Abstract
The aim of this study was to determine the prevalence of different diagnostic image viewing platforms used by radiologists while on-call, and to assess the opinions and preferences of radiology program directors and chief residents regarding their use. An online survey was sent electronically to radiology residency program directors and chief residents via the Association of University Radiologists. Forty-two radiology program directors and 25 chief residents completed the survey, yielding response rates of 24.9 and 8.5 %, respectively. From the survey results, 10 different Picture Archiving Communications Systems (PACS) were identified; GE (25 %), Philips (17 %), and Agfa Impax (15 %) were the most prevalent. Interestingly, only 5 % of all respondents use a secondary “Digital Imaging and Communications in Medicine” viewer for on-call studies. Perceptions of PACS functionality were generally neutral to weakly positive. Most respondents strongly agreed that it is important to have a single integrated PACS for viewing on-call studies and agreed that the PACS should be integrated into the Electronic Medical Records (EMR). The overwhelming majority of respondents use their institution’s PACS while on-call. The results show there is still a wide variety of PACS platforms used by different institutions; however, GE, Phillips, and Agfa were some of the most prevalent. Most radiologists surveyed have neutral to slightly positive perceptions about the functionality and ease of use of their PACS. Finally, while radiologists agree that PACS should be integrated with EMR, only 53 % of respondents currently have this arrangement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Throughout the United States, radiologists use a variety of Picture Archiving and Communication Systems (PACS) and Digital Imaging and Communications in Medicine (DICOM) viewers to interpret diagnostic images. In this study, our aim is to identify the prevalence of different diagnostic image viewing systems used by radiologists while on-call, and to investigate the opinions underpinning the use of these systems.
The PACS platform has revolutionized the way diagnostic digital images are obtained, stored, and interpreted. A PACS platform consists of three main components: the imaging modality (x-ray, CT, MRI, etc.), the radiologist’s workstation, and the archiving storage hardware. These three key elements are interconnected via a secure network that transmits the universal DICOM language (which encodes the diagnostic image) from one component to another. In this way, an image can be created from a modality such as a CT, interpreted and a report dictated by a radiologist at his workstation, and finally the image sent alongside the final dictated report to an archiving system for future retrieval. The concept of PACS was first introduced in the early 1980s, and the first implementation of PACS took place in 1982 at the University of Kansas [1]. However, it was not until 1993 at the Baltimore VA Medical Center that the first successful, full-scale transition to an entirely “filmless” imaging department took place in the United States [2]. Today, PACS is nearly ubiquitous throughout hospitals in the United States. When implemented properly, the system is highly effective and streamlines patient care.
Several studies found implementing a uniform PACS platform from a film-based system improves efficiency, enhances collaboration, and decreases costs [3–5]. Early financial assessments suggested that PACS might actually increase costs due to the significant investments required for both hardware and software. However, in 2006 a large-scale assessment of a hospital-wide PACS implementation revealed a net savings of $485,157 [3]. Perhaps most importantly, in all of these studies radiologist productivity increased, patient waiting time decreased, and critical results were relayed more efficiently [3–5]. Yet, despite these benefits, every PACS platform has hurdles to overcome. A recent study of Case Western’s implementation of a new PACS platform identified unexpected network issues due to high latency of images, which required widespread upgrades in bandwidth across several hospitals within the system [5]. While each hospital must carefully select a PACS based on criteria that suit its own needs, a few qualities have universally stood out. This includes security, prevention of lost data, and fast turnaround times [6]. With these criteria and others in mind, there are literally hundreds of available PACS vendors to choose from, but there is currently no universally accepted “ideal” PACS platform [7]. PACS administrators must work alongside radiologists to select a PACS platform that makes the process of image interpretation more efficient, faster, and simpler.
This is especially important now more than ever, as radiologists experience increasing demands from the passage of the Affordable Care Act (ACA) and from the steady rise in diagnostic imaging [8]. On-call and after-hours radiology reports have increased throughout the United States, and radiology programs have taken various measures to meet this increasing demand. In 2011, Deloney et al. describe the results of a national survey of program directors, which revealed that on-call studies have increased from prior years in programs across the board. Currently, 45 % of programs have staff radiologists in-house with residents covering on-call studies [9]. In 2012, more evidence surfaced in a study surveying chief residents. Not only did after-hours imaging studies increase but demand for final reports by staff radiologists increased as well. To respond to this demand, 20 % of all programs kept a staff radiologist in-house overnight, also an increase from previous years [10]. Hence, we see PACS performance put to the test in a variety of ways, as radiology residents are required to read increasing volumes of studies while on-call.
