Abstract
Complex and bidirectional interactions between the renin–angiotensin system (RAS) and autonomic nervous system have been well established for cardiovascular regulation under both physiological and pathophysiological conditions. Most research to date has focused on deleterious effects of components of the vasoconstrictor arm of the RAS on cardiovascular autonomic control, such as renin, angiotensin II, and aldosterone. The recent discovery of prorenin and the prorenin receptor have further increased our understanding of RAS interactions in autonomic brain regions. Therapies targeting these RAS components, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers, are commonly used for treatment of hypertension and cardiovascular diseases, with blood pressure-lowering effects attributed in part to sympathetic inhibition and parasympathetic facilitation. In addition, a vasodilatory arm of the RAS has emerged that includes angiotensin-(1–7), ACE2, and alamandine, and promotes beneficial effects on blood pressure in part by reducing sympathetic activity and improving arterial baroreceptor reflex function in animal models. The role of the vasodilatory arm of the RAS in cardiovascular autonomic regulation in clinical populations, however, has yet to be determined. This review will summarize recent developments in autonomic mechanisms involved in the effects of the RAS on cardiovascular regulation, with a focus on newly discovered pathways and therapeutic targets for this hormone system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease remains the leading cause of morbidity and mortality in the United States, despite decades of research into underlying mechanisms and optimal treatment approaches. In this regard, the renin–angiotensin system (RAS) has remained a focus of cardiovascular research for over a century. The RAS is well recognized for its importance in physiological regulation of blood pressure, extracellular volume, and cardiovascular control of neural and endocrine functions. In addition, the RAS has been shown to play a pathophysiological role in the development and progression of numerous cardiovascular-related diseases including hypertension, heart failure, obesity, chronic kidney disease, coronary artery disease, and stroke. As a result, pharmacological agents targeting the RAS are increasingly used in these clinical populations. At a mechanistic level, the cardiovascular regulatory actions of the RAS involve extensive interactions with the autonomic nervous system. This review will highlight recent developments in our understanding of these RAS–autonomic interactions for cardiovascular control, along with a discussion of potential implications for targeting the RAS to improve cardiovascular autonomic regulation in clinical populations.
RAS pathways for cardiovascular regulation
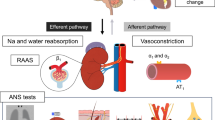
The RAS is a series of enzyme–substrate interactions that generates functional peptide hormones critical to physiological and pathophysiological regulation of cardiovascular function. The enzyme renin, an aspartyl protease, is synthesized and released from the juxtaglomerular cells of the kidneys in response to various stimuli including increased sympathetic nervous system (SNS) activity, decreased perfusion pressure in the renal afferent arterioles, decreased sodium chloride content in the macula densa segment of the renal distal tubules, and local actions of nitric oxide and prostanoids [1]. As shown in Fig. 1, renin catalyzes the conversion of angiotensinogen to the decapeptide angiotensin (Ang) I, which is subsequently cleaved by angiotensin-converting enzyme (ACE) to form the octapeptide Ang II [2]. In addition to this classical circulating system, components of the RAS are found locally within tissue systems such as brain, heart, kidney, adipose, skeletal muscle, and adrenal gland [2]. The existence and independence of these local RAS from the circulating system, however, has been challenged, with studies showing that while tissue Ang II generation does occur via actions of membrane-bound ACE, this process requires uptake of renin and angiotensinogen from the circulation [3]. The presence of an intracellular RAS has also been described in cardiac myocytes, vascular smooth muscle cells, renal proximal tubule cells, and neurons [4, 5]. In this intracellular RAS, Ang II can be generated within cells or internalized by cells following activation of cell surface receptors to elicit intracrine effects via AT1-like nuclear receptors. Finally, ACE-independent pathways can contribute to Ang II generation, particularly within tissues, and involve actions of proteinases such as chymase, kallikrein, and cathepsin G [6].
Overview of renin–angiotensin system formation and degradation pathways showing primary receptor-mediated cardiovascular and autonomic effects. Angiotensin-converting enzyme (ACE), neprilysin (NEP), propyl oligopeptidase (POP), thimet oligopeptidase (TOP), mononuclear leukocyte-derived aspartate decarboxylase (MLDAD), angiotensin type 1 receptor (AT1R), angiotensin type 2 receptor (AT2R), aminopeptidase A (APA), mas receptor (MasR), mas-related G-protein coupled receptor member D (MrgD), parasympathetic nervous system (PSNS), sympathetic nervous system (SNS), and antidiuretic hormone (ADH)
Ang II has primary actions at cell surface type 1 (AT1) G-protein coupled receptors to elevate blood pressure via numerous mechanisms including vasoconstriction, cellular proliferation, aldosterone and vasopressin release, oxidative stress, inflammation, immune activation, sympathetic activation, and baroreflex dysfunction [2]. While this is an understudied area of research, a handful of studies have also shown a role for intracellular Ang II in inducing cardiac hypertrophy and pressor responses via actions at nuclear AT1 receptors in rodents [7]. Ang II can also bind type 2 (AT2) receptors to counteract AT1 receptor-mediated vasoconstrictor and proliferative actions, although these receptors are more limited in terms of affinity and tissue expression [8]. Ang II is degraded by aminopeptidase A and N to form the active metabolites Ang III and Ang IV, respectively. Most biological actions of Ang III are mediated by AT1 receptors and include promotion of cellular proliferation, vasopressin release, thirst and sodium appetite, inflammation, and aldosterone release [9]. Ang III is reported to have similar affinity for AT1 receptors and to produce equipotent pressor responses compared with Ang II, although this remains an area of active debate [9, 10]. While less studied, Ang IV can also activate AT1 receptors centrally to induce hypertension in animal models [10] as well as Ang type 4 (AT4) receptors to modulate learning and memory functions.
The complexity of the Ang II-ACE-AT1 receptor vasoconstrictor arm of the RAS is further increased by the recent discovery of additional biologically active components including Ang-(1–12), prorenin and the prorenin receptor (Fig. 1). Ang-(1–12) is a C-terminally extended form of Ang I that is found in plasma and peripheral tissues, formed independent of renin, and processed to Ang II for cardiovascular actions [11]. Prorenin is an inactive precursor of renin, which contains a 43-amino acid prosegment covering the active cleft, and is found in the circulation at concentrations at least tenfold higher than renin. Renin and prorenin can both bind the prorenin receptor (PRR). Binding of prorenin to the PRR induces non-proteolytic activation to contribute to Ang II production in tissues, and also initiates intracellular signaling independent of Ang II actions [12].
Finally, a vasodilatory arm of the RAS has emerged, which is characterized by the heptapeptide Ang-(1–7) and generally opposes the deleterious cardiovascular actions of Ang II. Ang-(1–7) is formed from Ang II degradation by ACE2 or from cleavage of Ang I by various endopeptidases including neutral endopeptidase (NEP), prolyl oligopeptidase, and thimet oligopeptidase. In addition, Ang I can be converted by ACE2 to Ang-(1–9), which in turn can be cleaved by NEP or ACE to form Ang-(1–7). In animal models, Ang-(1–7) lowers blood pressure and induces cardioprotective effects through vascular, cardiac, renal, and neural mechanisms [13]. The literature suggests that most, if not all, of the physiological cardiovascular actions of Ang-(1–7) are mediated through mas G-protein coupled receptors [13]. A few recent studies, however, provide evidence of potential heterodimerization and functional interactions between mas and AT2 receptors, as well as a role for Ang-(1–7) in antagonizing AT1 receptor-mediated signaling [14, 15]. More recently, the endogenous heptapeptide alamandine was identified in human blood [16]. Alamandine is formed primarily from cleavage of Ang A via ACE2, but also from decarboxylation of Ang-(1–7) (Fig. 1). Alamandine differs from Ang-(1–7) only in its N-terminal amino acid [Ala1 versus Asp1 for Ang-(1–7)], and binds mas-related G-protein coupled receptor D (MrgD) to elicit vasodilatory and antihypertensive actions, similar to Ang-(1–7) [17].
