Abstract
Evaluate, through a randomized clinical trial, the efficacy of brushing associated with oral irrigation in maintaining implant and overdenture hygiene. Thirty-eight participants, who had a clinically acceptable conventional maxillary complete denture and mandibular overdenture retained by either implants or mini-implants using an O-ring-retained system, were enrolled to participate in the study. They were instructed to use two different hygiene methods, in a random sequence for a period of 14 days, with a 7-day wash-out interposed period: (I) mechanical brushing (MB); (II) association of mechanical brushing with oral irrigation (WP). Biofilms from both subgingival sulci and overdentures were collected and processed by Checkerboard DNA–DNA hybridization method at baseline and after using the proposed hygiene protocols. Comparisons were performed using Wilcoxon test and Friedman test with Benjamini–Hochberg false discovery rate, followed by Conover post-hoc test (α = 0.05). In the subgingival sulci-related biofilm, a lower number of microbial cells were detected, after WP compared to the MB method (P < 0.001). The findings of overdenture-related biofilm suggest that both methods were similar (P = 0.607) being the identified microbiota qualitatively coincident after each method. Despite the number of microbial counts, it was concluded that the association of mechanical brushing with oral irrigation was more effective in reducing microorganisms in the subgingival sulci biofilm; however, the same outcome was not observed in the overdentures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Implant-supported prostheses have become the treatment of choice for fully edentulous patients, mainly because they are related to an improvement in the oral health‐related quality of life [1]. However, it has been related to an increase in the peri-implant diseases and, consequently, a growing concern with longevity of the treatment [2, 3]. In spite of the development and improvement of the techniques and materials, aiming to reach a higher clinical success rate of implants, through osseointegration and biocompatibility, long-term success depends mainly on the efforts of both patients and professionals in maintaining the health of the peri-implant tissues [4, 5]. Thus, adequate daily hygiene techniques are essential for biofilm control and the prevention of peri-implant diseases [6].
Since biofilm accumulation is directly associated with mucositis and peri-implantitis [7], hygiene instructions for daily patient care should be addressed even before implant placement. In addition, as a result of advanced bone resorption, it may be difficult to locate the abutments,therefore, it is important that hygiene methods take into consideration the implant design, location, angulation, length and position of the abutments and the type of implant-supported prosthesis. These factors, together, are related to bring difficulty in accessing the implants, which may compromise proper oral hygiene and consequently suitable biofilm control [8].
Food debris, biofilm and calculus are often found on the surfaces of overdentures and brushing method alone is insufficient to ensure proper biofilm control. Additionally, studies have shown that chemical cleaners can promote deleterious effects on the overdentures properties, such as acrylic resin bleaching, metal corrosion and deterioration of joint systems [9, 10]. Despite numerous efforts to establish an appropriate hygiene method for implant and implant-supported prostheses, studies are required to evaluate the effectiveness of oral irrigation devices.
Oral irrigation devices, which have been known as hydro-propellers or water floss, are a promising option for implant and implant-supported prostheses hygiene. These devices work by pulsating pressured water, which can be associated with antiseptic agents, being able to reach areas that are commonly difficult to access in routine oral hygiene methods [11]. Its use is indicated in several cases, such as patients with reduced manual dexterity, the presence of periodontal or peri-implant pockets, very close implants and patients under orthodontic treatment [12]. Thus, oral irrigation devices could be applied as an adjuvant method to biofilm control in hard-to-reach areas [11, 13]. Nonetheless, studies evaluating the effectiveness of oral irrigation in removal subgingival sulci and overdenture-related biofilm were not yet performed.
In view of the above, the objective of this study is to evaluate, through a randomized crossover clinical study, whether the association of the brushing method with oral irrigation improves the hygiene care of overdenture users. The study investigated the effect of the proposed treatments in reducing the microbial load on the subgingival sulci and overdenture-related biofilms. The null hypothesis of the study is that both methods would have the same effect on the biofilm controlling.
Materials and methods
Sample size calculation
The sample size was estimated considering data from a pilot study. Means and standard variations values of total microbial cell counts, in the subgingival sulci biofilm, were considered in sample size calculation. A total of 38 participants were considered sufficient enough to detect relevant differences (α = 0.05; β = 0.20). In addition, to allow for possible withdrawals and losses, 20% was added to the estimated sample size, so that a total of 42 patients were included.