Recently, several studies have emerged reporting new software or hardware designed to improve training, efficiency, or user experience with PACS especially when used while on-call. One academic center implemented a unique web-based reporting system integrated to their PACS to improve the workflow for their residents on-call [11]. On-call PACS simulators were developed to help prepare new residents for the rigors of reading emergent imaging independently and to enhance their proficiency when using PACS in these situations [12]. Another study describes the launch of “SimpleDICOM suite,” designed to enhance the functionality of commercially available PACS [13]. One group analyzed six different user interface devices ranging from a five-button mouse to a gaming joystick, to see if any device provided a superior user experience or improved efficiency when using PACS [14]. Growing demands during on-call duties make having an effective, easy-to-use PACS especially important.
To date, few studies have looked at how the great variety of different PACS platforms and DICOM viewers affects on-call duties. This study seeks to answer that question.
Materials and Methods
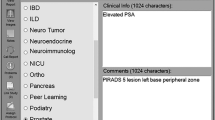
We surveyed radiology chief residents and program directors to identify the arrangements of PACS and EMR used on-call at teaching hospitals, and to assess their views regarding the use of these systems. The survey focused on four main areas: PACS and secondary DICOM viewers, worklist and turnaround time, EMR and PACS, and opinions and preferences regarding PACS. Secondary DICOM viewers can be defined as any DICOM viewer that is used by the radiologist that is not the primary DICOM viewer that is supported by their institution’s PACS. For instance, if a radiologist’s institution uses GE Centricity but the radiologist chooses to use Osirix when viewing images on-call, this would be considered a secondary DICOM viewer. The respondents were asked a series of multiple choice and free text questions regarding the current arrangement of the PACS and EMR used at their institution. Respondents were also asked to rate statements on a one- to five-point Likert scale (1 = “strongly disagree” to 5 = “strongly agree”; see Appendix for complete survey). The survey was sent electronically via email to radiology chief residents and program directors in July of 2013, and was hosted online by SurveyMonkey.com (SurveyMonkey, Portland, Oregon). These emails were distributed to the Association of Program Directors in Radiology and the American Alliance of Academic Chief Residents in Radiology. The results were compiled on SurveyMonkey software and subsequently downloaded to be statistically analyzed using Microsoft Excel (Microsoft Corporation, Redmond, Washington). IP addresses and demographic information was cross-referenced to ensure that survey responses were not duplicated or counted more than once in the results.
Results
Radiology Chief Residents and Program Directors Survey:
Respondents from 59 different teaching institutions with radiology programs participated in this study, yielding a 32 % institutional response rate. The survey response rate was 24.9 % for program directors (PD) and 8.5 % for chief residents (CR). Respondents were relatively equally distributed from the Midwest (30 %), Northeast (28 %), Southeast (21 %), and Southwest (15 %), with fewer respondents from the Northwest (6 %). The majority of respondents practiced in an Academic Hospital or VA (76 %). Other clinical settings included Community Hospitals (8 %), Imaging Centers (6 %), and Group or Clinical Practices (6 %). The size of the intuitions represented ranged from less than 20 residents and 25 Full Time Equivalent (FTE) Attendings to those with more than 50 residents and over 100 FTE Attendings.
PACS and Secondary DICOM Viewers
Individuals from 59 different institutions reported the PACS platform they use while on-call. Out of those who responded to the survey, the most prevalent PACS platform is GE (25 %), followed by Phillips (17 %) and Agfa Impax (15 %). Other PACS include Fuji (13 %), McKesson (13 %), Siemens (5 %), Carestream (3 %), Intelerad (3 %), an Internet-Based Browser (3 %), and Emageon (2 %) (Fig. 1).
A total of 59 individuals from different institutions answered questions regarding the use of secondary DICOM viewers while on-call. Ninety-five percent of all respondents do not use a secondary DICOM viewer, and only 5 % report using a DICOM viewer for on-call studies (Fig. 2). One hundred percent of those who did use secondary DICOM viewers (three respondents) were chief residents. All of these CR indicated they used the DICOM viewer to access outside consults because the in-house PACS was not available for these studies.