RAS and autonomic interactions in cardiovascular control
Ang II pathways
In addition to actions on the vasculature, kidneys, adrenal glands, and heart, an important mechanism by which the RAS contributes to cardiovascular regulation is through modulation of the autonomic nervous system. The autonomic nervous system regulates cardiovascular function via coordinated actions of (1) afferent autonomic neural pathways signaling distension of the great vessels and cardiac chambers, and (2) efferent pathways transmitting sympathetic and parasympathetic outflow to cardiovascular end organs such as the heart and vasculature. Most research to date has focused on the bidirectional stimulatory interactions between Ang II and the SNS. Renal sympathetic innervation is a major determinant of β1-adrenergic receptor-mediated renin release, thus contributing to the control of circulating Ang II levels (Table 1; Fig. 2). Consistent with this, renal denervation or electrical activation of the carotid baroreflex to suppress efferent sympathetic outflow reduces circulating renin activity, Ang II, and aldosterone in experimental animal models and patients with resistant hypertension [18, 19].
Bidirectional interactions between the renin–angiotensin and autonomic nervous systems. The sympathetic nervous system is a major determinant of renin release from the kidneys via norepinephrine actions on beta-1 adrenergic receptors in juxtaglomerular cells. Renin is a key enzyme catalyzing formation of angiotensin I from angiotensinogen, which is subsequently cleaved to form angiotensin II and angiotensin-(1–7). These angiotensin peptides can act at AT1 and mas receptors distributed throughout autonomic nervous system pathways (e.g., vagal afferents, nodose ganglion, regulatory brain regions, and sympathetic preganglionic neurons, ganglia, and nerve terminals) to influence sympathetic noradrenergic and parasympathetic cholinergic neurotransmission to cardiovascular end organs such as the heart, kidneys, and vasculature. Nucleus tractus solitarius (nucleus of the solitary tract; NTS), rostral ventrolateral medulla (RVLM), caudal ventrolateral medulla (CVLM), dorsal motor vagus (DMV), nucleus ambiguous (NA), glossopharyngeal nerve (CN IX), vagus nerve (CN X), beta-1 adrenergic receptor (β1), alpha-1 adrenergic receptor (α1), and muscarinic acetylcholine receptor (mAChR)
Conversely, Ang II AT1 receptors are abundant at each synaptic relay of the autonomic nervous system (e.g., preganglionic neurons, ganglia, nerve terminals, regulatory brain regions), to influence sympathetic and parasympathetic neurotransmission (Fig. 2) [20]. Ang II enhances SNS neurotransmission by stimulating presynaptic release of norepinephrine and epinephrine from sympathetic nerves, facilitating sympathetic ganglionic transmission, inhibiting norepinephrine reuptake in nerve terminals, increasing the density of sympathetic innervation in cardiovascular end organs, and enhancing vasoconstrictor responses to norepinephrine (Table 1; Fig. 2) [21]. The physiological importance of this sympathetic activation to the pressor effects of exogenous Ang II, however, remains controversial [21, 22]. This may reflect differences in the animal models used, sites and routes of administration, rates of infusion, and time course of studies. In particular, higher pharmacological doses of Ang II are often required to increase sympathetic outflow [21]. Despite this, emerging evidence suggests that activation of endogenous central angiotensinergic pathways (either through increased Ang II production or enhanced AT1 receptor expression and signaling) contributes to sympathetic hyperactivity and hypertension induced by high-salt diet, obesity, or cold exposure, and heart failure [23].
While Ang II does not readily cross the blood–brain barrier, it can be formed directly within the brain or can access the central nervous system via AT1 receptors distributed to circumventricular organs including the subfornical organ (SFO), area postrema, median eminence, and organum vasculosum of the lamina terminalis (OVLT) [24]. These circumventricular organs send efferent projections to brain regions implicated in the cardiovascular autonomic actions of Ang II including the arcuate (ARC) and paraventricular (PVN) nuclei of the hypothalamus, as well as the solitary tract nucleus [nucleus tractus solitarius] (NTS), caudal ventrolateral medulla (CVLM), and rostral ventrolateral medulla (RVLM) of the brainstem. The RVLM contains sympathetic premotor neurons that project to the intermediolateral column of the spinal cord, to influence sympathetic vasomotor tone. Ang II AT1 receptor-mediated activation of SFO/OVLT-PVN-RVLM pathways has been widely implicated in animal models of hypertension [25]. The actions of Ang II at AT1 receptors in the PVN and RVLM rapidly contribute to sympathoexcitation and hypertension in rats, in part by stimulating oxidative stress and immune pathways [25]. As recently reviewed, Ang II stimulates AT1 receptor-mediated oxidative stress to increase intracellular calcium, which inhibits voltage-gated potassium channels to increase spontaneous neuronal action potentials and firing [23]. This results in activation of glutamatergic and inhibition of GABAergic interneurons contributing to presympathetic neuron activation to increase SNS activity and elevate blood pressure. Similar to Ang II, Ang-(1–12) administration in the ARC, PVN, or RVLM increases blood pressure, heart rate, and sympathetic nerve activity [26]. The blood pressure and sympathetic effects of both Ang II and Ang-(1–12) are prevented by central administration of ACE inhibitors or AT1 receptor blockers (ARBs).
Ang II also impairs arterial baroreceptor reflex function in animal models, to allow for unrestrained sympathetic activation, by resetting the set point to higher levels of pressure as well as decreasing the baroreflex sensitivity [21, 26]. These baroreflex inhibitory effects are primarily mediated by actions of Ang II on the brain to reduce efferent vagal tone to the heart, although a few reports have suggested direct actions of Ang II in inhibiting the firing of aortic arch baroreceptors or the vagus nerve [21]. The effects of Ang II on baroreflex function involve the NTS, a brainstem region that is the first central locus receiving afferent baroreceptor input. Several neuropeptide or intracellular mediators are implicated in the ability of Ang II to suppress baroreflex function, including substance P, nitric oxide pathways, GABA release, the Rho kinase pathway, and endocannabinoids [20, 27,28,29]. Ang-(1–12) also impairs baroreflex sensitivity for control of heart rate and sympathetic activity when given in the NTS and CVLM, respectively, with effects requiring conversion to Ang II by ACE or chymase and subsequent binding to AT1 receptors [26, 30].
Similar to Ang II, Ang III can act at AT1 receptors distributed to autonomic nervous system pathways to facilitate postsynaptic noradrenergic neurotransmission, and inhibit the parasympathetic component of the arterial baroreceptor reflex [9, 10]. When administered directly into the brain, Ang III increases blood pressure and renal sympathetic nerve activity in anesthetized rats, to a similar magnitude as Ang II and with responses exacerbated under high sodium conditions [31]. The duration of pressor and sympathoexcitatory responses elicited by Ang III is shorter compared to Ang II, however, due to a reduced half-life. Central Ang III also exerts tonic stimulatory control of blood pressure in hypertensive rats, and contributes to sympathetic hyperactivity and cardiac dysfunction in a rat model of myocardial infarction [32, 33]. Interestingly, it has been proposed that Ang III is the major bioactive peptide of the brain RAS, and that Ang II requires conversion to Ang III to elicit AT1 receptor-mediated pressor and dipsogenic responses. This hypothesis is based primarily on findings that aminopeptidase inhibitors attenuate pressor responses to Ang II; however, this remains controversial [34].
