streaked on eosine methylene blue agar (EMB), MacConkey agar, xylose lysine deoxycholate agar (XLD) and brilliant green agar (BGA). Trypticase soy broth enrichments were streaked on cetrimide agar, Baired Parker agar (BPA) and mannitol–salt agar. After 24–48 h of incubation at 35 °C, colonies were streaked onto sterile plates of trypticase soy agar (TSA) for isolation of pure cultures. TSA plates were incubated for 18–24 h and cells from pure cultures were gram stained and further biochemical identification and serological analysis of individual colonies was performed.
Artificially and possibly contaminated pharma sample analysis
A total of 70 possibly and 50 artificially contaminated samples of the following excipients were analyzed: possibly contaminated samples were 18 lactose, 10 nicotinamide, 8 sodium starch glycollate, 6 xantan gum, 6 gelatin, 6 maize starch, 4 micro crystalline cellulose, 3 ranitidine HCL, 3 mannitol, 3 talc purified, and 3 ibuprofen suspensions. Artificially contaminated samples were 9 magnesium stearate, 8 aluminium hydroxide gel, 6 talc purified, 6 lactose, 6 gelatin, 5 maize starch, 4 attitude hand and body cream, 3 nutrilite daily tablets, and 3 simethicone emulsions. These samples were procured from Vimta Labs Limited, Hyderabad, Sipra Labs Private Limited, Hyderabad, Lucid Labs Private Limited, Hyderabad. These samples were inoculated separately into pre-enrichment broths with 10% (w/v) of product. Among 50 samples, 25 samples were inoculated with <2 CFU/g and remaining 25 samples were inoculated with >2 CFU/g separately as per USP and the pathogens were subjected for DNA extraction to identify the pathogens in uniplex and multiplex PCR methods.
DNA isolation
Bacterial pathogen DNA was isolated from different pharma contaminants using the phenol–chloroform method. The centrifuged pellet was resuspended in TE buffer (10 mM Tris/HCl, pH 8.0), 15 μl 20% SDS and 3 μl proteinase-K (20 mg/ml). The mixture was incubated at 37 °C for 1 h. After incubation, 100 μl of 5 M NaCl was added and mixed thoroughly. To this solution 80 μl of CTAB reagent (4.1 g of NaCl, 10 g of hexa decyl trimethyl ammonium bromide in 100 ml of distilled water) was added and incubated at 65 °C for 10 min. DNA was isolated by centrifugation after phenol–chloroform extraction and was washed with 70% ethanol and dried in a speed vacuum concentrator. The purity of the DNA was checked by 0.8% agarose gel electrophoresis and the quantity of extracted DNA was determined by spectrophotometer and subjected to uniplex, multiplex PCR, and other specificity and sensitivity tests as a template.
Uniplex PCR reaction
The primer sequences utilized for detection of the four selected bacterial pathogens are shown in Table 1. All primers were designed by Gene tool software and synthesized by Mermade IV oligo synthesizer at Bioserve Biotechnologies India Pvt Ltd. Individual PCR reactions for E.coli, Salmonella spp., S.aureus and P.aeruginosa were optimized. The PCR was carried out in 0.2 ml tubes with a reaction volume of 25 μl. All PCR reactions were contained 200 μM of dNTP, 1X PCR buffer, 1 U Taq DNA polymerase and 100 ng of extracted DNA. Optimization of the individual PCR assays were done with different concentrations of magnesium chloride (1.5 and 2.5 mM) and primer (5 and 10 pmol). The positive control consisted of DNA isolated from each standard bacterial strain grown in enrichment broth. The negative controls included PCR mixtures with primers, but without DNA. The reaction was performed in an automated thermal cycler with an initial denaturation at 95 °C for 5 min, followed by 35 cycles at 95, 55, and 68 °C for 30 s, 30 s, and 1 min, respectively, and a final extension at 68 °C for 7 min.
Optimization of multiplex PCR assay
The optimal conditions for multiplex PCR assay were applied by varying concentrations of MgCl2 (1.5 and 2.5 mM), Taq DNA polymerase (1 U and 2 U per reaction) and primers (1.0, 2.5, 5.0, 7.5, and 10.0 pmol). The positive control consisted of DNA isolated from all four bacterial strains grown in a broth culture. The negative control includes PCR reaction mixture all four primers, but without DNA. Reactions were carried out in an automated thermal cycler with an initial denaturation at 95 °C for 5 min followed by 35 cycles at 95, 55, and 68 °C for 30 s, 30 s, and 1 min, respectively, and a final extension at 68 °C for 7 min.