Worklist and Turnaround Time
A total of 52 respondents answered questions regarding worklist organization. Fifty-four percent of those surveyed have worklists separated by specialty, and the remaining 46 % have worklists that encompass multiple specialties (Fig. 3). “Multi-specialty” worklists included lists organized by individual filters, lists specified for the Emergency Department, and lists separated by modality.
A total of 55 respondents answered questions about radiologist report turnaround time (RRTT). The majority of radiologists responding completed reports in less than 2 h (roughly 75 %). Fifteen percent reported an RRTT of between 2 and 6 h, and the remainder took more than 6 h (Fig. 4).
EMR
CR and PD from 59 different institutions responded to questions regarding their Electronic Medical Records (EMR). Forty-seven percent of institutions represented have PACS that is integrated with its EMR and is accessible remotely for on-call studies. Five percent of institutions in the survey have PACS that is integrated with EMR, but is not accessible remotely. Forty-one percent of institutions represented in the survey have a PACS platform that is separate from the EMR (Fig. 5).
Respondents from 49 different institutions specified the EMR used by their institution. EPIC was by far the most prevalent, representing 49 % of all institutions surveyed. Other EMR systems included Cerner, Webcis, Affinity, Quest, and Ibex, among others (Fig. 6).
Opinions and Preferences
Overall, program directors and chief residents had generally neutral to positive views regarding their current PACS platforms, but chief residents were more positive. There were no statistically significant differences between the views of CR and PD.
Out of all the statements, PD and CR most strongly agreed with “It is important to have a single, integrated PACS platform at an institution for viewing on-call studies,” with averages of 4.54 and 4.39, respectively. PD and CR were almost identically in agreement to the statement that it is important for PACS to be integrated into EMR to facilitate remote access of studies, yielding average scores of 4.0 and 4.04, respectively. CR tended to slightly agree that their PACS viewer affects their on-call turnaround time (3.91); however, PD were more neutral towards this statement (3.58). PD views were also somewhat neutral to the more targeted statement “The PACS or DICOM viewer you use while on-call helps to decrease your radiologist report turnaround time,” with an average of 3.61. CR tended to agree with this statement (average score 3.94), but the difference in opinion versus PD was not statistically significant (p value 0.30). Finally, the greatest difference in opinion between PD and CR was with the statement “The PACS or DICOM viewer that you use while on-call is easy to use and navigate.” PD were more neutral towards this statement (3.63), whereas CR tended to agree with this statement (4.04), yielding an average difference of 0.41; however, this difference was not statistically significant (p value 0.13) (Fig. 7, Table 1).
Discussion
The results of this study give insights into diagnostic image viewers used on-call, but also revealed more broadly applicable findings about the use of PACS across different hospital systems. The study uncovered three main findings. First, while there are many different PACS vendors implemented at teaching hospitals, there is insufficient evidence to suggest that specific PACS platforms differentially impact on-call performance. Next, radiologists in teaching hospitals universally prefer to use their home institution’s PACS for on-call studies over other secondary DICOM viewers. Third, radiologists participating in this study prefer a single unified PACS in a healthcare institution and agree that EMR integration with remote access is important. However, our study revealed that only 41 % of all hospital systems represented by survey respondents currently use a PACS platform that is not integrated with EMR.
We identified 10 different PACS vendors used by the 59 different institutions represented in this study (Fig. 1). These findings suggest there is clearly still great variability with regards to PACS vendor selection at teaching hospitals, and currently there is no clear dominant player in the PACS market. However, out of our study results, GE was the most prevalent, followed by Phillips, Agfa, Fuji, and McKesson (percentage of total responses, 25, 17, 15, 13, and 13 %, respectively; Fig. 1). To our knowledge, there are no similar studies looking at PACS vendors specifically at teaching hospitals; however, in 2004 one study reported the benefits of the 15 leading PACS vendors across multiple different hospitals. The author identified GE (21 %), Siemens (21 %), Agfa (19 %), and Kodak (16 %) as owning the biggest market share at the time [7]. Almost 10 years later, GE and Agfa are still some of the most prevalent PACS as suggested by the data in this study. Without more specific questions polling the turnover of PACS platforms at an institution over time, or the reasoning behind selecting certain PACS platforms, we cannot conclude with certainty why these systems are most prevalent. Previous studies have found that some of the most important qualities of a PACS platform to a radiologist include security, backup, downtime prevention, and voice recognition software for transcription and reporting [6]. Further studies are needed to more specifically probe into why each PACS was selected initially and what drove the decision process when the PACS was chosen. There are many individuals who are involved in the selection of PACS, including radiology department chairs, hospital administrators, and PACS administrators. However, additional survey data is needed to determine exactly who makes this final decision at each institution. Keeping this in mind, studies have shown PACS administrators have a high level of influence when it comes to PACS selection and implementation [15]. Therefore, open communication between staff radiologists and PACS administrators is critical.