The evidence for RAS–autonomic interactions in humans is more tenuous, with acute Ang II administration producing inconsistent effects on sympathetic neural outflow and adrenal medullary catecholamine secretion in healthy subjects and patients with essential hypertension [21, 35,36,37]. This may reflect a reflexive decrease in sympathetic activity in response to the pressor response produced by peripheral Ang II administration, regional differences in changes in sympathetic outflow, limitations in the route and duration of administration in humans, and difficulties with quantitatively assessing cardiovascular autonomic activity in humans. Despite conflicting findings for sympathetic tone, Ang II has been found to alter the operating point and sensitivity of the arterial baroreceptor reflex in clinical populations [35, 36, 38, 39]. There is currently no information on the role of other components of Ang II pathways, such as Ang-(1–12) or Ang III, in cardiovascular control in humans.
Aldosterone
Ang II is a major stimulus for the secretion of aldosterone, a steroid hormone produced by the zona glomerulosa of the adrenal cortex. Classically, aldosterone activates nuclear mineralocorticoid receptors (MR) in the distal tubules and collecting ducts of the nephron to promote sodium retention and elevate blood pressure via genomic mechanisms. Aldosterone can also activate cell surface MR to promote vasoconstriction via more rapid non-genomic mechanisms [40]. In addition to direct renal and vascular actions, emerging evidence suggests that aldosterone activates brain MR to contribute to sympathetic activation, blood pressure elevation, and augmentation of the exercise pressor reflex in animal models of hypertension and heart failure [23, 25, 41]. Circulating aldosterone accesses neurons in the brain via MR distributed to circumventricular organs such as the SFO and OVLT, and the hypertensive effects of systemic aldosterone administration are attenuated by SFO lesions [23]. Aldosterone is also produced locally in the brain and can activate central MR to induce slower neuromodulatory effects to increase activity of epithelial sodium channels, resulting in release of endogenous ouabain from magnocellular neurons in the PVN. In addition, aldosterone increases expression of Ang II pathway components (e.g., ACE, AT1 receptors) and oxidative stress, to enhance angiotensinergic signaling and elevate blood pressure and sympathetic activity via an AT1 receptor-mediated mechanism [23]. Few studies have examined effects of aldosterone administration on cardiovascular autonomic regulation in clinical populations. A handful of studies have shown no effect of acute intravenous aldosterone infusion on muscle SNS activity, with either impairment or improvement of cardiac vagal tone, in healthy subjects [42,43,44,45]. Patients with aldosterone-producing adenoma, however, have increased muscle sympathetic nerve activity that is normalized following unilateral adrenalectomy, suggesting central sites of action for circulating aldosterone in humans [23]. The effects of blocking endogenous aldosterone actions with MR antagonists on cardiovascular autonomic control are discussed in the clinical implications section of this review.
Prorenin and prorenin receptor
While the importance of the brain RAS in hypertension is well recognized, there is low renin expression within the central nervous system for local Ang II formation. PRR is highly expressed in the brain and can bind renin and prorenin to increase catalytic efficiency for Ang II biosynthesis, as well as initiate intracellular signaling independent of Ang II [46]. Recent studies have begun to elucidate the role of the PRR in neural control of cardiovascular function, particularly related to the pathogenesis of neurogenic hypertension. In hypertensive rodents, PRR gene expression is upregulated in neurons in cardiovascular autonomic regulatory brain regions, including supraoptic nucleus, SFO, and PVN [47, 48]. In anesthetized rats, microinjection of human prorenin in the PVN increases splanchnic sympathetic nerve activity via direct PRR signaling [49]. Conversely, in hypertensive rodents, brain-targeted PRR inhibition attenuates hypertension, cardiac and vasomotor sympathetic tone, vasopressin release, and baroreflex dysfunction [50, 51]. Deleterious effects of prorenin on cardiovascular autonomic regulation involve increased Ang II formation, and potential direct effects to stimulate proinflammatory cytokines, reactive oxygen species, and microglia [49, 52]. In addition, prorenin increases firing activity of magnocellular and parvocellular neurons in the PVN via Ang II-dependent and Ang II-independent mechanisms, respectively, by increasing intracellular calcium to inhibit voltage-gated potassium currents [53].
Ang-(1–7) pathways
The search for an understanding of potential interactions between Ang-(1–7) and the autonomic nervous system has emerged as an important, yet understudied, area of research. Similar to Ang II AT1 receptors, Ang-(1–7) mas receptors are distributed to all pathways of the autonomic nervous system, including preganglionic neurons, ganglia, and nerve terminals, and in circumventricular organs and regulatory brain regions including the NTS, PVN, and RVLM [20, 54]. In terms of interactions with the SNS, Ang-(1–7) enhances norepinephrine reuptake and reduces evoked norepinephrine release from the hypothalamus and mesenteric arteries of hypertensive rats [55]. In addition, Ang-(1–7) reduces sympathetic nerve proliferation in the atria in a canine model of chronic atrial tachycardia [56]. While producing no effect on blood pressure in normal rodents, perhaps due to restraint of vasodilatory actions by arterial baroreflex buffering, chronic central Ang-(1–7) infusion lowers blood pressure in hypertensive animal models [55]. These blood pressure-lowering effects are associated with reductions in cardiac and renal sympathetic nerve activity and improvements in heart rate variability and the arterial baroreflex sensitivity for control of both heart rate and renal sympathetic nerve activity [26, 55]. Similarly, the nonpeptide Ang-(1–7) receptor agonist AVE0991 lowers blood pressure and improves baroreflex sensitivity in hypertensive rats [55]. Ang-(1–7) also attenuates cardiac and renal sympathetic responses to an acute emotional stressor in rats [57]. Conversely, global mas receptor knockout in mice reduces baroreflex sensitivity, implicating a protective role for endogenous Ang-(1–7) actions in cardiac autonomic tone [58]. Discordant effects can be observed, however, when Ang-(1–7) is administered directly into cardiovascular regulatory brain regions [26]. Similar to Ang II, microinjection of Ang-(1–7) in the NTS and CVLM produces depressor and bradycardic effects, whereas administration in the PVN and RVLM increases blood pressure, renal and splanchnic nerve activity, and cardiac sympathetic afferent reflex [59, 60]. The hypertensive and sympathoexcitatory effects of Ang-(1–7) in the RVLM are reported to involve activation of mas receptors on glial cells to engage glutamatergic and adenosine triphosphate-mediated mechanisms [59].
Another component of the Ang-(1–7)-forming axis, ACE2, is found in neurons and astroglial cells in cardiovascular brain regions including the OVLT, SFO, PVN, RVLM, and NTS [54]. ACE2 expression is reduced in these brain regions in animal models of hypertension and heart failure. ACE2 overexpression in the brain lowers blood pressure and reduces urinary norepinephrine excretion and renal sympathetic nerve activity in these models [61]. In addition, either ACE2 overexpression or the small molecule ACE2 activator XNT improves cardiac autonomic balance in response to diabetes and emotional stressors in animals [61]. Conversely, ACE2 genetic deletion or pharmacological inhibition elevates blood pressure, increases cardiac sympathetic tone, and reduces baroreflex sensitivity. While the beneficial effects of ACE2 on cardiovascular autonomic tone could be due to either reduced Ang II or increased Ang-(1–7) formation, most of these effects are blocked by the mas receptor antagonist A779, suggesting Ang-(1–7)-mediated mechanisms [61]. Similar to Ang-(1–7), central alamandine infusion improves baroreflex sensitivity for control of heart rate [17]. Alamandine, however, also has site-specific cardiovascular effects by acting at MrgD within the CVLM and RVLM to produce vasodilation and decrease blood pressure [16], and by acting in the PVN to increase blood pressure and renal sympathetic nerve activity [62].
Taken together, the cardiovascular actions of Ang-(1–7) and components of the protective counter-regulatory arm of the RAS appear to involve modulation of sympathetic and parasympathetic tone. Additional research is needed, however, to better understand site-specific actions of Ang-(1–7) in autonomic brain regions, as well as the magnitude and relative importance of autonomic mechanisms with regard to the cardiovascular effects of this hormone, particularly in the context of cardiovascular pathophysiology.
