Abstract
Dental caries is a type of oral microbiome dysbiosis and biofilm infection that affects oral and systemic conditions. For healthy life expectancy, natural bacteriostatic products are ideal for daily and lifetime use as anti-oral infection agents. This study aimed to evaluate the inhibitory effects of abietic acid, a diterpene derived from pine rosin, on the in vitro growth of cariogenic bacterial species, Streptococcus mutans. The effective minimum inhibitory concentration of abietic acid was determined through observation of S. mutans growth, acidification, and biofilm formation. The inhibitory effects of abietic acid on the bacterial membrane were investigated through the use of in situ viability analysis and scanning electron microscopic analysis. Cytotoxicity of abietic acid was also examined in the context of several human cell lines using tetrazolium reduction assay. Abietic acid was found to inhibit key bacterial growth hallmarks such as colony forming ability, adenosine triphosphate activity (both planktonic and biofilm), acid production, and biofilm formation. Abietic acid was identified as bacteriostatic, and this compound caused minimal damage to the bacterial membrane. This action was different from that of povidone-iodine or cetylpyridinium chloride. Additionally, abietic acid was significantly less cytotoxic compared to povidone-iodine, and it exerted lower toxicity towards epithelial cells and fibroblasts compared to that against monocytic cells. These data suggest that abietic acid may prove useful as an antibacterial and antibiofilm agent for controlling S. mutans infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Humans coexist with microorganisms such as bacteria, and commensal bacterial flora exists constitutively on the body surface and within internal organs. Among these are more than 700 types of oral bacteria that develop into a biofilm called dental plaque [1, 2]. Within this plaque, pathogenic bacteria colonize and aggregate with non-pathogenic bacteria, causing oral infections such as dental caries [3]. This disease is defined as an oral microbiome dysbiosis and biofilm infection, and it is considered as a worldwide dental care burden.
Although the microbiome within caries lesions is remarkably diverse, acidogenic bacteria such as Streptococcus mutans (S. mutans), a Gram-positive facultative anaerobic bacterium, are responsible for this polymicrobial disease [4]. S. mutans plays the major role in the initial attachment to the tooth surface and the biofilm assembly by producing abundant insoluble glucan, ultimately exacerbating the physical and biochemical virulence of dental plaque [5]. Recent evidence indicates a high prevalence of S. mutans within biofilms where Candida albicans, the most frequently detected oral fungi, resides, and S. mutans enhances the adherence of Candida albicans, suggesting that the interaction between these diverse species may mediate cariogenic development and oral microbiome dysbiosis [6]. Additionally, S. mutans is known to impact the pathogenesis of bacteremia, infective endocarditis, ulcerative colitis, cerebral hemorrhage, and cognitive impairment [7,8,9]. Given these observations, controlling S. mutans infections is highly important for the maintenance of oral and systemic health; however, the increase in the elderly population in Japan has resulted in an increase in the number of patients who are unable to clean their teeth without assistance. Additionally, conventional dental therapy consists mainly of mechanical debridement to remove oral biofilms, a process that is time-consuming, requires special instruments, and increases physical burden, particularly for elderly patients.
Antibiotics are occasionally applied after the removal of oral biofilm; however, long-term usage of antibiotics may result in other problems, such as acquired microbial resistance (AMR) and increased microbial virulence to the body [10, 11]. Long-term usage of antibiotics disrupts the balance of the oral bacterial flora, causing microbial substitution that may result in oral candidiasis and infection by methicillin-resistant Staphylococcus aureus (MRSA) [12, 13]. A number of mouthwashes are commercially available, and povidone-iodine and chlorhexidine are popular for use as antibacterial agents [14]. Povidone-iodine possesses a wide spectrum of antimicrobial activity, has the ability to penetrate biofilms, lacks associated resistance, exhibits anti-inflammatory properties, and causes low cytotoxicity [15]; however, the effectiveness of povidone-iodine in the context of oral care remains unclear [16]. Povidone-iodine, as a mouthwash, may exert only an immediate antibacterial effect [17]. Chlorhexidine is a cationic bisbiguanide possessing broad antibacterial activity, and this compound binds strongly to anionic bacterial cell surface and damages their inner cytoplasmic membrane [18]. Chlorhexidine is, however, known to be inactivated by saliva, pus, and blood [14]. As an increasing number of side effects such as burning sensations, mucosal erosion, and anaphylactic shock have been reported after the use of high concentrations for extended time periods, the use of low concentrations (0.05%) of this compound is thought to be safe, but such concentrations provide little antimicrobial effects [19].