Alternatively, vendors with a larger market share may have established their position in the PACS market through early entry. This can allow the vendor to create long-term relationships with different hospital networks. For example, GE was one of the first companies to offer PACS to hospitals and implemented the first PACS platform for the Department of Defense in the 1990s [2]. Today, they are one of the most prevalent PACS platforms in hospitals across the country.
In order to get a complete picture of the software-based practice environment that impacts radiologists on-call, our study ascertained the different EMR platforms that are used in concert with their institution’s PACS. From the responses to this survey, our study identified 14 different EMR systems representing a total of 49 teaching hospitals. EPIC was by far the most prevalent EMR in use (49 % of total, Fig. 6). Similar to the different PACS vendors represented in this study, there is still a great variety of different systems in use. However, the EPIC platform more clearly represents the most common EMR implemented by the hospitals represented in this study. Furthermore, nearly all participants of the study indicated the use of EMR at their institution. For comparison, in 2009 one study surveyed 63 % of all hospitals in the United States found that only 9 % had some form of EMR in place [16]. The results from our study suggest EMR adoption is on the rise and is nearly ubiquitous in the teaching hospitals represented in this study. Since this study focuses on teaching hospitals, many of which are part of a multi-hospital network, this may provide some explanation as to why the rates of EMR use are so high. A previous study by Li et al. showed that hospitals that were part of a multi-hospital network were more likely than independent hospitals to have EMR [17]. Furthermore, the passage of the Health Information Technology for Economic and Clinical Health Act (HITECH Act) in 2009 has substantially increased adoption of EMR with its requirements to demonstrating meaningful use [18].
The second primary finding of this study revealed that the overwhelming majority of respondents prefer to use their institution’s PACS for on-call studies versus using an alternative DICOM viewer. Ninety-five percent of all survey participants and 100 % of PD indicated they used their institution’s PACS for on-call studies. The three chief residents who did use a secondary DICOM viewer stated they did so out of necessity. Specifically, their institutions’ PACS were not available for outside studies while on-call. These findings suggest the need for a uniform PACS platform across different hospitals within a multi-hospital network. This is especially relevant today as more individual hospitals are joining larger networks of hospitals, thus requiring on-call radiology coverage to take place at different geographical locations [19]. By making all images in a hospital network available on a single “home institution’s” PACS, the process of interpreting diagnostic images is simplified for the radiologist and all staff involved, enhancing efficiency. This was demonstrated early on by the Baltimore VA Health Center, in which they integrated a single PACS across five hospitals in geographically different locations and realized a 70 % decrease in scheduled call coverage. Moreover, there was no increase in turnaround time, and triage for transfer patients between hospitals within their hospital network was simplified because the images could be reviewed instantly [15].
The results show a very low rate of secondary DICOM viewer use for on-call duties, which makes sense given the call structure of teaching hospitals. Most programs tend to have in-house call, so it seems logical that the radiologist on-call will use the supported in-house PACS. Additionally, as mentioned previously, increasing demands brought on by more after-hours imaging has led to more attending radiologists staying in-house for on-call duties [9, 10]. Therefore, both program directors and chief residents have become more likely to take in-house call. Secondary DICOM viewers are evolving, and now highly functional DICOM viewing software is available for mobile devices such as the iPhone and iPad, creating a very portable option that could be of use in multi-hospital networks [20]. Still, even with technological advances improving secondary DICOM viewers’ functionality and flexibility, radiologists in teaching hospitals rely on the institution’s PACS for on-call studies. This can be due to increased familiarity with the home system and greater functionality over external secondary viewers. These findings support the concept of a single, unified PACS across a hospital system.
Program directors and chief residents strongly agree that it is important to have a single, well-integrated PACS platform at an institution for viewing on-call studies (average rating, 4.54 and 4.39, respectively; Fig. 7). The key components of diagnostic imaging—obtaining images, reporting findings, and ultimately relaying the findings or storing them for retrieval—are simplified at institutions that cover multiple hospitals if unified by one PACS framework. Ease of access is critical. In the last few years, there has been a push towards making both old and new diagnostic images for a patient universally accessible, so they can be retrieved at any hospital that receives a patient’s consent. As described by Ge et al., Patient Controlled Access-key REgistery (PCARE) is an example of one such prototype just launched this past year that seeks to accomplish this goal [21].