Clinical implications of targeting the RAS
The literature provides strong evidence for facilitatory RAS–autonomic interactions in cardiovascular pathophysiology in animal models; however, these findings do not always translate to clinical studies. While there is general consensus that the blood pressure-lowering effects of RAS blockers involve modulation of the autonomic nervous system, the magnitude of this mechanism remains unclear due to the heterogeneity of responses among clinical trials. This may reflect differences in the route, dose, and duration of treatment, limitations of current methods to quantitatively measure cardiovascular autonomic activity in humans, and incomplete RAS inhibition resulting from the lower doses in clinical use, low brain or tissue penetration, an inability to enter the cell due to low lipophilicity to modulate intracellular RAS activity, or reactive increases in plasma renin activity or Ang I to activate non-canonical and/or tissue RAS pathways [63, 64]. Of interest, RAS blockers attenuate but often fail to normalize sympathetic overactivity and blood pressure in essential hypertension, potentially placing patients at residual risk for major cardiovascular events [65]. Additionally, sympathetic and RAS overactivity is exacerbated in patients with comorbid risk factors (e.g., cardiac hypertrophy, obesity, metabolic syndrome, renal failure, chronic heart failure), with beneficial cardiovascular effects of RAS blockade often magnified under these conditions.
ACE inhibitors and angiotensin receptor blockers
Pharmacological therapies blocking Ang II activity are widely used in the treatment of essential hypertension and cardiovascular-related diseases, due to their protective effects on blood pressure and cardiovascular end organs. These therapies are also often used in obese and type 2 diabetic patients due to their beneficial metabolic profile, including the ability to improve insulin sensitivity and reduce the incidence of new-onset diabetes in controlled clinical trials [66, 67]. The two main classes of drugs used clinically for inhibiting Ang II activity are ARBs and ACE inhibitors [68]. ARBs prevent the ability of Ang II to bind AT1 receptors and initiate intracellular signaling, while ACE inhibitors competitively block ACE to prevent Ang II formation from Ang I. These therapies also shift the balance of the RAS to increase circulating levels of Ang-(1–7), which may contribute to their beneficial cardiovascular effects [69,70,71]. ACE inhibitors block Ang II formation and Ang-(1–7) degradation by ACE to shunt metabolism towards Ang-(1–7) production. ARBs produce reflexive increases in plasma renin activity and ineffective Ang II, resulting in increased Ang-(1–7) formation. Some studies have shown neutral effects of ACE inhibitors and ARBs on measures of sympathetic tone such as plasma norepinephrine and muscle sympathetic nerve activity in clinical populations [37, 72,73,74,75,76]. The collective literature, however, suggests that the beneficial effects of these therapies on blood pressure are, at least in part, due to cardiovascular autonomic mechanisms (Table 2) [62]. ACE inhibitors and ARBs reduce both central sympathetic neural discharge and norepinephrine spillover rates, and improve tissue clearance at peripheral nerve terminals in essential hypertension [65]. These therapies also improve the gain and set point of the arterial baroreflex for control of heart rate and sympathetic activity to preserve autonomic reflex control.
The beneficial cardiovascular autonomic effects of ACE inhibitors and ARBs appear magnified in conditions with exaggerated sympathetic overactivity or baroreflex dysfunction such as obesity, congestive heart failure, chronic renal disease, and primary autonomic failure [65, 77, 78]. Obesity is associated with sympathetic and RAS overactivity, both of which can be attenuated by lifestyle modifications such as weight loss or by pharmacological RAS blockade [79,80,81]. Interestingly, depressor and sympathoinhibitory effects of weight loss are amplified in obese hypertensive subjects when combined with ACE inhibition, by reducing circulating RAS overactivation as well as hyperleptinemia [81]. In heart failure, ACE inhibitors and ARBs reduce muscle SNS activity (measured by microneurography) and improve cardiac SNS activity (measured by 123I-meta-iodobenzylguanidine scintigraphy) and enhance the baroreflex sensitivity for control of heart rate [82]. In chronic kidney disease, these therapies reduce, but do not normalize, blood pressure and sympathetic activity [83]. Based on this, recent studies have examined combination ARB and sympatholytic treatment, and have shown greater sympathoinhibitory effects compared with either drug alone in selected patients with chronic renal disease [77]. Finally, acute administration of the ARB losartan reduces nocturnal blood pressure and pressure natriuresis in patients with primary autonomic failure, without worsening morning orthostatic tolerance [78]. Of interest, primary autonomic failure is often associated with undetectable plasma renin activity due to loss of renal sympathetic innervation, suggesting non-canonical and renin-independent pathways for Ang II formation in these patients.
Direct renin inhibitors
Direct renin inhibitors offer a therapeutic approach to potentially achieve more complete RAS inhibition. Aliskiren is a first-in-class nonpeptide orally active renin inhibitor that binds renin and non-proteolytically activated prorenin to prevent cleavage of angiotensinogen to Ang I, to ultimately reduce Ang II formation. Aliskiren elicits sustained antihypertensive effects in clinical populations [84]; however, this drug has increased side effects compared with ACE inhibitors and ARBs, as well as contraindications in patients with diabetes or moderate to severe renal impairment. In hypertensive rats, centrally administered aliskiren lowers blood pressure, in part by reducing renal sympathetic nerve activity and restoring arterial baroreflex function (Table 2) [85]. The ability of aliskiren to inhibit sympathetic tone in patients with hypertension remains controversial. While a few studies provide evidence that aliskiren reduces resting and upright muscle sympathetic nerve activity in hypertensive subjects [86, 87], others show no effect in attenuating sympathetic activation produced by amlodipine or cold pressor test [88, 89]. In terms of parasympathetic function, aliskiren restores the arterial baroreflex sensitivity in rats with renovascular hypertension, and improves heart rate responses to deep breathing (sinus arrhythmia) in patients with diabetes [90, 91]. These limited studies suggest that the blood pressure-lowering effects of renin inhibition involve improved cardiovascular autonomic tone (Table 2); however, further research is needed. In this regard, an active clinical trial is examining effects of aliskiren versus the centrally acting α2-adrenergic agonist clonidine on endothelial function and muscle sympathetic nerve activity in obesity hypertension (NCT01983462).
Mineralocorticoid receptor antagonists
The MR is a steroid hormone receptor that can bind aldosterone, Ang II, cortisol or other hormone-independent ligands to promote hypertension via genomic and non-genomic mechanisms [92]. Spironolactone is a first-generation nonselective MR antagonist limited by anti-androgenic side effects including gynecomastia, breast tenderness, and erectile dysfunction. Eplerenone is a second-generation highly selective competitive MR antagonist with a more rapid time course to reach peak plasma concentrations and reduced side effects compared with spironolactone [93]. These MR antagonists effectively lower blood pressure and improve vascular function, particularly in drug-resistant and low-renin forms of essential hypertension [94]. Acute eplerenone also reduces nocturnal blood pressure in primary autonomic failure, implicating a role for MR activation in supine hypertension in these patients [95]. Chronic central MR antagonism lowers blood pressure, reduces efferent sympathetic discharge, and attenuates exaggerated exercise pressor reflex responses in rodent models of hypertension, myocardial infarction, and heart failure (Table 2) [23, 41]. Furthermore, spironolactone enhances cardiac vagal tone and renal baroreceptor reflex sensitivity in rodent models, suggesting improved parasympathetic function [96, 97]. In patients with hypertension, spironolactone lowers blood pressure, reduces plasma norepinephrine levels, and attenuates diuretic-induced sympathetic activation, with neutral effects on muscle sympathetic nerve activity (Table 2) [23]. Spironolactone also improves heart rate variability and blunts the morning surge in heart rate associated with sympathetic reactivity in patients with heart failure, suggesting improved cardiac sympathovagal balance [82, 98]. Current clinical trials are investigating the effects of eplerenone on exercise-induced sympathetic and pressor responses in essential hypertension and primary aldosteronism (NCT01996449), as well as the effects of spironolactone on baroreflex sensitivity and muscle sympathetic nerve activity during controlled hypoglycemia in healthy subjects (NCT03429946). While third-generation non-steroidal selective MR antagonists have been developed, they have not yet been marketed. It has been suggested that newer MR antagonists are needed that preferentially target inflammatory, pro-fibrotic, and potentially sympathoexcitatory effects of MR activation, without effects on renal potassium excretion or brain centers involved in normal physiological regulation of affect, stress, learning, and memory (e.g., cortical and hippocampal neurons) [99].
