Abstract
The purpose of this in vitro study was to compare the stress distribution and natural frequency of different shape and thickness retainer designs for maxillary posterior resin-bonded prostheses using finite element (FE) method. A 3D FE model of a three unit posterior resin-bonded prosthesis analysis model was generated. Three different shaped retainer designs, viz. C-shaped (three axial surface wraparounds), D-shaped (three axial surface wraparounds with central groove) and O-shaped (360° wraparounds), and three different thicknesses, viz., 0.4, 0.8, and 1.2 mm, resin-bonded prostheses were used in this study. The resin-bonded prosthesis analysis model was imported into an FE analysis software (ANSYS 10.0, ANSYS, USA) and attribution of material properties. The nodes at the bottom surface of the roots were assigned fixed zero displacement in the three spatial dimensions. A simulated angle of 45° loading of a 100 N force was applied to the node of the pontic lingual cusp surface. The stress distributions and corresponding natural frequencies were analyzed and resolved. The C-shaped retainer for 0.4 mm thickness recorded the greatest von Mises stresses of 71.4 MPa for all three groups. C-shaped, D-shaped and O-shaped retainer presented natural frequencies 3,988, 7,754, and 10,494 Hz, respectively. D-shaped retainer and O-shaped retainer increased natural frequencies and structural rigidity over the traditional C-shaped retainer. The maximum von Mises stresses values of the remaining tooth and prosthesis decreased with greater retainer thickness. D-shaped retainer and O-shaped retainer increased natural frequencies and structural rigidity over the traditional C-shaped retainer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Compared with traditional fixed partial dentures (FPDs), the main advantage of using resin-bonded prostheses is the preservation of dental hard tissues, following the concept of so-called minimal invasive dentistry. Resin-bonded prostheses are considered a viable alternative to conventional FPDs [1–3]. However, the bite forces challenge the retainer rigidity and adhesive bond between the restoration and dental tissues that may lead to failure and clinical debonding. Unfortunately, debonding has been the main disadvantage of this innovative technique. Consequently, the success rate of resin-bonded prostheses is directly related to the tooth preparation design for good retention and resistance form. With regard to the high patient satisfaction and relatively low incidence of failures and complications, the clinical performance of non-retentive resin-bonded prostheses can be considered satisfactory [4].
In industry, it is a conventional and successful method to apply a modal analysis to determine the characteristics, such as natural frequencies and mode shapes, of a material structure or a machine component while it is being designed [5]. The natural frequency in Hz is used as an indicator for assessing the stability in the design of a structure. Mechanically thinking, the natural frequency of an object is strongly correlated to the stability of the structure [6]. Some previous researches have been performed using natural frequency for the quantitative assessment of the early detection of a dental implant stability [7, 8] and metal frameworks of removable partial dentures [9]. However, relatively little information is known or has been published about the effect of natural frequency for resin-bonded prostheses.
From a biomechanical perspective, the retainers are important structures that connect the bridgework and abutment teeth and allow the transfer of the bite force. Nair et al. [10] evaluated the effects of different groove length and thickness of the retainers on the retention of maxillary anterior base metal resin-bonded retainers. Their results showed that placement of the grooves increased the retention values almost 2.5 times compared with the grooveless preparation and retention value was directly proportional to the groove length and retainer thickness. el Salam et al. [11] evaluated the effect of various tooth preparation designs, in this case the C-shape or with occlusal coverage and opposing grooves, on the bond strength for resin-bonded prostheses. The results suggested that a combination of 180° opposing groove placement at line angles “wraparound” and occlusal coverage resulted in the greatest bonding values. Nemoto et al. [12] reported on the design of resin-bonded prostheses with zirconia frameworks. Three types of frameworks were fabricated as 0.5 and 0.8 mm thick zirconia frameworks with grooves and holes and 0.5 mm thick zirconia frameworks without grooves and holes. The result suggests that the retention form had a significant effect on decreasing the framework deformation, indicating that the resin-bonded prostheses that use a 0.5 mm thick zirconia framework are effective for replacing a single anterior missing tooth. Lin et al. [13] evaluated the C-shaped retainer design factors using the finite element analysis: three values of retainer thicknesses (1.2, 0.8 and 0.4 mm), with the heights of 100, 75 and 50 % of the distance from 2 mm above the cement-enamel junction to the occlusal surface, and at an angle of the axial surface extensions (150°, 180° and 210°) were selected as the design parameters. The simulated results showed that the averaged stress values of the remaining tooth and prosthesis decreased with greater retainer thickness and height as a result of increasing prosthesis stiffness and maximizing of the bonding area between the enamel and the retainer, respectively.