Both program directors and chief residents also agree that the PACS should be integrated into the EMR to facilitate remote access of on-call imaging studies (average rating, 4.0 and 4.04, respectively; Fig. 7). Integration of PACS with EMR has the potential to improve patient care by making it easier to get real-time updates and clinical correlates to diagnostic studies. Furthermore, one study found that the integration of EMR and PACS improves accuracy and efficiency of patient management in a healthcare system, further supporting this idea [22]. Yet, despite these views and the apparent benefits, only 49 % of all survey respondents indicated that their institution had PACS that was integrated into the EMR and was accessible remotely for on-call studies (Fig. 5). The relatively low rate of PACS integration with EMR at the hospitals in this study highlights a potential area for improvement, given the purported benefits. Healthcare reform through the ACA and the HITECH Act are pushing meaningful use of health IT through reimbursement incentives and penalties [18]. In our current political landscape, there is intense focus on decreasing health care costs through integration. EMR and PACS can provide an excellent opportunity to create such new efficiencies. Additionally, future research can be directed at comparing outcomes of hospitals with PACS integrated into their EMR systems versus those without such integration.
As shown in Table 1 and Fig. 7, both chief residents and program directors tended to have neutral to positive views regarding their institution’s PACS. Interestingly, PD were relatively split between “neutral” and “strongly agree” with regards to the statement, “The PACS or DICOM viewer you use while on-call affects your radiologist report turnaround time” (13 and 12 out of 36 PD responses, respectively; Table 1). This pattern was also reflected in the responses to the statement, “The PACS or DICOM viewer you use while on-call helps to decrease your radiologist report turnaround time” (11 responses for “neutral” and 12 responses for “strongly agree”; Table 1). The results suggest that some program directors feel the PACS platform they use has a strong impact on their productivity and helps to decrease their turnaround time, while others believe the PACS platform has no effect on their productivity in either a positive or negative way. On the other hand, the majority of chief residents tended to agree with both of these statements, suggesting that chief residents generally believe the PACS at their institution helps to increase their productivity at least to some extent (Table 1). Finally, program directors and chief residents had mostly neutral to positive views when it came to the ease of use of their PACS for on-call studies, but chief residents were more positive (average rating, 3.63 and 4.04, respectively; Table 1). This seems to reflect general satisfaction with current PACS platforms at these teaching hospitals; however, it should be noted that five program directors and one chief resident disagreed or strongly disagreed with this statement. Due to the limited sample, future polling is needed to accurately determine the most significant reasons for low satisfaction with PACS used on-call. While many are satisfied with their PACS, not everyone is happy with the user-friendliness of their institution’s PACS (Table 1).
Although the results of this study represent 32 % of ACGME-accredited radiology teaching hospitals, some of the results rely on a relatively smaller sample of the chief resident and program director population (survey response rate of 8.9 and 24.9 %, respectively). Therefore, the attitudes of respondents may not necessarily reflect the views of all chief residents and program directors. Possibly, those who are unhappy with their PACS were less likely to spend the time to complete this survey. Furthermore, due to the small sample size, it was not possible to draw conclusions regarding which specific PACS platform was easiest to use or decreased turnaround time the most. Future surveys could be directed towards obtaining a larger sample of both program directors and chief residents. More specific questions targeting the software features and qualities of their specific PACS vendor may shed more light on why certain PACS are the most popular. Finally, it would also be beneficial to get more details of specifically how many hospitals fall under the network of a respondent’s institution and which hospital networks have different PACS at different hospitals.
Conclusions
Program directors and chief residents in radiology were surveyed regarding their current use of PACS and DICOM viewers while on-call, and their opinions regarding their institution’s PACS. The results show there are a great variety of different PACS platforms used by teaching hospitals represented in this study, but GE, Phillips, and Agfa were some of the most prevalent. There is insufficient evidence to suggest that any specific PACS platform impacts the performance of radiologists on-call versus other PACS platforms. The majority of respondents prefer to use their institution’s PACS instead of an alternative DICOM viewer. Finally, program directors and chief residents believe there should be a single, unified PACS at an institution for viewing on-call studies, and that the PACS should be integrated with their institution’s EMR; however, only 54 % of those surveyed report having a PACS platform that is integrated with EMR.