Dual neprilysin and angiotensin receptor inhibitor
NEP is an enzyme that degrades numerous vasodilatory and natriuretic hormones (e.g., natriuretic peptides, bradykinin, substance P), as well as reducing Ang II and increasing Ang-(1–7) formation. While NEP inhibition increases the bioavailability of these circulating vasodilatory and natriuretic mediators, clinical studies have not shown blood pressure-lowering effects of neprilysin inhibitors when administered alone, in part due to the increase in Ang II levels produced by these therapies. Therefore, combination therapies were developed to enhance the endogenous natriuretic peptide system to promote vasodilation, while reducing Ang II and increasing Ang-(1–7) levels, to improve overall neurohormonal balance. Sacubitril/valsartan (LCZ696) is a first-in-class dual NEP inhibitor and ARB approved to reduce the risk of cardiovascular death and hospitalization in heart failure [100]. Sacubitril/valsartan produces greater blood pressure-lowering effects when compared with an ARB alone or placebo in controlled trials in essential hypertension [101], and may produce insulin-sensitizing effects in obesity hypertension [102]. The specific mechanisms underlying the beneficial effects of this combination drug remain unclear but may include sympathoinhibition, improved endothelial and cardiac function, and antiarrhythmic, anti-atherosclerotic, and antithrombotic effects [103]. In support of a contribution of autonomic mechanisms, sacubitril/valsartan lowers blood pressure, reduces sympathetic vasomotor tone, and improves spontaneous baroreflex gain under low-salt conditions in hypertensive rats (Table 2) [104]; however, this finding has not been validated in clinical populations, with effects on sympathetic activity in heart failure currently under investigation (NCT02787798, NCT03415906).
Angiotensin-(1–7)
Ang-(1–7) has emerged as an attractive potential therapy for cardiovascular diseases based on its ability to produce vasodilatory, antihypertensive, anti-inflammatory, anti-atherosclerotic, and antithrombotic effects in experimental animal models. These antihypertensive effects appear to involve inhibition of sympathetic tone and facilitation of parasympathetic tone (Table 2). There are few clinical trials with Ang-(1–7), however, and its therapeutic potential is limited by a short half-life and rapid turnover. Similar to findings in animal models, urinary Ang-(1–7) levels are reduced and inversely correlated with blood pressure in patients with untreated essential hypertension, suggesting an association between Ang-(1–7) deficiency and hypertension [105]. To date, the majority of clinical trials with Ang-(1–7) have examined the effects of acute intra-arterial administration on the forearm or renal vasodilation. These studies have shown vasodilation in patients with essential and obesity hypertension, no effect in patients with heart failure treated with ACE inhibitors, and inconsistent effects in healthy subjects [106]. Ongoing controlled trials are examining the effects of acute intravenous Ang-(1–7) infusion on blood pressure and interactions with the autonomic nervous system in healthy subjects, essential hypertension, obesity hypertension, and primary autonomic failure (NCT02245230, NCT02591173, NCT03001271, NCT03604289). Methods to more chronically increase Ang-(1–7) levels or its actions are currently in development, and include oral formulations, stable analogs, mas receptor agonists, ACE2 activators, and recombinant human ACE2 [64]. Clinical targeting of Ang-(1–7) has also been explored for cancer, improving cognition following coronary artery bypass grafting, and hematological applications [107, 108].
Conclusions
The identification of autonomic mechanisms underlying cardiovascular effects of the RAS, as well as the beneficial effects of RAS inhibition, remains an active area of research. Studies in experimental animal models show extensive and reciprocal interactions between the RAS and autonomic nervous system for cardiovascular regulation, with an important role for activation of central angiotensinergic-sympathetic pathways in the development of hypertension and other cardiovascular diseases. These findings, however, do not always readily translate to clinical studies examining pharmacological targeting of the RAS. Nevertheless, there remains considerable evidence that cardiovascular effects of therapies targeting the RAS involve, at least in part, sympathetic inhibition and/or parasympathetic facilitation. The development of pharmacotherapies to provide more complete RAS inhibition or to activate Ang-(1–7) pathways may broaden the therapeutic potential for targeting the RAS, and may provide new insights into mechanistic interactions of this hormone system with the autonomic nervous system.
Abbreviations
- Ang:
-
Angiotensin
- ACE:
-
Angiotensin-converting enzyme
- AT1 :
-
Angiotensin type 1
- ARBs:
-
Angiotensin receptor blockers
- AT2 :
-
Angiotensin type 2
- ARC:
-
Arcuate nucleus
- CVLM:
-
Caudal ventrolateral medulla
- MrgD:
-
Mas-related G-protein coupled receptor D
- MR:
-
Mineralocorticoid receptors
- NEP:
-
Neutral endopeptidase
- OVLT:
-
Organum vasculosum of the lamina terminalis
- PRR:
-
Prorenin receptor
- PVN:
-
Paraventricular nucleus
- RAS:
-
Renin–angiotensin system
- RVLM:
-
Rostral ventrolateral medulla
- NTS:
-
Nucleus tractus solitarius [solitary tract nucleus]
- SFO:
-
Subfornical organ
- SNS:
-
Sympathetic nervous system
References
Kurtz A (2011) Renin release: sites, mechanisms, and control. Annu Rev Physiol 73:377–399
Lavoie JL, Sigmund CD (2003) Minireview: overview of the renin-angiotensin system–an endocrine and paracrine system. Endocrinology 144(6):2179–2183
Te Riet L, van Esch JH, Roks AJ, van den Meiracker AH, Danser AH (2015) Hypertension: renin-angiotensin-aldosterone system alterations. Circ Res 116(6):960–975
Lavoie JL, Liu X, Bianco RA, Beltz TG, Johnson AK, Sigmund CD (2006) Evidence supporting a functional role for intracellular renin in the brain. Hypertension 47(3):461–466
Li XC, Zhu D, Zheng X, Zhang J, Zhuo JL (2018) Intratubular and intracellular renin-angiotensin system in the kidney: a unifying perspective in blood pressure control. Clin Sci (Lond) 132(13):1383–1401
Uehara Y, Miura S, Yahiro E, Saku K (2013) Non-ACE pathway-induced angiotensin II production. Curr Pharm Des 19(17):3054–3059
Zhuo JL, Li XC (2011) New insights and perspectives on intrarenal renin-angiotensin system: focus on intracrine/intracellular angiotensin II. Peptides 32(7):1551–1565
Lemarie CA, Schiffrin EL (2010) The angiotensin II type 2 receptor in cardiovascular disease. J Renin Angiotensin Aldosterone Syst 11(1):19–31