However, sparse research has been conducted to compare the traditional C-shaped retainer to D-shaped and O-shaped retainer designs of resin-bonded prostheses. Previous studies have been based on empirical designs for posterior resin-bonded prostheses retainer. Botelho et al. [14, 15] introduced a D-shaped retainer that seems to increase structural rigidity over the traditional C-shaped framework. This D-shaped retainer was considered adequate to resist distortion during function. However, data are still scarce for supporting this assumption and a deeper analysis is merited on this topic. This paper is focusing on the effect of different shaped retainer designs, namely applying a three unit posterior resin-bonded prosthesis analysis model on three different shaped retainer designs, viz. C-shaped, D-shaped and O-shaped, and with three different thicknesses, viz., 0.4, 0.8, and 1.2 mm, for maxillary posterior resin-bonded prostheses using finite element static and modal analyses.
Materials and methods
Three-dimensional (3D) finite element (FE) model
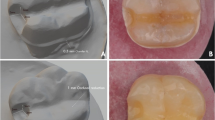
A 3D FE model was generated in four steps. First, a high-resolution 3D X-ray CT scanner (Alphard-3030, Asahi Roentgen, Kyoto, Japan) was used to scan the tooth at a voxel dimension of 100 μm. Exposure time was 17 s/frame. One slice out of every 10 slices was used for the modeling (i.e. 50 slices out of 501 slices).
Second, a medical image processing software (Mimics 10.0; Materialise, Leuven, Belgium) interactively read CT data in the DICOM (Digital Imaging and Communications in Medicine) format. Enamel, dentin, pulp 3D object were created by growing threshold regions on the entire stack of scans. Figure 1 shows an example of the segmentation and the reconstruction steps.
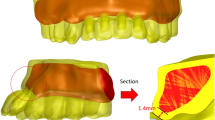
Third, primitive shapes, i.e. mainly rounded inserts and cylinders, and an enamel 3D object were used to create the surface of resin-bonded prosthesis. Three different shaped retainer designs (D-shaped, C-shaped, O-shaped) and with three different thicknesses (0.4, 0.8, and 1.2 mm) resin-bonded prostheses were created in this study.
Mimics MedCAD function, Boolean Minus, Unite function and remesh function were used to simulate resin-bonded prosthesis preparation, and to establish and assemble congruence of the interfacial mesh between the different objects that are thus enamel, dentin, pulp, resin-bonded prosthesis. All unwanted surfaces and interfaces were deleted as is the custom procedure. After remesh, a 3D object which contained the interfaces of interest was then converted into a 3D file using the Mimics Ansys area file (.lis) output format.
Then, fourth, the definitive Mimics Ansys area file (.lis) which contained all parts was then imported into an FEA software (ANSYS 10.0, ANSYS) and transformed areas to each part of volume for the generation of the volumetric meshes, with a total of 61,616 elements/12,329 nodes and attribution of material properties according to existing data. Automatic mesh generation using a tetrahedral mesher (tetrahedron elements with pyramid like shape and four nodal points) was ideally achieved.
Material properties, loading and boundary conditions
Material properties used in this study for FE analysis are listed in Table 1. Material properties were assumed to be isotropic, homogeneous, and linear-elastic. The stiffness of the pulp was not considered since its Young’s modulus is much lower than those of the other materials.
The nodes at the bottom surface of the roots were assigned fixed as zero displacement in the 3 spatial dimensions. To simulate usage of adhesive luting resin composite cements, the tooth and restorative materials were estimated to be bonded uniformly and perfectly. In order to simulate functional cusp loading in working side of jaw, a 100 N loading was applied to a node of the pontic (lingual cusp incline) at an angle of 45° from the buccal direction. The stress distributions, natural frequencies and mode shapes of the first vibrational mode were solved using the FE analysis software ANSYS 10.0.