Specificity of multiplex PCR
The PCR primers were also examined for their specificity. Other pharma contaminants such as Pseudomonas fluorescence NCIM 2390, Pseudomonas putida NCIM 2650, Pseudomonas stutzeri NCIM 5136, Burkholderia cepacia MTCC 438, Brevundimonas diminuta MTCC 1287, Pseudomonas cepacia NCIM 5089, Enterobacter aerogenes MTCC 2822, Klebsiella pneumoniae MTCC 109, Shigella sonnei MTCC 2957, Citrobacter freundii MTCC 1658, Enterobacter cloacae MTCC 7322, Staphylococcus intermedius MTCC 3050, Stapylococcus epidermidis MTCC 435, Staphylococcus haemolyticus MTCC 3383, Staphylococcus warneri MTCC 3620 were procured from MTCC and NCIM sources in addition to our specified pathogens. Reactions were carried out in an DNA thermal cycler (ABI-9700) with an initial denaturation at 95 °C for 5 min, followed by 35 cycles at 95, 55, and 68 °C for 30 s, 30 s, and 1 min, respectively, and a final extension at 68 °C for 7 min. The specificity was further confirmed by sequence analysis of amplified PCR product.
Agarose gel electrophoresis
Exactly 10 μl of the amplified PCR products were subjected to electrophoresis on 1% agarose gel containing 0.1 μg of ethidium bromide per ml, and then photographed using gel documentation system C-80 Epi Illumination UV dark room.
Sensitivity of multiplex PCR
The sensitivity of multiplex PCR was also examined by varying DNA concentrations ranging from (100, 50, 25, 12.5, 6.25, 3.12, and 1.56 ng), and primers (1–10 pmol). The reactions were carried out in an automated DNA thermal cycler (ABI-9700) with an initial denaturation at 95 °C for 5 min, followed by 35 cycles at 95, 55, and 68 °C for 30 s, 30 s, and 1 min, respectively, and a final extension at 68 °C for 7 min.
Nucleotide sequence analysis
Sequences for amplifying E.coli (KVR-559) were designed from 16S rRNA sequence; Salmonella spp. (KVR-275) designed from InvA gene, S. aureus (KVR-461) from m-RNA nuclease and P. aeruginosa (KVR-709) from oprL gene were subjected to sequencing for confirmation of the bacterial organisms and their homology to sequence databases in NCBI-GenBank.The sequences were submitted to GenBank and assigned accession numbers EU311614 (Salmonella spp.); EU311615 (S. aureus); EU293839 (E. coli); EU286532 (P. aeruginosa).
Results
Conventional analysis
The pharmaceutical samples and raw materials were inoculated in trypticase soy broth and fluid lactose broth. These suspensions were incubated at 35 °C for 24–48 h for enrichment. After incubation, the enriched broths were streaked onto selective/differential agar for isolation of the target microorganisms. After incubation, representative bacterial colonies were selected based on their morphological characteristics. E. coli shown as green metallic sheen colonies on EMB agar, and lactose fermenting non-mucoid colonies on MacConkey agar. Salmonella shown as red colonies with or without black centers on XLD agar and reddish pink colonies on BGA. P. aeruginosa shown as greenish fluorescence colonies on cetrimide agar. S. aureus shown as shiny black colonies with opaque zone and fermented colonies on mannitol–salt agar. These colonies were further confirmed by biochemical and serological analysis. The positive cultures morphological characteristics on selective media were depicted in Fig. 1.
Uniplex PCR assay
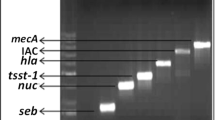
Uniplex PCR was employed to detect four bacterial pathogens, E. coli, Salmonella spp., S. aureus and P. aeruginosa from different pharma contaminants/samples. The primer sequences, target region, and amplicon sizes are summarized in Table 1. The results revealed that the primers are very sensitive and specific to detect bacterial pathogens by adopting annealing temperature at 55 °C, 5 pmol of primer and 1.5 mM MgCl2 concentration shown in Fig. 2. The amplified bacterial pathogens were validated by sequence analysis and subjected to NCBI-BLAST analysis for determining species specificity. Since, uniplex PCR depicted promising results, and for the reason that all pathogens were detected at similar annealing temperature (55° C), we devised multiplex PCR.