Yugandhar VG, Clark MA (2013) Angiotensin III: a physiological relevant peptide of the renin angiotensin system. Peptides 46:26–32
Dupont AG, Brouwers S (2010) Brain angiotensin peptides regulate sympathetic tone and blood pressure. J Hypertens 28(8):1599–1610
Ferrario CM, Ahmad S, Nagata S, Simington SW, Varagic J, Kon N, Dell’italia LJ (2014) An evolving story of angiotensin-II-forming pathways in rodents and humans. Clin Sci (Lond) 126(7):461–469
Campbell DJ (2008) Critical review of prorenin and (pro)renin receptor research. Hypertension 51(5):1259–1264
Santos RA (2014) Angiotensin-(1–7). Hypertension 63(6):1138–1147
Leonhardt J, Villela DC, Teichmann A, Munter LM, Mayer MC, Mardahl M, Kirsch S, Namsolleck P, Lucht K, Benz V, Alenina N, Daniell N, Horiuchi M, Iwai M, Multhaup G, Schulein R, Bader M, Santos RA, Unger T, Steckelings UM (2017) Evidence for heterodimerization and functional interaction of the angiotensin type 2 receptor and the receptor MAS. Hypertension 69(6):1128–1135
Gaidarov I, Adams J, Frazer J, Anthony T, Chen X, Gatlin J, Semple G, Unett DJ (2018) Angiotensin (1–7) does not interact directly with MAS1, but can potently antagonize signaling from the AT1 receptor. Cell Signal 50:9–24
Lautner RQ, Villela DC, Fraga-Silva RA, Silva N, Verano-Braga T, Costa-Fraga F, Jankowski J, Jankowski V, Sousa F, Alzamora A, Soares E, Barbosa C, Kjeldsen F, Oliveira A, Braga J, Savergnini S, Maia G, Peluso AB, Passos-Silva D, Ferreira A, Alves F, Martins A, Raizada M, Paula R, Motta-Santos D, Klempin F, Pimenta A, Alenina N, Sinisterra R, Bader M, Campagnole-Santos MJ, Santos RA (2013) Discovery and characterization of alamandine: a novel component of the renin-angiotensin system. Circ Res 112(8):1104–1111
Villela DC, Passos-Silva DG, Santos RA (2014) Alamandine: a new member of the angiotensin family. Curr Opin Nephrol Hypertens 23(2):130–134
Iliescu R, Lohmeier TE, Tudorancea I, Laffin L, Bakris GL (2015) Renal denervation for the treatment of resistant hypertension: review and clinical perspective. Am J Physiol Renal Physiol 309(7):F583–F594
Hong MN, Li XD, Chen DR, Ruan CC, Xu JZ, Chen J, Wu YJ, Ma Y, Zhu DL, Gao PJ (2016) Renal denervation attenuates aldosterone expression and associated cardiovascular pathophysiology in angiotensin II-induced hypertension. Oncotarget 7(42):67828–67840
Averill DB, Diz DI (2000) Angiotensin peptides and baroreflex control of sympathetic outflow: pathways and mechanisms of the medulla oblongata. Brain Res Bull 51(2):119–128
Reid IA (1992) Interactions between ANG II, sympathetic nervous system, and baroreceptor reflexes in regulation of blood pressure. Am J Physiol 262(6 Pt 1):E763–E778
Lohmeier TE (2012) Angiotensin II infusion model of hypertension: is there an important sympathetic component? Hypertension 59(3):539–541
Leenen FH (2014) Actions of circulating angiotensin II and aldosterone in the brain contributing to hypertension. Am J Hypertens 27(8):1024–1032
Allen AM, Zhuo J, Mendelsohn FA (2000) Localization and function of angiotensin AT1 receptors. Am J Hypertens 13(1 Pt 2):31S–38S
Hirooka Y, Kishi T, Ito K, Sunagawa K (2013) Potential clinical application of recently discovered brain mechanisms involved in hypertension. Hypertension 62(6):995–1002
Huber G, Schuster F, Raasch W (2017) Brain renin-angiotensin system in the pathophysiology of cardiovascular diseases. Pharmacol Res 125(Pt A):72–90
de Queiroz TM, Monteiro MM, Braga VA (2013) Angiotensin-II-derived reactive oxygen species on baroreflex sensitivity during hypertension: new perspectives. Front Physiol 4:105
Schaich CL, Shaltout HA, Grabenauer M, Thomas BF, Gallagher PE, Howlett AC, Diz DI (2015) Alterations in the medullary endocannabinoid system contribute to age-related impairment of baroreflex sensitivity. J Cardiovasc Pharmacol 65(5):473–479
Pellegrino PR, Schiller AM, Haack KK, Zucker IH (2016) Central angiotensin-II increases blood pressure and sympathetic outflow via rho kinase activation in conscious rabbits. Hypertension 68(5):1271–1280
Arnold AC, Isa K, Shaltout HA, Nautiyal M, Ferrario CM, Chappell MC, Diz DI (2010) Angiotensin-(1–12) requires angiotensin converting enzyme and AT1 receptors for cardiovascular actions within the solitary tract nucleus. Am J Physiol Heart Circ Physiol 299(3):H763–H771
Houghton BL, Huang C, Johns EJ (2010) Influence of dietary sodium on the blood pressure and renal sympathetic nerve activity responses to intracerebroventricular angiotensin II and angiotensin III in anaesthetized rats. Exp Physiol 95(2):282–295
Marc Y, Llorens-Cortes C (2011) The role of the brain renin-angiotensin system in hypertension: implications for new treatment. Prog Neurobiol 95(2):89–103
Huang BS, Ahmad M, White RA, Marc Y, Llorens-Cortes C, Leenen FH (2013) Inhibition of brain angiotensin III attenuates sympathetic hyperactivity and cardiac dysfunction in rats post-myocardial infarction. Cardiovasc Res 97(3):424–431
Kokje RJ, Wilson WL, Brown TE, Karamyan VT, Wright JW, Speth RC (2007) Central pressor actions of aminopeptidase-resistant angiotensin II analogs: challenging the angiotensin III hypothesis. Hypertension 49(6):1328–1335
Matsukawa T, Gotoh E, Minamisawa K, Kihara M, Ueda S, Shionoiri H, Ishii M (1991) Effects of intravenous infusions of angiotensin II on muscle sympathetic nerve activity in humans. Am J Physiol 261(3 Pt 2):R690–R696
Sayk F, Wobbe I, Twesten C, Meusel M, Wellhoner P, Derad I, Dodt C (2015) Prolonged blood pressure elevation following continuous infusion of angiotensin II-a baroreflex study in healthy humans. Am J Physiol Regul Integr Comp Physiol 309(11):R1406–R1414
Goldsmith SR, Hasking GJ, Miller E (1993) Angiotensin II and sympathetic activity in patients with congestive heart failure. J Am Coll Cardiol 21(5):1107–1113
Goldsmith SR, Hasking GJ (1995) Angiotensin II inhibits the forearm vascular response to increased arterial pressure in humans. J Am Coll Cardiol 25(1):246–250
Townend JN, Al-Ani M, West JN, Littler WA, Coote JH (1995) Modulation of cardiac autonomic control in humans by angiotensin II. Hypertension 25(6):1270–1275
Ruhs S, Nolze A, Hubschmann R, Grossmann C (2017) 30 years of the mineralocorticoid receptor: nongenomic effects via the mineralocorticoid receptor. J Endocrinol 234(1):T107–T124
Downey RM, Mizuno M, Mitchell JH, Vongpatanasin W, Smith SA (2017) Mineralocorticoid receptor antagonists attenuate exaggerated exercise pressor reflex responses in hypertensive rats. Am J Physiol Heart Circ Physiol 313(4):H788–H794
Yee KM, Struthers AD (1998) Aldosterone blunts the baroreflex response in man. Clin Sci (Lond) 95(6):687–692