Ethical statement
The study was approved and registered by the institutional ethics committee (CAAE: 35,321,514.1.0000.5419), in accordance with international protection guidelines and Helsinki Declaration. In agreement with ethical principles involving research in human subjects, all the procedures were done after informed and written signed consent by each subject. The study was registered at WHO International Clinical Trials Registry Platform, under identification number RBR-8d4vkr.
Inclusion and exclusion criteria
Thirty-eight participants were selected from the dental clinic of the Ribeirão Preto Dental School (University of São Paulo, Brazil). Enrolled participants were adults, aged at least 45 years, healthy and completely edentulous, either male or female, using maxillary conventional complete dentures and mandibular overdentures retained by two to four implants using an O-ring-retained system. The maxillary and mandibular dentures should be clinically satisfactory and fabricated by heat-polymerized acrylic resin and acrylic artificial teeth. The implants and overdentures should have been in function for at least six months, and the retention rings, from one to six months.
The removal of biofilm and calculus present on the surfaces of the implants and prosthetic abutments was performed by curettage. Thus, all the patients presented a similar initial clinical condition. In addition, prostheses were also properly cleaned and returned to their owners.
The ones who were excluded from the study were those uncontrolled diabetic patients; immunosuppressed patients; patients who had taken antibiotics, antifungals or corticosteroids in the last three months; current use of anticoagulants, anticonvulsants and immunosuppressants; and patients with relined, repaired or fractured prostheses.
Study design
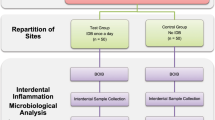
Patients were randomly assigned according a list with random numbers generated by a computer program. The numbers corresponded to the possible sequences to the following hygiene methods: (1) Mechanical brushing method – MB (Control); (2) Association of mechanical brushing (MB method) with oral irrigation – WP (Experimental). To MB method, participants received a hygiene kit containing a specific brush for dentures (Bitufo®, Itupeva, SP, Brazil), a soft bristle toothbrush (Oral B Indicator Plus – Procter & Gamble, São Paulo, SP, Brazil) and an dentifrice (Trihydral, Perland Pharmacos Ltda, Cornélio Procópio, PR, Brazil). To WP method, participants received besides the hygiene supplies to mechanical brushing, a low-pressure oral irrigation device (Waterpik, WP-360 Model, Waterpik, Fort Collins, CO, EUA). At the beginning of each hygiene method, the participants were individually instructed to correctly handle the denture brush, the toothbrush and the oral irrigation device. Regarding the mechanical brushing method, participants were instructed to adopt the following sequence: (1) Remove and rinse the prostheses after eating; (2) Clean the mouth and peri-implant tissues, in alternating horizontal motion, using the soft bristle brush and toothpaste provided; (3) Brush the prostheses, in alternating horizontal and vibrating motion, using the denture brush and toothpaste provided. Furthermore, participants were instructed to brush their dentures and peri-implant tissues after breakfast, lunch, and dinner (during 2 min, 3 times a day) and not use any hygiene products other than those supplied during the study period.
In the WP period, patients applied oral irrigation once a day after their last daily brushing. For oral hygiene, participants were instructed to set the oral irrigator tip close to the peri-implant tissues and prosthetic abutments without touching them. The water jet should be uniformly directed toward the gingival margin surrounding the implant during 20 s for each implant. For overdenture hygiene, the water jet should be uniformly directed toward the region of the capsules and retaining rings at approximately 0.5 cm for 20 s for each capsule/ring.
All the participants used each method for 14 days in a crossover sequence. A washout period was established for 7 days between the methods, in which the patients were oriented to use their habitual hygiene care. Professional cleaning of the implants and dentures was also provided after washout period to provide the same clinical condition before the beginning of second hygiene method.
Sample collection, processing and DNA–DNA hybridization
At the baseline and after 14 days of the application of each hygiene method, the number of microbial species colonizing the subgingival sulci and overdentures was evaluated using the checkerboard DNA–DNA hybridization technique. Species selected as the target for detection (34 bacterial and 5 fungal species) included primary colonizers, pathogens associated with denture stomatitis and periodontal disease-related microorganisms.