Recently, several reports have suggested the effectiveness of natural products against pathogens responsible for hospital-acquired infection such as Pseudomonas aeruginosa, MRSA, and biofilm-forming bacteria such as Streptococcus mutans [20,21,22,23]. Terpenoid compounds have been found to act as effective biofilm inhibitory agents. Terpene is a carbohydrate refined from plants, insects, and fungi. A constituent of terpene is isoprene, and terpenes are referred to as monoterpene, diterpene, sesquiterpene, and so on according to the number isoprene units [24, 25]. Some types of terpenes, such as paclitaxel, a mitotic inhibitor used in chemotherapy [26], and the analgesic agent menthol [27], have been reported to possess pharmacological effects, antibacterial effects [28, 29], anti-inflammatory effects, anti-viral effects, and anti-tumor effects [26]. In this study, we focused on abietic acid, a diterpene derived from pine rosin (Supplementary Fig. 1) [30]. Abietic acid is a natural compound that is easily obtained and that has several industrial applications, which include glue, ink, varnish, and base material of adhesive plaster. In dental fields, abietic acid is included in products that are already commercially available (temporary sealer; Plast Seal Quick®: Nippon Shika Yakuhin, Yamaguchi, Japan). The pharmacological effects of abietic acid, such as anti-inflammatory effects [31, 32], anti-tumor effects [33, 34], and anti-virus effects [35], have already been reported; however, few reports exist regarding its inhibitory effects on biofilm formation. Ganewatta et al. reported that a polymer containing abietic acid exhibited inhibitory effects on the formation of E. coli and S. aureus biofilms, but the effects on oral biofilms and infections remain unclear [36]. Therefore, we aimed to investigate the antibacterial and antibiofilm effects of abietic acid against cariogenic S. mutans, and we assessed its functionality as an oral agent by examining the cytotoxic effects.
Materials and methods
Reagents
Abietic acid (Sigma-Aldrich, St. Louis, MO, USA) was dissolved to a stock concentration of 25.6 mg/mL in dimethyl sulfoxide (DMSO, Sigma-Aldrich) and used at varying concentrations ranging from 4 to 512 µg/mL. Each solution was diluted using either culture medium or phosphate-buffered saline (PBS). Negative control samples without abietic acid were supplemented with DMSO to a level equivalent to the maximum concentration of DMSO in the abietic acid solution (2.5–20 µL/mL) in each assay. Povidone-iodine (10% Negmin®: Mylan, Tokyo, Japan) and cetylpyridinium chloride (CPC: Merck KGaADarmstadt, Germany) were used as positive controls. Povidone-iodine was diluted to a final concentration of 0.01%, 0.1%, and 1% (1%; the clinical in-use dose). Cetylpyridinium chloride was diluted to a stock concentration of 0.5% using sterilized water and was further diluted to a working concentration of 0.05% (the clinical in-use dose) using the culture medium.
Bacteria
The S. mutans ATCC25175 strain was cultured in tryptic soy broth with yeast extract (TSBY: Becton, Dickinson and Company, Sparks, MD, USA) until logarithmic growth phase. Bacterial suspensions were diluted to 1 × 105 or 1 × 109 with TSBY by measuring the optical density at 660 nm using a photometer (Miniphoto 518R: Taitec, Saitama, Japan), and they were incubated at 37 °C for subsequent assays.
Human cells
A human monocytic cell line (THP-1) and a human epithelial cell line (HeLa) were obtained from ATCC (Manassas, VA, USA). Primary cultured human gingival fibroblasts (HGFs) were isolated from non-inflammatory gingiva of clinically healthy humans after informed consent was obtained as previously described [37]. The study was approved by the Ethics Committee at Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences and Okayama University Hospital (No. 661). HeLa and HGF cells were cultured in Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum (FBS) and 1 × 102 units/mL penicillin–streptomycin solution (Life Technologies). THP-1 cells were incubated in RPMI 1640 medium containing 10% inactivated FBS, 2 mM l-glutamic acid, 1 mM pyruvate sodium, 1 × 102 unit/mL penicillin–streptomycin solution (Life Technologies), and 10 mM HEPES (Sigma-Aldrich). The cells were cultured for 24 h to ensure that the cells were attached prior to subsequent assays.
Bacterial colony-forming ability
To examine planktonic S. mutans, the bacterial culture (1 × 105 CFU/mL) was inoculated in abietic acid or TSBY solution for 1 h at 37 °C. The suspension was serially diluted with PBS, and the 50 µL aliquot was inoculated on Mitis-Salivarius agar plates. The plates were incubated for 48 h at 37 °C, and the number of colonies was counted. To examine biofilm-forming S. mutans, the bacterial culture (1 × 105 CFU/mL) was inoculated into TSBY with 1% sucrose in uncoated glass tubes. The slant culture was allowed to form biofilms for 18 h. Next, the medium was discarded, and the resulting biofilm was immersed in several concentrations of abietic acid or PBS and then incubated aerobically on a horizontal shaker (NR-3: Taitec, Saitama, Japan) at 120 rpm for 1 h at 37 °C. The abietic acid solution was discarded and then washed with PBS three times. The biofilm was then sonicated at 15 kHz for 10 s in PBS on ice using an ultrasonic disruptor (UR21-P: Tomy, Tokyo, Japan) as previously reported [38]. The colony counting on the agar plates was performed as described above. Adenosine triphosphate (ATP) activity of the sonicated biofilm was also measured to evaluate the number of viable bacteria inside the biofilm. The ATP activity was measured using Lucifel-HS (Kikkoman, Tokyo, Japan).