Schmidt BM, Montealegre A, Janson CP, Martin N, Stein-Kemmesies C, Scherhag A, Feuring M, Christ M, Wehling M (1999) Short term cardiovascular effects of aldosterone in healthy male volunteers. J Clin Endocrinol Metab 84(10):3528–3533
Heindl S, Holzschneider J, Hinz A, Sayk F, Fehm HL, Dodt C (2006) Acute effects of aldosterone on the autonomic nervous system and the baroreflex function in healthy humans. J Neuroendocrinol 18(2):115–121
Monahan KD, Leuenberger UA, Ray CA (2007) Aldosterone impairs baroreflex sensitivity in healthy adults. Am J Physiol Heart Circ Physiol 292(1):H190–H197
Cuadra AE, Shan Z, Sumners C, Raizada MK (2010) A current view of brain renin-angiotensin system: is the (pro)renin receptor the missing link? Pharmacol Ther 125(1):27–38
Li W, Peng H, Cao T, Sato R, McDaniels SJ, Kobori H, Navar LG, Feng Y (2012) Brain-targeted (pro)renin receptor knockdown attenuates angiotensin II-dependent hypertension. Hypertension 59(6):1188–1194
Shan Z, Shi P, Cuadra AE, Dong Y, Lamont GJ, Li Q, Seth DM, Navar LG, Katovich MJ, Sumners C, Raizada MK (2010) Involvement of the brain (pro)renin receptor in cardiovascular homeostasis. Circ Res 107(7):934–938
Huber MJ, Basu R, Cecchettini C, Cuadra AE, Chen QH, Shan Z (2015) Activation of the (pro)renin receptor in the paraventricular nucleus increases sympathetic outflow in anesthetized rats. Am J Physiol Heart Circ Physiol 309(5):H880–H887
Li W, Peng H, Mehaffey EP, Kimball CD, Grobe JL, van Gool JM, Sullivan MN, Earley S, Danser AH, Ichihara A, Feng Y (2014) Neuron-specific (pro)renin receptor knockout prevents the development of salt-sensitive hypertension. Hypertension 63(2):316–323
Li W, Sullivan MN, Zhang S, Worker CJ, Xiong Z, Speth RC, Feng Y (2015) Intracerebroventricular infusion of the (Pro)renin receptor antagonist PRO20 attenuates deoxycorticosterone acetate-salt-induced hypertension. Hypertension 65(2):352–361
Shi P, Grobe JL, Desland FA, Zhou G, Shen XZ, Shan Z, Liu M, Raizada MK, Sumners C (2014) Direct pro-inflammatory effects of prorenin on microglia. PLoS One 9(10):e92937
Pitra S, Feng Y, Stern JE (2016) Mechanisms underlying prorenin actions on hypothalamic neurons implicated in cardiometabolic control. Mol Metab 5(10):858–868
Gironacci MM, Cerniello FM, Longo Carbajosa NA, Goldstein J, Cerrato BD (2014) Protective axis of the renin-angiotensin system in the brain. Clin Sci (Lond) 127(5):295–306
de Souza-Neto FP, Carvalho Santuchi M, de Morais ESM, Campagnole-Santos MJ, da Silva RF (2018) Angiotensin-(1–7) and alamandine on experimental models of hypertension and atherosclerosis. Curr Hypertens Rep 20(2):17
Shangguan W, Shi W, Li G, Wang Y, Li J, Wang X (2017) Angiotensin-(1–7) attenuates atrial tachycardia-induced sympathetic nerve remodeling. J Renin Angiotensin Aldosterone Syst 18(3):1470320317729281
Martins Lima A, Xavier CH, Ferreira AJ, Raizada MK, Wallukat G, Velloso EP, dos Santos RA, Fontes MA (2013) Activation of angiotensin-converting enzyme 2/angiotensin-(1–7)/Mas axis attenuates the cardiac reactivity to acute emotional stress. Am J Physiol Heart Circ Physiol 305(7):H1057–H1067
de Moura MM, dos Santos RA, Campagnole-Santos MJ, Todiras M, Bader M, Alenina N, Haibara AS (2010) Altered cardiovascular reflexes responses in conscious angiotensin-(1–7) receptor Mas-knockout mice. Peptides 31(10):1934–1939
Bilodeau MS, Leiter JC (2018) Angiotensin 1–7 in the rostro-ventrolateral medulla increases blood pressure and splanchnic sympathetic nerve activity in anesthetized rats. Respir Physiol Neurobiol 247:103–111
Ren X, Zhang F, Zhao M, Zhao Z, Sun S, Fraidenburg DR, Tang H, Han Y (2017) Angiotensin-(1–7) in paraventricular nucleus contributes to the enhanced cardiac sympathetic afferent reflex and sympathetic activity in chronic heart failure rats. Cell Physiol Biochem 42(6):2523–2539
Xia H, Lazartigues E (2010) Angiotensin-converting enzyme 2: central regulator for cardiovascular function. Curr Hypertens Rep 12(3):170–175
Shen YH, Chen XR, Yang CX, Liu BX, Li P (2018) Alamandine injected into the paraventricular nucleus increases blood pressure and sympathetic activation in spontaneously hypertensive rats. Peptides 103:98–102
Leenen FH, Ruzicka M, Floras JS (2012) Central sympathetic inhibition by mineralocorticoid receptor but not angiotensin II type 1 receptor blockade: are prescribed doses too low? Hypertension 60(2):278–280
Ferrario CM, Mullick AE (2017) Renin angiotensin aldosterone inhibition in the treatment of cardiovascular disease. Pharmacol Res 125(Pt A):57–71
Grassi G (2016) Sympathomodulatory effects of antihypertensive drug treatment. Am J Hypertens 29(6):665–675
Abuissa H, Jones PG, Marso SP, O’Keefe JH Jr (2005) Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for prevention of type 2 diabetes: a meta-analysis of randomized clinical trials. J Am Coll Cardiol 46(5):821–826
Yang Y, Wei RB, Wang ZC, Wang N, Gao YW, Li MX, Qiu Q (2015) A meta-analysis of the effects of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers on insulin sensitivity in hypertensive patients without diabetes. Diabetes Res Clin Pract 107(3):415–423
Robles NR, Cerezo I, Hernandez-Gallego R (2014) Renin-angiotensin system blocking drugs. J Cardiovasc Pharmacol Ther 19(1):14–33
Benter IF, Yousif MH, Al-Saleh FM, Raghupathy R, Chappell MC, Diz DI (2011) Angiotensin-(1–7) blockade attenuates captopril- or hydralazine-induced cardiovascular protection in spontaneously hypertensive rats treated with NG-nitro-l-arginine methyl ester. J Cardiovasc Pharmacol 57(5):559–567
Kucharewicz I, Pawlak R, Matys T, Pawlak D, Buczko W (2002) Antithrombotic effect of captopril and losartan is mediated by angiotensin-(1–7). Hypertension 40(5):774–779
Yousif MH, Dhaunsi GS, Makki BM, Qabazard BA, Akhtar S, Benter IF (2012) Characterization of angiotensin-(1–7) effects on the cardiovascular system in an experimental model of type-1 diabetes. Pharmacol Res 66(3):269–275
Lang CC, Stein CM, He HB, Wood AJ (1996) Angiotensin converting enzyme inhibition and sympathetic activity in healthy subjects. Clin Pharmacol Ther 59(6):668–674
Azevedo ER, Mak S, Floras JS, Parker JD (2017) Acute effects of angiotensin-converting enzyme inhibition versus angiotensin II receptor blockade on cardiac sympathetic activity in patients with heart failure. Am J Physiol Regul Integr Comp Physiol 313(4):R410–R417
Krum H, Lambert E, Windebank E, Campbell DJ, Esler M (2006) Effect of angiotensin II receptor blockade on autonomic nervous system function in patients with essential hypertension. Am J Physiol Heart Circ Physiol 290(4):H1706–H1712
de Champlain J, Karas M, Assouline L, Nadeau R, LeBlanc AR, Dube B, Larochelle P (2007) Effects of valsartan or amlodipine alone or in combination on plasma catecholamine levels at rest and during standing in hypertensive patients. J Clin Hypertens (Greenwich) 9(3):168–178