Results
Localized high stress concentration was observed around the connectors in all simulated models (cf. Fig. 2a and Table 1).The maximum von Mises stresses values [20–22] in remaining tooth and prosthesis, and natural frequencies of the prosthesis are shown in Table 2. The C-shaped retainer for 0.4 mm thickness recorded the greatest von Mises stresses 71.4 MPa for all three groups. Figure 2b is a schematic drawing that illustrated the loading direction. Figure 3 shows the von Mises stress distributions for different designs of 0.8 mm retainer. The stress values in the top end of C-shaped wing were the lowest for all three groups. It can also be seen that stress values of the D-shaped retainer of 0.8 mm thickness were 23 % lower than C-shaped retainer.
Figure 4 presents the mode shapes of the vibrating resin-bonded prostheses and the natural frequencies of 0.8 mm retainer. The plane of the first vibrational mode bending axis for C-shaped retainer almost paralleled to the X–Z plane, however, the plane of bending axis for D-shaped retainer and O-shaped retainer almost paralleled to the X–Y plane, which was perpendicular to the C-shaped retainer’s. C-shaped, D-shaped and O-shaped retainer presented natural frequencies 3,988, 7,754, 10,494 Hz, respectively. D-shaped retainer and O-shaped retainer increased natural frequencies and structural rigidity over the traditional C-shaped retainer. The O-shaped retainer recorded the greatest natural frequencies and resistance to dislodgment.
Discussion
In FEA, the Mimics segmentation and editing tools enable to manipulate the data to enamel, dentin, soft tissue, etc. Once an area of interest is separated, it can be visualized in 3D presentation. The value of biting force has been reported to be as high as 790 N [23]. However, it has to be remembered that the load of 790 N is the so-called peak load. Given this, the average applied load in dysfunction such as bruxism may be as high as 225 N (s.d. 130 N) [23]. Distributed over a number of worn teeth, this would result in much lower stress applied to each tooth. Mean masticatory forces have been reported by Anderson [24, 25] to be in the range of 70.6–146.1 N. Thus, the applied 100 N load in this present study lies within the range of these values in this study.
The success rate of resin-bonded prostheses is directly related to the tooth preparation design for good retention and resistance form [12]. Retainers of C-shaped, D-shaped and O-shaped resin-bonded prostheses are located above the retention line of the tooth. There is only little space in molars and premolars due to occluding cusps. As a result, a tooth preparation is required to assure the clearance of the retainers for C-shaped, D-shaped and O-shaped resin-bonded prostheses in molars and premolars.
This FE study used von Mises stress as the stress assessment indicator. The von Mises stress also called the equivalent stress. Based on the failure mode of a material being due to distortional energy caused by a stress state, the von Mises stress is a single normal stress value, which is equivalent to an actual combined state of stress [26]. The maximum-distortion-energy theory predicts elastic failure when the von Mises stress reaches the yield strength.
The optimal adhesion simulated in our model does not represent the clinical situation where a repetitive fatigue loading situation is characteristic. Nevertheless, this the optimal adhesion between the retainer and abutment teeth has been approved in previous simulations that can significantly analysis the risk for retainer/abutment interface failure [27, 28]. By evaluating the resultant of static stress and natural frequencies on FE models, we will explore the debonding failure of different retainer designs and study the properties of the different thicknesses. Omission of resin cement lute might influence the accuracy of the mechanical responses. However, the aim of this study was to understand the biomechanical performances with multiple retainer design factors and their interactions of resin-bonded prosthesis under sufficient interfacial bonded strength between metal and abutment teeth.
In general, the first vibrational mode is bending mode, the second mode is a torsion vibration, and the third mode is an axial vibration. Let alone, the bite force status of resin-bonded prostheses is intimately associated with bending mode. Therefore, natural frequencies and mode shapes of the first vibrational mode were analyzed in this present study.