Bacterial growth activity
Turbidity and ATP activity were examined to determine the growth rate of S. mutans (1 × 105 CFU/mL) in abietic acid or TSBY solution. The optical density was measured at 660 nm using an absorption spectrometer (Miniphoto 518R: Taitec) following incubation of the bacterial culture in sterilized glass tubes at 37 °C for up to 18 h. ATP activity of S. mutans was measured using Lucifel-HS (Kikkoman, Tokyo, Japan) after incubation in 96-well plates (Corning, New York, NY, USA) at 37 °C for up to 18 h. Crystal violet staining was performed to quantify the amount of S. mutans biofilm. Bacterial cultures (1 × 105 CFU/mL) were inoculated into abietic acid or TSBY solution with 1% sucrose in 96-well plates and incubated for 12 h. Next, the plates were washed twice with PBS, fixed with 99.8% methanol, and stained with 0.1% crystal violet (Sigma-Aldrich)/PBS solution. Plates were carefully washed with distilled water until the color could no longer be removed, and the remaining stain was eluted by 99.5% ethanol. Absorbance was measured at a wavelength of 595 nm (SH-1000 Lab: Colona Electric Co., Ibaraki, Japan).
Extracellular acidification of bacteria
Acid production by S. mutans was evaluated by measuring the pH of bacterial suspensions as previously reported [39] with some modifications. S. mutans was inoculated into abietic acid or TSBY solution (1 × 105 CFU/mL) and incubated up to 18 h. At each time point, the bacterial culture was centrifuged at 3000 rpm for 10 min, and the pH of the supernatant was measured using a pH meter (Twin pH meter B-212; HORIBA, Kyoto, Japan) at 25 °C.
In situ viability analysis of bacteria
The LIVE/DEAD® BacLight™ Bacterial Viability Kit (Life Technologies, Carlsbad, CA, USA) (Appl Environ Microbiol. 1998) was used to estimate both viable and dead counts of bacteria in the abietic acid solution. The kit is composed of two nucleic acid-binding dyes, including SYTO 9™, which is a green fluorescence pigment that penetrates intact bacterial membranes freely, and propidium iodide, a red fluorescence pigment, which is highly charged and penetrates only damaged membranes. Therefore, simultaneous application of both dyes results in green coloration of viable cells and red coloration of dead cells. The 100 µL aliquots of S. mutans (1 × 105 CFU/mL) in abietic acid or TSBY solution were dispensed into 96-well plates (Corning) and incubated at 37 °C for up to 18 h. For microscopic analysis, S. mutans (1 × 109 CFU/mL) in abietic acid or TSBY solution were incubated at 37 °C for 1 h. The subsequent reactions with dyes were performed following the manufacturer’s protocol. Fluorescence intensity of the stained samples at 530 nm and 630 nm was measured using a fluorophotometer (Gemini XPS: Molecular Devices, Sunnyvale, CA, USA) at an excitation wavelength of 485 nm. The ratio of fluorescence observed at 530 nm to the fluorescence at 630 nm was measured to determine the ratio of the number viable cells to the number of dead cells. Microscopic analysis of the stained samples was performed using a fluorescence microscope (Olympus BX50: Olympus, Tokyo, Japan).
Scanning electron microscopy analysis
Bacterial morphology was observed using a field emission-type scanning electron microscope (FE-SEM DS-720, Topcon, Kyoto, Japan). S. mutans cultures (1 × 105 CFU/mL) in abietic acid/TSBY were incubated in sterilized tubes for 1 h at 37 °C, and 1 mL aliquots of the bacterial suspension were filtered with percolators (SEM pore: JEOL, Tokyo, Japan). Bacteria collected from the filters were fixed with 0.25% formaldehyde/PBS solution, and they were washed with PBS three times. Samples were then evaporated using a vacuum vapor deposition with platinum palladium (Eiko IB-3 Ion Coater:Eiko engineering, Ibaraki, Japan) and observed with SEM at 10.0 kV of accelerating voltage.
Cell cytotoxicity assay
Cytotoxicity was assessed using a reagent containing a tetrazolium compound [3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H tetrazolium, inner salt; MTS] (CellTiter 96® Non-Radioactive Cell Proliferation Assay: Promega, Madison, WI, USA). HeLa cells, HGF (2 × 105 cells/well) and THP-1 cells (1 × 105 cells/well) were treated with several concentrations of abietic acid. After 24 and 48 h of incubation, color development was observed according to the manufacturer’s technical bulletin. The absorbance was then measured at a wavelength of 490 nm (SH-1000 Lab: Colona Electric Co., Ibaraki, Japan).
Statistical analysis
All results were confirmed with at least three independent experiments, each of which was performed in triplicate. The data are presented as the mean ± standard deviation (SD) from at least three independent experiments. One-way analysis of variance (ANOVA) was used to test the difference between three or more groups, and a multiple comparison test was further conducted by the Tukey–Kramer test. Statistical analysis was performed using the JMP Statistics Software Package (SAS Institute, Cary, NC), and p < 0.05 indicates statistical significance.