The implant sites were isolated with cotton rolls and air-dried prior to biofilm collection. Subgingival sulci biofilms were collected from the highest values of probing depth sites using two sterile paper points (Dentsply Indústria e Comércio Ltda., Petrópolis, RJ, Brazil) during 30 s. Overdentures were rinsed in running water for 5 s and air-dried using a triple syringe, for 10 s, before biofilm collecting. In the aseptic zone, sterile microbrushes (KG Brush Fine; KG Sorensen; Medical Burns Indústria e Comércio de Pontas e Brocas Ltda; Cotia, SP, Brazil) were rubbed on the O-ring-retained system and retention ring surfaces. One microbrush was used for each capsule/ring.
All the procedures used for sample processing and the interpretation of the results were carried out as described previously [14]. The samples were transferred to individual microtubes containing 150 μL of TE [(10 mM Tris–HCl (Sigma Aldrich, St. Louis, MO, EUA) and 1 mM EDTA (Sigma), pH 7.6)] followed by the addition of 150 μL of 0.5 M NaOH (Sigma Aldrich) for cell lysis. Thus, the DNA was denatured (95 °C, 5 min), precipitated [5 M C2H7NO2 (Sigma Aldrich)] and deposited in individual hybridization channels (Minislot 30, Immunetics, Cambridge, MA, EUA) on nylon membranes (Hybond N + , GE Healthcare, Chalfont, Buckinghamshire, United Kingdom). Genomic DNA mixtures containing 105 and 106 cells from each of the 39 species studied were used as comparison standards for microbial quantification. After the pre-hybridization treatment, the membranes received genomic probes (1 ng/μL) of the target species. Previous sensitivity and specificity tests were performed for each labelled probe to optimize the amount of probe needed to detect both 105 and 106 microbial cells of each species with the lowest possible background.
The hybridization reaction between the investigated biofilm samples and the genomic probes was performed in a hybridization oven (63 °C, 16 h) under gentle agitation. Subsequently, the membranes were washed twice (67 °C, 30 min) in wash solution 1 [2 M Urea (Sigma Aldrich), 0.1% Sodium dodecyl sulfate (Sigma Aldrich), 50 mM NaH2SO4 pH 7 (Sigma Aldrich), 150 mM NaCl, 1 mM MgCl2 (Sigma Aldrich), 0.4% w/v Blocking Reagent (GE Healthcare)]. Then, two more washes (RT, 15 min) were performed with wash solution 2 [1 M Trizma (Sigma Aldrich), 2 M NaCl e 1 M MgCl2].
Positive hybridization signals were directly detected by chemiluminescence (CDP-Star Reagent, GE Healthcare) by exposure to a film for autoradiography (HyperFilm, GE Healthcare). The exposed films were revealed and fixed in conventional radiographic processing solutions (Kodak, Rochester, NY, EUA) and scanned. The numbers of microbial cells presented in the tested samples were determined using the software Image Quant TL (GE Healthcare) by comparisons with the reference standards of 105 and 106 cells.
Data analysis
The blinding of most of the researchers involved was sought because blinding of the participants to the methods used was impossible. A researcher (A), who was not involved with other operational phases of the research, obtained a list with random numbers. These sequences had the same probability of being assigned. Another researcher (B), carrying the randomization list, explained the protocol to participants and delivered the products to them. This researcher was also responsible for providing oral hygiene instructions to participants, explaining the correct handling of the denture brush, toothbrush and oral irrigation device. A researcher (C) collected the biofilm from peri-implant sulci and overdentures. A Researcher (D) conducted the laboratorial steps and forwarded the tabulated data to Researcher (E), who conducted the statistical analysis.
In this study, site (peri-implant sulci and overdentures) and hygiene methods (MB and WP) were considered as the variables. The data were first tested for homoscedasticity and normality distribution, and the influence of the hygiene methods was assessed using Wilcoxon test and Friedman test with Benjamini–Hochberg false discovery rate. Subsequent multiple comparisons were performed by Conover post-hoc test. All analyses were conducted with R: A Language and Environment for Statistical Computing Software, at a significance level of 0.05.