In a previous study, Lin et al. [13] reported no stress differences were found according to the angle of the C-shaped retainer extension because stress transmission was concentrated at the connectors. In this present study, the C-shaped retainer did not transmit the simulated bite force to the top end of the C-shaped wing. The result was in agreement with some previous reports [13–15]. However, one of the most important factors that influenced the stress distributions for the resin-bonded prosthesis models was certainly the retainer shape used in this study. The conventional C-shaped retainers were in general more flexible in the wings which may cause that they debond relatively easily. This was not only attributed to the limited surface area of C-shaped retainer for bonding, but it is also correlating with the stability of the C-shaped structure. Given this, greater rigidity conferred by D-shaped and O-shaped retainer, along with the greater surface area for bonding, may have been contributed for the elevated forces to debond the resin-bonded prostheses.
This investigation has evaluated the effect of retainer thickness for posterior resin-bonded prostheses using finite element static and modal analyses. Botelho et al. [14, 15] have reported the clinical cases about C-shaped, D-shaped and O-shaped resin-bonded prostheses. Evidence-based information continues to accumulate on improved design features and tooth preparations for resin-bonded prostheses. However, long-span and C-shaped RBFDP designs still appear to show significantly more debonds than O-shaped and D-shaped prostheses. The clinical evaluation of thick retainer (0.8, and 1.2 mm) that reduce inter-abutment stresses may lead to further advancement in our knowledge on how to make more retentive resin-bonded prostheses. The design principles for such resin-bonded prostheses require an abutment with periodontal health, appropriate periodontal support, a minimum retainer thickness of 0.8–1.2 mm, an O-shaped and D-shaped wraparound and/or the use of grooves or slots on the major and minor retainer. The results of this finite element analysis study supported some previous findings and lead to a finding that the stress values of the remaining tooth and prosthesis (restoration) decreased with greater retainer thickness. Clinical studies are required to validate this FE analysis hypothesis.
Conclusions
The following conclusions may be drawn from this study:
-
Stress concentrations were found to be higher in the C-shaped retainer resin-bonded prostheses than in the D-shaped and O-shaped retainer groups.
-
The D-shaped and O-shaped retainer provided more even stress distribution for resin-bonded prostheses than the traditional C-shaped retainer.
-
The maximum von Mises stresses values of the remaining tooth and prosthesis decreased with greater retainer thickness.
-
The D-shaped retainer and O-shaped retainer increased the natural frequencies and structural rigidity over the traditional C-shaped retainer.
References
van Heumen CC, Tanner J, van Dijken JW, Pikaar R, Lassila LV, Creugers NH, Vallittu PK, Kreulen CM. Five-year survival of 3-unit fiber-reinforced composite fixed partial dentures in the posterior area. Dent Mater. 2010;26:954–60.
Lin J, Shinya A, Gomi H, Shinya A. Bonding of self-adhesive resin cements to enamel using different surface treatments: bond strength and etching pattern evaluations. Dent Mater J. 2010;29:425–32.
Botelho MG. Improved design of long-span resin-bonded fixed partial dentures: three case reports. Quintessence Int. 2003;34:167–71.
Boening KW, Ullmann K. A retrospective study of the clinical performance of porcelain-fused-to-metal resin-bonded fixed partial dentures. Int J Prosthodont. 2012;25:265–9.
Verma SP, Girgis RS. Resonance frequencies of electrical machine stators having encased construction, Part I: derivation of the general frequency equation. IEEE T Power Ap Syst. 1973;PAS-92:1577–85.
Verma SP, Girgis RS. Experimental verification of resonant frequencies and vibration behaviour of stators of electrical machines, Part 1: Models, experimental procedure and apparatus. IET Electr Power App. 1981;128:12–21.
Huang HM, Chiu CL, Yeh CY, Lee SY. Factors influencing the resonance frequency of dental implants. J Oral Maxillofac Surg. 2003;61:1184–8.
Huang HM, Chiu CL, Yeh CY, Lin CT, Lin LH, Lee SY. Early detection of implant healing process using resonance frequency analysis. Clin Oral Implants Res. 2003;14:437–43.
Inoue T, Oki M, Phankosol P, Ohyama T, Taniguchi H. Vibration analysis of maxillary removable partial denture frameworks. J Oral Rehabil. 2002;29:341–9.