Results
Effects of abietic acid on colony-forming ability of S. mutans
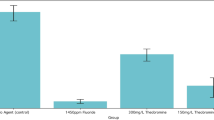
To examine the effects of abietic acid on the colony-forming ability of planktonic S. mutans, the bacteria were treated with abietic acid at varying concentrations in the growth medium, and this was followed by bacterial colony counting (Fig. 1a). The number of S. mutans decreased in a dose-dependent manner, and 50% minimum inhibitory concentration (MIC50) was determined to be 16 µg/mL of abietic acid and 0.1% of povidone-iodine. The effects of abietic acid were significant at a concentration of 64 µg/mL (7 ± 5%, p < 0.001 vs. no drug). We also examined viable cell count by sonicating the S. mutans biofilms treated with abietic acid (Fig. 1b). A 16 µg/mL concentration of abietic acid did not have any effect on S. mutans in the biofilm; however, above this concentration, the cell number decreased in a dose-dependent manner, and the effects were significant at a concentration of 64 µg/mL abietic acid (11 ± 7%, p < 0.001 vs. no drug). ATP activity of S. mutans in biofilm exhibited a pattern similar to that of colony-forming ability (Fig. 1c). The 16 µg/mL and 32 µg/mL concentrations of abietic acid did not have any effect on ATP activity; however, 64 µg/mL and 128 µg/mL concentrations of abietic acid decreased the ATP activity, and the inhibitory effects caused by 128 µg/mL abietic acid were approximated at 80% (83 ± 7%, p < 0.01 vs. no drug).
Antibacterial effects of abietic acid on colony-forming ability. The y-axis shows the relative change in viable cell count (vs. no drug) for a Colony number of planktonic S. mutans treated with the stimulus for 1 h and b Colony number of S. mutans recovered from sonic-disrupted biofilms treated with the stimulus for 1 h, and the ATP activity for c ATP activity of S. mutans recovered from sonic-disrupted biofilms treated with the stimulus for 1 h. The x-axis shows the concentration of abietic acid and povidone-iodine. DMSO (5 µL/mL) was used as the solvent for abietic acid. Stimulation with povidone-iodine served as a positive control. The dotted line shows 50% inhibition. n = 3 *p < 0.01, **p < 0.001 (vs. no drug)
Effects of abietic acid on S. mutans growth, acid production, and biofilm formation
Bacterial growth was examined by measuring bacterial turbidity following serial dilution of abietic acid based on the data described as shown in Fig. 1 (Fig. 2a). Although 4 µg/mL abietic exerted no effect on growth, 16 µg/mL abietic acid was effective in decreasing the turbidity, and the inhibitory effects were approximated at 80% after 12 h (79 ± 8%, p < 0.001 vs. no drug). Both, abietic acid at 64 µg/mL concentration and the positive control (1% povidone-iodine), inhibited bacterial viability by nearly 100%, and the effects of abietic acid on ATP activity of S. mutans were also evaluated (Fig. 2b). Abietic acid at a concentration of 4 µg/mL was still found to exert no effect on ATP activity. In the presence of 16 µg/mL of abietic acid, the curve of ATP activity exhibited a low inclination compared to that of the negative controls after 12 h. The ATP activity, however, continuously increased and reached high levels similar to those of the negative controls after 18 h. The ATP activity remained unchanged in the presence of 64 µg/mL of abietic acid, indicating bacteriostatic effects of abietic acid on bacterial growth. Abietic acid concentrations of 4 µg/mL and 16 µg/mL caused acidification of S. mutans to approximately pH 4.5 after 12 h and 18 h, respectively. In the presence of 64 µg/mL abietic acid, however, the pH remained stable (pH 6.7 ± 0.05), demonstrating the inhibitory effect of abietic acid on S. mutans acidification (Fig. 2c). Biofilm formation was examined by a crystal violet staining assay after a 12-h treatment with abietic acid. The low concentrations of abietic acid (4 µg/mL and 16 µg/mL) did not exert any effect on S. mutans biofilm formation; however, the inhibitory effect was significant in the presence of 64 µg/mL abietic acid (99 ± 0.4%, p < 0.001 vs. no drug) (Fig. 2d).