Results
Participants’ characteristics
A total of 77 individuals were assessed. Third-five individuals were not included: 9 did not meet inclusion criteria; 6 did not agree to participate; 18 did not return to appointments; and 2 had received a new denture. During the experiment, 4 withdrew because of incorrect implementation of the protocol and failure to attend appointments (Fig. 1). Thus, the final sample consisted of 38 participants, 9 male and 29 female (mean age: 57.9 years; standard deviation 6.2), having an elementary school education level (65.8%). Participants' professional activities were retired/pensioner (21.1%), unemployed (36.8%) and employed (42.1%) and the marital status was predominantly married (63.2%) (Table 1).
Effectiveness of hygiene protocols
The checkerboard DNA–DNA hybridization technique allowed the identification and quantification of 39 strains present in the subgingival sulci biofilm and overdentures (capsules and retaining rings), of thirty-eight participants, before (baseline) and after the hygiene methods. Pathogenic species related to the etiology of perimplantitis were evaluated according to five microbial complexes (red, orange, yellow, green and purple) [15]. The less frequently associated colonizing microorganisms in periodontal diseases were grouped in the group “other species” and species of Candida were grouped in the group “fungi”. Table 2 shows the microorganism genome counts present in subgingival sulci and overdenture-related biofilms, at baseline, MB and WP.
In the subgingival sulci-related biofilm, Candida dubliniensis, Streptococcus sobrinus, Streptococcus salivarius, Pseudomonas putida, Prevotella intermedia and Klebsiella pneumoniae were not identified at baseline, as well as after the use of hygiene methods. Lower counts of Campylobacter rectus (P = 0.001) and Porphyromonas endodontalis (P = 0.003) were observed after WP in comparison to MB. Moreover, a significant reduction of Veillonella parvula (P = 0.012) was observed after WP in comparison to baseline. Aggregatibacter actinomycetemcomitans, Bacteroides fragilis, Enterococcus faecalis, Lactobacillus casei, Staphylococcus pasteuri, Streptococcus constellatus and Streptococcus mutans were not identified after WP. After MB, there were no counts of Neisseria mucosa, Candida glabrata and Candida krusei. Regarding genome counts of microorganisms in the different complexes, statistically significant difference was found, indicating reduction of orange (P < 0.001) and green (P = 0.030) complexes, as well as microorganisms grouped as “other species” (P = 0.006) after WP in comparison to MB. Purple complex presented lower bacterial counts after WP in comparison to baseline (P = 0.012) (Table 3). When comparing the total microbial cell counts, a statistically significant difference between the hygiene methods was observed (P = 0.007). After WP, a lower number of microbial cells were detected in the subgingival sulci biofilm, compared to the MB method (P < 0.001). Regarding the baseline, MB promoted a reduction in the cell counts, but the difference was not significant (Fig. 2).
Total counts of microbial cells at peri-implant sulci (Baseline, MB, WP) and overdenture (Baseline, MB, WP). A lower number of microbial cells were detected, after WP compared to the MB method (P < 0.001). In the overdenture-related biofilm, both methods were similar (P = 0.607). Small letters: comparisons at peri-implant sulci. Capital letters: comparisons at overdenture. Different letters indicate the significant difference (P < 0.05)
In the overdenture biofilm, C. dubliniensis was not identified, regardless of the period evaluated. Lower counts of Lactobacillus casei (P = 0.032) and Streptococcus parasanguinis (P = 0.049) were observed after WP in comparison to baseline. None of five microbial complexes related to the etiology of perimplantitis, microorganisms grouped as “other species” and fungi presented significant alteration regarding bacterial counts after MB and WP (Table 3). Moreover, when comparing the total microbial cell counts, no statistically significant difference between the hygiene methods was observed (P = 0.607) (Fig. 2).
Discussion
Studies involving the daily hygiene of implants and implant-supported prostheses are scarce and new approaches should be addressed to the patients. Knowing that biofilm control is essential for the longevity of rehabilitation treatment, an association between conventional brushing and oral irrigation was evaluated, for daily hygiene of implants and overdentures, through a randomized crossover clinical study. Based on the results, the null hypothesis was rejected, since there was statistical difference between the hygiene methods in microbial cell counts in the subgingival sulci biofilm.