Lane 1, Escherichia coli (559 bp) product, when amplified with DNA of E.coli; lane 2, Salmonella spp.(275 bp) product, when amplified with DNA of Salmonella spp.; lane 3, Staphylococcus aureus (461 bp) product, when amplified with DNA of S. aureus; lane 4, Pseudomonas aeruginosa (709 bp) product, when amplified with DNA of P. aeruginosa; NC negative control; M marker (100 bp ladder)
Multiplex PCR assay
The multiplex PCR assay was optimized by varying the primer (1.0–10.0 pmol) and MgCl2 concentrations. But bands were distinct when species-specific primers are 2.5 pmol of each primer/reaction, 1.5 mM MgCl2, and annealing at temperature 55 °C. The same conditions were adopted for further studies. The multiplex PCR results determined the presence of four bacterial pathogens in single reaction with varying amplicon sizes P. aeruginosa (709 bp); E. coli (559 bp); S. aureus (461 bp); Salmonella spp. (275 bp), respectively, shown in Fig. 3.
Specificity of multiplex PCR
To ensure the specificity of the primers used in above multiplex PCR assay, primers were cross-examined with other pharma contaminants such as Pseudomonas fluorescence NCIM 2390, Pseudomonas putida NCIM 2650, Pseudomonas stutzeri NCIM 5136, Burkholderia cepacia MTCC 438, Brevundimonas diminuta MTCC 1287, Pseudomonas cepacia NCIM 5089, Enterobacter aerogenes MTCC 2822, Klebsiella pneumoniae MTCC 109, Shigella sonnei MTCC 2957, Citrobacter freundii MTCC 1658, Enterobacter cloacae MTCC 7322, Staphylococcus intermedius MTCC 3050, Stapylococcus epidermidis MTCC 435, Staphylococcus haemolyticus MTCC 3383, and Staphylococcus warneri MTCC 3620 with varying primer concentrations (results not shown). Multiplex PCR was carried out using species-specific primers (2.5 pmol), 1.5 mM MgCl2 and at annealing temperature at 55 °C. The outcome of the experiment concluded that only indicator pathogens P. aeruginosa (709 bp), E. coli (559 bp), S. aureus (461 bp), and Salmonella spp., (275 bp) were amplified and absence of non-specific bands were pictured as shown in lane 1 of Fig 4. We also amplified with the mixture of other pharma contaminants DNA and no bands were seen as shown in NC lane of Fig. 4. We attempted to test the different strains of E.coli (6), S. aureus (6), P.aeruginosa (5), Salmonella spp. (5) and other non-indicator pathogens (15) for determining the specificity of our primers. The results of the strain-specific PCR are tabulated in Table 3.
Sensitivity of multiplex PCR by DNA concentration
The sensitivity of multiplex PCR method was regulated by varying DNA quantity (100–1.56 ng) of each pathogen P. aeruginosa, E. coli, S. aureus, Salmonella spp., 2.5 pmol concentration, 1.5 mM MgCl2 and at annealing temperature at 55 °C. All the indicator pathogens were detected even at 1.56 ng of DNA quantity. There is gradual or distinct decrease in the band intensity when used DNA from higher concentration (100 ng) to lower concentration (1.56 ng) shown in Fig. 5.
Detection of indicator pathogens in artificially inoculated pharma contaminants by multiplex PCR
Fifty samples were spiked with P. aeruginosa, E. coli, S. aureus, Salmonella spp. and the extracted DNA was subjected to multiplex PCR with 2.5 pmol, 1.5 mM MgCl2 concentrations and annealing temperature at 55 °C. Our analysis revealed that multiplex PCR were able to determine less than 2 CFU/g and more than 2 CFU/g of all the four indicator pathogens with distinct amplicon sizes (709, 559, and 461, 275 bp) in artificially contaminated pharmaceutical raw materials and finished products. The results are shown in Fig. 6.