Antibacterial effects of abietic acid on growth, acidification, and biofilm. The effects of abietic acid on bacterial growth, acid production, and biofilm formation were examined using S. mutans treated with several concentrations of abietic acid for up to 18 h. DMSO (2.5 µL/mL) was used as the solvent for abietic acid. Stimulation with povidone-iodine (1%) served as a positive control. a The y-axis shows the turbidity of the bacterial culture measured by spectrometry. A660: absorbance at 660 nm. n = 3 **p < 0.001 (vs. no drug). b Luciferase was measured as a reporter of ATP concentration in growing S. mutans. The y-axis shows luciferase activity (relative light units; RLU). n = 3 **p < 0.001 (vs. no drug). c The alteration of pH of the bacterial culture by abietic acid was measured by a pH meter. n = 3 **p < 0.001 (vs. no drug). dS. mutans biofilms were formed by incubating with 1% sucrose for 12 h. After crystal violet staining, the absorbance of the staining was measured to quantify biofilm formation. The y-axis shows the absorbance at 595 nm (A595). n = 3 **p < 0.001 (vs. no drug)
Effects of abietic acid on S. mutans viability
Fluorometric viability was determined using two nucleic acid-binding dyes, SYTO 9™ and propidium iodide (Fig. 3a). After 18 h, the intensity of the red fluorescence was significantly high in the presence of 16 µg/mL of abietic acid (1.7-fold, p < 0.001 vs. no drug; 1.6-fold, p < 0.001 vs. 4 µg/mL abietic acid), indicating that the bacterial membrane was disrupted by 16 µg/mL of abietic acid. Both 64 µg/mL of abietic acid and the positive control (1% povidone-iodine) induced similar patterns of intensity to those observed in the presence of 16 µg/mL of abietic acid. The fluorescence microscopy image indicated that red fluorescence was sporadically observed in the presence of 16 µg/mL abietic acid and more frequently in samples treated with 64 µg/mL of abietic acid and positive controls (1% povidone-iodine and 0.05% CPC). Little red fluorescence was observed in the presence of 4 µg/mL abietic acid (Fig. 3b).
Antibacterial effects of abietic acid on bacterial viability. In situ fluorescence viability analysis of S. mutans was performed. DMSO (2.5 µL/mL) was used as the solvent for abietic acid. Stimulation with povidone-iodine (1%) and CPC (0.05%) served as a positive control for bactericidal action. SYTO 9 (green: viable cells); propidium iodide (red: dead cells). a Fluorophotometric measurement was performed using S. mutans treated with several concentrations of abietic acid for 18 h. The y-axis shows ratio of green/red fluorescence as indicated by the intensity at the wavelength of 530 nm divided by that of 630 nm, and the horizontal axis shows the culture periods. n = 3 **p < 0.001 (vs. no drug). b Fluorescence microscopic analysis was performed using S. mutans incubated in abietic acid/TSBY solution for 1 h. Scale bar 100 µm. Three independent experiments were performed, and representative images are shown (color figure online)
Effect of abietic acid on S. mutans morphology
Morphology of S. mutans was observed by SEM after 1 h of treatment with abietic acid at 37 °C (Fig. 4). In S. mutans treated with a serial dose of abietic acid, a structural change was visible, where the bacterial surfaces became rough and irregular. There was no significant difference in the surfaces between samples of varying abietic acid concentrations. In contrast, bacterial surfaces were partially disrupted, and the bacterial extracellular matrixes were visible in the S. mutans treated with povidone-iodine or CPC.
Effect of abietic acid on S. mutans morphology. S. mutans was treated with several concentrations of abietic acid for 1 h, and bacterial morphologies were examined by SEM. Stimulation with povidone-iodine and CPC served as a positive control for bactericidal action. Three independent experiments were performed, and representative images are shown. Scale bar 1 µm
Cell toxicity of abietic acid on human cell lines
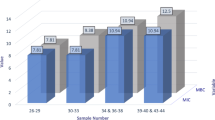
Cytotoxicity of abietic acid on HeLa cells, THP-1 cells, and HGF was examined by MTS assay. Varying concentrations of abietic acid were used, including effective antibacterial concentrations up to 128 µg/mL. No cell toxicity was observed, but rather, proliferative effects on HeLa cells and HGF were observed after 24 and 48 h of stimulation (Fig. 5a and b). The higher concentrations of abietic acid (512 µg/mL) showed toxicities similar to those induced by 1% povidone-iodine (data not shown). Toxicities of abietic acid on THP-1 cells were more significant, at a moderate concentration of abietic acid compared to cytotoxicity observed in other cell types, and 64 µg/mL concentrations or higher were toxic after 24 and 48 h (Fig. 5c).
Cytotoxicity of abietic acid in human cells. Cytotoxicity of abietic acid on a HGF, b HeLa cells, and c THP-1 cells was examined using MTS assay for 24 (closed square) and 48 h (square). DMSO (5 µL/mL) was used as the solvent for abietic acid. Stimulation with povidone-iodine (1%) served as a positive control for bactericidal action. The y-axis shows the relative ratio to A490 (absorbance at 490 nm) of negative control (no drug added) after 24 h and 48 h. n = 3 *,†p < 0.01, **,††p < 0.001 (vs. no drug)
Discussion
Extensive antibiotic use over the past decades has led to the emergence and spread of antibiotic-resistant bacteria [40, 41]. The medical society is now facing the necessity to establish new approaches for controlling bacterial infections, including bacterial biofilm-related oral diseases. Bactericidal agents, such as povidone-iodine, are effective for preventing oral bacteremia; however, these treatments are occasionally harmful for the normal mouth flora, especially in elderly patients. Therefore, bacteriostatic natural products are ideal for daily and continued use as anti-oral infection agents. Povidone-iodine is a complex of iodine and polyvinylpyrrolidone. Iodine is slowly released from the complex, and it can penetrate the biofilms and bacterial membranes [42]. In the presence of abietic acid (> 64 µg/mL), bacterial colony number and ATP activity were significantly decreased, although the antimicrobial effect on S. mutans was found to be less for the biofilm form than the planktonic form. Although the underlying mechanism for penetration into biofilms remains unclear, abietic acid is certainly capable of antibiofilm effects similar to those induced by povidone-iodine.