With respect to the subgingival sulci-related biofilm, the results showed that after WP hygiene method, there were lower numbers of microbial cells in comparison to the MB hygiene method. The association of mechanical brushing with oral irrigation not only reduced microbial load, but also reduced the number of species identified (Table 2). Contrary to these results, previous studies have shown similar effects on the peri-implant microbiota after using different materials or hygiene methods [16,17,18]. At this point, it is worth highlighting that there are no clinical studies in the literature that relates the effect of oral irrigation on the subgingival sulci-related biofilm.
When used in the treatment of gingivitis, oral irrigation has shown a remarkable effect on the subgingival marginal microbiota [19]. It has been suggested that the reduction of the clinical signs of gingivitis may be related to the reduction of the specific bacteria present in the biofilm and/or the reduction in the number of toxic substances produced by them [18]. These findings can be justified by the action of the irrigation apparatus, which first generates a direct impact of the jet against the surface and then the water or solution flows through the surfaces promoting a rinsing effect [20, 21]. When it reaches the periodontal or peri-implant sulcus, this hydrodynamic action is responsible for disaggregating the subgingival sulci biofilm, which can suffer quantitative and qualitative alterations [20].
In our study, a reduction in the majority of the evaluated species was verified in the subgingival sulci biofilm (Table 2); however, only the reductions in C. rectus and P. endodontalis were statistically significant, when comparing the effect of WP and MB on individual bacterial counts. Considering the five microbial complexes related to the etiology of perimplantitis, lower bacterial counts were evaluated to orange, green and purple complexes. This may be considered an important result regarding the use of this method in the daily maintenance of health tissues and in the prevention of the development of peri-implant diseases, once they are considered periodontopathogenic species frequently associated with peri-implantitis [15, 22, 23]. A. actinomycetemcomitans, B. fragilis, E. faecalis, L. casei, S. pasteuri, S. constellatus and S. mutans were not identified after WP hygiene method. It was already reported that interactions between different species and even different kingdoms, can promote the development of a resistant polymicrobial biofilm [24]. Therefore, reduction of microbial colonization could represent a discontinuity in network of microbial interactions restoring peri-implant tissues health.
It was observed that the reductions of microbial strains were different in overdenture and peri-implant sulci. In the overdenture biofilm, we noticed a significant reduction of Lactobacillus casei and Streptococcus parasanguinis. Although modest alteration in bacterial counts could be observed, after use of both hygiene methods, the reduction was not statistically significant. In addition, none of five microbial complexes related to the etiology of perimplantitis, microorganisms grouped as “other species” and fungi presented significant alteration regarding bacterial counts after MB and WP (Table 3). Usually, biofilm on prosthetic surfaces exhibits different complexity and degree of maturation, being composed of distinct types of microorganisms, including aerobic, facultative and strict anaerobic bacteria and fungi [25]. Maybe, the characteristics of overdenture and subgingival sulci biofilm and interactions inter and intra species could explain the variation in the reduction of different microorganisms.
S. sobrinus, S. salivarius, P. putida, P. intermedia and K.pneumoniae were not found in subgingival sulci-related biofilm in any of the study evaluations. Additionally, C. dubliniensis was not found on both overdenture and subgingival sulci-related biofilm. Such result may be related either to the absolute absence of this specie at the evaluation time, or to its low concentration in function of a limitation of the checkerboard DNA–DNA hybridization technique, which only allows microbial detection from a minimum of 104 cells. Considering the detection failure occurrence, calibration of probe concentration, to increase the test sensitivity, might prevent the event in future studies. Nonetheless, Socransky et al. observed that the adjustment of sensitivity can reduce the ability of the method to quantify larger numbers of cells and also amplify non-specific signals [26].
In the overdenture-related biofilms, both hygiene methods were similar and the identified microbiota appeared qualitatively coincident after each hygiene protocol. This matter was not expected since the proposed hygiene protocol was well defined, and patients were oriented and motivated to follow it. It is known that brushing is not sufficient to remove the microorganisms present into micro-retention and irregularities of the prosthetic surfaces. Bacteria and yeasts can successfully colonise these areas being more difficult to remove them mechanically [27, 28]. By this reason, the oral irrigation device, originally developed for oral cavity hygiene, was used to reach areas that are difficult to access with the brush bristles. However, the results showed that the experimental method was not adequate to promote a significant reduction in the microorganisms present in the prosthetic components of the overdentures.