Detection of indicator pathogens in artificially contaminated pharma samples by multiplex PCR. Lane 1, Pseudomonas aeruginosa (709 bp); Escherichia coli (559 bp); Staphylococcus aureus (461 bp); Salmonella spp.(275 bp) products, when amplified with DNA mixture of artificially contaminated (<2 CFU/g) pharma sample; lane 2, P. aeruginosa (709 bp); E. coli (559 bp); S. aureus (461 bp); Salmonella spp.(275 bp) products, when amplified with DNA mixture of artificially contaminated (>2 CFU/g) pharma sample; M marker (100 bp ladder)
Comparison of multiplex PCR vis-a-vis conventional culture method (bacteriological culture-USP)
In this study, we tested 70 possible contaminated raw materials and finished products by employing conventional culture and PCR methods for the presence of indicator pathogens. Our results deduced that only 15 samples of 70 possible contaminants were positive by conventional culture, but by PCR methodology 25 samples were positive out of 70 possible contaminants. Some of the indicator pathogens that were detected from possible contaminants by multiplex PCR are represented in Fig. 7. In artificially contaminated samples, below 2 CFU/g were not detected by conventional method of detection, where as in multiplex PCR, the detection limits have been found to be 1 CFU/g or ml. The current study reveals the necessity of developing multiplex PCR, particularly for bulk pharma testing where specificity, sensitivity, and time are given as prime importance. Comparisons of these two detection modules were represented by statistical bar graph (Fig. 8), which reveals the percentage of each indicator pathogen detected by multiplex PCR in possible contaminants were more sensitive than conventional methods. Out of 70 samples, E. coli was detected in 11%, S. aureus in 11%, P. aeruginosa in 8% and Salmonella spp. in 4% samples (Table 2) by species-specific multiplex PCR.
Possibly contaminated pharma samples were tested for the presence of indicator pathogens. Lane 1, Escherichia coli (559 bp) in lactose; lane 2, Salmonella spp.(275 bp) in Xanthom gum; lane 3, Staphylococcus aureus (461 bp) in mannitol; lane 4, Pseudomonas aeruginosa (709 bp) in maize starch; lane 5 NC negative control; M marker (100 bp ladder)
Discussion
In recent times PCR has been accepted as the method of choice for rapid and reliable detection of microbes in food, water, and pharma samples. This technique can be extremely useful for pure microbial cultures, but when applied directly to food, water, and pharma samples its efficiency can be markedly reduced. The crux of this problem lies in the sample preparation method, which may inadvertently introduce inhibitory substances and preclude the PCR. Appropriate methods have thus been devised to overcome this problem and facilitate the development of PCR-based routine methods for bacterial detection in food, water, and pharma samples [20].
Undoubtedly, simple, rapid, and reproducible test system would enhance the analytical capability of the Food and Drug Administration and consequent consumer protection. To accomplish this goal, preliminary identification of pharma contaminants, standard culture methods were used as screening methods. In this study, uniplex PCR was developed which was further elevated to multiplex PCR for simultaneous detection of indicator pathogens that were evaluated and compared with conventional microbiological tests for their ability to accurately identify the recovered pharmaceuticals and cosmetics containing antimicrobial preservatives.
During this study, a major effort was directed to determine the feasibility of extending the convenience, accuracy, and reproducibility of multiplex PCR for identification of contaminated pharmaceuticals and cosmetics finished products. Apparently, since these industrial indicator pathogens were able to survive in the presence of antimicrobial and various concentrations of alcohols, where conventional methods failed to identify these pathogens because of lack of sensitivity in the adapted methodologies. The current study demonstrates the sensitive methodology to detect indicator pathogens with minimum quantity of DNA (~1 ng). A public health laboratory must be able to quickly and correctly identify isolates to expedite epidemiological investigations and consumer protection. The multiplex PCR is a useful and reliable tool especially for laboratories lacking the equipment or personnel with expertise to apply conventional methods to identify indicator pathogens from non-sterile pharmaceuticals and cosmetics.
More recently, molecular assays such as nucleic acid hybridization techniques (DNA probes) and nucleic acid amplification procedures (PCR) have been developed. PCR has been shown to combine rapid results and high specificity in detecting both pathogenic and spoilage microorganisms [41, 44]. By recognizing conserved genomic DNA sequences unique to a particular organism and amplifying that region of the genome to increase sensitivity, contamination by that organism can be ascertained. Previous work developed primer sequences for the detection of C. jejuni, E. coli O157:H7, and Salmonella [22, 43].