The time-course analysis of S. mutans growth indicated that effective concentrations of abietic acid (64 µg/mL) inhibited bacterial growth and acid production, but they did not decrease ATP activity. This suggests that abietic acid does not annihilate bacteria, and instead inhibits their acidogenic ability and growth (bacteriostatic). As 64 µg/mL of abietic acid significantly inhibited S. mutans biofilm formation, long-term use of this bacteriostatic agent may be useful to prevent S. mutans biofilm infection with less side effects, such as microbial substitution.
As described above, iodine can penetrate the bacterial membrane, enter into the cytosol, and inhibit protein synthesis [42]. In the presence of abietic acid, bacterial surfaces observed by SEM were rough despite the absence of bacteriolysis. Therefore, the effect of abietic acid on bacterial membranes was examined by fluorometric viability using two nucleic acid-binding dyes, SYTO 9 and propidium iodide. The green fluorescence pigment (SYTO 9) recognizes all bacteria, and the red fluorescence pigment (propidium iodide) recognizes nucleic acids through injured cell walls, and thus a large ratio of red fluorescence intensity indicates that bacterial cell walls were damaged functionally despite no significant morphological injury. In the presence of 64 µg/mL abietic acid, bacterial nucleic acid was stained strongly with propidium iodide, while the bacterial ATP synthesis activities were maintained. Therefore, high concentration of abietic acid may damage cell walls to some degree, but the functional damage may be minimal. Further investigation is required to determine the underlying mechanism.
In vitro analysis indicated that abietic acid exhibited no cytotoxicity to epithelial cells and mesenchymal fibroblasts under 128 µg/mL and caused cytotoxicity to monocytic cells at concentrations over 64 µg/mL. For future clinical use, the antibacterial effects on other bacterium, such as obligate anaerobes, should be further examined, and the optimum concentration for abietic acid-induced growth inhibition should be determined. Abietic acid could be used in the production of oral rinse products for the control of oral infections while lessening the toxicity to epithelial cells and fibroblasts. Additionally, further studies will support the development of an antimicrobial filling material that contains abietic acid for dental caries treatment.
This study assessed the effects of abietic acid using only a single strain of S. mutans ATCC25175. As S. mutans has been subclassified into several types based on different immunological, biological, and genetic properties [43], it is necessary to investigate the effects of abietic acid using other types of S. mutans. Additionally, it is already evident that oral bacteria, including both cariogenic and periodontal pathogenic bacteria, are involved in systemic diseases both directly and indirectly [44]. The influence of Porphyromonas gingivalis on gut microflora [45] and the influence of the genus Fusobacterium on colorectal cancer [46] are particularly focused. Therefore, it is important to investigate the effects of abietic acid using oral biofilms consisting of many bacterial species, including both commensal and pathogenic bacteria. Further studies, including clinical trials, should be performed to establish an ideal system for preventing oral biofilm infections without cytotoxicity and excessive disruption of normal bacterial flora.
In conclusion, this study highlighted the observation that abietic acid inhibited S. mutans ATCC25175 growth in both planktonic and biofilm, acid production, and biofilm formation. Abietic acid exerted its effects with no significant damage to cell walls, and the antibacterial effects appear to be bacteriostatic. Although further research is required to clarify the underlying mechanism, abietic acid could provide a useful tool for controlling oral infections by inhibiting oral bacterial growth and biofilm formation.
References
Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol. 2005;43:5721–32.
Paster BJ, Olsen I, Aas JA, Dewhirst FE. The breadth of bacterial diversity in the human periodontal pocket and other oral sites. Periodontology. 2000;2006(42):80–7.
Cisar JO, Kolenbrander PE, McIntire FC. Specificity of coaggregation reactions between human oral Streptococci and strains of Actinomyces viscosus or Actinomyces naeslundii. Infect Immun. 1979;24:742–52.
Simón-Soro A, Mira A. Solving the etiology of dental caries. Trends Microbiol. 2015;23(2):76–82.
Bowen WH, Koo H. Biology of Streptococcus mutans-derived glucosyltransferases: role in extracellular matrix formation of cariogenic biofilms. Caries Res. 2011;45(1):69–86.
Metwalli KH, Khan SA, Krom BP, Jabra-Rizk MA. Streptococcus mutans, Candida albicans, and the human mouth: a sticky situation. PLoS Pathog. 2013;9(10):e1003616.
Nakano K, Hokamura K, Taniguchi N, Wada K, Kudo C, Nomura R, Kojima A, Naka S, Muranaka Y, Thura M, Nakajima A, Masuda K, Nakagawa I, Speziale P, Shimada N, Amano A, Kamisaki Y, Tanaka T, Umemura K, Ooshima T. The collagen-binding protein of Streptococcus mutans is involved in haemorrhagic stroke. Nat Commun. 2011;2:485.