Regarding the daily care of implants and peri-implant tissues, several materials for oral hygiene have been shown to be safe; among them are interdental brushes, hand or electric toothbrushes, different types of dental threads, mouthwashes and oral irrigation devices [29, 30]. However, to date, there is no definition of an effective protocol for proper daily implant hygiene [31]. In the present study, the products were selected to provide an effective cleaning of the prosthesis, components and prosthetic abutments, aiming the biofilm removal of peri-implant tissues and overdentures. A soft toothbrush with a small head and straight profile was chosen to avoid damage to the peri-implant tissues and prosthetic abutments, as well as to ensure access between the implants and hard-to-reach areas [32]. A denture-specific brush was selected to promote the overdentures cleanness. A specific brush was recommended because its anatomical shape is appropriate to provide cleaning of the internal and external surfaces of the prosthesis [33]. Trihydral dentifrice was provided during the research period as its abrasiveness is similar to those specific-denture dentifrices [34]. Moreover, it has no acid potential which prevents excessive damage to the material [35] avoiding the possibility of corrosion of the surface of the titanium components [36, 37].
The oral irrigation device has been effective in removing biofilm and food residues; however, it should be used at low-pressure because its misuse and excessive water pressure can damage the junctional epithelium and lead to bacteria spreading [29]. For this reason, only the tip for low-pressure irrigation was given to the patients. The portable model was chosen due to its practicality, lightness and greater ease of use in daily practice. Although water is not classified as an antiseptic or antimicrobial agent, its use in oral irrigation devices at low-pressure has been recommended [32, 38]. The experimental period was set at 14 days according to data reported previously [39]. Cutler et al. demonstrated that oral irrigation with water for 14 days had an improved therapeutic benefit for adult periodontitis over that of routine oral hygiene alone. After 14 days, the authors evidenced a down-modulation of the pro-inflammatory cytokine profile, reduction in probing pocket depths, bleeding on probing, gingival index and plaque index.
Based on the absence of antibiofilm activity of WP on overdentures, the association of oral irrigation with antimicrobial solutions could result in the dissolution of the organic matrix of the biofilm, which along with the hydrodynamic action, would promote the removal of the biofilm more effectively. Therefore, future studies could be carried out to prove this hypothesis. In the present study, 63.2% of the patients were elderly. Due to impaired manual dexterity [39] and decreased visual acuity [40], the performance of proper and effective hygiene procedures may have been compromised. This factor could explain the maintenance of microbial cells in the prosthetic components of overdentures. Therefore, the fundamental role of maintenance programs is related to the choice of hygiene methods, which should be appropriate for each case and in the motivation of the patient. It has been noted that patients adapt more easily to a smaller number of materials, simplicity of use, affordable cost and less time spent for hygiene [11, 29].
A limitation of the study is related to the short period of use of the hygiene methods. A longer period of use and follow-up would allow a better evaluation of the effects of brushing associated with oral irrigation on the long-term maintenance of peri-implant tissues and overdentures. Another limitation concerns the use of the DNA checkerboard technique to evaluate the antimicrobial action of the hygiene methods. Besides allowing the simultaneous evaluation of multiple species of microorganisms in a large number of samples, the checkerboard DNA–DNA hybridization technique allows identification and quantification of both viable and non-viable species [41]. Indeed, the amount of viable cells could be measured by culture methods,however, considering handling and culturing difficulties associated with traditional culture methods, particularly in relation to fastidious and anaerobic-strict species, molecular methods would produce more satisfactory results.
The comparison between antimicrobial solutions and water, when used in the oral irrigation device, is an important analysis to be made in future studies, aiming to evaluate the effect of the association of hydrodynamic action with the chemical solution, when used in the maintenance of peri-implant health. In addition, analyses regarding the adverse effects on the overdentures’ materials, such as the loss of retention of the rings, after the use of the hygiene methods, are required. Also, the association with other dentifrices and antimicrobial agents could be evaluated, simulating the period of six months of use, the time commonly recommended by manufacturers for exchange of retention rings. It is known that the retentive devices are composed of a variety of materials, such as silicon, nylon and fluorocarbon, so it would be important to compare the damage caused by the hygiene methods on the materials, as well as evaluate the effects of the properties of different materials on microbial adhesion.