The first PCR application to pharmaceutical quality control has recently been reported. The BAXTM system (Dupont Qualicon, Wilmington, DE), a PCR-based assay for detecting Salmonella spp. was evaluated for pharmaceutical quality control. The technological improvement simplified the PCR analysis by providing a user friendly assay with minimum sample preparation and handling. Using this system [13], detected Salmonella typhimurium, a USP microbial indicator [39], in 25 samples of raw materials and finished products after 24-h enrichment. This represented a faster turn over time than the standard 5–6 day detection time.
Similarly, Jimenez et al. [16] studied the detection time of E. coli, S. aureus, P. aeruginosa, and A. niger in cosmetic/pharma samples and reduced from 6–8 days (standard methods) and by PCR analysis to 24–27 h. In this study, we could able to optimize the detection time for E. coli, Salmonella spp., S. aureus, and P. aeruginosa from 5–7 days to less than 24 h, and simultaneous detection of all four indicator pathogens by multiplex PCR was performed on all artificially contaminated samples. During manufacturing, microorganisms are subjected to processes that might kill or reduce microbial densities. Furthermore, finished products contain preservatives and other antimicrobial components which injure microbes sub-lethally and in some cases require a low nutrient enrichment media to enhance microbial growth [16].
Sample pre-enrichment is the most vital step during isolation of Salmonella spp. from pharma samples. To optimize S. typhimurium PCR detection, particularly in minimal bacterial load samples, a different type of pre-enrichment broth was performed. Buffered peptone water (BPW) was previously used to enhance the recovery of Salmonella spp. in food samples using conventional and PCR methods [8].
The importance of resurgence and recovery procedures availed in food industry has been overlooked in the isolation techniques of pharmaceutical microbiological studies [31]. When pharmaceutical raw materials and products contaminated with mixed bacterial cultures of E. coli, P. aeruginosa, S. aureus, and S. typhimurium were pre-enriched in lactose broth with and without Tween-20, 10 (40%) of 25 samples did not show the presence of the Salmonella spp. The presence of non-Salmonella bacteria influenced the performance of the PCR-based assay was reported [16]. But when the same samples were enriched in BPW, all the samples were shown positive for Salmonella. Jimenez et al. [16] revealed that all ten samples that were shown PCR negative in lactose broth were found to be positive with BPW enrichment medium. BPW enrichment medium increased S. typhimurium bacterial growth resulting in rapid PCR detection. In this study, we used trypticase soy broth containing 4% Tween-20 and 0.5% soy lecithin for enrichment of E. coli, S. aureu, and P.aeruginosa and BPW for S. typhimurium.
Sample preparation prior to PCR analysis can be the most limiting factor during development and optimization of a given PCR assay [14]. To overcome PCR inhibition problems and to increase the sensitivity of the assay, pre-enrichment methods were used. After the enrichment step, sufficient bacteria were grown and allowed the pathogens to be detected by PCR when the original sample had ≤1 CFU/ml. There was no difference in terms of sensitivity, between the phenol–chloroform and the spin column methods of isolating DNA, previously reported [30]. In current study, DNA was extracted from contaminated sample suspensions by using the phenol–chloroform method. With the latest advances in microbial genomics, the availability of primer sequences are limitless, allowing in selecting targets from different loci of bacterial genome reported [16]. In this study, we have designed primers by utilizing Gene Tool Lite (version 1.0) Bioinformatics solution software in conserved regions of respective bacterial genome. The primer sequence, the target, and the PCR product sizes are summarized in Table 1. Initially the uniplex PCR conditions were standardized and revealed that the primers are very sensitive to detect the specific organisms. We further developed multiplex PCR where all four PCR primers have similar melting temperatures (Tm 55 °C) which will simultaneously detect all indicator pathogens. Our current studies were in agreement with the findings of Henegariu et al. [9] that the relative concentrations of the primers were found to be the most important factor in determining approximately equal yields of amplification products from of the each organism in a single reaction.