Kojima A, Nakano K, Wada K, Takahashi H, Katayama K, Yoneda M, Higurashi T, Nomura R, Hokamura K, Muranaka Y, Matsuhashi N, Umemura K, Kamisaki Y, Nakajima A, Ooshima T. Infection of specific strains of Streptococcus mutans, oral bacteria, confers a risk of ulcerative colitis. Sci Rep. 2012;2:332.
Watanabe I, Kuriyama N, Miyatani F, Nomura R, Naka S, Nakano K, Ihara M, Iwai K, Matsui D, Ozaki E, Koyama T, Nishigaki M, Yamamoto T, Tamura A, Mizuno T, Akazawa K, Takada A, Takeda K, Yamada K, Nakagawa M, Tanaka T, Kanamura N, Friedland RP, Watanabe Y. Oral Cnm-positive Streptococcus Mutans expressing collagen binding activity is a risk factor for cerebral microbleeds and cognitive impairment. Sci Rep. 2016;9(6):38561.
Fung-Tomc J. Correlation of in vitro and in vivo resistance development to antimicrobial agents. Antimicrob Newslett. 1990;7:17–24.
Pallasch TJ, Slots J. Antibiotic prophylaxis and the medically compromised host. Periodontology. 2000;1996(10):107–38.
Scully C, El-Kabir M, Samaranayake LP. Candida and oral candidosis: a review. Crit Rev Oral Biol Med. 1994;5:125–57.
Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R. Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis. J Antimicrob Chemother. 2008;61:26–38.
Brecx M, Netuschil L, Hoffmann T. How to select the right mouthrinses in periodontal prevention and therapy. Part II. Clinical use and recommendations. Int J Dent Hyg. 2003;1(4):188–94.
Bigliardi PL, Alsagoff SAL, El-Kafrawi HY, Pyon JK, Wa CTC, Villa MA. Povidone iodine in wound healing: a review of current concepts and practices. Int J Surg. 2017;44:260–8.
Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI. Prevention of ventilator-associated pneumonia with oral antiseptics: a systematic review and meta-analysis. Lancet Infect Dis. 2011;11(11):845–54.
Addy M, Wright R. Comparison of the in vivo and in vitro antibacterial properties of providone iodine and chlorhexidine gluconate mouthrinses. J Clin Periodontol. 1978;5(3):198–205.
Jones CG. Chlorhexidine: is it still the gold standard? Periodontology 2000. 1997;15:55–62.
Krautheim AB, Jermann TH, Bircher AJ. Chlorhexidine anaphylaxis: case report and review of the literature. Contact Dermat. 2004;50(3):113–6.
Aremu OS, Gopaul K, Kadam P, Singh M, Mocktar C, Singh P, Koorbanally NA. Synthesis, characterization, anticancer and antibacterial activity of some novel pyrano [2,3-d] pyrimidinone carbonitrile derivatives. Anticancer Agents Med Chem. 2017;17:719–25.
Chung PY, Toh YS. Anti-biofilm agents: recent breakthrough against multi-drug resistant Staphylococcus aureus. Pathog Dis. 2014;70:231–9.
Perumal S, Mahmud R. Chemical analysis, inhibition of biofilm formation and biofilm eradication potential of Euphorbia hirta L. against clinical isolates and standard strains. BMC Complement Altern Med. 2013;13:346.
Wu CY, Su TY, Wang MY, Yang SF, Mar K, Hung SL. Inhibitory effects of tea catechin epigallocatechin-3-gallate against biofilms formed from Streptococcus mutans and a probiotic lactobacillus strain. Arch Oral Biol. 2018;26:69–77.
Keeling CI, Bohlmann J. Genes, enzymes and chemicals of terpenoid diversity in the constitutive and induced defense of confers against insects and pathogens. New Phytol. 2006;170:657–75.
Kitaoka N, Lu X, Yang B, Peters RJ. The application of synthetic biology to elucidation of Plant mono-, sesqui-, and diterpenoid metabolism. Mol Plant. 2015;8:6–16.
Kowalski RJ, Giannakakou P, Hamel E. Activities of the microtubule-stabilizing agents epothilones A and B with purified tubulin and in cells resistant to paclitaxel (Taxol®). J Biol Chem. 1997;272:2534–41.
Galeotti N, Di Cesare Mannelli L, Mazzanti G, Bartolini A, Ghelardini C. Menthol: a natural analgesic compound. Neurosci Lett. 2002;322(3):145–8.
Horiuchi K, Shiota S, Hatano T, Yoshida T, Kuroda T, Tsuchiya T. Antimicrobial activity of oleanolic acid from Salvia officinalis and related compounds on vancomycin-resistant enterococci (VRE). Biol Pharm Bull. 2007;30:1147–9.
Raut JS, Shinde RB, Chauhan NM, Karuppayil SM. Terpenoids of plant origin inhibit morphogenesis, adhesion, and biofilm formation by Candida albicans. Biofouling. 2013;29:87–96.