Ajayi AA, Reid JL (1988) Renin-angiotensin modulation of sympathetic reflex function in essential hypertension and in the elderly. Int J Clin Pharmacol Res 8(5):327–333
Stupin A, Drenjancevic I, Rasic L, Cosic A, Stupin M (2017) A cross-talk between the renin-angiotensin and adrenergic systems in cardiovascular health and disease. SEEMEDJ 1(1):90–107
Arnold AC, Okamoto LE, Gamboa A, Shibao C, Raj SR, Robertson D, Biaggioni I (2013) Angiotensin II, independent of plasma renin activity, contributes to the hypertension of autonomic failure. Hypertension 61(3):701–706
Cabandugama PK, Gardner MJ, Sowers JR (2017) The renin angiotensin aldosterone system in obesity and hypertension: roles in the cardiorenal metabolic syndrome. Med Clin N Am 101(1):129–137
Engeli S, Bohnke J, Gorzelniak K, Janke J, Schling P, Bader M, Luft FC, Sharma AM (2005) Weight loss and the renin-angiotensin-aldosterone system. Hypertension 45(3):356–362
Masuo K, Mikami H, Ogihara T, Tuck ML (2001) Weight reduction and pharmacologic treatment in obese hypertensives. Am J Hypertens 14(6 Pt 1):530–538
Floras JS, Ponikowski P (2015) The sympathetic/parasympathetic imbalance in heart failure with reduced ejection fraction. Eur Heart J 36(30):1974–1982b
Neumann J, Ligtenberg G, Klein IH, Boer P, Oey PL, Koomans HA, Blankestijn PJ (2007) Sympathetic hyperactivity in hypertensive chronic kidney disease patients is reduced during standard treatment. Hypertension 49(3):506–510
Pantzaris ND, Karanikolas E, Tsiotsios K, Velissaris D (2017) Renin inhibition with aliskiren: a decade of clinical experience. J Clin Med 6(6):61
Huang BS, White RA, Bi L, Leenen FH (2012) Central infusion of aliskiren prevents sympathetic hyperactivity and hypertension in Dahl salt-sensitive rats on high salt intake. Am J Physiol Regul Integr Comp Physiol 302(7):R825–R832
Siddiqi L, Oey PL, Blankestijn PJ (2011) Aliskiren reduces sympathetic nerve activity and blood pressure in chronic kidney disease patients. Nephrol Dial Transplant 26(9):2930–2934
Okada Y, Jarvis SS, Best SA, Bivens TB, Adams-Huet B, Levine BD, Fu Q (2013) Chronic renin inhibition lowers blood pressure and reduces upright muscle sympathetic nerve activity in hypertensive seniors. J Physiol 591(23):5913–5922
Jarvis SS, Okada Y, Levine BD, Fu Q (2015) Central integration and neural control of blood pressure during the cold pressor test: a comparison between hydrochlorothiazide and aliskiren. Physiol Rep 3(9):e12502
Fogari R, Zoppi A, Mugellini A, Maffioli P, Lazzari P, Monti C, Derosa G (2011) Effect of aliskiren addition to amlodipine on ankle edema in hypertensive patients: a three-way crossover study. Expert Opin Pharmacother 12(9):1351–1358
Maser RE, Lenhard MJ, Kolm P, Edwards DG (2013) Direct renin inhibition improves parasympathetic function in diabetes. Diabetes Obes Metab 15(1):28–34
Mengal V, Silva PH, Tiradentes RV, Santuzzi CH, de Almeida SA, Sena GC, Bissoli NS, Abreu GR, Gouvea SA (2016) Aliskiren and l-arginine treatments restore depressed baroreflex sensitivity and decrease oxidative stress in renovascular hypertension rats. Hypertens Res 39(11):769–776
DuPont JJ, Hill MA, Bender SB, Jaisser F, Jaffe IZ (2014) Aldosterone and vascular mineralocorticoid receptors: regulators of ion channels beyond the kidney. Hypertension 63(4):632–637
Brown NJ (2003) Eplerenone: cardiovascular protection. Circulation 107(19):2512–2518
Dudenbostel T, Calhoun DA (2017) Use of aldosterone antagonists for treatment of uncontrolled resistant hypertension. Am J Hypertens 30(2):103–109
Arnold AC, Okamoto LE, Gamboa A, Black BK, Raj SR, Elijovich F, Robertson D, Shibao CA, Biaggioni I (2016) Mineralocorticoid receptor activation contributes to the supine hypertension of autonomic failure. Hypertension 67(2):424–429
Lincevicius GS, Shimoura CG, Nishi EE, Perry JC, Casarini DE, Gomes GN, Bergamaschi CT, Campos RR (2015) Aldosterone contributes to sympathoexcitation in renovascular hypertension. Am J Hypertens 28(9):1083–1090
Marques Neto SR, Silva AD, Santos MD, Ferraz EF, Nascimento JH (2013) The blockade of angiotensin AT1 and aldosterone receptors protects rats from synthetic androgen-induced cardiac autonomic dysfunction. Acta Physiol (Oxf) 208(2):166–171
Davies JI, Witham MD, Struthers AD (2005) Autonomic effects of spironolactone and MR blockers in heart failure. Heart Fail Rev 10(1):63–69
Gomez-Sanchez EP (2016) Third-generation mineralocorticoid receptor antagonists: why do we need a fourth? J Cardiovasc Pharmacol 67(1):26–38
Kaplinsky E (2016) Sacubitril/valsartan in heart failure: latest evidence and place in therapy. Ther Adv Chronic Dis 7(6):278–290
Ye L, Wang J, Chen Q, Yang X (2017) LCZ696, a promising novel agent in treating hypertension (a meta-analysis of randomized controlled trials). Oncotarget 8(64):107991–108005
Engeli S, Stinkens R, Heise T, May M, Goossens GH, Blaak EE, Havekes B, Jax T, Albrecht D, Pal P, Tegtbur U, Haufe S, Langenickel TH, Jordan J (2018) Effect of sacubitril/valsartan on exercise-induced lipid metabolism in patients with obesity and hypertension. Hypertension 71(1):70–77
Menendez JT (2016) The mechanism of action of LCZ696. Card Fail Rev 2(1):40–46
Kusaka H, Sueta D, Koibuchi N, Hasegawa Y, Nakagawa T, Lin B, Ogawa H, Kim-Mitsuyama S (2015) LCZ696, angiotensin II receptor-neprilysin inhibitor, ameliorates high-salt-induced hypertension and cardiovascular injury more than valsartan alone. Am J Hypertens 28(12):1409–1417
Ferrario CM, Martell N, Yunis C, Flack JM, Chappell MC, Brosnihan KB, Dean RH, Fernandez A, Novikov SV, Pinillas C, Luque M (1998) Characterization of angiotensin-(1–7) in the urine of normal and essential hypertensive subjects. Am J Hypertens 11(2):137–146
Touyz RM, Montezano AC (2018) Angiotensin-(1–7) and vascular function: the clinical context. Hypertension 71(1):68–69
Machado-Silva A, Passos-Silva D, Santos RA, Sinisterra RD (2016) Therapeutic uses for angiotensin-(1–7). Expert Opin Ther Pat 26(6):669–678
Ho JK, Nation DA (2018) Cognitive benefits of angiotensin IV and angiotensin-(1–7): a systematic review of experimental studies. Neurosci Biobehav Rev 92:209–225
Acknowledgements
ACA is supported by NIH grants R00HL122507 and UL1TR002014. AJM is supported by American Heart Association grant 18POST33960087.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Miller, A.J., Arnold, A.C. The renin–angiotensin system in cardiovascular autonomic control: recent developments and clinical implications. Clin Auton Res 29, 231–243 (2019). https://doi.org/10.1007/s10286-018-0572-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-018-0572-5