In previous studies [15] for the detection of E. coli, S. aureus, P. aeruginosa, and A. niger in pharmaceutical samples, simultaneous detection of the pathogens (multiplex PCR) were attempted using RoboCycler 96-gradient PCR with different annealing temperatures of primer profile for E. coli (54 °C), S. aureus (65 °C), P. aeruginosa (55 °C), and A. niger (62 °C), respectively, was reported. In that study they attempted in using different annealing temperatures for detecting E.coli, S. aureus, P.aeruginosa, and A. niger, and moreover gradient PCR in a single PCR run was reported. In current study, we formulated the all four primers will anneal at single temperature (55 °C) not deviating more than ±5 °C. By simultaneously amplifying more than one locus in the same reaction, multiplex PCR is becoming a rapid and convenient screening assay in both the clinical and the research laboratory [9].
Little is known about the factors and common difficulties influencing a multiplex PCR. Other critical factors in multiplex PCR include the concentration of the PCR buffer, the balance between the magnesium chloride and deoxyribonucleotide triphosphate concentrations and the cycling temperatures [9]. The specificity of the primers used in the multiplex PCR assay revealed the absence of non-specific amplification with other food contaminants such as Clostridium perfringens NCIM 2677, Klebsiella pneumonia NCIM 2957, and Shigella sonnei MTCC 2957 (Enterobacteria). The specificity was further validated by sequence analysis of amplified PCR product and NCBI-BLAST.
Jimenez [15] showed simultaneous detection of E.coli, S. aureus, P.aeruginosa, and A. niger with detection levels <10 CFU/g or ml using RoboCycler 96-gradient PCR was reported. But in the present study twin goals were achieved; first the detection limits of multiplex PCR are found to be 1 CFU/g or ml, secondly multiplex PCR method improved the sensitivity of the detection limit by utilizing minimum quantity of DNA (1.56 ng) for all the four indicator pathogens.
Ecactly 35% were detected from possible contaminated samples, of these E. coli were (11%), S. aureus (11%), P. aeruginosa (8%) and Salmonella species (4%) confirmed by multiplex PCR, while only 21% were detected by standard conventional microbiological methods for E.coli (9%), S.aureus (7%), P.aeruginosa (4%), Salmonella spp. (1%) shown in Table 2.
Multiplex method is rapid and the level of sensitivity achieved in our experiments is applicable to the practical survey of microbial contamination in pharma samples. A major outcome of the study is the development of a multiplex PCR to detect multiple pathogens using compatible primers and the DNA extracts from the pharma samples. The implications of the present study are promising and choice of primers in PCR can be extended to detect indicator pathogens present in pharmaceuticals, raw materials, and cosmetic finished products. The use of molecular analyses such as PCR and multiplex assays have resulted in optimization of product manufacturing, quality control evaluation, and product release in cosmetic and pharmaceutical laboratories in few instances. When compared with standard methods, these technologies provide rapid and reliable microbiological monitoring of raw materials, finished products, and water systems allowing faster corrective actions and sample release. Molecular methods have enhanced the ability of an industrial microbiology laboratory to rapidly assess system breakdowns and quality processes.
To optimize pharmaceutical process control, corrective actions must be performed in real time, not after 7 or more days of manufacturing. Rapid methods will identify microbial contamination with detection times ranging from 90 min to 30 h allowing the monitoring of critical control points, reducing losses, and optimizing resources. A recent technical report by the Parenteral Drug Association (PDA) provided some information and guidelines for the evaluation, validation, and implementation of rapid microbiological methods [29]. Further developments in rapid method technologies might lead to online monitoring of pharmaceutical manufacturing and environments.