Zeiss HH. The chemistry of the resin acids. Chem Rev. 1948;42:163–87.
Fernández MA, Tornos MP, García MD, de Heras B, Villar AM, Sáenz MT. Anti-inflammatory activity of abietic acid, a diterpene isolated from Pimenta recemosa var. grissea. J Pharm Pharmacol. 2001;53:867–72.
Kim NH, Son Y, Jeong SO, Hur JM, Bang HS, Lee KN, Kim EC, Chung HT, Pae HO. Tetrahydroabietic acid, a reduced abietic acid, inhibits the production of inflammatory mediators in RAW264.7 macrophages activated with lipopolysaccharide. J Clin Biochem Nutr. 2010;46:119–25.
Ukiya M, Kawaguchi T, Ishii K, Ogihara E, Tachi Y, Kurita M, Ezaki Y, Fukatsu M, Kushi Y, Akihisa T. Cytotoxic activities of amino acid-conjugate derivatives of abietane-type diterpenoids against human cancer cell lines. Chem Biodivers. 2013;10:1260–8.
Yoshida N, Takada T, Yamamura Y, Adachi I, Suzuki H, Kawakami J. Inhibitory effects of terpenoids on multidrug resistance-associated protein 2- and breast cancer resistance protein-mediated transport. Drug Metab Dispos. 2008;36:1206–11.
Ohtsu H, Tanaka R, In Y, Matsunaga S, Tokuda H, Nishino H. Abietane diterpenoids from the cones of Larix kaempferi and their inhibitory effects on Epstein-Barr virus activation. Planta Med. 2001;67:55–60.
Ganewatta MS, Miller KP, Singleton P, Mehrpouya-Bahrami P, Chen YP, Yan Y, Nagarkatti M, Nagarkatti P, Decho AW, Tang C. Antibacterial and biofilm-disrupting coatings from resin acid-derived materials. Biomacromol. 2015;16:3336–44.
Naruishi K, Takashiba S, Nishimura F, Chou HH, Arai H, Yamada H, Murayama Y. Impairment of gingival fibroblast adherence by IL-6/sIL-6R. J Dent Res. 2001;80:1421–4.
Matsumi Y, Fujita K, Takashima Y, Yanagida K, Morikawa Y, Matsumoto-Nakano M. Contribution of glucan-binding protein A to firm and stable biofilm formation by Streptococcus mutans. Mol Oral Microbiol. 2015;30:217–26.
Song JH, Kim SK, Chang KW, Han SK, Yi HK, Jeon JG. In vitro inhibitory effects of Polygonum cuspidatum on bacterial viability and virulence factors of Streptococcus mutans and Streptococcus sobrinus. Arch Oral Biol. 2006;51(12):1131–40 (Epub).
Almagor J, Temkin E, Benenson I, Fallach N, Carmeli Y, DRIVE-AB consortium. The impact of antibiotic use on transmission of resistant bacteria in hospitals: Insights from an agent-based model. PLoS One. 2018;13:e0197111.
World Health Organization (WHO). Antimicrobial resistance: global report on surveillance. Geneva: WHO; 2014.
Krzyściak W, Jurczak A, Kościelniak D, Bystrowska B, Skalniak A. The virulence of Streptococcus mutans and the ability to form biofilms. Eur J Clin Microbiol Infect Dis. 2014;33:499–515.
Hamada S, Slade HD. Biology, immunology, and cariogenicity of Streptococcus mutans. Microbiol Rev. 1980;44(2):331–84.
He J, Li Y, Cao Y, Xue J, Zhou X. The oral microbiome diversity and its relation to human disease. Folia Microbiol. 2015;60:69–80.
Arimatsu K, Yamada H, Miyazawa H, Minagawa T, Nakajima M, Ryder MI, Gotoh K, Motooka D, Nakamura S, Iida T, Yamazaki K. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci Rep. 2014;6:4828.
Kostic AG, Gevers D, Pedamallu CS, Michaud M, Duke F, Earl AM, Ojesina AI, Jung J, Bass AJ, Tabernero J, Baselga J, Liu C, Shivdasani RA, Ogino S, Meyarson M. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res. 2012;22:292–8.
Acknowledgements
The authors would like to thank Prof. Teruo Kuroda, Department of Microbiology, School of Pharmaceutical sciences, Hiroshima University, for his support from the beginning of this research. We would like to express our gratitude to Prof. Hiroshi Maeda, Department of Endodontics, Osaka Dental University, for his continuous dedication to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest regarding this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10266_2019_456_MOESM1_ESM.tiff
Supplementary Fig. 1: Structural formula of abietic acid: Terpenes consist of isoprene units with 5 carbons. Abietic acid is a diterpene derived from four isoprenes (molecular weight: 302.44)
Rights and permissions
About this article
Cite this article
Ito, Y., Ito, T., Yamashiro, K. et al. Antimicrobial and antibiofilm effects of abietic acid on cariogenic Streptococcus mutans. Odontology 108, 57–65 (2020). https://doi.org/10.1007/s10266-019-00456-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-019-00456-0