Conclusion
Within the limitation of this study, brushing associated with oral irrigation was more effective in reducing the total number of microorganisms present in the subgingival sulci biofilm. However, the antimicrobial action against the microorganisms in the prosthetic components of overdentures was not observed.
References
Oh SH, Kim Y, Park JY, Jung YJ, Kim SK, Park SY. Comparison of fixed implant-supported prostheses, removable implant-supported prostheses, and complete dentures: patient satisfaction and oral health-related quality of life. Clin Oral Implants Res. 2016;27:e31–e3737.
Meijer HJA, Raghoebar GM, de Waal YCM, Vissink A. Incidence of peri-implant mucositis and peri-implntitis in edentulous patients with an implant-retained mandibular overdenture during a 10-year follow-up period. J Clin Periodontol. 2014;41:1178–83.
Liu XQ, Chen QW, Feng HL, et al. Oral hygiene maintenance of locator attachments implant overdentures in edentulous population: A longitudinal study. Beijing Da Xue Xue Bao Yi Xue Ban. 2019;51:136–44.
Jepsen S, Berglundh T, Genco R, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015;42:S152–S157157.
Monje A, Aranda L, Diaz KT, et al. Impact of maintenance therapy for the prevention of peri-implant diseases: a systematic review and meta-analysis. J Dent Res. 2016;95:372–9.
Pulcini A, Bollaín J, Sanz-Sánchez I, et al. Clinical effects of the adjunctive use of a 0.03% chlorhexidine and 0.05% cetylpyridinium chloride mouth rinse in the management of peri-implant diseases: A randomized clinical trial. J Clin Periodontol. 2019;46:342–53.
Canullo L, Peñarrocha-Oltra D, Covani U, Botticelli D, Serino G, Penarrocha M. Clinical and microbiological findings in patients with peri-implantitis: a cross-sectional study. Clin Oral Implants Res. 2016;27:376–82.
Todescan S, Lavigne S, Kelekis-Cholakis A. Guidance for the maintenance care of dental implants: Clinical review. J Can Dent Assoc. 2012;78:c107.
Derafshi R, Mohaghegh M, Saki M, Safari A, Haghighi MR. The effects of denture cleansing solutions on the retention of attachments of implant supported overdentures. J Dent (Shiraz). 2015;16:68–72.
Kürkcüoğlu I, Özkir SE, Köroğlu A, Sahin O, Yilmaz B. Effect of denture cleansing solutions on different retentive attachments. J Prosthet Dent. 2016;115:606–10.
Lyle DM. Implant maintenance: Is there an ideal approach? Compend. 2013;34:386–9.
Sharma NC, Lyle DM, Qaqish JG, Galustians J, Schuller R. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2008;133:565–71.
Magnuson B, Harsono M, Stark PC, Lyle D, Kugel G, Perry R. Comparison of the effect of two interdental cleaning devices around implants on the reduction of bleeding: a 30-day randomized clinical trial. Compend Contin Educ Dent. 2013;34:2–7.
Nascimento C, Miani PK, Pedrazzi V, et al. Leakage of saliva through the implant-abutment interface: in vitro evaluation of three different implant connections under unloaded and loaded conditions. Int J Oral Maxillofac Implants. 2012;27:551–60.
Porras R, Anderson GB, Caffesse R, Narendran S, Trejo PM. Clinical response to 2 different therapeutic regimens to treat peri-implant mucositis. J Periodontol. 2002;73:1118–25.
Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent R. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998;25:134–44.
Heitz-Mayfield LJ. Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol. 2008;35:292–304.
Swierkot K, Brusius M, Leismann D, et al. Manual versus sonic-powered toothbrushing for plaque reduction in patients with dental implants: an explanatory randomized controlled trial. Eur J Oral Implantol. 2013;6:133–44.
Chaves ES, Kornman KS, Manwell MA, Jones AA, Newbold DA, Wood RC. Mechanism of irrigation effects on gingivitis. J Periodontol. 1994;65:1016–21.