References
Oosterwijk H: PACS fundamentals. OTech Inc, Aubrey, 2004
Siegel EL, Reiner BI, Siddiqui KM: Ten filmless years and ten lessons: a 10th-anniversary retrospective from the Baltimore VA Medical Center. J Am Coll Radiol 1:824–833, 2004
Fang YC, Yang MC, Hsueh YS: Financial assessment of a picture archiving and communication system implemented all at once. J Digit Imaging 19:44–51, 2006
Macyszyn L, Lega B, Bohman LE, et al: Implementation of a Departmental Picture Archiving and Communications System (PACS): a productivity and cost analysis. Neurosurgery 2013
Mansoori B, Erhard KK, Sunshine JL: Picture archiving and communication system (PACS) implementation, integration & benefits in an integrated health system. Acad Radiol 19:229–235, 2012
Joshi V, Lee K, Melson D, Narra RV: Empirical investigation of radiologists’ priorities for PACS selection: an analytical hierarchy process approach. J Digit Imaging 24:700–708, 2011
Ondo K: PACS direct experiences: implementation, selection, benefits realized. J Digit Imaging 17:249–252, 2004
Smith-Bindman R, Miglioretti DL, Johnson E, et al: Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 307(22):2400–2409, 2012
Deloney LA, Rozenshtein A, Deitte LA, Mullins ME, Robbin MR: What program directors think: results of the 2011 Annual Survey of the Association of Program Directors in Radiology. Acad Radiol 19:1583–1588, 2012
Sauk S, Jokerst C, Gould J, Evens R: Results of the 2012 Survey of the American Association of Academic Chief Residents in Radiology. Acad Radiol 20:320–331, 2013
O’Connell T, Chang D: Informatics in radiology: web-based preliminary reporting system for radiology residents with PACS integration. RadioGraphics 32:2127–2134, 2012
Towbin A, Paterson B, Chang P: Informatics in radiology. Computer-based simulator for radiology: an educational tool. RadioGraphics 28:309–316, 2008
Branstetter B, Uttecht S, Lionetti D, Chang P: Informatics in radiology. Simple DICOM suite: personal productivity tools for managing DICOM objects. Radiographics 27:1523–1530, 2007
Weiss D, Siddiqui K, Scopelliti J: Radiologist assessment of PACS user interface devices. J Am Coll Radiol 3:265–273, 2006
Nagy P, Bowers G, Reiner BI, Siegel EL: Defining the PACS profession: an initial survey of skills, training and capabilities for PACS administrators. J Digit Imaging 18(4):252–259, 2005
Jha AK, DesRoches CM, Campell G, et al: Use of electronic health records in US hospitals. N Engl J Med 360(16):1628–1638, 2009
Li P, Bahensky JA, Jaana M, Ward MM: Role of multihospital system membership in electronic medical record adoption. Health Care Manage Rev 33(2):169–177, 2008
HITECH Programs & Advisory Committees. Available at http://www.healthit.gov/policy-researchers-implementers/hitech-programs-advisory-committees. Accessed May 23, 2014.
Moses H, Matheson DH, Dorsey R, et al: The anatomy of health care in the United States. JAMA 310(18):1947–1963, 2013
De Maio P, White LM, Bleakney R, Menezes RJ, Theodoropoulos J: Diagnostic accuracy of an iPhone DICOM viewer for the interpretation of magnetic resonance imaging of the knee. Clin J Sport Med 2013
Ge Y, Ahn DK, Unde B, Gage HD, Carr JJ: Patient-controlled sharing of medical imaging data across unaffiliated healthcare organizations. J Am Med Inform Assoc 20:157–163, 2013
Ratib O, Swiernik M, McCoy JM: From PACS to integrated EMR. Computerized Medical Imaging and Graphics. Comput Med Imaging Graph 27(2–3):207–215, 2003
Conflict of Interest
All authors state they have no conflicts of interest.
No grants or other institutional funding was used to conduct this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tesoriero, J.A., Eddy, P. & Hasso, A.N. PACS Used While On-Call: A National Survey of Radiology Program Directors and Chief Residents. J Digit Imaging 28, 205–212 (2015). https://doi.org/10.1007/s10278-014-9741-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-014-9741-9