References
Basset DCJ, Stokes KJ, Thomas WRG (1970) Wound infections due to Pseudomonas multivorans. A water-borne contaminant of disinfectant solutions. Lancet 1:1188–1191. doi:10.1016/S0140-6736(70)91783-6
Berkelman RL, Anderson RL, Davis BJ, Highsmith AK, Petersen NJ, Bono WW et al (1984) Intrinsic bacterial contamination of a commercial iodophor solution. Appl Environ Microbiol 47:752–756
Brasher CW, Depaola A, Jones DD, Bej AK (1998) Detection of microbial pathogens in shellfish with multiplex PCR. Curr Microbiol 37:101–107. doi:10.1007/s002849900346
Casey W, Muth H, Kirby J, Allen P (1998) Use of nonselective preenrichment media for the recovery of enteric bacteria from pharmaceutical products. Pharm Technol 22:114–117
Desvignes AF, Bernard J, Campion G (1973) Etude de la contaminacion microbienne de diverses preparations pharmaceutiques. Ann Pharm Fr 23:775–785
Flickinger B (2000) Making dollars and sense with rapid microbiology. Pharm Qual April/May:22–28
Glencross EJG (1972) Pancreatin as a source of hospital acquired salmonellosis. BMJ 2:376–378
Gouws PA, Visser M, Brszel VS (1998) A polymerase chain reaction procedure for the detection of Salmonella spp. within 24 hours. J Food Prot 61:1039–1042
Henegariu O, Heerema NR, Dlouhy SR, Vance GH, Vogt PH (1997) Multiplex PCR: critical parameters and step-by-step protocol. Biotechniques 23:504–511
Hills S (1946) The isolation of Clostridium tetani from infected talc. Newzealand Med J 45:419–423
Hill WE (1996) The polymerase chain reaction: applications for the detection of food borne pathogens. Crit Rev Food Sci Nutr 36(1–2):123–173
Ignar R, English D, Jimenez L (1998) Rapid detection of microbial contamination in triclosan and high fluoride denitrifices using an ATP bioluminescence assay. J Rapid Methods Autom Microbiol 6:51–58. doi:10.1111/j.1745-4581.1998.tb00183.x
Jimenez L, Smalls S, Scalici C, Bosko Y, Ignar R, English D (1998) Detection of Salmonella spp., contamination in raw materials and pharmaceutical products using the BAX TM system, a PCR assay. J Rapid Methods Autom Microbiol 6:67–76. doi:10.1111/j.1745-4581.1998.tb00185.x
Jimenez L, Ignar R, Smalls S, Grech Hamilton J, Bosko Y, English D (1999) Molecular detection of bacterial indicators in cosmetic/pharmaceutical samples. J Ind Microbiol Biotechnol 21:93–95. doi:10.1038/sj.jim.2900611
Jimenez L (2001) Simultaneous PCR detection of a bacteria and mold DNA sequences in pharmaceutical samples by using a gradient thermocycler. J Rapid Methods Autom Microbiol 9:263–270. doi:10.1111/j.1745-4581.2001.tb00252.x
Jimenez L, Scalici C, Smalls S, Bosko Y, Ignar R (2001) PCR detection of Salmonella typhimurium in Pharmaceutical raw materials and products Contaminated with a mixed bacterial culture using the BAX™ system. PDA J Pharm Sci Technol 55:286–289
Josephson KL, Gerba CP, Pepper IL (1993) Polymerase chain reaction detection of nonviable bacterial pathogens. Appl Environ Microbiol 59:3513–3515
Kallings LO, Ringertz O, Silverstolpe L (1966) Microbiological contamination of medical preparations. Acta Pharmaceu Suet 3:219–228
Knabbel DB, Crawford RL (1995) Extraction and purification of microbial DNA from petroleum-contaminated soils and detection of low numbers of toluene, octane, and pesticide degraders by multiplex polymerase chain reaction and Southern analysis. Mol Ecol 4:579–591. doi:10.1111/j.1365-294X.1995.tb00258.x
Lampel AK, Orlandi PA, Kornegay L (2000) Improved template preparationfor PCR-based assays for detection of food-borne bacterial pathogens. Appl Environ Microbiol 66:4539–4542. doi:10.1128/AEM.66.10.4539-4542.2000
Lang DJ, Kunz LS, Martin AR, Schroeder SA, Thomson LA (1967) Carmine as a source of nosocomial salmonellosis. N Engl J Med 276:829–832
Mahon J, Murphey CK, Jones PW, Barrow PA (1994) Comparison of multiplex PCR and standard bacteriological methods of detecting Salmonella on chicken skin. Lett Appl Microbiol 19:169–172. doi:10.1111/j.1472-765X.1994.tb00934.x