Cobb CM, Rodgers RL, Killoy WJ. Ultrastructural examination of human periodontal pockets following the use of an oral irrigation device in vivo. J Periodontol. 1988;59:155–63.
Ciancio SG. The dental water jet: a product ahead of its time. Compendium. 2009;30:7–14.
Mombelli A, Décaillet F. The characteristics of biofilms in peri-implant disease. J Clin Periodontol. 2011;38:203–13.
Ebadian AR, Kadkhodazadeh M, Zarnegarnia P, Dahlén G. Bacterial Analysis of Peri-Implantitis and Chronic Periodontitis in Iranian Subjects. Acta Med Iran. 2012;50:486–92.
Marsh PD, Zaura E. Dental biofilm: ecological interactions in health and disease. J Clin Periodontol. 2017;18:12–22.
Nikawa H, Hamada T, Yamashiro H, Kumagai H. A review of in vitro and in vivo methods to evaluate the efficacy of denture cleansers. Int J Prosthodont. 1999;12:153–9.
Socransky SS, Haffajee AD, Smith C, et al. Use of checkerboard DNA–DNA hybridization to study complex microbial ecosystems. Oral Microbiol Immunol. 2004;19:352–62.
Shay K. Denture hygiene: a review and update. J Contemp Dent Pract. 2000;1:28–41.
Zissis AJ, Polyzois GL, Yannikakis SA, Harrison A. Roughness of denture materials: a comparative study. Int J Prosthodont. 2000;13:136–40.
Kracher CM, Smith WS. Oral health maintenance of dental implants. Dent Assist. 2010;79:27–35.
Loroupoulou A, Slot DE, Van der Weijden F. Mechanical self-performed oral hygiene of implant supported restorations: a systematic review. J Evid Based Dent Pract. 2014;14:60–9.
Pedrazzi V, Escobar EC, Cortelli JR, et al. Antimicrobial mouthrinse use as an adjunt method in peri-implant biofilm control. Braz Oral Res. 2014;28:1–9.
Humphrey S. Implant Maintenance. Dent Clin North Am. 2006;50:463–78.
Fernandes RAG, Lovato-Silva CH, Paranhos HFO, Ito IY. Efficacy of three denture brushes on biofilm removal from complete dentures. J Appl Oral Sci. 2007;15:39–433.
Leite VMF, Pinheiro JB, Pisani MX, et al. In vitro antimicrobial activity of an experimental dentifrice based on Ricinus communis. Braz Dent J. 2014;25:191–6.
Fais LMG, Fernandes-Filho RB, Pereira-da-Silva MA, Vaz LG, Adabo GL. Titanium surface topography after brushing with fluoride and fluoride-free toothpaste simulating 10 years of use. J Dent. 2012;40:265–75.
Robin A, Meirelis JP. Influence of fluoride concentration and pH on corrosion behavior of titanium in artificial saliva. J Appl Electrochem. 2007;37:511–7.
Santiago Júnior JF, Lemos CAA, Batista VES, et al. Maintenance in implant-supported prostheses: oral hygiene. Rev Odontol Araç. 2013;34:56–64.
Cutler CW, Stanford TW, Abraham C, et al. Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque. J Clin Periodontol. 2000;27:134–43.
Kulak-Ozkan Y, Kazazoglu E, Arikan A. Oral hygiene habits, denture cleanliness, presence of yeasts and stomatitis in elderly people. J Oral Rehabil. 2002;29:300–4.
Schembri A, Fiske J. The implications of visual impairment in an elderly population in recognizing oral disease and maintaining oral health. Spec Care Dentist. 2001;21:222–6.
Nascimento C, Issa JPM, Watanabe E, Ito IY. DNA Checkerboard method for bacterial pathogen identification in oral diseases. Int J Morphol. 2006;24:619–24.
Acknowledgments
We thank the Coordination for the Improvement of Higher Education Personnel—Brazil (CAPES)—Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All other authors declare no conflict of interest associated with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Salles, M.M., Oliveira, V.C., Macedo, A.P. et al. Brushing associated with oral irrigation in maintaining implants and overdentures hygiene – a randomized clinical trial. Odontology 109, 284–294 (2021). https://doi.org/10.1007/s10266-020-00543-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-020-00543-7