Nair A, Regish KM, Patil NP, Prithviraj DR. Evaluation of the effects of different groove length and thickness of the retainers on the retention of maxillary anterior base metal resin bonded retainers-an in vitro study. J Clin Exp Dent. 2012;4:e91–6.
El Salam Shakal MA, Pfeiffer P, Hilgers RD. Effect of tooth preparation design on bond strengths of resin-bonded prostheses: a pilot study. J Prosthet Dent. 1997;77:243–9.
Nemoto R, Nozaki K, Fukui Y, Yamashita K, Miura H. Effect of framework design on the surface strain of zirconia fixed partial dentures. Dent Mater J. 2013;32:289–95.
Lin CL, Hsu KW, Wu CH. Multi-factorial retainer design analysis of posterior resin-bonded fixed partial dentures: a finite element study. J Dent. 2005;33:711–20.
Botelho MG, Leung KC, Ng H, Chan K. A retrospective clinical evaluation of two-unit cantilevered resin-bonded fixed partial dentures. J Am Dent Assoc. 2006;137:783–8.
Botelho MG, Dyson JE. Long-span, fixed-movable, resin-bonded fixed partial dentures: a retrospective, preliminary clinical investigation. Int J Prosthodont. 2005;18:371–6.
Hasegawa A, Shinya A, Lassila LV, Yokoyama D, Nakasone Y, Vallittu PK, Shinya A. Accuracy of three-dimensional finite element modeling using two different dental cone beam computed tomography systems. Odontology. 2013;101:210–5.
Manly Richard S, Hodge Harold C, Ange Louise E. Density and refractive index studies of dental hard tissues: II. Density distribution curves. J Dent Res. 1939;18:203–11.
Hase H, Shinya A, Yokoyama D, Shinya A, Takahashi Y. Three-dimensional finite element analysis of Aramany class IV obturator prosthesis with different clasp designs. Dent Mater J. 2014;33:383–8.
Morris HF. Veterans administration cooperative studies project no. 147/242, part VII: the mechanical properties of metal ceramic alloys as cast and after simulated porcelain firing. J Prosthet Dent. 1989;61:160–9.
Shinya A, Yokoyama D, Lassila LV, Shinya A, Vallittu PK. Three-dimensional finite element analysis of metal and FRC adhesive fixed dental prostheses. J Adhes Dent. 2008;10:365–71.
Lin J, Shinya A, Gomi H, Shinya A. Finite element analysis to compare stress distribution of connector of lithia disilicate-reinforced glass-ceramic and zirconia-based fixed partial denture. Odontology. 2012;100:96–9.
Lin J, Shinya A, Lassila LVJ, Vallittu PK. Composite resin reinforced with pre-tensioned fibers: a three-dimensional finite element study on stress distribution. Odontology. 2013;101:29–33.
Nishigawa K, Bando E, Nakano M. Quantitative study of bite force during sleep associated bruxism. J Oral Rehabil. 2001;28:485–91.
Anderson DJ. Measurement of stress in mastication. I. J Dent Res. 1956;35:664–70.
Anderson DJ. Measurement of stress in mastication. II. J Dent Res. 1956;35:671–3.
Warren CY, Richard GB. Roark’s formulas for stress and strain. 7th ed. New York: McGraw-Hill; 2002. p. 41–6.
Yokoyama D, Shinya A, Gomi H, Vallittu PK, Shinya A. Effects of mechanical properties of adhesive resin cements on stress distribution in fiber-reinforced composite adhesive fixed partial dentures. Dent Mater J. 2012;31:189–96.
Zheng Z, Lin J, Shinya A, Matinlinna JP, Botelho MG, Shinya A. Finite element analysis to compare stress distribution of gold alloy, lithium-disilicate reinforced glass ceramic and zirconia based fixed partial denture. J Investig Clin Dent. 2012;3:291–7.
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, J., Zheng, Z., Shinya, A. et al. Structural stability of posterior retainer design for resin-bonded prostheses: a 3D finite element study. Odontology 103, 333–338 (2015). https://doi.org/10.1007/s10266-014-0173-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-014-0173-2