Mahony JB, Luinstra KE, Tyndall M, Sellors JW, Krepel J, Chernesky M (1995) Multiplex PCR for detection of Chlamydia trachomatis and Nesseria gonorrhoeae in genitourinary specimens. J Clin Microbiol 33:3049–3053
Martinez-Bermudez A, Rodriguez de Lecea J, Soto-Esteras T, Vazquez-Estevez C, Chena-Canete C (1991) Tipos de contaminantes microbianos de materias primas farmaceuticas. Rev Latinoam Microbiol 33:153–157
Mestrandrea LW (1997) Microbiological monitoring of environmental conditions for nonsterile pharmaceutical manufacturing. Pharmaceu Technol 21:59–74
Mitchell RG, Hayward AC (1966) Postoperative urinary tract infection caused by contaminating irrigation fluid. Lancet 9i:793–795. doi:10.1016/S0140-6736(66) 91866-6
Orth DS (1989) Microbiological considerations in cosmetic formula development and evaluation. I. Microbiological quality of a product. Cosmet Toilet 104:49–64
Palmieri MJ, Carito SL, Meyer RF (1988) Comparison of rapid NFT and API 20E with conventional methods for identification of gram-negative nonfermentative bacilli from pharmaceuticals and cosmetics. Appl Environ Microbiol 54:2838–2841
PDA (2000) “Evaluation, validation, and implementation of new microbiological testing methods,” PDA Technical Report #33. PDA J Pharmaceu Sci and Technol 54
Phuektes P, Mansell PD, Browning GF (2001) Multiplex polymerase chain reaction assay for Simultaneous detection of S. aureus and streptococcal causes of bovine mastitis. J Dairy Sci 84:1140–1148
Ray B (1986) Impact of bacterial injury and repair in food microbiology: Its past, present and future. J Food Prot 49:651–655
Read RB (1984) Bacteriological analytical manual. 6th ed:1–19
Russell M (1988) Microbiological control of raw materials. In: Bloomfield SF, Baird R, Lear RE, Leech R (eds) Microbial quality assurance in pharmaceuticals, Cosm and Toiletries. Ellis Horwood, Chichester, pp 35–48
Safranek TJ, Jatvis WR, Carson LA, Cusick LB, Silcox VA (1987) Mycobacterium chelonae wound infections after plastic surgery employing contaminated gentiane violet skin marking solutions. N Engl J Med 317:197–201
Sutton SVW, Magee MA, Brannan DK (1997) Cosmetic microbiology, A practical handbook. In: Brannan DK (ed), CRC Press, New York pp 96–122
Underwood E (1992) Ecology of microorganisms as it affects the pharmaceutical industry. In: Hugo WB, Russell AD (eds) Pharmaceu Microbiol. Blackwell, Oxford, pp 353–368
Underwood E (1998) Pharmaceutical Microbiology, 6th edn. In: Hugo WB, Russel AD (eds) Blackwell Science, Oxford, pp 339–354
U.S Pharmacopeial Convention Inc. (1985) The United States pharmacopeia XXI revision and the national formulary, 16th edn., p 1151–1156
United States Pharmacopeial Convention (2000) Microbial test limits, In: U.S. Pharmacopoeia. United States Pharmacopeial Convention, Rockville, 24:1814–1818
Van Der Zee H, Huis in’t Veld JH (1997) Rapid and alternative screening methods for microbiological analysis. J AOAC 80:934–940
Waage AS, Vardund T, Lund V, Kapperud G (1999) Detection of small numbers of Campylobacter jejuni and Campylobacter coli cells in environmental water, sewage, and food samples by a seminested PCR assay. Appl Environ Microbiol 65:1636–1643
Wilson IG (1997) Inhibition and facilitation of nucleic acid ampli®cation. Appl Environ Microbiol 63:3741–3751
Winters DK, Slavik MF (1995) Evaluation of a PCR-based assay for specific detection of Campylobacter jejuni in chicken washes. Mol Cell Probes 9:307–310. doi:10.1016/S0890-8508(95) 91556-7
Winters DK, O’Leary AE, Slavik MF (1998) Polymerase chain reaction for rapid Detection Of Campylobacter jejuni in artificially contaminated foods. Lett Appl Microbiol 27:163–167. doi:10.1046/j.1472-765X.1998.00411.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karanam, V.R., Reddy, H.P., Subba Raju, B.V. et al. Detection of indicator pathogens from pharmaceutical finished products and raw materials using multiplex PCR and comparison with conventional microbiological methods. J Ind Microbiol Biotechnol 35, 1007–1018 (2008). https://doi.org/10.1007/s10295-008-0376-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10295-008-0376-z